Electrophysiological Measurements and Analysis of Nociception in Human Infants
Summary
The assessment and treatment of pain in infants is difficult because infants cannot verbally report their experience. In this video we describe quantitative electrophysiological methods and analysis techniques that can be used to measure the response to noxious events from the infant nervous system.
Abstract
Pain is an unpleasant sensory and emotional experience. Since infants cannot verbally report their experiences, current methods of pain assessment are based on behavioural and physiological body reactions, such as crying, body movements or changes in facial expression. While these measures demonstrate that infants mount a response following noxious stimulation, they are limited: they are based on activation of subcortical somatic and autonomic motor pathways that may not be reliably linked to central sensory processing in the brain. Knowledge of how the central nervous system responds to noxious events could provide an insight to how nociceptive information and pain is processed in newborns.
The heel lancing procedure used to extract blood from hospitalised infants offers a unique opportunity to study pain in infancy. In this video we describe how electroencephalography (EEG) and electromyography (EMG) time-locked to this procedure can be used to investigate nociceptive activity in the brain and spinal cord.
This integrative approach to the measurement of infant pain has the potential to pave the way for an effective and sensitive clinical measurement tool.
Protocol
Before any studies can be conducted on infants’ ethical approval and informed written parental consent needs to be sought.
In this study ethical approval was obtained from the University College Hospital Ethics Committee and informed written parental consent was obtained before each procedure. This study conformed to the standards set by the Declaration of Helsinki and Good Clinical Practice guidelines.
1. Data collection – setup
- Place a minimum of 16 individual disposable EEG Ag/AgCl cup electrodes on the infant’s head after skin prepping according to the 10-20 electrode placement system (Figure 1A). More comprehensive coverage can be achieved using an EEG cap with embedded electrodes. Use of an EEG cap makes the process faster and less disruptive, particularly as electrodes are prepared with inductive gel before placing the cap on the head. The application of disposable EEG electrodes requires more time and skill, but generally results in a better recording. Consider reducing the number of electrodes if access to the infant is limited, but always use midline electrodes (Cz, CPz and FCz). Use FCz as the reference electrode for the recording.
- Use EEG conductive paste to optimise electrode/skin electric coupling.
- Place an elastic net over the electrodes to hold them in place.
- Tie the electrode leads together to minimise electrical interference.
- Place a ground electrode onto the chest or head.
- Place EMG electrodes on the biceps femoris of both legs after skin prepping (Figure 1B).
- To record ECG activity place lead 1 ECG electrodes onto the body after skin prepping (one electrode on the left side of the chest, one on the right and use the same ground electrode as for the EEG).
- Place a movement transducer on the abdomen to measure respiration.
- Place a pulse oximeter probe on the foot to measure oxygen saturation and heart rate. Make sure that the probe is secured in place and that a continuous signal is recorded without dropouts. The oximeter probe needs to be placed on the foot that is contralateral to the foot which you intend to stimulate.
- Set up a tripod-mounted camcorder to frame the face of the infant so that changes in facial expression can be recorded.
- Place a light-emitting diode (LED) in the camera frame. The LED is linked to the timing circuit so that it will flash when stimulation is presented to synchronise the EEG, EMG and video recording.
2. Data collection – recording
- Start video recording.
- Start pulse oximetry recording.
- Start EEG/EMG recording.
- Wait until the infant is settled.
- Hold the foot as if performing a heel lance and manually event mark the EEG and EMG recordings. This epoch will be used to identify a section of control background EEG and EMG.
- Apply touch stimulation by lightly tapping a rubber bung that is attached to the arm of a tendon hammer against the surface of the heel. Stimulate the foot that is not attached to the pulse oximeter. When the infant is stimulated the EEG/EMG and video recording must be event-marked in order to identify the time in the recording when the stimulation took place. The touch stimulation can be event-marked by attaching an impedance head to the tendon hammer which electronically links the stimulator to the recording equipment. The video recording is event-marked by the LED flash. Repeated touches may be applied and the stimulus can be applied to different regions of the body, i.e. the shoulder
- Apply a non-noxious control stimulation by rotating the lancet by 90 degrees and placing it against the foot so that when the spring-loaded blade is released it does not contact the skin. This event can be time-locked using an accelerometer attached to the top surface of the lance. The accelerometer detects the vibration that occurs when the blade is released.
- Perform the clinically-essential heel lance in accordance with clinical practice in the neonatal unit. Wait until the EEG activity is settled before doing the heel lance. Time-locking of the heel lance can be performed in the same way as for the control stimulation. Following the heel lance, do not squeeze the foot for at least 30 seconds to ensure that the recorded responses are solely due to the lance.
- Ensure that the required quantity of blood is collected and prepare the samples for clinical analysis.
- Save the data and stop all the recordings.
- Record the infant’s demographic information and the experimental details and input them into a database for safe storage and future reference.
- Repeat this procedure in the required sample of infants. In this example the number of infants = 23.
3. EEG data analysis
- Create EEG epochs of 1.7 seconds that correspond to each touch, control and lance stimulation and background EEG. Epochs should start 0.6 seconds before each event. The number of epochs corresponding to each modality should be the same.
- Baseline correct the epochs by subtracting the mean baseline signal and high-pass filter them at 0.1 Hz.
- Consider the epochs recorded at CPz or Cz for further analysis and exclude epochs which were contaminated by movement artefact. Movement artefact is defined as a change in amplitude greater than 50μV in less than 50ms.
- Align the traces to correct for latency jitter between 50 and 300 ms post stimulation and conduct Principal Component Analysis (PCA) in this time interval to identify the tactile potential (i.e. EEG activity related to tactile stimulation). Consider the epochs to be the variables and the time points the observations. PCA decomposes the EEG epochs into basic waveforms, termed principal components (PCs) and represent systematic variation in the amplitude of the signal across time points.
- Run one-way analysis of variance (ANOVA) on the weights of each of the first 2 PCs to determine which PC represents the tactile potential. This will be the PC whose weights were significantly larger following tactile stimulation compared to background EEG.
- Align the traces to correct for latency jitter between 300 and 700 ms post stimulation and conduct PCA in this time interval.
- Run one-way ANOVA on the weights of each of the first 2 PCs to determine which PC represents the nociceptive-specific potential. This will be the PC whose weights were significantly larger following noxious stimulation compared to tactile stimulation and background EEG.
4. EMG data analysis
- Calculate the root-mean-square (RMS) of the EMG signal in the first 1000 ms post stimulation for the control and lance stimuli.
- Perform a t-test on the RMS values to determine the nociceptive-specific spinal reflex withdrawal.
5. Representative Results
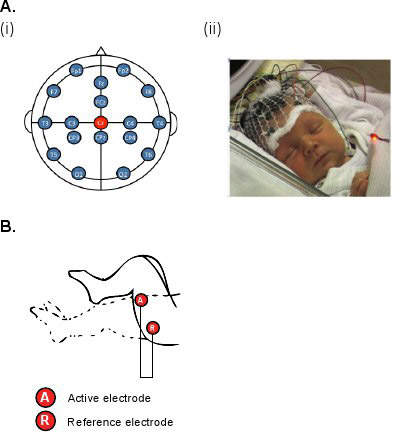
Figure 1. (A) (i) Diagram and (ii) photo of the electrode placements for EEG recordings (modified international 10/20 electrode placement system); (B) Diagram of the electrode placements for EMG recordings on the biceps femoris.
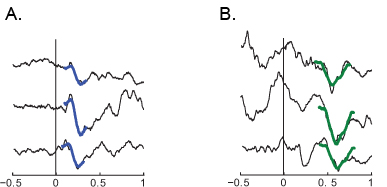
Figure 2. (A) Examples of the sensory potential at Cz evoked by touch in 3 infants; (B) examples of the nociceptive-specific potential at Cz evoked by noxious lance in 3 infants.
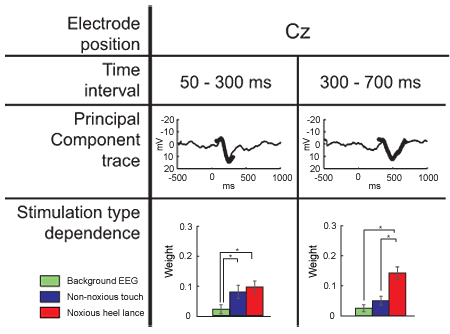
Figure 3. Dependence of the PC weights on stimulus modality at Cz (mean ± SEM). The PC obtained between 50-300 ms after the stimulus onset represents a tactile potential and the PC obtained between 300-700 ms after the stimulus onset represents a nociceptive-specific potential. The PCs (bold lines) are overlaid on the grand averages obtained across all stimulation types (background EEG, touch, noxious lance) after the individual traces were aligned in the stated time interval.

Figure 4. (A) Example of EMG activity in one infant after (i) noxious heel lance and (ii) touch of the heel. (B) Mean (±SE) EMG root-mean-square EMG activity in infants after the noxious heel and non-noxious touch stimuli.
Discussion
This video shows how electrophysiological responses, evoked by tactile and noxious stimulation, can be characterised in the human infant using EEG and EMG recordings. Studies of this type will help to understand the development and plasticity of human pain processing, and lead to improved clinical assessment and treatment of infant pain 1, 2.
The success of these experiments requires the close collaboration of a multidisciplinary team. Expertise is required in the field of neonatology, clinical neurophysiology, bioengineering and developmental neuroscience.
It is essential that the infant’s care take highest priority when these experiments are undertaken. The research nurse or doctor who performs the heel lance has responsibility for the infant’s wellbeing and needs to ensure that the experiment is done in accordance with clinical practice. Approval from the hospital ethical committee and written parental consent are necessary to undertake these studies.
The heel lance is a clinically-required event and cannot be repeated for the purpose of the study. It is therefore essential that the recording is collected in a reliable and robust way that does not interfere with clinical practice 3, 4. In particular, it is crucial that the method used to time-lock the stimulation is reliable and does not impede the clinical blood collection.
All the measures of infant pain are necessarily indirect, as such it is important to ascertain that the recorded activity is specifically evoked by the noxious event and not other aspects of the infant’s care 2. This can be achieved via careful technical design and post-processing of the data.
Disclosures
The authors have nothing to disclose.
Acknowledgements
This work was funded by the Wellcome Trust.
References
- Fitzgerald, M., Walker, S. M. Infant pain management: a developmental neurobiological approach. Nat. Clin. Pract. Neurol. 5 (1), 35-35 (2009).
- Slater, R. Oral sucrose as an analgesic drug for procedural pain in newborn infants: a randomised controlled trial. Lancet. 376 (9748), 1225-1225 (2010).
- Slater, R. Evoked potentials generated by noxious stimulation in the human infant brain. Eur. J. Pain. 14 (3), 321-321 (2010).
- Slater, R. Premature infants display increased noxious-evoked neuronal activity in the brain compared to healthy age-matched term-born infants. Neuroimage. 52 (2), 583-583 (2010).

