Preparation and Pathogen Inactivation of Double Dose Buffy Coat Platelet Products using the INTERCEPT Blood System
Summary
This article describes the process used by Örebro University Hospital to produce double dose buffy coat platelet concentrates prepared from whole blood donations and treated with the INTERCEPT Blood System for pathogen inactivation. The in vitro quality of the final platelet units are evaluated over 7 days of storage.
Abstract
Blood centers are faced with many challenges including maximizing production yield from the blood product donations they receive as well as ensuring the highest possible level of safety for transfusion patients, including protection from transfusion transmitted diseases. This must be accomplished in a fiscally responsible manner which minimizes operating expenses including consumables, equipment, waste, and personnel costs, among others.
Several methods are available to produce platelet concentrates for transfusion. One of the most common is the buffy coat method in which a single therapeutic platelet unit (≥ 2.0 x1011 platelets per unit or per local regulations) is prepared by pooling the buffy coat layer from up to six whole blood donations. A procedure for producing “double dose” whole blood derived platelets has only recently been developed.
Presented here is a novel method for preparing double dose whole blood derived platelet concentrates from pools of 7 buffy coats and subsequently treating the double dose units with the INTERCEPT Blood System for pathogen inactivation. INTERCEPT was developed to inactivate viruses, bacteria, parasites, and contaminating donor white cells which may be present in donated blood. Pairing INTERCEPT with the double dose buffy coat method by utilizing the INTERCEPT Processing Set with Dual Storage Containers (the “DS set”), allows blood centers to treat each of their double dose units in a single pathogen inactivation processing set, thereby maximizing patient safety while minimizing costs. The double dose buffy coat method requires fewer buffy coats and reduces the use of consumables by up to 50% (e.g. pooling sets, filter sets, platelet additive solution, and sterile connection wafers) compared to preparation and treatment of single dose buffy coat platelet units. Other cost savings include less waste, less equipment maintenance, lower power requirements, reduced personnel time, and lower collection cost compared to the apheresis technique.
Protocol
1. Whole Blood Collection
- Collect whole blood from volunteer donors in 450 ml top/bottom collection sets according to local blood collection guidelines.
- The whole blood is stored for a minimum of 2 hr on a cooling plate before centrifugation and separation.
2. Buffy Coat Preparation
- Centrifuge the whole blood using a hard spin to separate the blood into three layers: red blood cells, buffy coat, and plasma. Centrifuge parameters used were 4,880 RCF for 11 min at 22±2 °C.
- Use an automated blood separator to express the plasma into the top satellite bag and the red blood cells (RBC) into the bottom satellite bag, leaving the buffy coat in the collection container. Target mean volume and hematocrit ranges for buffy coats are approximately 48 ml and 37%, respectively.
- The buffy-coats are stored overnight on a platelet agitator at 22±2 °C.
3. Buffy Coat Pooling
- Sterile connect 7 buffy coats and 300 ml of SSP+ platelet additive solution (PAS) in a train configuration with parallel lines to reduce the train length; the PAS should be at the top of the train. Clamp the line between the PAS and the first buffy coat.
- Open the sterile connections between the buffy coat units and allow the buffy coats to drain into the last container.
- Open the weld and the clamp between the PAS and the first buffy coat. Allow one-third of the additive solution to rinse through each of the buffy coat containers sequentially. Repeat 2 more times each time using one-half of the remaining PAS.
- The average buffy coat pool volume should be approximately 600 ml. If the target volume and hematocrit of the individual buffy coats are met, the plasma ratio will be 32 – 47% as required for the INTERCEPT pathogen inactivation treatment later in the process.
- Discard the empty SSP+ and buffy coat containers.
- For optimal platelet recovery, keep the pool on the agitator for 1 hr prior to centrifugation.
- Sterile connect a platelet storage container with integrated leukoreduction filter to the buffy coat pool.
- Perform a “soft spin” of the buffy coat pool to separate the red blood cells from the platelets in suspension (462 RCF for 9 min, 20 sec). Express the platelet suspension using an automated blood separator through the leukoreduction filter into the platelet storage container.
- The previously described processing requirements ensure that the platelet suspension meets the INTERCEPT processing specifications of 300 ml – 420 ml volume, 2.5-7.0 x 1011 platelet dose, and ≤ 4 x 106/ml red cells.
4. INTERCEPT Treatment
- Perform the INTERCEPT treatment before the end of Day 1 after collection (day 0 is the day of collection).
- Unwrap the INTERCEPT Processing Set with Dual Storage Containers from the clear plastic pouch.
- Sterile connect the platelet suspension container to the tubing of the amotosalen container on the INTERCEPT processing set.
- Label the INTERCEPT processing set storage containers with the appropriate blood product identification following local requirements.
- Hang the platelets and break first the bottom cannula on the amotosalen container, allowing the amotosalen solution to flow into the illumination container. Break the top cannula on the amotosalen container allowing the platelets to flow through the amotosalen container into the illumination container.
- Gently mix the platelet and amotosalen mixture and express the air from the illumination container into the amotosalen container.
- Express a small amount of the platelet mixture into the tubing, filling about 4 cm of the tubing. This ensures platelets in both the tubing and illumination container undergo the pathogen inactivation treatment.
- Seal the tubing between the illumination container and amotosalen container. Leave no more than approximately 4 cm of tubing extending from the illumination container. Remove and discard the empty platelet and amotosalen containers and close the clamps on the sampling pouches.
- Place the processing set into the illuminator with the illumination container in the large compartment on the left and the organizer in the smaller compartment on the right side.
- Use the hand-held barcode device to enter the donation ID, product code, and processing set lot number into the illuminator. Close the metal cover and when prompted on the illuminator graphical interface, close the drawer. Press “Start” to start the Illumination.
- After illumination, remove the processing set from the illuminator. The illuminator automatically prints the treatment report for the treated platelet unit(s).
- Unwrap the containers from the organizer and hang the platelets and processing set, break the cannula at the outlet of the illumination container, and allow the platelets to flow into the compound adsorption device (CAD) container.
- Taking care not to bend the CAD wafer, express the air from the CAD container into the illumination container using a plasma extractor.
- Seal the tubing near to the inlet port of the CAD container. Remove and discard the empty illumination container.
- Place the CAD container with the attached storage containers on a platelet agitator for at least 6 hr, but no more than 16 hr. This will result in reduction of residual amotosalen to a concentration of ≤ 2 μM.
- After CAD treatment, remove the platelet units from the agitator. Hang the platelets. Break the cannula and allow platelets to flow into the storage containers.
- Express the air from the storage containers into the CAD container. Let the residual platelet concentrate flow back into the storage containers by gravity. Seal the tubing above the Y-fitting and remove the empty CAD container.
- Redistribute the volume between the storage containers as needed. Volume adjustments are made by weighing the storage containers. Seal the tubing to each storage container a few centimeters above the inlet of the storage container; this facilitates obtaining a sterile sample from the final product as described in 5.2.
5. Product Sampling
- For routine QC testing, the final storage containers can be sampled once by using the sampling pouch on the storage containers. To do so, ensure the platelet unit is well mixed, then open the clamp to the pouch and squeeze several times. Seal the tubing after the pouch has filled with platelets. Transfer the platelet sample into an appropriate laboratory tube and perform assays immediately.
- To obtain samples at multiple time points over the course of storage, such as for a validation study, sterile connect a new sampling container to the tubing of the platelet storage container. Ensure that platelets are well mixed prior to transfer to the sampling container.
6. In vitro Function Evaluation
- For this validation study, in vitro evaluation was performed after CAD treatment (Day 1 or Day 2, depending on CAD duration) and again on Day 4 (or Day 5) and Day 7. In vitro measurements included volume, platelet count, pH, blood gas (pO2, pCO2), glucose, lactate, and swirling.
- Volume was determined by weight using 1.01 g/ml as the specific gravity of platelets in additive solution.
- Hemoglobin contamination was evaluated visually using comparison to a color chart.
- Swirling was determined visually.
- See “Table of equipment” for methodology of other assays.
7. Representative Results
The process of producing double dose buffy coat platelets begins with the production of individual buffy coats which meet target specifications for volume and hematocrit. As it is not practical to measure the hematocrit of the individual buffy coats during the final process validation, we began by undertaking a separate effort to optimize our buffy coats to ensure we could consistently meet target volume and hematocrit. As shown in Table 1, our optimized buffy coats compared favorably to the target values for both volume and hematocrit at 46 ± 2 ml and 37 ± 3%, respectively.
After pooling, the volume and hematocrit of the buffy coat pool should be approximately 600 ml and 20%, respectively, prior to the soft spin centrifugation. As illustrated in Table 2, our buffy coat pools averaged 615 ± 5 ml; the hematocrit averaged 19 ± 1%.
The soft spin centrifugation results in a double dose platelet concentrate that will meet the input requirements for pathogen inactivation utilizing the INTERCEPT Blood System DS processing set. Key input parameters for INTERCEPT treatment include volume, platelet count, plasma ratio, and RBC content. In addition, we aim to recover ≥ 75% of the platelets in the platelet concentrate as compared to the buffy coat pool. Per local requirements, the white blood cell (WBC) contamination must be <1×106/unit. The platelet concentrates in our validation met the key parameters for INTERCEPT treatment as well as the targets for WBC contamination and platelet recovery as shown in Table 3.
The INTERCEPT process for pathogen inactivation is performed on the double dose platelet concentrate using a single INTERCEPT processing set. The processing set contains two integral storage containers which allow the treated unit to be split into two individual therapeutic platelet doses at the completion of the pathogen inactivation process. European guidelines require that 75% of units tested contain ≥ 200×109 platelets per therapeutic dose1; local requirements in Sweden require that 75% of the units tested contain >240×109 platelets per dose. After INTERCEPT treatment, the average platelet content was 265 ± 22 x109 (n=24). Furthermore, 88% of units met or exceeded 240×109 platelets per therapeutic dose; this is well within both the European guidelines and Swedish regulations. See Figures 1 & 2 for an illustration of the double dose buffy coat preparation and INTERCEPT treatment processes respectively.
For this validation, we measured the in vitro characteristics of the platelet concentrates after INTERCEPT treatment (i.e. after the split into the individual storage containers); parameters were measured over 7 days of storage. Mean and standard deviation were collected for platelet dose, pH, pO2, pCO2, lactate production and glucose consumption.
Figure 3 shows the mean starting platelet dose of the double dose platelet concentrate before INTERCEPT treatment and the mean platelet dose in each of the split products after INTERCEPT treatment over 7 days of storage. Platelet loss during storage was approximately 9%. This reduction is not different from the expected loss of platelets during storage of conventional platelets.2
Table 4 summarizes the in vitro characteristics of the INTERCEPT platelets after treatment and splitting into single units.
Per European requirements, the pH of platelets must remain above 6.4 through the end of shelf life. During processing, the pH of the platelet concentrates drops slightly based on the platelet concentration, volume, and the gas permeability of the platelet storage container. Figure 4 illustrates the pH of the split platelet products over 7 days of storage. During storage, the pH is stable and well maintained within the processing requirements.
As shown in Figures 5A and 5B, the platelet O2 consumption and the CO2 production indicate continued respiration by the INTERCEPT platelets in the PL2410 container during 7 days of storage. Figures 6A and 6B show the lactate and glucose levels over 7 days of storage. Platelet glucose consumption and lactate production are consistent with each other during the 7 days of storage. 5 units had glucose level less than 1.11 mmol/l (the lower limit for the glucose assay).
The buffy coat preparation and pooling validation produced platelet concentrates that met the input criteria for INTERCEPT treatment; specifically, volume, platelet count, plasma ratio, and red blood cell contamination. The final units met the validation criteria over 7 days of storage including platelet dose and pH.
| Parameter | Target Range | Results Mean ± SD |
| Volume (ml) | ~ 48 | 46 ± 2 |
| Hematocrit (%) | ~ 37 | 37 ± 3 |
| Hold time before pooling | Overnight on agitator | Overnight on agitator |
Table 1. Characteristics of the Individual Buffy Coats (n=19).
| Parameter | Target Range | Results Mean ± SD |
| Volume (ml) | ~ 600 | 615 ± 5 |
| Hematocrit (%) | ~ 20 | 19 ± 1 |
| Hold time before centrifugation | 1 hr on agitator | 1 hr on agitator |
Table 2. Characteristics of the Buffy Coat Pools (n=12).
| Parameter | Target | Results Mean ± SD |
| Volume (ml) | 370 – 420 | 404 ± 8 |
| Platelet count (x109/unit) | 250 – 700 | 577 ± 62 |
| Mean Platelet recovery (%) | ≥ 75 | 75 ± 4 |
| Plasma ratio (%) | 32 – 47 | 38 ± 1 |
| RBC (x106/ml) | ≤ 4 | 1.2 ± 0.4 |
| WBC (x106/unit) | ≤ 1 | 0.11 ± 0.1 |
| Hold time before INTERCEPT (hr) | ≤ end of day 1 | ≤ end of day 1 |
Table 3. Characteristics of the Double-Dose Platelet Concentrates (n=12).
| Mean ± SD | Min | Max | |
| Volume (ml) | 199 ± 16 | 182 | 236 |
| Platelet count (x109/unit) | 265 ± 22 | 225 | 292 |
| pH (22 °C) | 6.9 ± 0.1 | 6.8 | 7.0 |
| pO2 (kPa) | 21.4 ± 4.8 | 12.8 | 27.3 |
| pCO2 (kPa) | 4.3 ± 0.4 | 3.3 | 4.9 |
| Lactate (mmol/l) | 9.1 ± 1.7 | 6.8 | 12.4 |
| Glucose (mmol/l) | 5.3 ± 0.9 | 3.7 | 6.5 |
Table 4. Characteristics of the INTERCEPT Treated Platelets Day 1/2 (Single Units, n=24).
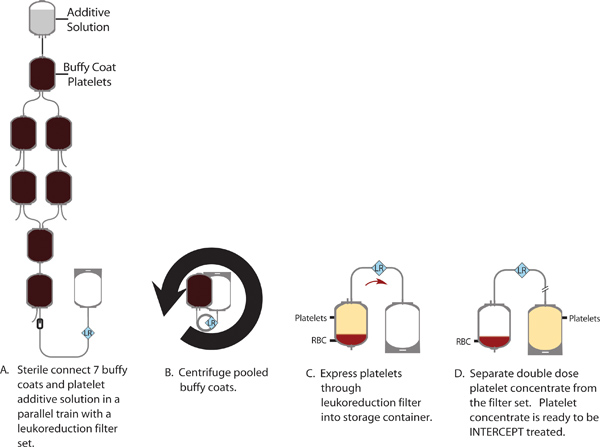
Figure 1. Production of a double dose platelet concentrate from a pool of 7 buffy coats.
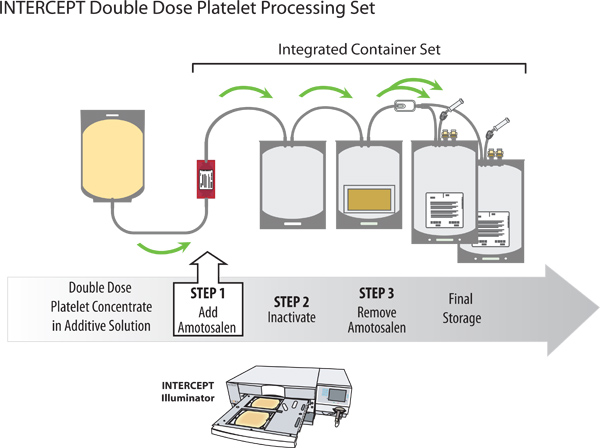
Figure 2. Pathogen inactivation of a double dose platelet concentrate with the INTERCEPT Blood System.
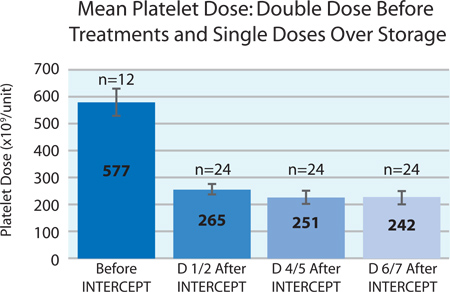
Figure 3. Mean platelet dose before and for 7 days after INTERCEPT treatment (n=12 before INTERCEPT; n=24 after INTERCEPT).
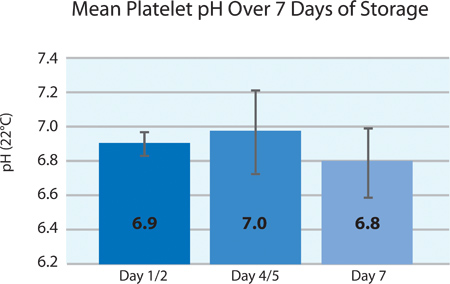
Figure 4. Mean platelet pH ±SD after INTERCEPT treatment (n=24).
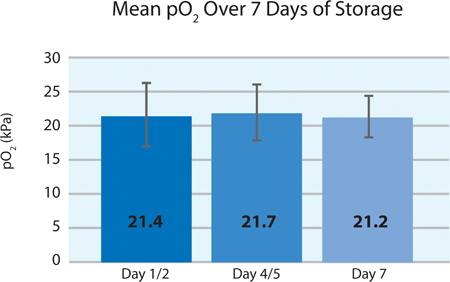
Figure 5A. Mean pO2 ±SD after INTERCEPT treatment (n=24).
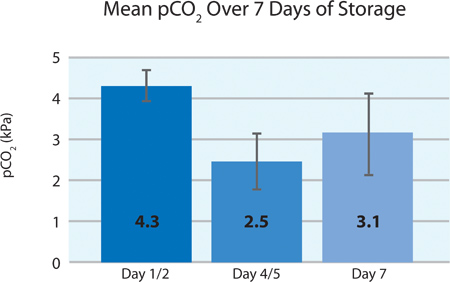
Figure 5B. Mean pO2 ±SD after INTERCEPT treatment (n=24).
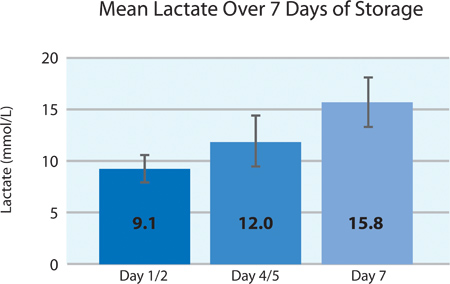
Figure 6A. Mean lactate levels ±SD after INTERCEPT treatment (n=24).
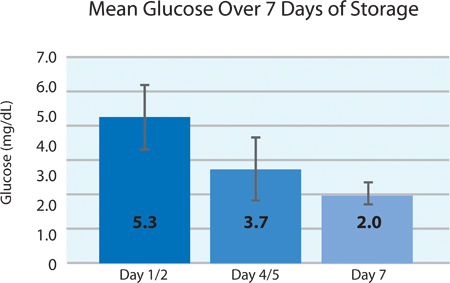
Figure 6B. Mean glucose levels ±SD after INTERCEPT treatment (n=24).
Discussion
Buffy coat platelets require several processing steps that result in post-collection costs, including personnel time, consumables, equipment, and waste, which must be factored into the overall cost of producing the platelet units. Improving the platelet yield from each buffy coat (via optimizing the buffy coat volume and hematocrit) allows the production of a double dose buffy coat platelet unit from a pool of seven buffy coats. When this optimization is performed, the number of buffy coats required to produce a fixed number of platelet doses may be reduced, thereby improving the overall utilization of buffy coats and enabling the production of additional platelet concentrates (PCs). Personnel time as well as consumable and equipment costs such as pooling sets, platelet additive solution, sterile connection wafers, filter sets, and centrifugation procedures are reduced by up to 50%. In addition to optimizing platelet production and reducing associated costs, this pooling method can generate a platelet concentrate (PC) that meets the input requirement for use with the INTERCEPT dual storage container processing set, allowing us to provide enhanced protection to our transfusion recipients as well.
The INTERCEPT Blood System for pathogen inactivation uses amotosalen and ultraviolet A (UVA) light to covalently cross-link DNA and RNA, preventing nucleic acid replication and rendering pathogens unable to cause disease.3 It effectively inactivates a broad spectrum of pathogens including viruses, bacteria, parasites, and contaminating donor white blood cells.4-6 INTERCEPT provides an alternative to the current testing paradigm for emerging pathogens, which historically involves a substantial delay while a new test is developed and ultimately requires a significant financial investment to implement when a test becomes available.7,8 It can also provide an alternative to redundant safety measures such as bacterial detection9 and gamma irradiation.10-12 In addition, INTERCEPT allows us to treat double dose platelet units which benefits our production efficiency and helps us adhere to our budgets.
INTERCEPT and the double dose buffy coat method can be adapted to a variety of blood center workflows. As examples, whole blood collections can be increased to 500 ml; collections could also be stored overnight at 22 °C prior to separation. In addition, an alternate buffy coat pooling method is possible (e.g. an octopus method instead of a train method) and/or an automated device (e.g. TACSI) can be utilized for the second centrifugation and separation of the platelet suspension from the remaining red cells.
If increased platelet content is needed, several techniques are available including pre-selection of donors based on platelet count, overnight incubation of the whole blood, adjustment of centrifugation settings, or utilizing a pool of 8 buffy coats in lieu of 7.
Due to the limitation of pooling sets currently available and the capacity of centrifuge buckets, the total volume of the buffy coat pool should be approximately 600 ml. The centrifugation process and settings described in this protocol have been optimized to yield product that meets the INTERCEPT parameters for a pool of 7 buffy coats. The centrifugation settings must be modified if the number of buffy coats in the pool is modified.
In some countries, the minimum platelet dose is higher and the QC requirements are more stringent than in Sweden. As such, our results may not be universally applicable. In these countries, the double dose PC prior to INTERCEPT treatment will need to contain a larger number of platelets in order to meet local requirements after INTERCEPT treatment and split. Because the maximum platelet content and treatment volume for INTERCEPT are 7×1011 platelets and 420 ml respectively, the percentage of units which exceed the INTERCEPT processing requirements or have insufficient platelet content to be split into two therapeutic doses, will vary depending on factors such as local requirements for platelet dose, QC criteria, buffy coat optimization results, and production stability.
If a double dose PC exceeds the INTERCEPT processing requirements, it may be manually adjusted to meet the requirements and subsequently treated. In those few occasions where the 7-buffy coat pool yields insufficient platelets for a double dose product after INTERCEPT, we elect not to perform the INTERCEPT treatment. Alternatively, other blood centers may choose to treat the PC with a single dose INTERCEPT processing set (i.e. the Large Volume set) and store the PC as a single larger therapeutic dose, thereby performing pathogen inactivation on all units. In order to ensure we meet our QC requirements and to pathogen inactivate as many of our platelet units as possible, we select buffy coats based on the donor platelet counts, which, when pooled, will result in a minimum platelet content of 5.6×1011 platelets in the pool. This ensures sufficient platelet content to produce two therapeutic doses after INTERCEPT treatment.
Our validation demonstrates that 7 whole blood derived buffy coat units can be successfully pooled and treated with the INTERCEPT process for platelets, resulting in 2 pathogen inactivated platelet products that meet the acceptance criteria for manufacturing (Swedish requirements and European guidelines) and for support of patients requiring platelet transfusions according to clinical practice guidelines and standard platelet infusion methods in Sweden.
Disclosures
The authors have nothing to disclose.
Acknowledgements
Funding for the publication is provided by Cerus Corp, manufacturer of the INTERCEPT Blood System.
Materials
| Material / Equipment | Company | Catalogue Number | Comments |
| Whole blood donation, primary separation, and platelet production | |||
| Blood collection pack | Fenwal | R6485 | Top/Bottom set |
| Automated component extractor | Fenwal | Optipress-II | |
| Blood mixer and balance system | Baxter | Easymix V3 | |
| Platelet leukocyte filtration set | Fenwal | K4R7042 | |
| Centrifuge | Hettich | Roto Silenta 63 RS | Version 5.5 |
| Platelet additive solution – SSP+ | MacoPharma | SSP2030U | 300 ml |
| Sterile tubing welder | Terumo | T-SCD | |
| INTERCEPT treatment & storage | |||
| INTERCEPT processing set | Cerus | INT2503 | Dual Storage (DS) set |
| INTERCEPT Illuminator | Cerus | INT100 | |
| PC sample pack | Fenwal | FTX 1122 | |
| Incubator | Helmer | PC2200/PC3200 | |
| Agitator | Helmer | PF48H/PF96H | |
| Evaluation of in vitro Platelet Function | |||
| Blood gas analyzer | Radiometer | ABL 735 | Used for pH, blood gases, and lactate measurement |
| Chemistry system | Ortho Clinical Diagnostic | Vitros 5.1 | Used for glucose measurement |
| Hematology analyzer | Boule Medical AB | Medonic CA620-Cellguard | Used for platelet count measurement |
| Flow cytometer | BD | FACSCanto | Used for white blood cell measurement |
References
- . . Guide to the preparation, use and quality assurance of blood components. , (2010).
- Van Rhenen, D. J., Vermeij, J., Mayaudon, V., et al. Functional characteristics of S-59 photochemically treated platelet concentrates derived from buffy coats. Vox Sang. 79, 206-214 (2000).
- Wollowitz, S. Targeting DNA and RNA in pathogens: mode of action of amotosalen HCl. Transfus. Med. Rev. 31, 11-16 (2004).
- Irsch, J., Lin, L. Pathogen Inactivation of Platelet and Plasma Blood Components for Transfusion Using the INTERCEPT Blood SystemTM. Transfus. Med. Hemother. 38, (2011).
- Lin, L., Dikeman, R., Molini, B., et al. Photochemical treatment of platelet concentrates with amotosalen and long-wavelength ultraviolet light inactivates a broad spectrum of pathogenic bacteria. Transfusion. 44, 1496-1504 (2004).
- Lin, L., Hanson, C., Alter, H., et al. Inactivation of viruses in platelet concentrates by photochemical treatment with amotosalen and long-wavelength ultraviolet light. Transfusion. 45, 580-590 (2005).
- Allain, J. P., Cianco, C., Blajchman, A., et al. Protecting the blood supply from emerging pathogens: the role of pathogen inactivation. Transfus. Med. Rev. 19, 110-126 (2005).
- Stramer, S., Hollinger, F., Katz, L., et al. Emerging infectious disease agents and their potential threat to transfusion safety. Transfusion. 49, 1S-29S (2009).
- Nussbaumer, W., Allesdorfer, D., Grabmer, C., et al. Prevention of transfusion of platelet components contaminated with low levels of bacteria: a comparison of bacteria culture and pathogen inactivation methods. Transfusion. 47, 1125-1133 (2007).
- Schlenke, P. Protection against Transfusion-Associated Graft-versus-Host Disease in Blood transfusion: Is Gamma-Irradiation the Only Answer? Transfus. Med. Hemother. 31, 24-31 (2004).
- Lin, L., Corash, L., Osselear, J. C. Protection Against TA-GVHD Due to Platelet Transfusion By Using Pathogen Inactivation with the INTERCEPT Blood SystemTM – Gamma Irradiation is Not the Only Answer. Haematologica. 95 (Extra 1), 230-237 (2010).
- Corash, L., Lin, L. Novel processes for inactivation of leukocytes to prevent transfusion-associated graft-verus-host disease. Bone Marrow Transplant. 33, 1-7 (2004).

