Performing and Processing FNA of Anterior Fat Pad for Amyloid
Summary
Fat pad aspiration is a preferred, minimally invasive, and low cost approach as compared to other methods to detect amyloid for diagnosis of systemic amyloidosis. This video article demonstrates a procedural outline for performing fat pad aspiration with appropriate processing of the specimen for the optimal diagnostic outcome.
Abstract
Historically, heart, liver, and kidney biopsies were performed to demonstrate amyloid deposits in amyloidosis. Since the clinical presentation of this disease is so variable and non-specific, the associated risks of these biopsies are too great for the diagnostic yield. Other sites that have a lower biopsy risk, such as skin or gingival, are also relatively invasive and expensive. In addition, these biopsies may not always have sufficient amyloid deposits to establish a diagnosis. Fat pad aspiration has demonstrated good clinical correlation with low cost and minimal morbidity. However, there are no standardized protocols for performing this procedure or processing the aspirated specimen, which leads to variable and nonreproducible results. The most frequently utilized modality for detecting amyloid in tissue is an apple-green birefringence on Congo red stained sections using a polarizing microscope. This technique requires cell block preparation of aspirated material. Unfortunately, patients presenting in early stage of amyloidosis have minimal amounts of amyloid which greatly reduces the sensitivity of Congo red stained cell block sections of fat pad aspirates. Therefore, ultrastructural evaluation of fat pad aspirates by electron microscopy should be utilized, given its increased sensitivity for amyloid detection. This article demonstrates a simple and reproducible procedure for performing anterior fat pad aspiration for the detection of amyloid utilizing both Congo red staining of cell block sections and electron microscopy for ultrastructural identification.
Protocol
Introduction
Systemic amyloidosis is a highly variable disease that refers to extracellular deposition of various proteins that are collectively referred to as amyloid. Deposition of these amyloid fibrils with beta pleated configuration leads to various clinical presentations depending on the organs involved. The most clinically relevant manifestations of systemic amyloidosis are noted when there is involvement of critical organs such as the heart, liver, and/or kidney. Historically, these involved organs would be biopsied to demonstrate the presence of amyloid. These moderately invasive procedures carried a significant risk including hemorrhage. Fat pad aspiration has since been shown to provide a reliable and noninvasive method for the detection of amyloid in systemic amyloidosis 1. This procedure is essentially comparable to the liposuction of the subcutaneous fat in the anterior abdominal wall under local anesthesia to retrieve fibroadipose tissue for evaluating scant amyloid deposits in small blood vessel walls 2.
The most frequently utilized method for amyloid identification in tissue remains the characteristic apple-green birefringence pattern seen when Congo red stained sections are visualized under a polarized light microscope 3. When fat pad aspiration is performed, Congo red stains can be done on either direct smeared slides or cell block preparations of the aspirated adipose tissue. However, patients in early stages of amyloidosis have scant amyloid deposits, which greatly reduces the sensitivity of Congo red stained cell block sections 4,5. Ultrastructural evaluation of fat pad aspirates by electron microscopy has better reproducibility and improved sensitivity 4. Therefore, it is recommended to submit all fat pad aspirates for both preparation of a cell block and for performing electron microscopy 2.
Fat pad aspiration is a relatively low cost and noninvasive method for obtaining tissue to diagnose systemic amyloidosis. This article describes fat pad aspiration procedure along with details about sample processing to submit specimen for both Congo red staining and ultrastructural evaluation by electron microscopy. In this video, we demonstrate this reproducible and simple procedure to retrieve optimal diagnostic material.
1. Performing the FNA of Anterior Fat Pad
A. Anesthetization of the local area (Figure 1 & 2)
- Using alcohol swabs or the skin cleansing agent preferred by a particular institution, clean the skin on the lower quadrant area of the abdomen lateral to the midline and below the umbilicus (Figure 1).
- Mark a rhomboid shaped area about 2 x 2 inches as shown in Figure 1 with a marking pen.
- Aspirate approximately 10 mL of 1% lidocaine with an 18G needle. Attach a 25G 1 ½ inch needle to the syringe. Remove any trapped air by tapping the upright syringe while pressing the plunger until liquid is dispensed and no air bubbles are present.
- Anesthetize along the borders of the rhomboid area already marked as shown in Figure 2. Start by inserting the 25G needle just under the skin at point A and carefully push the needle subcutaneously to point X. Pull back on the syringe plunger to ensure that you are not within a vessel. Then slowly push the plunger to infiltrate up to 2.5 mL of lidocaine (about ¼ of the lidocaine in 10 mL syringe) while withdrawing the needle to point A without letting the needle come out of the skin at point A (Figure 2a3). With the needle still under the skin change the direction towards point Y (Figure 2a4) and push the needle subcutaneously to point Y (Figure 2b1). As before, confirm that the needle is not in a vessel and dispense approximately 2.5 mL of lidocaine while slowly withdrawing the needle through point A (Figure 2b3 through 2b4). Repeat similar steps starting from point B and dispensing lidocaine subcutaneous from points B to X and B to Y (Figure 2c1 through 2d4). Prevent bleeding from the pricks A and B by firm application of sterile gauge piece.
- You may now check that the area is anesthetized by lightly touching the skin within the anesthetized rhomboid by tip/corner of cotton gauze piece, by comparing with adjacent unanesthetized skin.
B. Performing fat pad aspiration (Figure 3)
(Application of local anesthesia prior to performance of fat pad aspiration may be bypassed, depending on the regional and individual preferences. Properly performed FNAB procedure for anterior fat pad aspiration can be completed in one prick. However, depending on the pain threshold of individual patient, maneuvering of 18G needle back and forth in to the subcutaneous fat tissue is relatively distressing. The anesthetization method described here achieves the effect in only two pricks with 25G needle and averts the pain with improved tolerance to the procedure.)
- Assemble 18G 1 ½ inch needle onto a 10 mL syringe. Mount the syringe-needle assembly in the syringe grip (“FNAB grip/gun”) for proper application and release of vacuum.
- Insert the tip of the needle into the subcutaneous fat within the cleansed and anesthetized rhomboid area (Figure 3a).
- Fully retract the plunger of the syringe with the needle inserted in the subcutaneous tissue to generate vacuum (Figure 3b).
- Maintain the vacuum and maneuver the needle back and forth in various directions in to the subcutaneous fat (Figure 3c through 3i). Each stroke should be as long as possible with the length of the needle selected without letting the needle come out of the skin. Maximum sampling is achieved by changing direction with each stroke (Figure 3i). It is important to keep the direction of the needle tangential to the serosa and parallel to the skin surface to avoid puncturing of the peritoneal cavity.
- The fibroadipose tissue accumulates in the syringe. Once enough fibroadipose tissue fragments (up to 1 mL of fragments rich blood mixed specimen) are retrieved, release the vacuum completely and remove the needle (Figure 3k).
- Have the patient or the assistant apply firm pressure on the area of procedure with a pad of gauze to prevent extravasation of blood.
2. Specimen Processing
- Place at least 5-6 fragments of fibroadipose tissue in glutaraldehyde solution for electron microscopy (Figure 4B).
- Depending on the institutional protocol, a few smears of the fibroadipose tissue fragments may be prepared by spreading them between two slides (Figure 4A).
- The remaining material is allowed to clot in the syringe (this may take 5-7 minutes, depending on the clotting time) (Figure 4C).
- Aspirate 10% formalin in the syringe so that the clotted fibroadipose tissue material is dislodged from the wall of the syringe and free floating (Figure 4C2). Remove the plunger from the syringe (Figure 4C3) and transfer the clotted fibroadipose tissue into the 10% formalin container from the open end of the syringe opposite the nozzle end (Figure 4C4).
- Label the containers appropriately and submit the glutaraldehyde for electron microscopy and the formalin for H & E section and Congo red stain for evaluation under polarizing microscopy. If smears are prepared, they may be processed according to the protocol of the individual laboratory.
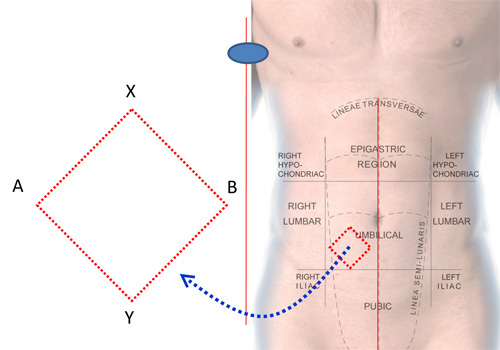
Figure 1. Area to be anesthetized for FNAB of anterior fat pad.

Figure 2. Anesthetization of the local area.
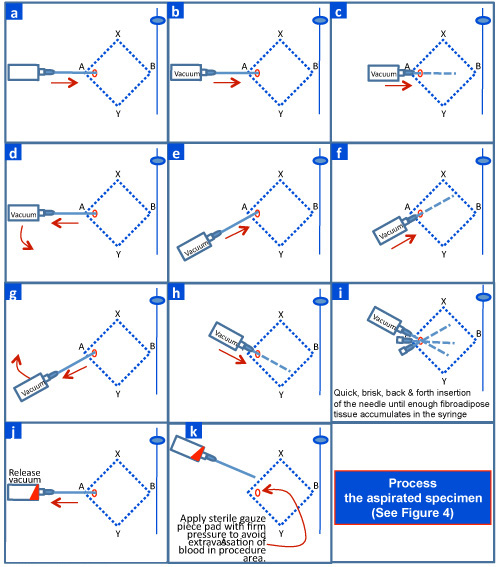
Figure 3. Performing FNAB of anterior fat pad.
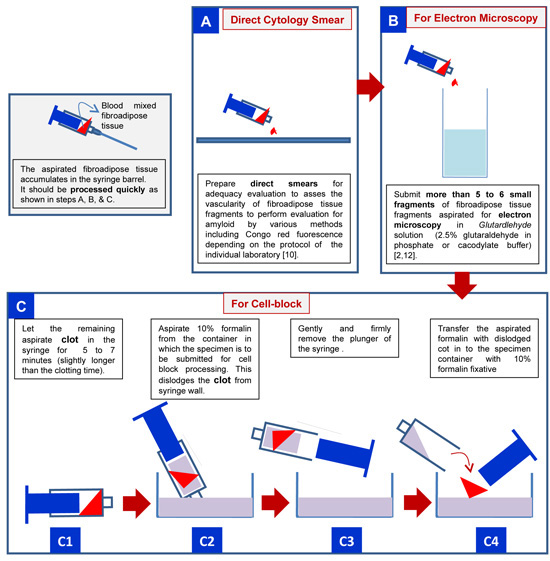
Figure 4. Processing of anterior fat pad aspirate to be submitted to laboratory for detecting amyloid deposits.
3. Representative Results
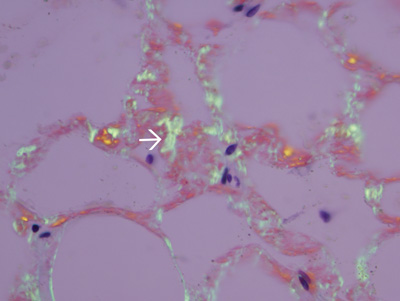
Figure 5. Amyloid in the wall of small blood vessels in fibroadipose tissue fragments. Fibroadipose tissue was formalin-processed, paraffin embedded, stained with Congo red, and examined by polarizing light microscopy. Amyloid in the wall of small blood vessels shows apple green birefringence (white arrow).
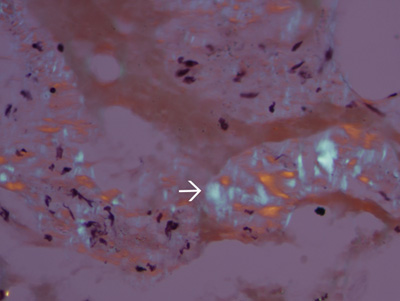
Figure 6. Tissue lacking amyloidosis. The apple green birefringence is absent in tissues of a different patient without amyloidosis. Blue birefringence (white arrow) of collagen fibers, are usually present in almost all specimens.
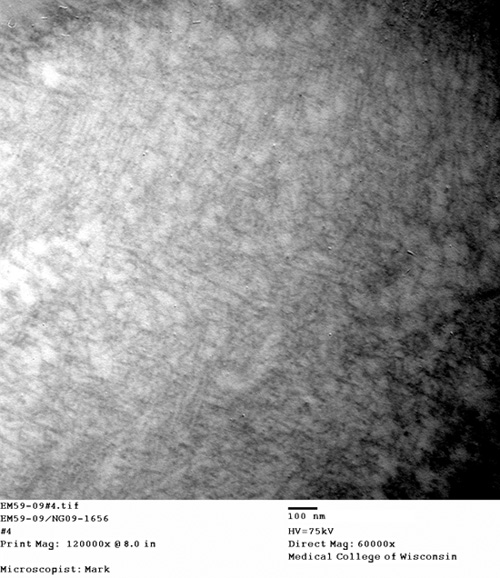
Figure 7. Fibrils consistent with amyloid in the blood vessel wall. Electron micrograph of straight, non-branching, randomly-scattered 8-10 nm diameter fibrils formed by amyloid in the blood vessel wall.
Discussion
Diagnosis of amyloidosis is usually achieved with a tissue biopsy of the affected organs such as the kidney, liver, and/or heart. This approach has high diagnostic yield, however, is invasive and may be associated with complications including hemorrhage 2. Rectal, gingival, and bone marrow biopsies were preferred for diagnosis as relatively less invasive approach in 1960s 6,7,8. Abdominal fat pad aspiration was reported in 1973 as a safe, minimally invasive, simple, and less expensive procedure for the tissue diagnosis of systemic amyloidosis 1. However, the details of the procedure and approach to processing of the retrieved specimen is not coherently reported. This video and the article describe the procedure step by step.
The approach for detecting amyloid in fat pad aspiration, similarly, is also not well standardized with a few studies comparing and evaluating various approaches 1,5,6,7,8. Evaluation of anterior fat pad aspirates with Congo red staining is less sensitive with lower interobserver reproducibility especially in early cases of amyloidosis with scant amyloid deposits 5. Immunohistochemistry performed on formalin fixed paraffin-embedded cell block sections and Congo red fluorescence performed on cytology smears have been reported to improve the diagnostic sensitivity 9,10. Electron microscopy improves the detection and identification of scant amyloid fibrils in small blood vessel walls in the fibroadipose tissue in fat pad aspirates 4, 5. Based on this information, this article describes processing of the specimen to prepare cell blocks (for evaluation of Congo red stained cell block sections under polarizing microscope for diagnostic apple green birefringence and also for immunohistochemistry as indicated) and for electron microscopy. However, depending on the approach selected for evaluation of the specimen for amyloid, it may be subjected to cytology smear preparation, cell block preparation, and processing for electron microscopy. Some laboratories perform the tests on the smears prepared from the aspirated fibroadipose tissue fragments and stained with Congo red to study the fluorescence 10.
Generally in a late amyloidosis, the light microscopy with Congo red polarizing microscopy may be sufficient; however, in early stages of the disease Congo red staining with polarizing microscopy on cell block sections is less sensitive and reliable for fat pad aspirates 4,5,11. Other special stains including Thioflavin T may be used with similar limitations. Other approaches to detect amyloid include evaluation of the aspirate smears for amyloid with Congo red polarizing microscopy and fluorescence 10. In our experience this method is less reproducible. Evaluation of the blood vessels in fat pad for amyloid by electron microscopy overcomes these limitations 4,11. Further characterization of amyloid has been reported by immunoelectron microscopy 12; however, these methods may not be available widely in a non-tertiary care setting.
Needles used for performing aspiration procedures may be categorized according to their gauge sizes into fine (21-25G), intermediate (18-20G), and large (eg- 14G) 11. Anterior fat pad aspirations have been reported to be performed by using variable gauges ranging from intermediate (18 to 20G) to fine (21 to 22G) 2,10. Most of the mass lesions are aspirated with finer gauge needles (such as 25G) to obtain good cytology smears along with additional passes with wider gauge needle (such as 18G) to retrieve additional sample for cell blocks.
During anterior fat pad aspiration, the cohesive fibroadipose tissue does not aspirate well with finer needles. Cell block preparation and electron microscopy are important for evaluation of small blood vessel walls in fibroadipose tissue fragments in the fat aspirates. Wider gauge needles (such as 18G) are recommended to yield diagnostic adequate material 2,10. As the procedure is comparable to the conventional FNAB, fat pad aspiration is referred to as FNAB even though wider gauge needles may be used for performing it 5.
Disclosures
The authors have nothing to disclose.
Acknowledgements
We thank Ms. Bonnie Phetteplace, RN for assistance during video graphing the FNAB procedure demonstration.
Materials
Alcohol swabs, gauze pads, marking pen, 10 mL syringes x2, 1% lidocaine (local anesthetic- If lidocaine is used alone, it causes an initial burning sensation after instillation. This can be prevented by using a 1:1 mixture of 1% lidocaine and 1% sodium-bi-carbonate), 18 gauge(G) 1 ½ inch needles x2 (for performing FNAB), 25G 1 ½ inch needle (for injecting local anesthetic), FNA syringe holder (“gun”), bandage, vial of glutaraldehyde (for electron microscopy), and biopsy container of 10% formalin.
References
- Westermark, P., Stenkvist, B. A new method for the diagnosis of systemic amyloidosis. Arch Intern Med. 132, 522-523 (1973).
- Devata, S., Hari, P., Markelova, N., Li, R., Shidham, V. B. Detecting AL Amyloid in Abdominal fat pad aspirates: Is Congo red sufficient?. Amyloid. , .
- Merlini, G., Bellotti, V. Molecular Mechanisms of Amyloidosis. New Engl J Med. 349 (6), 583-596 (2003).
- Shidham, V. B., Kumar, N., Cihlar, K., Varsegi, G., Markelova, N., Li, R., Hari, P. Fine needle aspiration of abdominal fat pad for diagnosis of early amyloidosis: How can the clinical role of the test be improved?. Mod Pathol. 20, 1A-380A (2007).
- Halloush, R., Lavrovskaya, E., Mody, D., Lager, D., Truong, L. D. Diagnosis and typing of systemic amyloidosis: The role of abdominal fat pad fine needle aspiration. Cytojournal. 6, 24-24 (2010).
- Hazenberg, I. I., Rijswijk, C. V. a. n., H, M. Diagnostic Accuracy of Subcutaneous Abdominal Fat Tissue Aspiration for Detecting Systemic Amyloidosis and Its Utility in Clinical Practice. Arthritis Rheum. , 54-546 (2006).
- Guy, C. D., Jones, C. K. Abdominal fat pad aspiration biopsy for tissue confirmation of systemic amyloidosis: specificity, positive predictive value, and diagnostic pitfalls. Diagn Cytopathol. 24, 181-185 (2001).
- Westermark, P. Diagnosing Amyloidosis. Scand J Rheumatol Suppl. 24, 327-329 (1995).
- Linke, R. P. Highly Sensitive Diagnosis of Amyloid and Various Amyloid Syndromes Using Congo Red Fluorescence. Virchow Arch. 436, 439-448 (2000).
- Giorgadze, T. A., Shiina, N., Baloch, Z. W., Tomaszewski, J. E., Gupta, P. K. Improved detection of amyloid in fat pad aspiration: an evaluation of Congo red stain by fluorescent microscopy. Diagn Cytopathol. 31, 300-306 (2004).
- DeMay, R. M. Fine Needle Aspiration Biopsy. The Art & Science of Cytopathology. , 465-46 (1996).
- Arbustini, E., Vrga, L., Concardi, M., Pallandini, G., Obici, L., Merlini, G. Electron and Immuno-electron Microscopy of Abdominal Fat Identifies and Characterizes Amyloid Fibrils in Suspected Cardiac Amyloidosis. Amyloid. 9, 108-114 (2002).

