Non-invasive Optical Imaging of the Lymphatic Vasculature of a Mouse
Summary
Recently developed imaging techniques using near-infrared fluorescence (NIRF) may help elucidate the role the lymphatic system plays in cancer metastasis, immune response, wound repair, and other lymphatic-associated diseases.
Abstract
The lymphatic vascular system is an important component of the circulatory system that maintains fluid homeostasis, provides immune surveillance, and mediates fat absorption in the gut. Yet despite its critical function, there is comparatively little understanding of how the lymphatic system adapts to serve these functions in health and disease1. Recently, we have demonstrated the ability to dynamically image lymphatic architecture and lymph “pumping” action in normal human subjects as well as in persons suffering lymphatic dysfunction using trace administration of a near-infrared fluorescent (NIRF) dye and a custom, Gen III-intensified imaging system2-4. NIRF imaging showed dramatic changes in lymphatic architecture and function with human disease. It remains unclear how these changes occur and new animal models are being developed to elucidate their genetic and molecular basis. In this protocol, we present NIRF lymphatic, small animal imaging5,6 using indocyanine green (ICG), a dye that has been used for 50 years in humans7, and a NIRF dye-labeled cyclic albumin binding domain (cABD-IRDye800) peptide that preferentially binds mouse and human albumin8. Approximately 5.5 times brighter than ICG, cABD-IRDye800 has a similar lymphatic clearance profile and can be injected in smaller doses than ICG to achieve sufficient NIRF signals for imaging8. Because both cABD-IRDye800 and ICG bind to albumin in the interstitial space8, they both may depict active protein transport into and within the lymphatics. Intradermal (ID) injections (5-50 μl) of ICG (645 μM) or cABD-IRDye800 (200 μM) in saline are administered to the dorsal aspect of each hind paw and/or the left and right side of the base of the tail of an isoflurane-anesthetized mouse. The resulting dye concentration in the animal is 83-1,250 μg/kg for ICG or 113-1,700 μg/kg for cABD-IRDye800. Immediately following injections, functional lymphatic imaging is conducted for up to 1 hr using a customized, small animal NIRF imaging system. Whole animal spatial resolution can depict fluorescent lymphatic vessels of 100 microns or less, and images of structures up to 3 cm in depth can be acquired9. Images are acquired using V++ software and analyzed using ImageJ or MATLAB software. During analysis, consecutive regions of interest (ROIs) encompassing the entire vessel diameter are drawn along a given lymph vessel. The dimensions for each ROI are kept constant for a given vessel and NIRF intensity is measured for each ROI to quantitatively assess “packets” of lymph moving through vessels.
Protocol
All animal studies were performed in accordance with the standards of the University of Texas Health Science Center (Houston, TX), Department of Comparative Medicine, and Center for Molecular Imaging after review and approval of the protocol by their respective Institutional Animal Care and Use Committee (IACUC) or Animal Welfare Committee (AWC).
1. Preparation of Animals 24 Hr Prior to Imaging
The steps below must be done (as needed) the day before lymphatic imaging takes place.
- Place animal in an induction box and sedate with isoflurane.
- Once the animal is in a state of profound anesthesia (monitored with toe-pinch maneuver), place sedated animal on a diaper/fluff pad and position nose in a nose cone connected to isoflurane gas.
- Clip all hair/fur (if any) around the area to be imaged.
- Apply depilatory agent (NAIR) to the clipped area and leave it on the skin for up to 3 min.
- Gently wipe off all depilatory agent with warm, damp gauze or paper towel.
- Gently rinse the skin with warm water and gently dry the area with gauze or paper towel.
- Allow animals to recover on a heating pad or under a heat lamp, and return to their cage.
2. Day of Imaging
- Reconstitute imaging agent with sterile water, then dilute using sterile, normal (0.85%) saline to achieve 645 μM (5 μg/10 μl) for ICG or 200 μM (6.8 μg/10 μl) for cABD-IRDye800. Keep solutions in dark conditions and use within 6 hr of reconstitution.
- Place animal in an induction box and sedate with isoflurane.
- Once the animal is in a state of profound anesthesia (monitored with toe-pinch maneuver), place sedated animal on its side on a diaper/fluff pad and position nose in a nose cone connected to gas isoflurane.
- Turn off the lights (so the room is dark). If needed, a small desk halogen light can be used for a small amount of light to see injections.
- Using an insulin syringe with a 31-gauge needle, inject ID 5 μl to 50 μl of ICG or cABD-IRDye800 in the dorsal aspect of each hind paw and/or on the left and right side of the base of the tail, depending on the area of interest (see Discussion). Each injected dose may range from 0.083 to 1.25 mg/kg (ICG) or 0.113 to 1.7 mg/kg (cABD-IRDye800). Injection volumes will vary with animal strain and injection site. For athymic mice, the volume of injection can be 5 μl (hind paw) or 10 μl (base of tail). If animal is not under the imaging system for the injection(s), place the animal under the imaging system immediately after the injection(s).
- If no dye uptake is seen in the lymphatics, step 2.5 will need to be repeated as needed per animal protocol.
- Once lymphatics are seen, cover the injection site with black electrical tape or black paper.
- Acquire lymphatic images for up to 1 hr using V++ software and a small animal, NIRF imaging system. (Animals are sedated with isoflurane and respirations are monitored while images are acquiring.) While small animal, NIRF imagers are commercially available, we utilize a customized, small animal NIRF imaging system consisting of a 785-nm laser diode (1005-9mm-78503, Intense, North Brunswick, NJ) outfitted with an aspheric lens (C24TME-B, Thorlabs, Newton, NJ), diffuser (ED1-C20, Thorlabs), and filter (LD01-785/10-25, Semrock, Rochester, NY) to create a uniform excitation field that illuminates the animal at an incident fluence rate of less than 1.4 mW per square centimeter10. An electron multiplying charged-coupled device (EMCCD, PhotonMax512, Princeton Instruments, Trenton, NJ) camera system with two 830-nm filters (AND11333, Andover Corp., Salem, NH) and a 28-mm Nikkor lens (1992, Nikon, Melville, NY) is used to capture lymphatic images with integration times of 200 msec for dynamic imaging and 800 msec for static imaging5. See Figure 1 for system configuration, the Table for additional details of each component, and the Discussion for a brief discussion of key imager properties.
- Allow animals to recover on a heating pad or under a heat lamp and return to their cage, or euthanize.
- Analyze images using ImageJ or MATLAB software. See Figure 6.
Representative Results
Example of NIRF Lymphatic Imaging in Mice
When ICG or cABD-IRDye800 is injected ID at the base of the tail of a normal mouse, the lymphatic vasculature between the injection site at the base of the tail and the inguinal lymph node (LN) should be immediately visualized. Shortly after injection (a few seconds to minutes), the lymphatic vessel between the inguinal LN and the axillary LN should be visualized as seen in Figure 2. Since the lymphatics in mice vary from animal to animal as they do in humans, variation in architecture between animals may be seen as shown in Figure 3. When ICG or NIRF-cABD is injected ID on the dorsal aspect of the hind paw of a normal mouse, two lymphatic vessels can be visualized draining to the popliteal LN as shown in Figure 4. In some cases, it is difficult to distinguish both vessels because of their close proximity with each other.
Precautions for NIRF Lymphatic Imaging Impacted
At times, visualization of the lymphatics is delayed, most commonly due to the injection being administered subcutaneously (SC) instead of ID. When SC injections are given, lymphatic transport may not be immediately visualized as seen in Figure 5(a) because of the additional time required for the dye to reach and be taken up by the lymphatic capillaries in the skin. This is why it is important to inject ID instead of SC. On occasion, abnormal lymphatic vessels are observed, as seen in Figure 5(b), in the area of a wound such as a bite or cut from the hair/fur clippers. The animal’s body temperature should be maintained within normal range, as changing body temperature can result in inconsistent lymphatic function. Limitations of the technique include obscuration of fluorescent lymphatic vessels by skin pigmentation, the inability to image the deep thoracic lymphatic ducts due to light scattering in the tissue, and the unknown effect of anesthesia on lymphatic function.
Generally, it takes the ID depot of ICG or cABD-IRDye800 up to 2 days to clear the liver and bladder, and up to 3 days to clear the injection site. When residual fluorescent signal has cleared, the imaging protocol can be repeated, allowing longitudinal lymphatic imaging to evaluate changes in architecture or lymph function after some intervention.
Analysis of Lymphatic Function
The acquired images can be loaded into ImageJ or MATLAB for data analysis. Constant-area, circular ROIs are selected or “drawn” along the entire length of the fluorescent lymphatic vessel as done for human10 and animal5 lymphatic imaging as shown in Figures 6(a) and Figure 6(d). The ROIs are selected such that their diameter is approximately the diameter of the image of the fluorescent vessel. The mean fluorescence intensity within each ROI is plotted as a function of imaging time to assess the propulsive velocity and the frequency of “packets” of dye-laden lymph propelled along the lymphatic vessels as shown in Figures 6(b) and Figure 6(e). To assess the lymphatic propagation velocity and frequency of lymphatic propulsion, two ROI’s, with clearly defined maxima or minima fluorescent intensity variations representing the propagation of packets of lymph, are selected and their fluorescent intensity profiles are plotted as shown in Figures 6(c) and 6(f). The propagation velocity is computed by taking the ratio of the distance between the two ROI’s and the transit time for a packet of lymph to propagate between them. By assessing the number of fluorescent pulses or “packets” arriving at a single ROI per time, the contractile frequency is computed. While this technique provides the only method to assess propulsion frequency and velocity of a propelled lymphatic “packet,” others have indirectly evaluated lymphatic transport by measuring the depot clearance of an imaging agent and thus calculating removal rate constants11. In cancer metastases10 and early infection, we find loss of lymphatic propulsion in animals. Others report changes in contractility in response to arthritis12. In humans, we report increased propulsion following lymphedema treatments including pneumatic compression drainage13 and manual lymphatic drainage (massage)14.
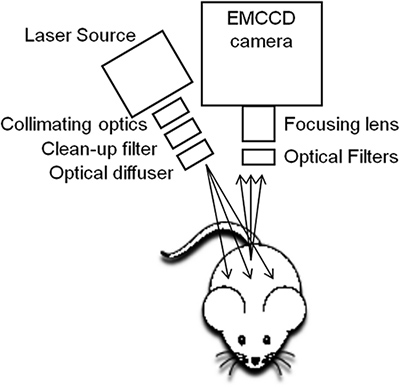
Figure 1. The NIRF imaging system is custom-built for small animal lymphatic imaging. The device consists of a 785-nm laser diode outfitted with an aspheric lens, diffuser, and filters to create a uniform excitation field that illuminates the animal and an EMCCD camera, focusing lens, and optical filters to capture images of fluorescent lymph10.
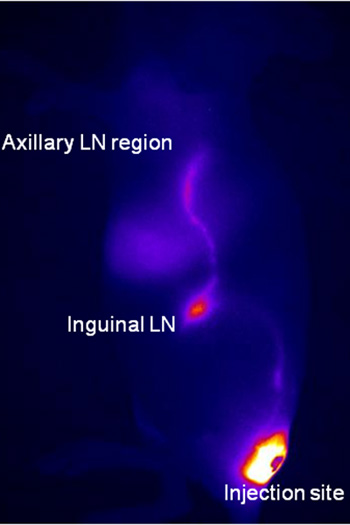
Figure 2. When 10 μl of ICG or cABD-IRDye800 is injected ID at the base of the tail of a normal mouse using a 31-gauge needle, the lymphatic vasculature between the injection site at the base of the tail and the inguinal lymph LN should be immediately visualized. Dynamic fluorescence images are acquired immediately after injection and for up to 20 min following injection. Shortly after injection (a few seconds to minutes), lymphatic vessels between the injection site and the inguinal LN and subsequently to the axillary LN region are visualized on the lateral view. The image shown in Figure 2 was taken 5 min. after injection with 10 μl of ICG ID at the base of the tail. The bright spot between the inguinal and axillary regions is the liver.
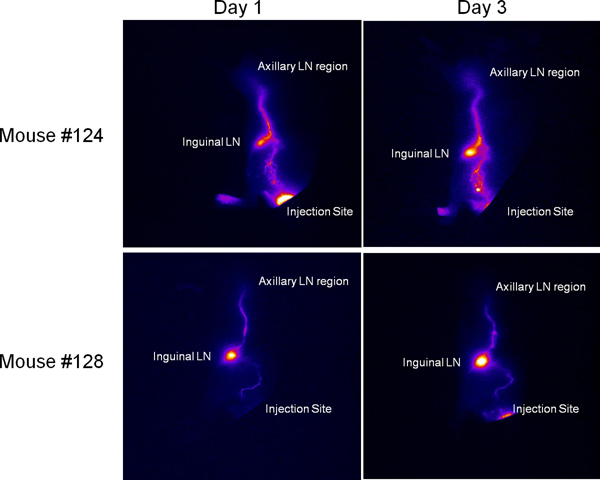
Figure 3. Since the lymphatics in mice vary from animal to animal as they do in humans, variation in architecture between animals may be seen and is stable over time. Mouse #124 was injected with ICG at the base of the tail and imaged immediately on day 1. The top panel contains the image obtained at day 1 as well as an image obtained 2 days later (on day 3) using the same mouse and injection/imaging protocol. The bottom panel contains images obtained from another mouse (#127) injected with ICG and immediately imaged day 1 and subsequently imaged on day 3. While the lymphatic architecture (the pattern of lymphatic vessels) varies between mouse #124 and #127, the images obtained using NIRF are consistent for each mouse on days 1 and 3.
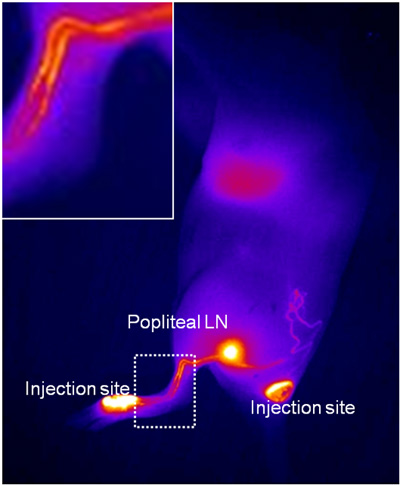
Figure 4. When 5-10 μl of ICG or NIRF-cABD is injected ID on the dorsal aspect of the hind paw of a normal mouse, two lymphatic vessels should be visualized draining to the popliteal LN. Dynamic fluorescence images are acquired immediately after injection and for up to 20 min following injection. In some cases it is difficult to distinguish both vessels because of their proximity as illustrated in the enlarged image represented by the dashed box. For the representative mouse shown here, 10 μl of ICG was injected in the dorsal aspect of the left, hind paw (first injection site) and in the left side of the tail base (second injection site). This image was captured approximately 2 – 3 min after the first injection and approximately 30 sec – 1 min following the second injection.
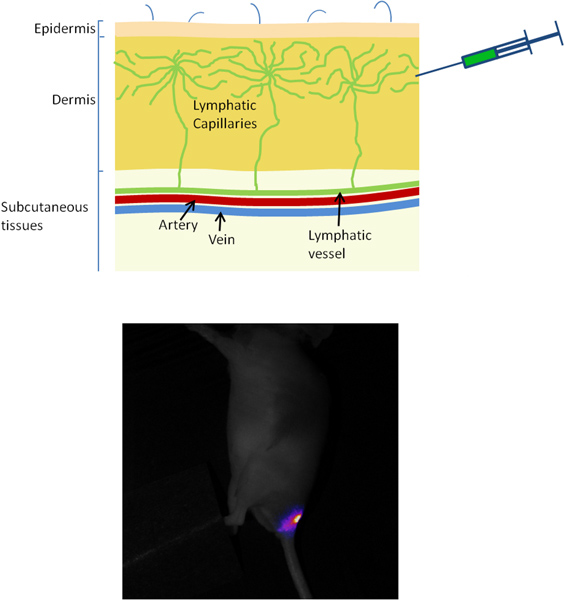
Figure 5. (a) Occasionally visualization of the lymphatics is delayed or impaired, most commonly due to the injection being administered SC instead of ID. When 10 μl of ICG or cABD-IRDye800 is injected SC at the base of the tail of a normal mouse using a 31-gauge needle, lymphatic transport will not be immediately visualized because of the additional time required for the dye to reach and be taken up by the lymphatic capillaries in the skin. Also, due to the relatively deep SC injection, there may be no lymphatic uptake and therefore no visualization of the vessels and lymph nodes. In Figure 5(a), a mouse was injected with 10 μl of ICG at the base of the tail SC and images were acquired 5 min after injection. The dye at the injection site can be visualized and no lymphatic vessels or lymph nodes can be visualized. This is the reason ID injections are important. (b) Visualization from animal’s ventral side of aberrant lymphatic vessels resulting from a wound encountered one day earlier during fur removal with clippers (tissue injury site noted on animal’s right side). The image was captured approximately 5 min after 10 μl of ICG was administered ID at the base of the tail on each the left and right side. On the non-injured (animal’s left) side, the inguinal LN can be visualized as well as the relatively straight efferent lymph vessel draining up toward the axillary LNs. On the mouse’s right side, however, normal lymph vasculature was interrupted due to wounding and appears aberrant due to tissue repair (scabbing).
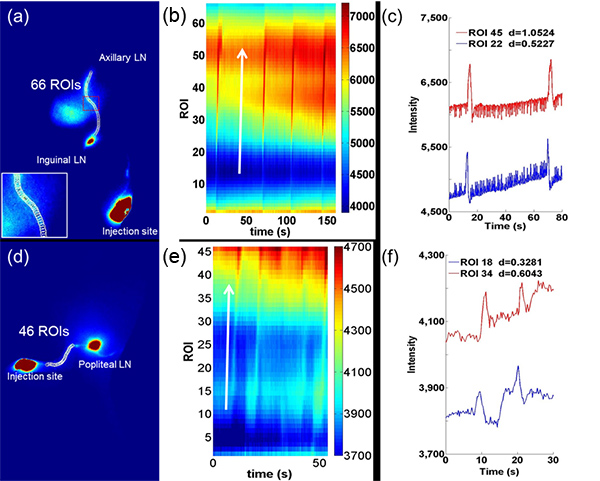
Figure 6. Quantitative analysis of lymphatic contractile function consists of selecting ROIs along the lymphatic vessels draining from (a) the inguinal LN to the axillary LN and (d) the injection site on the dorsal aspect of the paw to the popliteal LN. A magnified image (inset in (a)) of the red dashed rectangle illustrates the selection of ROIs along the fluorescent vessel. A compilation of average fluorescence intensity as a function of time for all ROIs from (a) and (d) is represented by the pseudo-color plot shown in (b) and (e), respectively. The perturbations in fluorescence intensity across pixels represent a lymphatic “pulse” propagating through the ROIs and are parallel to the arrows. The average fluorescence intensity for single ROIs 22 and 45 from (b) are shown in (c) and the average fluorescence intensity for single ROIs 18 and 34 from (e) are shown in (f). Fluorescence intensity profiles as a function of time (as shown in (c) and (f)) facilitate the identification of packets of propagating lymph and the extraction of the transit time and distance between two ROIs. The two ROIs are selected based in part on their location along the lymphatic vessel and the clarity with which the maxima and minima representing lymph propagation are shown. Velocity is computed as the ratio of the distance between two ROIs and the transit time that is taken between peak fluorescence intensity. Click here to view larger figure
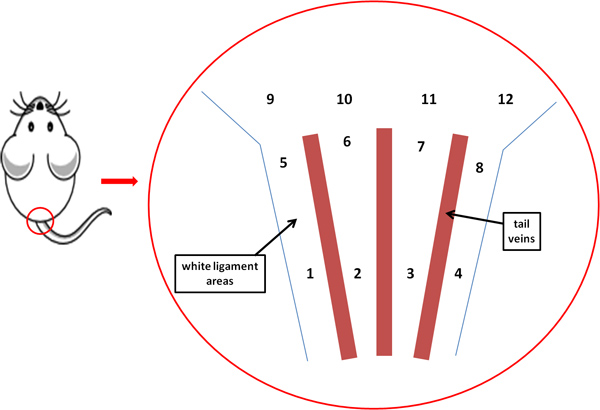
Figure 7. To visualize the lymphatics draining from the inguinal region to the axillary region, inject the left or right side of the base of the tail. In general, to visualize the left side, inject in location 5, 6, 9, or 10; and to visualize the right side, inject in location 7, 8, 11, or 12. Locations 1 through 4 may be too inferior on the tail for optimum uptake to visualize lymphatic drainage from the inguinal region to the axillary region.
Discussion
We use a custom, small animal NIRF imaging system to capture images of labeled lymph vessels in mice. To construct movies of lymph movement, 300 or more images are collected. For functional analysis of lymphatics from movies, two or more ROIs are manually drawn along a lymph vessel. The dimensions of the ROIs are kept constant for each vessel and are approximately the diameter of the vessel. While whole animal spatial resolution can depict fluorescent lymphatic vessels of 100 microns or less, a macrolens for finer resolution images can be employed10. White-light images for anatomical reference can also be acquired using a low-power lamp. It should be noted that if imaging agents are comprised of other fluorescent dyes with different excitation/fluorescence emission spectra, then the filters described above must be altered to maintain imaging performance, and agent dosage may need adjusting as well. Also, if the excitation wavelength is less than 750 nm, then autofluorescence may result, background signal will increase, and imaging sensitivity will decrease. In addition, instability of agents in solution may preclude the use of some NIRF dyes, such as Cyanine 7 (Cy7).
Selection of the appropriate injection site will depend on which lymphatic vessels are being studied. To visualize the lymphatics draining from the inguinal region to the axillary region, you will need to inject the left or right side of the base of the tail, as shown in Figure 7. To visualize the lymphatics draining from the palatial region, you will need to inject the dorsal aspect of the hind paw. It is essential to keep the animal’s body temperature within normal range, as changing body temperature can result in inconsistent lymphatic function. In addition, because of the limited dynamic range of most CCDs, the injection sites should be covered with black paper to block fluorescent light thereby enabling visualization of dimmer draining lymphatic vessels. Imaging should be performed in a dark room to reduce unwanted background signals due to emission of light in the fluorescence band from the room lights. The animal must also be lying on a black background while imaging is being performed to reduce the light backscatter.
NIRF lymphatic imaging may enable a better understanding of lymphatic diseases and how lymphatic architecture and function changes with respect to disease or injury. For example, the research team has used NIRF imaging in small animals to provide lymphatic phenotyping of animals6,15 and to detect changes in lymphatic function and architecture with cancer metastases10. In humans, the technique has been used to detect early signs of lymphedema2, assess response to lymphedema therapy13,14,16 , and phenotype family members with hereditary lymphatic disorders. However, non-invasive visualization of deep lymphatics (>3 cm) in humans is limited by the scatter of light in tissue. Images of lymphatic structures up to 3 cm in depth have been acquired in swine9 and human imaging. In humans, MRI and dynamic lymphoscintigraphy have been used to quantify the transit time of contrast agent from the injection site to the lymph nodes in disease. However, they lack sufficient temporal and spatial resolution to visualize the lymphatic propulsion events readily imaged with NIRF. In addition, healthy lymphatics are not visualized with MRI owing to lack of contrast. NIRF imaging is non-invasive, unlike confocal, multiphoton microscopy, and intravital imaging. Typically confocal and multiphoton microscopy techniques utilize partially or totally resected tissue. Scintographic methods necessitate the use of radionuclides and sometimes minor vessel cannulation. Another method to visualize the lymphatics involves intravital imaging during which the mouse is euthanized and the dermis is pulled back following ID injection of Evans blue dye. However, this method does not provide functional or longitudinal imaging17,18 . LN metastases can be imaged using a Siemens Inveon PET/CT; however, this technique does not allow visualization of lymphatic structure or function19.
While the authors do not recommend nor endorse any specific commercial imaging device, our experience indicates that the choice of light source and optical filters may be the single most important factor which determines the sensitivity of the device. As described by Zhu et al., for successful imaging of low concentrations of dye, there must be minimal overlap between the emission spectrum of light source and the transmission spectrum of the optical filters20. Another key consideration is the absorption and emission spectrum of the NIRF dye used. In this paper ICG and cABD-IRDye800 have similar spectra and so the described laser diode wavelength and filter combinations can be used for each; however, if another dye is to be used which does not absorb and/or fluoresce at these wavelengths, the wavelength of the light source and the optical filters should be adjusted accordingly. ICG can be sufficient for many applications, and is already FDA-approved. NIRF-cABD is not FDA-approved for use in humans, but may be useful for animal imaging. ICG does not have chemical linking residues for attaching targeting moieties, so other fluorescent agents, such as NIRF-cABD, are being developed.
Disclosures
The authors have nothing to disclose.
Acknowledgements
This work was supported by the following grants to Eva Sevick: NIH R01 CA128919 and NIH R01 HL092923.
Materials
| Solutions, Reagents, and Equipment | Company | Catalog Number | Comments |
| Indocyanine green (ICG) | Patheon Italia S.P.A. | NDC 25431-424-02 | Reconstitute to 645 μM (5 μg/10 μL) |
| Cyclic Albumin Binding Domain(cABD) | Bachem | Custom | Reconstitute to 200 μM (6.8 μg/10 μL) |
| IRDye800 | Li-COR | IRDye 800CW | Reconstitute according to manufacture’s instructions; conjugate with cABD at equilmolar concentrations |
| Sterile Water | Hospira, Inc., Lake Forest, IL | NDC 0409-4887-10 | |
| NAIR | Church & Dwight Co., Inc. | Local Stores | www.nairlikeneverbefore.com |
| Imaging System (components below) | Center for Molecular Imaging | N/A | Custom-built in our laboratories. |
| Electron-multiplying charge-coupled device (EMCCD) camera | Princeton Instruments, Trenton, NJ | Photon Max 512 | |
| Nikon camera lens | Nikon Inc., Melville, NY | Model No. 1992, Nikkor 28mm | |
| Optical filter | Andover Corp., Salem,NH | ANDV11333 | Two 830.0/10.0 nm bandpass filters are used in front of lens |
| 785-nm laser diode | Intense Ltd, North Brunswick, NJ | 1005-9MM-78503 | 500 mW of optical output |
| Collimating optics | Thorlabs, Newton, NJ | C240TME-B | Collimates laser output prior to cleanup filter |
| Clean-up filter | Semrock, Inc., Rochester, NY | LD01-785/10-25 | Removes laser emission in fluorescence band |
| Optical diffuser | Thorlabs, Newton, NJ | ED1-C20 | Diffuses the laser over the animal |
| V++ | Digital Optics, Browns Bay, Auckland, New Zealand | Version 5.0 | Software used to control camera system and save images to computer. http://digitaloptics.net/ |
| Analytic Software Either of the following software packages can be used for image analysis | |||
| ImageJ | National Institutes of Health, Bethesda, MD | Most current version available | Freeware available at http://rsbweb.nih.gov/ij/ |
| MATLAB | MathWorks, Natick, MA | Version 2008a or later | http://www.mathworks.com/ |
References
- Alitalo, K. The lymphatic vasculature in disease. Nat. Med. 17, 1371-1380 (2011).
- Rasmussen, J. C., Tan, I. C., Marshall, M. V., Fife, C. E., Sevick-Muraca, E. M. Lymphatic imaging in humans with near-infrared fluorescence. Curr. Opin. Biotechnol. 20, 74-82 (2009).
- Rasmussen, J. C., et al. Human Lymphatic Architecture and Dynamic Transport Imaged Using Near-infrared Fluorescence. Transl. Oncol. 3, 362-372 (2010).
- Sevick-Muraca, E. M. Translation of near-infrared fluorescence imaging technologies: emerging clinical applications. Annu. Rev. Med. 63, 217-231 (2012).
- Kwon, S., Sevick-Muraca, E. M. Noninvasive quantitative imaging of lymph function in mice. Lymphat. Res. Biol. 5, 219-231 (2007).
- Kwon, S., Sevick-Muraca, E. M. Mouse phenotyping with near-infrared fluorescence lymphatic imaging. Biomed Opt Express. 2, 1403-1411 (2011).
- Marshall, M. V., et al. Near-infrared fluorescence imaging in humans with indocyanine green: a review and update. The Open Surgical Oncology Journal. 2, 12-25 (2010).
- Davies-Venn, C. A., et al. Albumin-Binding Domain Conjugate for Near-Infrared Fluorescence Lymphatic Imaging. Mol. Imaging Biol. , (2011).
- Sharma, R. Quantitative imaging of lymph function. Am. J. Physiol. Heart Circ. Physiol. 292, 3109-3118 (2007).
- Kwon, S., Sevick-Muraca, E. M. Functional lymphatic imaging in tumor-bearing mice. J. Immunol. Methods. 360, 167-172 (2010).
- Karlsen, T. V., McCormack, E., Mujic, M., Tenstad, O., Wiig, H. Minimally invasive quantification of lymph flow in mice and rats by imaging depot clearance of near-infrared albumin. Am. J. Physiol. Heart Circ. Physiol. 302, 391-401 (2012).
- Zhou, Q., Wood, R., Schwarz, E. M., Wang, Y. J., Xing, L. Near-infrared lymphatic imaging demonstrates the dynamics of lymph flow and lymphangiogenesis during the acute versus chronic phases of arthritis in mice. Arthritis Rheum. 62, 1881-1889 (2010).
- Adams, K. E., et al. Direct evidence of lymphatic function improvement after advanced pneumatic compression device treatment of lymphedema. Biomed. Opt. Express. 1, 114-125 (2010).
- Tan, I. C., et al. Assessment of lymphatic contractile function after manual lymphatic drainage using near-infrared fluorescence imaging. Arch. Phys. Med. Rehabil. 92, 756-764 (2011).
- Lapinski, P. E., et al. RASA1 maintains the lymphatic vasculature in a quiescent functional state in mice. J. Clin. Invest. 122, 733-747 (2012).
- Maus, E. A., et al. Near-infrared fluorescence imaging of lymphatics in head and neck lymphedema. Head Neck. 34, 448-453 (2012).
- Galanzha, E. I., Tuchin, V. V., Zharov, V. P. Advances in small animal mesentery models for in vivo flow cytometry, dynamic microscopy, and drug screening. World J. Gastroenterol. 13, 192-218 (2007).
- Schramm, R., et al. The cervical lymph node preparation: a novel approach to study lymphocyte homing by intravital microscopy. Inflammation research : official journal of the European Histamine Research Society. 55, 160-167 (2006).
- Hall, M. A., et al. Imaging prostate cancer lymph node metastases with a multimodality contrast agent. Prostate. 72, 129-146 (2012).
- Zhu, B., Sevick-Muraca, E. M. Minimizing excitation leakage and maximizing measurement sensitivity for molecular imaging with near-infrared fluorescence. J. Innovat. Opt. Health Sci. 4, 301-307 (2011).

