Investigation into Deep Breathing through Measurement of Ventilatory Parameters and Observation of Breathing Patterns
Summary
Here, we present a protocol to assess two deep breathing patterns of natural and diaphragmatic breathing for their effectiveness and ease of execution. Fifteen participants were selected, utilizing an electrocardiograph and expired gas analyzer for measurement of the ventilatory parameters, together with visual assessment by video capture of thoracoabdominal movement.
Abstract
In this protocol, two deep breathing patterns were shown to 15 participants to determine an easy yet effective method of breathing exercise for future application in a clinical setting. The women in their twenties were seated comfortably in a chair with back support. They were fitted with an airtight mask connected to a gas analyzer. Three electrodes were placed on the chest connected to a wireless transmitter for relaying to the electrocardiograph. They executed a 5 min rest phase, followed by 5 min of deep breathing with a natural breathing pattern, terminating with a 5 min rest phase. This was followed by a 10 min intermission before commencing the second instruction phase of substituting the natural breathing pattern with the diaphragmatic breathing pattern. Simultaneously, the following took place: a) continuous collection, measurement and analysis of the expired gas to assess the ventilatory parameters on a breath-by-breath basis; b) measurement of the heart rate by an electrocardiograph; and c) videotaping of the participant’s thoracoabdominal movement from a lateral aspect. From the video capture, the investigators carried out visual observation of the fast-forward motion-images followed by classification of the breathing patterns, confirming that the participants had carried out the method of deep breathing as instructed. The amount of oxygen uptake revealed that, during deep breathing, the work of breathing decreased. The results from the expired minute ventilation, respiration rate and tidal volume confirmed increased ventilatory efficiency for deep breathing with the natural breathing pattern compared to that with the diaphragmatic breathing pattern. This protocol suggests a suitable method of instruction for assessing deep breathing exercises on the basis of oxygen consumption, ventilatory parameters, and chest wall excursion.
Introduction
The cardiopulmonary physical therapist normally treats the patient according to the individual's needs and requirements. However, in general, the patient is left to carry out preoperative deep breathing exercise by him/herself. Therefore, it is imperative to find a simple and effective instruction method for the patient to carry out deep breathing exercises1.
Diaphragmatic breathing is such a breathing exercise and one method of breathing control2,3. The therapeutic outcome of this method includes a reduction in work of breathing and improvement in efficiency of breathing2,3, and this brings about an increase in tidal volume, resulting in a reduction in respiratory rate. However, some researchers have pointed out that diaphragmatic breathing exercise may cause asynchronous and paradoxical motion of the rib cage due to abdominal excursions in some patients4,5. In such cases, the use of a patient's natural breathing pattern may be efficacious. Regarding the question of deep breathing being effective as a means of a reduction in the mechanical work of breathing and improvement of ventilatory efficiency, it may be useful to quantify ventilatory parameters by the use of a gas analyzer.
It is well known that cardiopulmonary exercise testing is carried out using a gas analyzer6,7. Some investigators8,9 have reported measurement for diaphragmatic breathing with a gas analyzer in patients with chronic obstructive pulmonary disease. Jones et al.8 compared diaphragmatic breathing, pursed-lip breathing, and a combination of both, with that of spontaneous breathing. During these three methods of breathing, oxygen consumption (VO2) and respiratory rate (f) were measured, which showed that a higher resting VO2 may be explained by the increased mechanical work of breathing8. Ito et al.9 examined the immediate effect of diaphragmatic breathing or respiratory muscle stretch on VO2, f and tidal volume (VT). We may expect from the results of the aforementioned studies that similar evidence could be obtained by application of similar breathing exercises to confirm an effective deep breathing method of instruction.
This protocol describes the method for measurement of ventilatory parameters and chest wall excursion in deep breathing with two breathing patterns, together with their results and analysis. Continuous and quantitative sampling of ventilatory parameters can measure breathing precisely compared to alternative techniques. VO2 obtained in this protocol can be regarded as an indicator of work of breathing8. Further, f, VT, and minute ventilation are related to ventilatory efficiency. Information on breathing pattern can also be obtained from these ventilator parameters plus inspiratory and expiratory time. This protocol also involves assessment of chest wall excursion through video capture, which corresponds to observation by a physical therapist of the patient's chest wall excursion during breathing exercise. The overall goal of this study was to find a viable and efficient method of deep breathing exercise based on analysis of oxygen consumption, ventilatory parameters, and chest wall excursion.
Protocol
This protocol was in accordance with the ethical principles of the Declaration of Helsinki. The procedure was explained to all participants before commencement of the study.
1. Participant screening
- Recruit 15 healthy women in their twenties through convenience sampling. Check medical history verbally. Exclude participants with cardiopulmonary disease.
- Explain the procedure to the participant.
- Ask the participant to refrain from eating and drinking 2 h prior to the commencement of the measurement and to bring a tight-fitting black shirt.
2. Procedure
- Preparation for the procedure
- Calibrate the gas analyzer that has integrated components of a pneumotachograph and oxygen/carbon dioxide concentration meters 15 – 30 min before the measurement. Follow manufacturer's protocols.
- Attach a video camera to a tripod at a distance of 1.5 m from the chair the participant will sit on. Prepare to record a lateral view of the sitting participant in a range from the top of the cranium to the seat of the chair.
- Instruct the waiting participant to put on the tight-fitting black shirt in a cubicle, and when ready, stand by the side of the chair in the laboratory.
- Place three electrodes (positive, negative and ground) on the skin of the chest in standing, each with a wire to connect to a transmitter that relays to the electrocardiograph.
- Seat the participant comfortably for 5 min in a chair with a back support at an angle of 70° and, if necessary, insert a small cushion in the neck and/or lumbar region.
- Explain to the participant deep breathing with a natural breathing (NB) pattern of slow and deep breaths, breathing in through the nose and blowing out through the mouth with no consideration or knowledge given on specific movement of the chest.
- Ask the participant to take a natural deep breath without any guidance. Prepare to begin measurement if the investigator is satisfied with breathing performance. Observe the participant's thoracoabdominal movement during inspiration and expiration.
- Measurement of deep breathing with the NB pattern
- Fit the participant with a sampling mask over the mouth and nose for measurement of the expired gas. Perform a seal test: close the hole for the sampling tube of the mask with a finger and ask the participant to breathe out gently and confirm whether air leaks from the mask. Connect a sampling tube to the mask for measurement of the ventilatory parameters.
- Ask the participant to refrain from talking during the procedure.
- Instruct the participant to rest for 5 min, and simultaneously begin recording the expired gas and heart rate, together with video capture. After the 5 min rest phase, instruct the participant to begin deep breathing for 5 min with NB pattern. On termination, instruct the participant to rest for 5 min.
- Continue recording and measuring throughout the three phases.
- Perform only one three-phase trial for each participant.
- Rest phase
- Inform the participant that the experimenter will take off the mask and allow her a 10 min intermission phase.
- Instruct the participant that she may sit and talk in the laboratory, but not drink. Begin timing the intermission phase with a stopwatch at the moment of taking off the mask.
- Measurement of deep breathing with the diaphragmatic breathing (DB) pattern
- Seat the participant as in step 2.1.5.
- Explain to the participant deep breathing with a diaphragmatic breathing (DB) pattern. Ask the participant to lace her fingers, place them on her abdomen and take a deep breath in through the nose, expanding the abdomen under the hands and then blowing out through the mouth and gently retracting the abdomen.
- Instruct the participant to practice this deep breathing with the DB pattern until the investigator is satisfied. Observe that thoracoabdominal expansion takes place during inspiration followed by its contraction on expiration.
- Fit the participant with a sampling mask over the mouth and nose for measurement of the expired gas. Perform a seal test: close the hole for the sampling tube of the mask with a finger and ask the participant to breathe out gently and confirm whether air leaks from the mask. Connect a sampling tube to the mask for measurement of the ventilatory parameters.
- Ask the participant to refrain from talking during the measurement.
- Instruct the participant to rest for 5 min, and simultaneously begin recording the expired gas and heart rate, together with video capture. After the 5 min rest phase, instruct the participant to begin deep breathing for 5 min with the DB pattern. On termination, instruct the participant to rest for 5 min. Continue recording and measuring throughout the three phases.
- Take the mask off the participant following the 5 min rest phase.
- Ask the participant immediately which of the two deep breathing techniques was more comfortable. Record the participant’s response on a spreadsheet.
- Remove the electrodes, leads and transmitter from the participant and let her leave.
- Perform only one three-phase trial for each participant.
3. Measurement of the Ventilatory Parameters
- Sample the breath-by-breath expired gas using a gas analyzer (see Table of Materials and Figure 2).
- Measure the following ventilatory parameters: oxygen uptake (VO2), carbon dioxide output (VCO2), expired minute ventilation (VE), respiratory rate (f), tidal volume (VT), expiratory time (Te), and inspiratory time (Ti).
- Measure the heart rate using a medical telemetry sensor for the electrocardiograph (see Table of Materials and Figure 2), which is connected to the gas analyzer.
NOTE: The gas analyzer is operated using computer software provided by the manufacturer (Table of Materials).
- Collect the data for each 5 min phase of rest and deep breathing for NB and DB patterns. Save the data on the ventilatory parameters in CSV format using computer software (see Table of Materials and Figure 3,4).
- Collect mean data for each 5 min phase of this protocol. Average data for the optionally set phase is obtained on a breath-by-breath basis.
- Enter the data for each participant into the spreadsheet program (see Table of Materials and Figure 5) and determine the mean and standard deviation (SD) for the initial rest and deep breathing phases for NB and DB.
4. Assessment of the Breathing Pattern
- Record thoracoabdominal movement from a lateral view of the participant using a video camera (Table of Materials).
- Make sure that the background color is in sharp contrast to the participant’s silhouette.
- Record the video image at 1/30 s per frame, which is the standard speed for the video camera used.
- Upload the motion-images into a personal computer using video editing software 1 (Table of Materials).
- Observe 5 min video images of the deep breathing phases at double speed under visual assessment and classify the breathing patterns as upper costal, diaphragmatic or thoracoabdominal. Use video editing software 2 (Table of Materials).
NOTE: Video images are analyzed by a cardiopulmonary physical therapist (MY).
5. Participants’ preferred pattern for deep breathing
- Prepare a spreadsheet for the participant's response.
- Ask the participant which of the two deep breathing techniques is more comfortable following the measurement of the DB pattern.
- Fill in the spreadsheet with the participant's response.
- Be ready to listen to the participant if she wants to talk about the procedure. Do not include the participant’s comments in the analysis.
6. Statistical Analysis
NOTE: Perform statistical analysis using commercial computer software (Table of Materials), and then provide all the button clicks.
- Ventilatory parameters
- Do not analyze the 5 min rest phase following the two deep breathing phases in this protocol.
- Determine the mean and SD for the initial rest phases and deep breathing phases for each parameter.
- Employ two-way repeated-measures analysis of variance (2-way ANOVA) to evaluate the ventilatory parameters and heart rate for the initial rest phases and two deep breathing phases.
NOTE: Factor "instruction" includes two levels NB and DB, and factor "phase" has two levels rest phase and deep breathing phase. - Using the Bonferroni method, evaluate between each factor for parameter measurement, yielding significant interaction following 2-way ANOVA.
- Classification of breathing patterns exhibited by the participants including their preferred pattern for deep breathing.
- Categorize the number of participants according to their breathing pattern in upper costal, diaphragmatic or thoracoabdominal breathing.
- Compile from the spreadsheet the number of participants according to their preferred pattern of deep breathing.
Representative Results
The Ventilatory Parameters and Heart Rate
Based on the data (Figure 5), the NB and DB patterns were analyzed statistically (Figure 6 and Table 1). The f, VT and Te were found to have a significant interaction (p<0.05, respectively). A significant decrease in the f was found for both the NB and DB patterns during deep breathing compared to the initial rest phases (p<0.05, respectively), and, during deep breathing with the NB pattern, the f decreased to a greater extent compared to that for the DB pattern (Figure 6 and Table 1). The VT and Te revealed a significant increase during deep breathing compared to the initial rest phases for the NB and DB patterns, and, those for both deep breathing with the NB pattern were greater compared to those for the DB pattern (Figure 6). All of the parameters except VE and HR revealed main effect for the "phase" factor (Table 1).
A reduction in the work of breathing was reflected in a decrease in VO2, and, during deep breathing with the NB and DB patterns, the VO2 decreased with reduced work of breathing (Table 1). The improvement in ventilatory efficiency is reflected in an increase in VT and a decrease in f or VE. Deep breathing with the NB pattern was superior in ventilatory efficiency compared to that with the DB pattern. Generally, the relationship between VE and alveolar ventilation (VA) is calculated by the formula: VE= VT × f and VA = (VT– anatomic dead space) × f. Assuming that VE is a constant, a decreased respiratory rate and an increased VT indicate an improvement in VA. As VE yielded no significant interaction and main effect following 2-way ANOVA (Table 1), VE for deep breathing with both breathing patterns appeared to be equal. The respiratory rate during deep breathing with the NB pattern was significantly smaller compared to the DB pattern, but, for VT during deep breathing, it was significantly greater compared to that for the DB pattern (Figure 6 and Table 1). In other words, the alveolar ventilation or gas exchange during deep breathing with the NB pattern appears more efficient than for that during deep breathing with the DB pattern.
Breathing Patterns and Participants' Preference
Shown is the result of the visual assessment for thoracoabdominal movement during deep breathing with two methods of instructions (Table 2). For the NB pattern,The majority of the participants presented an upper costal or thoracoabdominal movement. During deep breathing with the DB pattern, all but one participant showed a thoracoabdominal or diaphragmatic movement. This result shows that the participants were able to carry out deep breathing as instructed. Thirteen out of the 15 participants expressed that they found the NB pattern easier to carry out than the DB pattern.
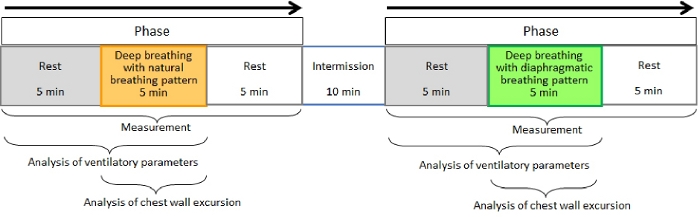
Figure 1. Flow chart for the protocol. Please click here to view a larger version of this figure.
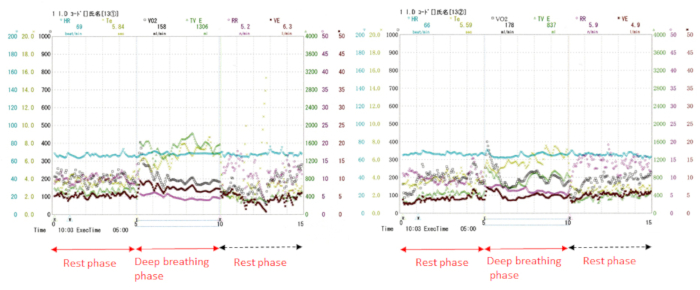
Figure 2. Ventilatory parameters as were seen displayed on the screen.
Left, Natural breathing pattern; Right, Diaphragmatic breathing pattern. Display shows a sample of individual data for each of the breath-by-breath samples for the ventilatory parameters and heart rate. Please click here to view a larger version of this figure.
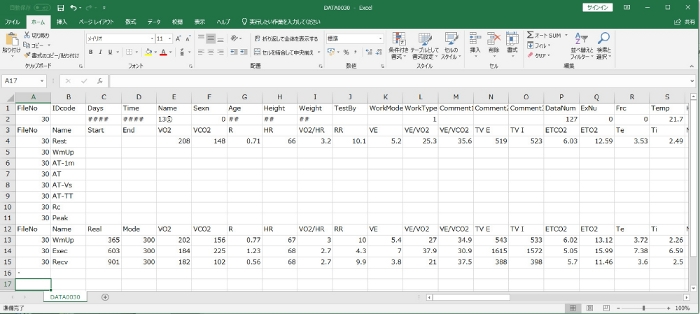
Figure 3. CSV format for ventilatory parameters during deep breathing with a natural breathing pattern.
The spreadsheet shows a sample of ventilatory parameters and heart rate following measurement. Please click here to view a larger version of this figure.
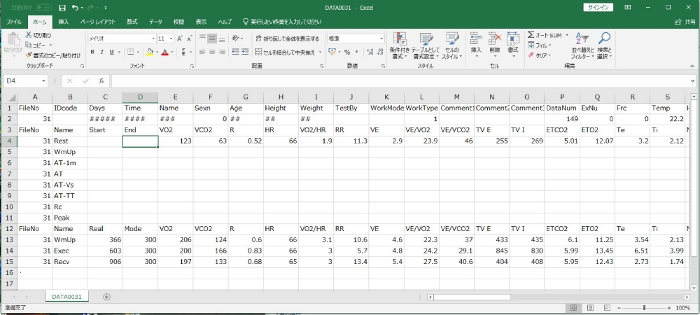
Figure 4. CSV format for ventilatory parameters during deep breathing with a diaphragmatic breathing pattern.
The spreadsheet shows a sample of ventilatory parameters and heart rate following measurement. Please click here to view a larger version of this figure.
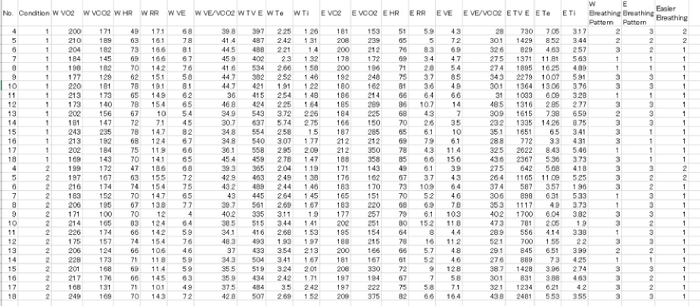
Figure 5. Raw data for all participants, which was converted from CSV data. Please click here to view a larger version of this figure.
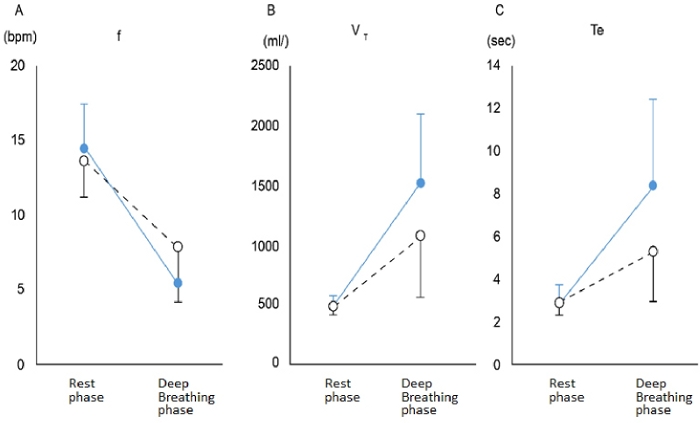
Figure 6. Significant interaction between ventilatory parameters.
Solid blue circle, deep breathing with natural breathing pattern; White circle, deep breathing with diaphragmatic breathing pattern. (A) shows the f, respiratory rate, (B) shows the VT, tidal volume, and (C) shows the Te, expiratory time. Please click here to view a larger version of this figure.
| Natural Breathing Pattern | Diaphragmatic Breathing Pattern | 2-way ANOVA | |||||
| Rest | Deep breathing | Rest | Deep breathing | Instruction | Phase | Interaction | |
| VO2 (L/min) | 0.20±0.02 | 0.19±0.01 | 0.20±0.02 | 0.19±0.01 | <0.01 | ||
| VCO2 (L/min) | 0.17±0.03 | 0.23±0.07 | 0.16±0.02 | 0.21±0.07 | <0.01 | ||
| VE (l/min) | 6.8±1.1 | 7.7±3.6 | 6.3±1.1 | 7.7±3.9 | |||
| f (/min) | 14.4±3.0 | 5.4±2.3* | 13.6±2.3 | 7.8±3.6†,§ | <0.01 | <0.05 | |
| VT (/ml) | 483±76 | 1507±579* | 464±61 | 1057±509†,§ | <0.05 | <0.01 | <0.05 |
| Te (s) | 2.79±0.92 | 8.37±4.00* | 2.82±0.53 | 5.25±2.31†,§ | <0.05 | <0.01 | <0.05 |
| Ti (s) | 1.63±0.43 | 4.51±1.70 | 1.69±0.33 | 3.67±1.08 | <0.01 | ||
| HR (bpm) | 69.1±7.6 | 71.7±8.9 | 68.5±7.6 | 70.1±8.5 | |||
Table 1. Comparison between the two breathing patterns. VO2, oxygen uptake; VCO2, carbon dioxide output; VE, minute ventilation; f, respiratory rate; VT, tidal volume; Te, expiratory time; Ti, inspiratory time; HR, heart rate; *, p<0.05 (Rest vs. Deep breathing during NB); †, p<0.05 (Rest vs. Deep breathing during DB); §, p<0.05 (NB vs. DB during Deep breathing). This table has been modified from one published in the Journal of Physical Therapy Science, 2018.
| Instruction | Upper costal | Thoracoabdominal | Diaphragmatic |
| Natural breathing pattern | 7 | 6 | 2 |
| Diaphragmatic breathing pattern | 1 | 8 | 6 |
Table 2. Result of the visual assessment for thoracoabdominal movement during deep breathing with two breathing patterns. This table has been modified from one published in the Journal of Physical Therapy Science, 2018.
Discussion
By the use of this protocol, effective instruction for deep breathing can be examined through oxygen consumption, ventilatory parameters, and chest wall excursion. The participants had a mean age of 21.6 years, mean body mass of 51.9 kg, mean height of 159.3 cm and a body mass index of 20.5 kg/m2. No incentives were offered to partake in this protocol. There are three critical steps within the protocol. First, concerning the control of food intake, the ratio of carbon dioxide output to oxygen uptake provides information about the nutrient mixture catabolized for energy10. Food intake in lower physical activity has a greater effect compared to higher physical activity on VO2 measured in expired gas11. The result for VO2 (Table 1) demonstrates a lower physical activity during deep breathing. Consequently, it is imperative to set conditions for food intake prior to measurement. Second, the participants are required to refrain from talking during measurement so as not to influence expired gas data. Third, to avoid possible learning effects of the DB pattern on the NB pattern, the execution of the breathing pattern sequence for the measurement is important (Figure 1).
In general, breathing exercise takes 3-5 min to execute. Therefore, the investigators allocated a 5 min deep breathing phase sandwiched between the two rest phases. The participants carried out only one trial for NB and DB deep breathing phase, for this protocol was designed to simulate initial instruction in a clinical setting of a 5-min breathing exercise. However, participants did not have an ideal diaphragmatic breathing pattern when carrying it out for the first time in this protocol (Table 2). Modification of this protocol may require further instruction time and practice for learning diaphragmatic breathing to compare the two breathing methods.
For the measurement of the expired gas on a breath-by-breath basis, the number of samples per min for the ventilatory parameters is equal to the respiratory rate per min. The number of samples per min is known to increase during vigorous physical activity, but that for the ventilatory parameters decreases during deep breathing as was shown in this protocol. Considering the above fact, the average time for data collection should be determined.
By the use of a video camera, it is possible for one investigator to carry out this protocol. In addition, a breathing pattern can be easily judged by fast-forwarding the motion-images. During the preliminary testing for this protocol, markers were placed on the sternum and abdomen, followed by videotaping. However, these markers were of no assistance for the visual judgment. Consequently, it was decided to have the participant wear a tight-fitting black shirt. Furthermore, it may be easier to observe the thoracoabdominal excursion if the color of the shirt is in contrast to that of the background. In this protocol, the wall’s background color is white beige in contrast to the black shirt. The investigators recommend the use of different protocol(s)12,13 if one intends to study breathing patterns particularly with attention to the kinematics of the thorax.
As for the sample size used this protocol, calculation by post-hoc power analysis14 yielded 0.75. To satisfy statistical power of 0.8 defined by Cohen14, a minimum sample size of 17 participants would have been required for this protocol, which meant that it had a shortage of two participants. Further, the distribution of pulmonary ventilation could not be assessed, as would have been possible with electrical impedance tomography15.
Ventilatory parameters obtained in this protocol include mechanism of intervention and energy cost in a systematic review of breathing control2. Alternative method for this procedure would be to analyze the ventilatory parameters in the rest phase following deep breathing, consequently determining the effect on ventilatory parameters immediately following deep breathing. Further, we could compare the ventilatory parameters pre- and post-deep breathing exercise. This may result in a change in the ventilatory parameters if participants become proficient in the two patterns of deep breathing. Henceforth, the investigators would like to explore how ventilatory parameters in the elderly and individuals in supine and/or side lying would differ from those in this study.
Disclosures
The authors have nothing to disclose.
Acknowledgements
The authors thank Dr. Shimpachiro Ogiwara, former Professor at the University of Kanazawa, and Mrs. Sandra M. Ogiwara, CSP (UK), BScPT (C), for English editing of the manuscript.
Materials
| Expired gas analyzer | Minato Medical Science, Osaka, Japan | AE-300S | |
| Expired gas analyzing software | Minato Medical Science, Osaka, Japan | AT for Windows | |
| Medical telemetry sensor for electrocardiograph | Nihon Kohden, Tokyo, Japan | BSM-2401 | |
| Spreadsheet program | Microsoft, https://www.microsoft.com/ja-jp | Excel | |
| SPSS Statistical Software | IBM, https://www.ibm.com/jp-ja/analytics/spss-statistics-software | Version 23.0 | |
| Video camera | Sony, Tokyo, Japan | DCR-SR 100 | |
| Video editing software 1 | Sony, Tokyo, Japan | PlayMemories Home | |
| Video editing software 2 | Adobe, https://www.adobe.com/jp/ | Premiere Elements 11 |
References
- Yokogawa, M., et al. Comparison of two instructions for deep breathing exercise: non-specific and diaphragmatic breathing. Journal of Physical Therapy Science. 30, 614-618 (2018).
- Lewis, L. K., Williams, M. T., Olds, T. Short-term effect on outcomes related to the mechanism of intervention and physiological outcomes but insufficient evidence of clinical benefits for breathing control: a systematic review. Australian Journal of Physiotherapy. 53, 219-227 (2007).
- Cahalin, L. P., Braga, M., Matsuo, Y., Hernandez, E. D. Efficacy of diaphragmatic breathing in persons with chronic obstructive pulmonary disease: A review of the literature. Journal of Cardiopulmonary Rehabilitation. 22, 7-21 (2002).
- Sackner, M. A., Gonzalez, H. F., Jenouri, G., Rodriguez, M. Effects of abdominal and thoracic breathing on breathing pattern components in normal subjects and in patients with chronic obstructive pulmonary disease. The American Review of Respiratory Disease. 130, 584-587 (1984).
- Gosselink, R. A., Wagenaar, R. C., Rijswijk, H., Sargeant, A. J., Decramer, M. L. Diaphragmatic breathing reduces efficiency of breathing in patients with chronic obstructive pulmonary disease. American Journal of Respiratory and Critical Care Medicine. 151, 1138-1142 (1995).
- Adachi, H. Cardiopulmonary Exercise Test. International Heart Journal. 58, 654-665 (2017).
- Guazzi, M., Bandera, F., Ozemek, C., Systrom, D., Arena, R. Cardiopulmonary Exercise Testing: What Is Its Value. Journal of the American College of Cardiology. 70, 1618-1636 (2017).
- Jones, A. Y., Dean, E., Chow, C. C. Comparison of the oxygen cost of breathing exercises and spontaneous breathing in patients with stable chronic obstructive pulmonary disease. Physical Therapy. 83, 424-431 (2003).
- Ito, M., Kakizaki, F., Tsuzura, Y., Yamada, M. Immediate effect of respiratory muscle stretch gymnastics and diaphragmatic breathing on respiratory pattern. Internal Medicine. 38, 126-132 (1999).
- Jansson, E. On the significance of the respiratory exchange ratio after different diets during exercise in man. Acta Physiologica Scandinavica. 114, 103-110 (1982).
- Yokogawa, M., et al. Effects of food intake on physiological responses to cardiopulmonary exercise testing. Journal of Physical Therapy Science. 19, 145-150 (2007).
- Romei, M., et al. Effects of gender and posture on thoraco-abdominal kinematics during quiet breathing in healthy adults. Respiratory Physiology & Neurobiology. 172, 184-191 (2010).
- Binazzi, B., et al. Breathing pattern and kinematics in normal subjects during speech, singing and loud whispering. Acta Physiologica. 186, 233-246 (2006).
- Faul, F., Erdfelder, E., Lang, A. -. G., Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Method. 39, 175-191 (2007).
- Reychler, G., et al. Incentive spirometry and positive expiratory pressure improve ventilation and recruitment in postoperative recovery: A randomized crossover study. Physiotherapy Theory and Practice. 35, 199-205 (2019).

