Quantifying Arms and Legs Contributions during Repetitive Electrically-Assisted Sit-To-Stand Exercise in Paraplegics: A Pilot Study
Summary
Arms contribution in Sit-To-Stand (SitTS) is determined by the legs’ muscle condition. Several compensating strategies were discovered in efforts to achieve complete SitTS cycles. These findings triangulate the spinal cord injury (SCI) persons’ biomechanical measures with their subjective feeling of load borne by both their limbs throughout the SitTS approaches.
Abstract
Execution of Sit-to-Stand (SitTS) in incomplete spinal cord injury (SCI) patients involves motor function in both upper and lower extremities. The use of arm support, in particular, is a significant assistive factor while executing SitTS movement in SCI population. In addition, the application of functional electrical stimulation (FES) onto quadriceps and gluteus maximus muscles is one of the prescribed management for incomplete SCI to improve muscle action for simple lower limb movements. However, the relative contribution of upper and lower extremities during SitTS has not been thoroughly investigated. Two motor incomplete SCI paraplegics performed repetitive SitTS to fatigue exercise challenge. Their performance was investigated as a mixed-method case-control study comparing SitTS with and without the assistance of FES. Three sets of SitTS tests were completed with 5-min resting period allocated in between sets, with mechanomyography (MMG) sensors attached over the rectus femoris muscles bilaterally. The exercise was separated into 2 sessions; Day 1 for voluntary SitTS and Day 2 for FES-assisted SitTS. Questionnaires were conducted after every session to gather the participants' input about their repetitive SitTS experience. The analysis confirmed that a SitTS cycle could be divided into three phases; Phase 1 (Preparation to stand), Phase 2 (Seat-off), and Phase 3 (Initiation of hip extension), which contributed to 23% ± 7%, 16% ± 4% and 61% ± 6% of the SitTS cycle, respectively. The contribution of arms and legs during SitTS movement varied in different participants based on their legs' Medical Research Council (MRC) muscle grade. In particular, the applied arm forces start to increase clearly when the leg forces start to decline during standing. This finding is supported by the significantly reduced MMG signal indicating leg muscle fatigue and their reported feeling of tiredness.
Introduction
Sit-To-Stand (SitTS) is a significant movement in a human's activity of daily living (ADL). It is also a prerequisite for basic functional activities such as standing, transferring, and walking. For patients with incomplete spinal cord injury (SCI), paraplegics in particular, SitTS exercise is a crucial activity for their functional independence1,2. This exercise is essential for independence training, which eventually helps SCI population to improve their quality of life. In order to perform a sufficient and adequate SitTS exercise, the knowledge regarding their biomechanics and muscle activity should be feasibly measurable during the training.
In a clinical rehabilitation program, SCI patients with grade American Spinal Cord Injury Association (ASIA) Impairment Scale, AIS C have a better progression and chance of recovering their motor function than those with grade AIS B, who has complete motor deficits. The SitTS performance plays an important measure in an SCI patient to indicate their motor functionality during the recovery process3. However, SCI AIS C patients require both support from the upper and lower limbs to achieve successful series of repeated SitTS movements. The upper limb support plays an important role in unloading the knees while providing adequate lifting forces and assuring the body balance during the exercise4.
The purpose of this study is to describe the biomechanical contributions of arms and legs throughout repetitive SitTS in incomplete SCI individuals. This study positions the biomechanical analysis in relation to the participants' subjective sense of their arms and legs muscle performance and feelings of 'effort and tiredness' throughout the SitTS exercise.
Many previous SitTS studies only concentrated on investigating the kinematics and kinetics aspects of the activity4,5,6,7. In a wider context of SitTS training, the development of this method which includes the instrumented standing frame (SF) and force plate analysis, could lead researchers to assess both upper and lower limb contribution of other populations such as stroke, elderly, and patients with osteoarthritis8,9,10. A previous study by Zoulias et al., instrumented custom-built hardware and software of SF presented a large frame design11. This method can be challenging to replicate. Hence this SitTS study highlighted a portable instrumented SF that can be adopted by other researchers with an existing motion analysis laboratory setup.
Protocol
The SitTS exercise and informed consent in this manuscript are described under ethical consideration by University of Malaya Medical Centre Ethics Committee (2017119-4828)12. Study procedures were explained in detail to each participant, and written informed consent was obtained before beginning the SitTS trial. This study was conducted as mixed-mode, where quantitative data were obtained using biomechanical analysis, whereas subjective scores were obtained from feedback sessions (of the participants) and audio recordings (of the researcher-participants interactions during the study). This pilot study compared the participant's contributions of arms and legs in SitTS exercise voluntarily versus their performance with the presence of FES.
1. Participants selection
- Perform an evaluation with potential SCI participants.
- Explain the details of the SitTS protocol, including the length of study (4 days) and length of session (SitTS: 2 h).
NOTE: Voluntary SitTS was conducted on Day 1, followed by rest for 2 days. Functional electrical stimulation (FES)-assisted SitTS is then continued on the next day and defined as Day 2. - Describe the medical requirements to the potential participant, including male or female with SCI AIS C (who can stand up), 18-60 years old, greater than 12-month post-injury, and demonstrate a willingness to wear specific clothes.
NOTE: SCI AIS C participants provided written, informed consent to volunteer in this study. Participant 1 was a male (45 years; Body Mass Index (BMI) 20.32 kg/m2) and Participant 2 was a female (49 years; BMI 33.54 kg/m2). Both of them presented 95 months and 33 months after the SCI injury, respectively. Both participants had their lower extremities (LE) muscle grade assessed. The LE muscle grade of Participant 1 were 2 (right side) and 4 (left side). Meanwhile, Participant 2 had LE muscle grade of 4 bilaterally12. Both participants had good trunk control. Participant 1 was diagnosed with a flaccid right leg with absent knee and ankle reflexes indicating a lower motor neuron injury. Besides that, his right leg was observed not to show any response to FES. - Describe the exclusion criteria to the potential participants, including medical conditions that would cause them to fail in completing the instructions during the study. Other exemption criteria include participants that have osteoporosis and bone fracture12, cardiac pacemaker or other implanted electronic system, had existing electrical stimulation device (implantable cardioverter defibrillator, pacemaker, or spinal stimulation) or had botulinum toxin.
- Explain the details of the SitTS protocol, including the length of study (4 days) and length of session (SitTS: 2 h).
2. SitTS experimental setup
NOTE: In this SitTS exercise, three parameters will be recorded. The first parameter is arms force and the second parameter is legs force. The third parameter is mechanomyography (MMG) which looks at the rectus femoris muscle activity.
- Chair and SF setup.
- Design an armless chair with a height of 45 cm13,14 without a backrest according to the dimension of force plate 1 embedded in the floor of the motion analysis laboratory (Figure 1).
- Place the chair on the top of the force plate 1.
- Instrument each SF leg independently with force sensor15 at the bottom of SF's leg given the sensitive range of each sensor is from 0-12 kg (Figure 2).
NOTE: The sum values of four force sensor readings from SF were referred to as the arms force contribution. - Position a portable and foldable SF in front of the chair within arm's reach12. Position four legs of the SF securely outside of force plate 2 to avoid double measurements (Figure 1).
- Motion analysis setup
- Enter participant's details (i.e., leg length, ankle width, knee width) in the motion analysis system.
- Place sixteen reflective markers on the participant's lower limbs with double-sided tape as mentioned in steps 2.2.3-2.2.5.
- Attach these markers directly over the bilateral anterior and posterior of the superior iliac spine. Second, attach markers on the lateral epicondyle of the left and right knee.
- Attach the marker over the lateral surface of the bilateral thigh and shank. Next, attach a marker on the lateral left and right malleolus.
- Attach markers over the left and right of the second metatarsal head. Attach the markers on the calcaneus at the same height of the second metatarsal head.
NOTE: The placement of reflective markers is based on the setup of the motion analysis system16.
- Participant's preparation
- Instruct the participant to be seated with their knees flexed at 90° with both feet positioned on force plate 2.
- Ensure the participant's head and trunk are faced forward while sitting in an upright position. Ensure the participant is barefooted.
- Place hands on the handle of the SF.
- Identify the rectus femoris muscle by palpating the middle and bulky area of the thigh.
- Place two MMG sensors at the thigh area of the rectus femoris muscle bilaterally, one MMG per leg, to accurately measure the leg muscles' sit-to-stand and stand-to-sit efforts12.
- Secure the sensors with a double-sided tape. Strap the MMG sensors around the thigh to reduce motion artefacts12.
- Connect the MMG sensors to the MMG device and the computer.
3. SitTS protocol
- Day 1: Perform voluntary SitTS exercise.
NOTE: Participants were instructed to do a repetitive SitTS event with the assistance of the SF.- Before the experiment starts, ensure to turn on all setups to record the selected parameters.
NOTE: The parameters recorded were force sensors for upper limb contribution, force plate for lower limb contribution, and MMG data for muscle rectus femoris activity. - Ask the participant to stand up from the stationary sitting position at the end of a countdown of 5 s timed by an electronic timer.
- Let the participant stand for 3 s and then sit back on the chair.
- Ask the participant to rest for 5 s.
NOTE: This was the resting interval in between the trials. - Continue to do SitTS trials (repeat steps 3.1.2 and 3.1.4 until the participant cannot perform the same routine any longer).
- Turn off all the recorded data.
- Then, ask the participant to rest for 5 min before continuing the next set of the SitTS routine. Give 5 min break in between sets to provide muscle recovery amongst sets17.
- Repeat steps 3.1.1-3.1.7 for another two sets.
- Allow the participant to rest for at least 48 h.
- Before the experiment starts, ensure to turn on all setups to record the selected parameters.
- Day 2: Perform FES-assisted SitTS exercise.
NOTE: Participants were instructed to do repetitive SitTS events with the assistance of the SF and FES.- Place FES electrodes on quadriceps and gluteus maximus muscles18.
- For quadriceps muscle, place the first electrode horizontally about two finger widths above the knee. Position the second electrode horizontally about a palm width below the hip joint.
- For the gluteus maximus muscle, ask the participant to bend forward and place the first electrode vertically closest to the hip bone. Attach the second electrode vertically closest to the tail bone, side by side from the first electrode.
- Attach all FES electrodes to the FES device and connect them to the FES software in the computer.
- Set up the FES software by selecting the pulse width of 300 and the frequency of 35 Hz.
- Define the FES current intensity by asking the participant if they can tolerate the current given to achieve knee and hip extension7. Determine the FES current amplitude through a number of practices before starting the actual trial.
NOTE: Table 1 shows the FES current stimulated towards the participants' selected muscles during assisted FES SitTS session. - Before the experiment starts, ensure to turn on all setups to record the selected parameters.
- Ask the participant to stand up from the stationary sitting position at the end of a countdown of 5 s timed by an electronic timer. At the end of the countdown, switch on the FES.
- Let the participant stand for 3 s. Then switch off the FES and let the participant sit back on the chair.
- Ask the participant to rest for 5 s.
- Continue to do SitTS trials (repeat steps 3.2.7-3.2.10 until the participant cannot perform the same routine any longer).
- Turn off all the recorded data.
- Then, ask the participant to rest for 5 min before continuing the next set of the SitTS routine.
- Repeat steps 3.2.7-3.2.13 for another two sets.
4. Data acquisition and analysis
- Arm force contribution
- Extract all raw data of the force sensor to the workbook file in the computer for offline analysis.
- Leg force contribution
- Analyze raw data of the SitTS kinematic and kinetic in the motion analysis software. Extract the force plate data and knee angle data to the workbook file in the computer for offline analysis.
NOTE: Force plate data represent the leg force contribution
- Analyze raw data of the SitTS kinematic and kinetic in the motion analysis software. Extract the force plate data and knee angle data to the workbook file in the computer for offline analysis.
- MMG of rectus femoris muscle
- Extract and store raw MMG data of rectus femoris muscle using two acquisition units and a vibromyography software to the workbook file for offline analysis.
NOTE: The MMG signal were recorded by a vibromyography sensor at a sampling rate of 2 kHz. A finite impulse response band-pass filter between 20 Hz and 200 Hz was used to relay and transform the raw data of the MMG signal as recommended by the manufacturer for the muscle effort assessment19. For every trial, all data set were normalized and then synchronized as a complete cycle of SitTS exercise. An independent sample t-test was done to observe significant differences in mean time between voluntary and FES-assisted SItTS exercises.
- Extract and store raw MMG data of rectus femoris muscle using two acquisition units and a vibromyography software to the workbook file for offline analysis.
5. Feedback session
- Record audio during the feedback session (researcher-participant interactions).
- Ask four questions regarding the stability and fatigue experienced by the participants during the accomplishment of SitTS in Day 1 and Day 2.
NOTE: In this section, stability was interpreted by the participants as the highest balance in the SitTS event. The highest balance was achieved when they could hold on to the selected event longest. Meanwhile, fatigue was identified as their feeling of 'tiredness' that leads to their lowest performance retrieved during the SitTS exercise. - Collect and transcribe the audio.
Representative Results
A total of 399 and 463 SitTS trials were completed without and with FES assisted correspondingly. The trials that contributed to each set are tabulated in Table 2. The participants could perform more SitTS trials with the presence of electrical stimulation on their legs, i.e., FES. Overall, both participants managed to perform more SitTS trials with the aid of FES. This suggests that FES helps in stimulating participants' quadriceps to execute SitTS action in a prolonged period20. There were three phases of SitTS described in this study. Phase 1 began with the start of the movement and lasted when the buttocks left the seat. Phase 2 referred to the time when buttocks leave the seat up to the maximum hip flexion event. Phase 3 denoted from the beginning of hip extension and lasted until the end of the movement. Each phase contributed 23% ± 7% for Phase 1, 16% ± 4% for Phase 2, and 61% ± 6% for Phase 3 of the SitTS cycle, as illustrated in Figure 3. Three phases of SitTS were defined in this study following an earlier study by Kagaya et al. that had a similar protocol of exercise in which SCI participants used the aid of hand-assists21. Phase 1 displayed the highest standard deviation (SD) of its contribution with ±7% proving that participants recruit diverse strategies to initiate buttocks lift-up from the seat throughout the study.
Overall, the mean time of FES-SitTS cycle between the initial trial in each set was identified to be significantly shorter (t = 1.28 s) as compared to the final trials (t = 1.66 s) in each set (p < 0.0005), as shown in Table 3. This indicates slower standing-up movement, most likely due to muscle tiredness or fatigue, and the added effort to stabilize themselves during the standing-up movement. FES-evoked exercise caused participants to be more prone to fatigue towards the end of their SitTS action in each set. Meanwhile, a non-significant difference of mean time was observed during voluntary SitTS activity p = 0.571, which suggests that there are several strategies of SitTS accomplishment initiated by participants throughout the voluntary SitTS session. There were some factors that might contribute to these several strategies, which consumed diverse time allocation. Participants' feet placement22,23 and trunk control22 during the early phase of voluntary SitTS played a major contribution as there were a few times participants tended to lift one of the feet and sway their trunk from front to back24 first before they started leaving the chair. This is also associated with the previous study by Lee & Lee24 that investigated the forward-and-backward swaying in preparation to stand was affected by the height of the chair.
The presence of negative values at the leg% during the early to middle stage of SitTS (Figure 4A, Figure 5A, Figure 6A, and Figure 7A) were due to the calibration procedure of force plate 2 that was taken while participants' feet were in contact with these force plate. This initialized the stationary sitting force as zero, as their legs were lifted slightly when repositioning in preparation to stand, resulting in the force value appearing negative. Since both participants had the pattern of adjusting their feet position by lifting the leg during the early stage of SitTS, force plate 2 showed a negative magnitude of force which indicated the eliminated force that existed by the feet before the calibration process took place. The habit of adjusting their feet position before actually standing might be a common practice of biomechanical preparation among all, which needs to be considered in other standing-related exercises25. Similarly, Camargos et al. reported that patients need to adopt a spontaneous SitTS strategy which results in higher functional levels25. Additionally, normalized root mean square (RMS)-MMG exhibited a similar graph pattern throughout the study. The amplitude of RMS-MMG was correlated to quadriceps muscle contraction and its force production26. The highest peak amplitude of normalized RMS-MMG described that the quadriceps muscles produced the highest force in between Phase 1 and Phase 2 of SitTS cycle (Figure 4C, Figure 5C, Figure 6C, and Figure 7C ). These highest forces were generated by the participants to prepare their legs for early knee joint stabilization before its extension. In addition, quadriceps muscles were observed to produce greater muscle contraction during the late phase of SitTS to help the legs to stabilize the feet and legs for standing posture22,25.
Furthermore, muscle contraction at the right leg was significantly higher as compared to the left leg for both participants during voluntary SitTS action (p < 0.05). These voluntary SitTS allowed them to use all strength from their limbs, especially from their legs, to execute the SitTS action. Hence both participants were assumed to use more effort on the right leg during these actions. In addition, Participant 1 had contracture of the right quadriceps muscle, which resulted in continuous contraction, thereby generating constant muscle force throughout the experiment.
Meanwhile, Table 4 summarises the answers given by the participants regarding their experience in performing the SitTS exercise. The contribution of arms and legs during SitTS movement varied among the participants based on their MRC muscle strength grade. In this study, the lower limbs' muscle strength for each participant is accessible in step 1.1.2. Hence in this step, the SCI participants' arms and legs contributions are presented individually, as shown in Figure 4 to Figure 7.
Biomechanical contributions of arms versus legs
Overall, throughout the SitTS action in both sessions, Participant 1's arm percentage showed a higher contribution in total body weight percentage as compared to his leg percentage (Figure 4A and Figure 5A). This result occurred as Participant 1 completely utilized his strength in both arms and left legs to bring up his upper body for standing. Both arms were used to support the left leg in providing stability for the whole body. Therefore, he endured most of his body weight using the arms and SF during the accomplishment of SitTS. Participant 1 had several joint contractures in the right knee and right ankle of the leg. As a result, Participant 1 did not put his body weight onto the right leg during the exercise. By comparing the two sessions, a higher contribution of Participant 1's arm percentage was presented during FES SitTS. This result proposes that his arms were utilized to control a full right knee extension that was stimulated by FES. Even though the muscles were electrically-stimulated in Participant 1, his right knee could not provide full knee extension during the end phase of SitTS. This statement is validated as the right knee angle did not reach normal knee extension range of motion (0° to 5°) during late phase of SitTS, as shown in Figure 4B and Figure 5B.
For Participant 2, there were huge increases of leg percentage from Phase 2 to Phase 3 of SitTS in both sessions. In general, Participant 2 had a better score of MRC muscle grade for legs as compared to Participant 1. As a result, Participant 2's arms and legs contribution pattern changed drastically throughout the SitTS action. Towards the end of the SitTS cycle, Participant 2's legs contributed 79.5% (without FES) and 78.8% (with FES) of the load-bearing, proving that her legs provided good weight-bearing to support her whole body during standing. The results suggested that the arms play a minor role in assisting Participant 2 during SitTS study.
In contrast, by comparing 2 sessions (Figure 6A and Figure 7A), a higher contribution of leg% during the end phase of voluntary SitTS proposed that Participant 2 exerted more strength onto her legs to bear the full body weight. In addition, during the final set of voluntary SitTS, Participant 2 exhibited a smaller knee angle during the early stage of the movement (Figure 6B). This finding suggests that towards the final set of voluntary SitTS tasks, Participant 2 compensated her fatigued state by positioning a smaller knee angle that provided lesser pressure on the feet27. In addition, FES stimulation helped Participant 2 perform SitTS by giving less strength exertion to the legs at the force plate during the end phase of session 2.
Subjective feedback
Among the 3 phases, which included 5 events of SitTS (Figure 3), both participants reported that their arms were the most tired during Event B while their legs were most tired during Event C. These 2 events were closely related to each other as both events occurred at Phase 2 of the SitTS motion. During Event B, i.e., when the buttocks lift-up was initiated, Participant 1 was observed to increase arm strength to lift his upper body from the chair (Figure 4A and Figure 5A). Meanwhile for Participant 2, the maximum contribution of arms was detected during Event B for FES-assisted SitTS (Figure 7A). These coincided with the accomplishment of SitTS action that was continued with the preparation of legs to stand without falling during Event C as observed by the motion analysis system (Figure 4B, Figure 5B, Figure 6B, and Figure 7B). These assumptions were verified as both participants' knee angles started to decrease (knee started to extend). These ideas are supported by participants' opinions during the interview. Participant 2 selected Event A in both conditions as the most stable position. The answer given by Participant 2 was expected as she felt secure while sitting on the chair.
Conversely, without the help of FES, Participant 1 felt most stable during Event C. This result was due to the presence of arm strength that assisted him to carry his body weight upward. While with the aid of FES, Event E was chosen as the most stable as he agreed that FES had helped him to straighten both his knees and allowed him to stand up confidently. Besides that, Participant 1 experienced the least stable position at Event E during voluntary SitTS due to his weak right leg (Quadriceps MRC muscle grade: Grade 2). These statements were proven by his major arms contribution towards the end of SitTS phase, as illustrated biomechanically in Figure 4A and Figure 5A. Next, with the aid of FES, Participant 1 felt the least stable during Event B, as reflected in Figure 3. Even with the presence of FES, Participant 1 believed that these events were where the initial transition of his body moving from sitting to standing. Meanwhile, Participant 2 felt the least stable during Event C in both sessions. These corresponded with the arrangement of both legs and arms to stand without falling as observed by the motion analysis system and illustrated in Figure 6 and Figure 7. The verbal expression was biomechanically verified as Participant 2's knee started to fully extend (Figure 6B and Figure 7B).
In addition, the normalized RMS-MMG of the quadriceps muscle showed a peak value during Event C. This indicated his effort to straighten his body to increase the hip angle when standing. Additionally, during the final trial of FES assisted SitTS session (Figure 7C), both quadriceps muscles displayed a small constant normalized RMS-MMG value throughout SitTS phase as agreed by Participant 2, who already felt tired, which emphasized the point of using the upper body to straighten herself in the final few standing process. In addition, following the FES-assisted SitTS session, both participants were confident with the use of FES device. Overall, participants experienced positive outcomes during their exercise.
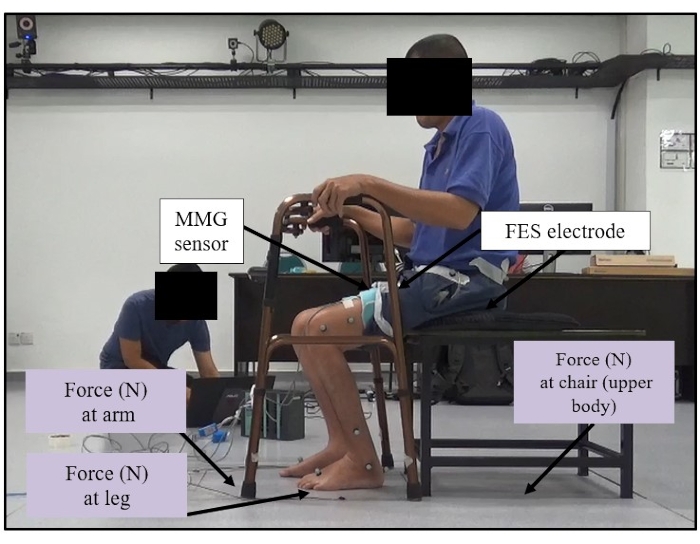
Figure 1: Custom-made chair setup. The custom-made chair was placed inside force plate 1. Both feet were placed on force plate 2. This figure shows the overall setup of the participant's initial position on the custom-made chair and instrumented SF with the force plates. Please click here to view a larger version of this figure.
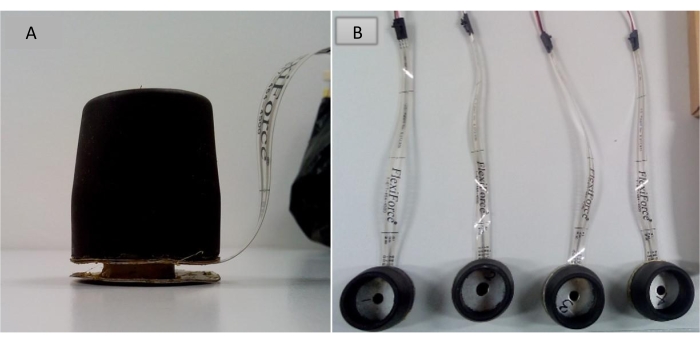
Figure 2: Placement of the force sensor. (A) An instrumented force sensor was placed at the bottom part of the rubber stopper of SF (side view). (B) The placement of four instrumented force sensors (top view). The figure presents the placement of the force sensor at the bottom part of the rubber stopper of the SF. Please click here to view a larger version of this figure.
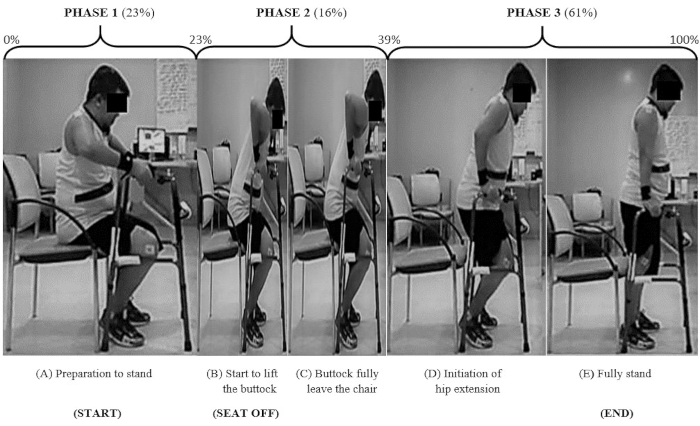
Figure 3: A cycle of SitTS activity assisted by SF. The figure describes a complete cycle of SitTS with the presence of a standing frame. Please click here to view a larger version of this figure.
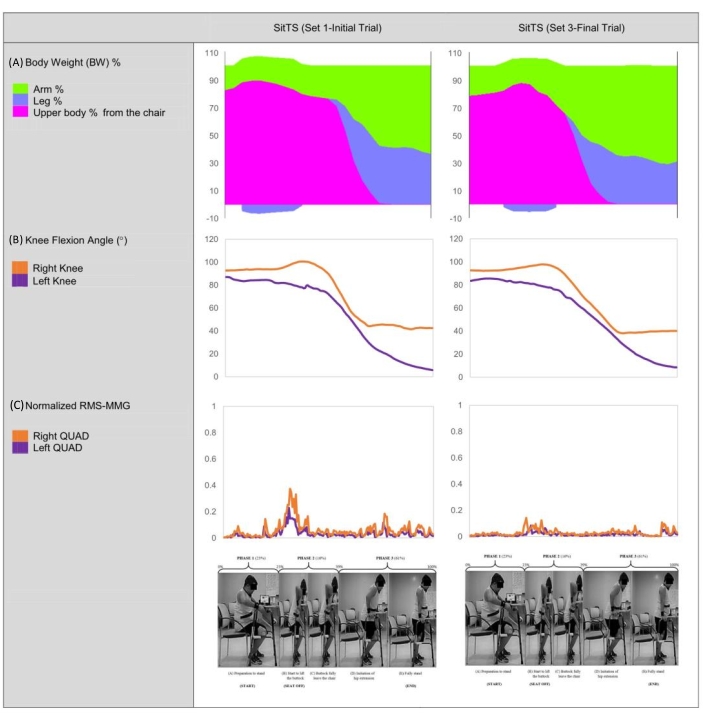
Figure 4: Participant 1's body weight contribution, knee flexion angle, and normalized quadriceps RMS-MMG during voluntary SitTS (Set 1-Initial Trial versus Set 3-Final Trial). The figure illustrates the parameters obtained by Participant 1 during the voluntary SitTS exercise. Please click here to view a larger version of this figure.
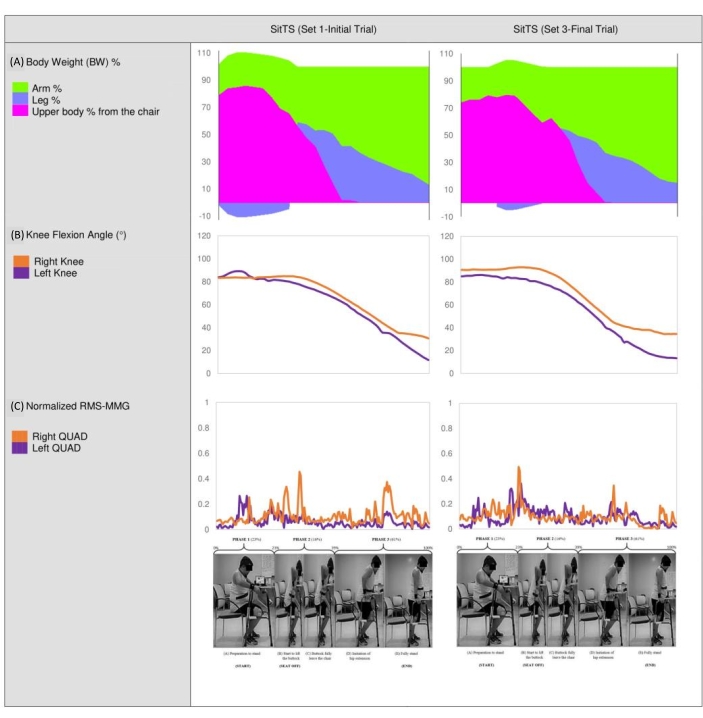
Figure 5: Participant 1's body weight contribution, knee flexion angle, and normalized quadriceps RMS-MMG during assisted FES SitTS (Set 1-Initial Trial versus Set 3-Final Trial). The figure explains the parameters obtained by Participant 1 during FES assisted SitTS exercise. Please click here to view a larger version of this figure.
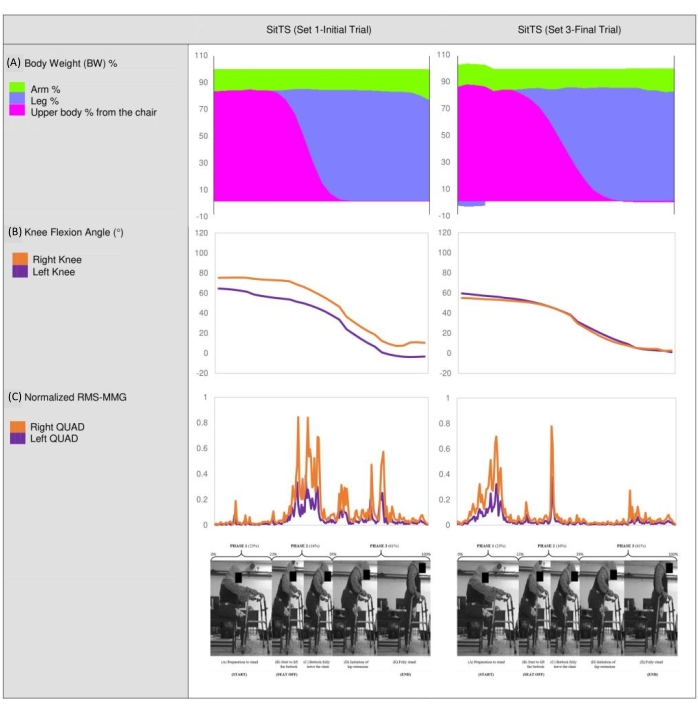
Figure 6: Participant 2's body weight contribution, knee flexion angle, and normalized quadriceps RMS-MMG during voluntary SitTS (Set 1-Initial Trial versus Set 3-Final Trial). The figure illustrates the parameters obtained by Participant 2 during the voluntary SitTS exercise. Please click here to view a larger version of this figure.
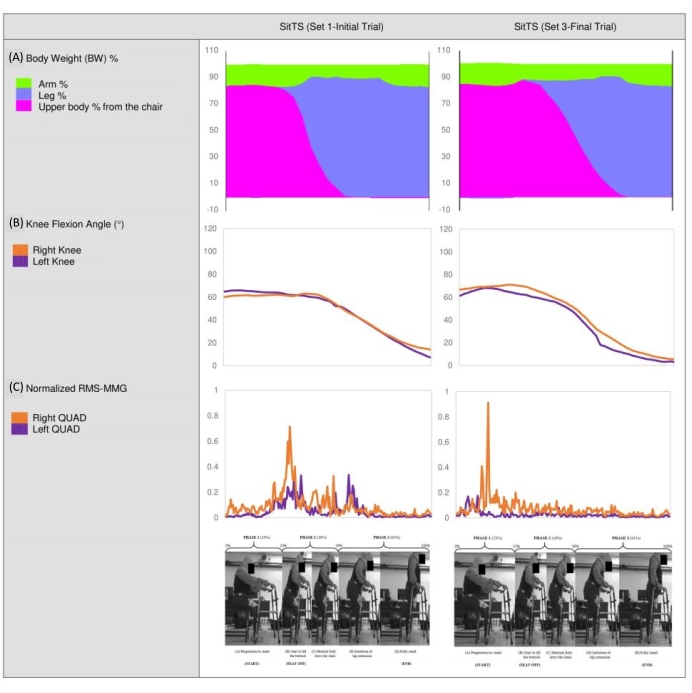
Figure 7: Participant 2's body weight contribution, knee flexion angle, and normalized quadriceps RMS-MMG during assisted FES SitTS (Set 1-Initial Trial versus Set 3-Final Trial). The figure explains the parameters obtained by Participant 2 during FES assisted SitTS exercise. Please click here to view a larger version of this figure.
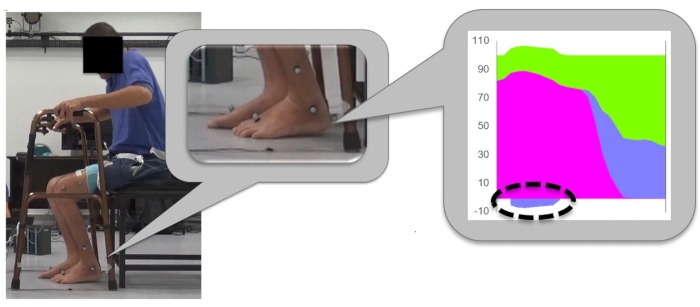
Figure 8: The condition of SCI participants lifting the leg hence producing the negative value of the legs force during the early phase of SitTS. The figure verifies the negative value obtains from the legs' force when participant tries to lift the heel during the initial phase of SitTS. Please click here to view a larger version of this figure.
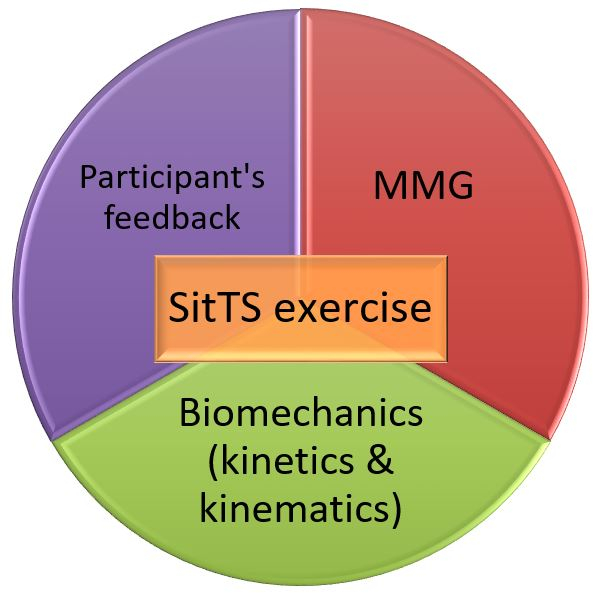
Figure 9: The combination of the determinants in the SitTS experiment. The figure concludes the combined parameters involved in the SitTS study. Please click here to view a larger version of this figure.
| Participant | Leg | FES current (mA) | |
| Quadriceps | Gluteal Maximus | ||
| 1 | R | 58 | 46 |
| L | 46 | 46 | |
| 2 | R | 35 | 28 |
| L | 35 | 28 | |
Table 1: FES current stimulated during SitTS study. The table shows the amplitude of FES current for each participant on the quadriceps and gluteal maximus muscle.
| Participant | Number of SitTS trials | |||||
| No FES | FES | |||||
| Set 1 | Set 2 | Set 3 | Set 1 | Set 2 | Set 3 | |
| 1 | 96 | 30 | 31 | 96 | 61 | 36 |
| 2 | 95 | 92 | 55 | 89 | 91 | 90 |
Table 2: Number of completed trials of SitTS movements by two SCI individuals. The table provides the total number of SitTS trials by the participants.
| Trials | N | No FES | FES |
| Mean time (s) | Mean time (s) | ||
| Initial | 60 | 1.57 ± 0.244 | 1.28 ± 0.123a |
| Final | 60 | 1.84 ± 0.210 | 1.66 ± 0.295a |
Table 3: Mean time for a complete cycle of SitTS during initial and final trials in each set. The table presents the mean time taken for participants to complete a cycle of SitTS during initial and final trials in each set. An independent sample t-test was done, values were given as mean ± SD (N = 60). Means with superscripts 'a' were significant (p < 0.0005).
| Participant 1 | Participant 2 | ||||||
| Without FES | With FES | Without FES | With FES | ||||
| Which event(s) do you think is the most tiring for your upper limbs? | B | B | B | B | |||
| Which event(s) do you think is the most tiring for your lower limbs? | C | C | C | C | |||
| Which event(s) do you think is the most stable during experiment? | C | E | A | A | |||
| Which event(s) do you think is the least stable during experiment | E | B | C | C | |||
Table 4: Reported stability and fatigue experienced by participants during the accomplishment of SitTS activity. The table shows the answer given by participants regarding their stability and fatigue experienced during SitTS exercise.
Discussion
The current study demonstrated a bodyweight contribution in SCI individuals during SitTS exercise. This study presented SF as an essential assistive device for paraplegics to do a successful SitTS cycle. Moreover, an instrumented SF was developed to ensure the arms force can be assessed too28. The application of MMG was added in the study to observe prime SitTS muscle that helps researchers to understand SitTS performance better. Furthermore, the feedback session enabled researchers to obtain insights regarding their subjective feeling that support the evidence of quantitative data of the SitTS study.
Representative results showed a negative magnitude of legs force which indicated the eliminated force that existed at the feet before the calibration process took place (Figure 8). These SitTS protocol addressed a limitation of producing negative value of legs' force during the early phase of the exercise. Hence researchers shall anticipate a modification technique of these conditions for future similar SitTS exercises. Additionally, we found that MMG device is more suitable to measure muscle activity during the FES-assisted SitTS exercise as compared to the electromyography (EMG).
MMG proposes an alternative to the utilization of EMG, especially in addressing the sensitive response to skin impedance changes. These impedance fluctuations may be initiated by sweating & incorrect measurements caused by the FES-induced electrical artifacts. While EMG detects the electrical activity of prime muscle of these movements, the presence of electrical stimulation through the muscle during the exercise interferes with the electrical-based motor action potential captured. MMG has been reported to be unaffected by the limitations of EMG29, which makes it advantageous for FES assisted SitTS exercise applications. Wessell et al. reported that MMG is more sensitive to muscle's mechanical responses generated by electrical stimulus compared to EMG, which is affected by other common electrical background30.
This study is limited by two main practical factors. Firstly, only 2 SCI participants fulfilled the inclusion criteria of the SitTS study from our accessible SCI volunteers. The low sample size of the population presents as the limitation of the study as they may not represent the highly different incomplete SCI population. This SitTS pilot study revealed the variation in arms and legs contribution based on their legs' MRC muscle grade. Further studies with more participants with different MRC muscle grade scores are recommended to further explain other potentially varying limbs strategies. Another limitation of this study is the learning effect achieved by the participants after completing the SitTS exercise on Day 1 that may have affected their performance on Day 2. The SitTS exercise was expected to display a higher number of trials on Day 2 since the same training had been done before in Day 1, and FES was applied in addition31. Hence, alternating the treatment between Day 1 and Day 2 (with and without FES) and between participants is ideal for performing the SitTS experiment to ascertain any potential benefit over the other. In this study, the order of the SitTS exercise for Participant 2 was switched (i.e., FES-assisted in Day 1 and voluntary SitTS in Day 2), and these orders shall be alternated with new participants' intake in the future.
The significance of this SitTS study highlighted a portable instrumented SF where it can be easily replicated by other researchers with an existing motion analysis laboratory setup. This technique was supported by another study from Chang et al. that also had instrumented walker with two load cells. Their study focused on the implanted neuroprosthesis users who mostly relied on their upper limbs during stand-to-sit activity28.
Although the FES intervention in SitTS exercise did not obviously alter the biomechanical contributions of arms and legs, the participants' perception of arms and leg fatigue was positively influenced by FES. This may not manifest itself in terms of the ground reaction force or joint angles but was felt by the SCI participants while performing the SitTS exercise. FES application gave participants a major impact to execute the better training performance in terms of more trials can be achieved. Both participants acknowledged the therapeutic benefit of the FES, in particular, the increased muscle mass11; hence they felt more motivated to participate in the SitTS study. The findings of this study provide important insight into FES in the clinical rehabilitation program. FES is believed to have more potential benefits for the post-SCI population.
The results obtained are helpful for researchers and clinicians to interpret the fatigue stage of patients throughout SitTS training in a clinical rehabilitation setting, especially for spinal cord injury patients whose legs were reported to be partially involved when stimulated with FES5. As SitTS training has high outcome specificity2, it is crucial for the training sessions to be fully informed of the movement and muscle performance. Clinicians may use these important parameters to evaluate the fatigue experienced by the targeted participants. Hence the current SitTS results promote a more rational approach to designing a proper SitTS training program.
Since SCI patients do not utilize the momentum transfer manouver5 as do healthy able-bodied people, it becomes more important that the training be done using a complete but relatively simple and portable setup as SCI patients relied heavily on their arm support to perform SitTS28. This should include primary outcome measures recommended in the clinical practice guideline14. Hence this study may benefit the clinical society as it is easy to replicate while taking into account the participants' feedback, at the same time looking at the biomechanics and the muscle activity level through MMG. Other potential outcomes that can be gained from SitTS training are bone mineral density improvement11 and better ground reaction force transfer rate7 with different stimulation parameters. The setup can also be used for safe and controlled stand-to-sit movement28 training among people with incomplete SCI.
Disclosures
The authors have nothing to disclose.
Acknowledgements
The authors acknowledge and appreciate all the SCI volunteers who participated in this study. This research was supported by the Ministry of Higher Education, Malaysia, and the University of Malaya through Fundamental Research Grant Scheme (FRGS) Grant No. FP002-2020; FRGS/1/2020/SKK0/UM/02/1.
Materials
| Customade chair | A customade chair was built to following to the force plate's dimension. | ||
| FES RehaStim 2 | Hasomed | A device that can stimulate electrical current towards the muscle. | |
| FlexiForce A201 | Tekscan, Inc., USA | Force ranges: 0-100 lbs. (440 N) | Force sensors is used to capture arms force at standing frame. |
| Foldable standing frame | Height: 70.0 cm – 90.0 cm. | A walking frame that was bought from local medical company. | |
| Motion Analysis | Vicon Oxford, UK | A system that records kinematic and kinetics of the activity. | |
| Serial port terminal application | CoolTerm | version 1.4.6; Roger Meier's | An application to record the force sensor data. |
| Vibromyography software | BIOPAC System Inc., USA | AcqKnowledge 4.3.1 | A software to record and strore raw MMG data. It also function for offline analyses. |
| VMG transducers and BIOPAC Vibromyography system | BIOPAC System Inc., USA | BP150 and HLT100C | A device to measure muscle activity. |
References
- Nithiatthawanon, T., Amatachaya, P., Thaweewannakij, T., Manimmanakorn, N., Mato, L., Amatachaya, S. The use of lower limb loading ability as an indicator for independence and safety in ambulatory individuals with spinal cord injury. European Journal of Physical and Rehabilitation Medicine. 57 (1), 85-91 (2021).
- Chaovalit, S., Taylor, N. F., Dodd, K. J. Sit-to-stand exercise programs improve sit-to-stand performance in people with physical impairments due to health conditions: a systematic review and meta-analysis. Disability and Rehabilitation. 42 (9), 1202-1211 (2020).
- Tekmyster, G., et al. Physical therapy considerations and recommendations for patients following spinal cord stimulator implant surgery. Neuromodulation. , (2021).
- Kamnik, R., Bajd, T., Kralj, A. Functional electrical stimulation and arm supported sit-to-stand transfer after paraplegia: A study of kinetic parameters. Artificial Organs. 23 (5), 413-417 (1999).
- Bahrami, F., Riener, R., Jabedar-Maralani, P., Schmidt, G. Biomechanical analysis of sit-to-stand transfer in healthy and paraplegic subjects. Clinical Biomechanics. 15 (2), 123-133 (2000).
- Roy, G., Nadeau, S., Gravel, D., Piotte, F., Malouin, F., McFadyen, B. J. Side difference in the hip and knee joint moments during sit-to-stand and stand-to-sit tasks in individuals with hemiparesis. Clinical Biomechanics. 22 (7), 795-804 (2007).
- Crosbie, J., Tanhoffer, A., Fornusek, C. FES assisted standing in people with incomplete spinal cord injury: a single case design series. Spinal Cord. 52 (3), 251-254 (2014).
- Eitzen, I., Fernandes, L., Nordsletten, L., Snyder-Mackler, L., Risberg, M. A. Weight-bearing asymmetries during Sit-To-Stand in patients with mild-to-moderate hip osteoarthritis. Gait & Posture. 39 (2), 683-688 (2014).
- Petrella, M., Selistre, L. F. A., Serrao, P., Lessi, G. C., Goncalves, G. H., Mattiello, S. M. Kinetics, kinematics, and knee muscle activation during sit to stand transition in unilateral and bilateral knee osteoarthritis. Gait & Posture. 86, 38-44 (2021).
- Mao, Y. R., et al. The crucial changes of Sit-to-Stand phases in subacute stroke survivors identified by movement decomposition analysis. Frontiers in Neurology. 9, (2018).
- Zoulias, I. D., et al. Novel instrumented frame for standing exercising of users with complete spinal cord injuries. Scientific Reports. 9 (1), 13003 (2019).
- Abd Aziz, M., Hamzaid, N. A., Hasnan, N., Dzulkifli, M. A. Mechanomyography-based assessment during repetitive sit-to-stand and stand-to-sit in two incomplete spinal cord-injured individuals. Biomedical Engineering/Biomedizinische Technik. 65 (2), 175-181 (2020).
- Mazza, C., Benvenuti, F., Bimbi, C., Stanhope, S. J. Association between subject functional status, seat height, and movement strategy in sit-to-stand performance. Journal of the American Geriatrics Society. 52 (10), 1750-1754 (2004).
- Moore, J. L., Potter, K., Blankshain, K., Kaplan, S. L., O’Dwyer, L. C., Sullivan, J. E. A core set of outcome measures for adults with neurologic conditions undergoing rehabilitation: A clinical practice guideline. Journal of Neurologic Physical Therapy. 42 (3), 174-220 (2018).
- Abd Aziz, M., Hamzaid, N. A. FES Standing: The effect of arm support on stability and fatigue during Sit-to-Stand manoeuvres in sci individuals. International Conference for Innovation in Biomedical Engineering and Life Sciences. IFMBE Proceedings. 67, (2017).
- Plumlee, E., et al. Effects of ankle bracing on knee joint biomechanics during an unanticipated cutting maneuver. Conference Proceedings of the Annual Meeting of the American Society of Biomechanics. , 807-808 (2010).
- Estigoni, E. H., Fornusek, C., Hamzaid, N. A., Hasnan, N., Smith, R. M., Davis, G. M. Evoked EMG versus muscle torque during fatiguing functional electrical stimulation-evoked muscle contractions and short-term recovery in individuals with spinal cord injury. Sensors (Basel). 14 (12), 22907-22920 (2014).
- Hamzaid, N., Fornusek, C., Ruys, A., Davis, G. Development of an isokinetic FES leg stepping trainer (iFES-LST) for individuals with neurological disability. 2009 IEEE International Conference on Rehabilitation Robotics. , 480-485 (2009).
- Assess muscle effort with vibromyography. Sonostics Inc Available from: https://www.biopac.com/application-note/vibromyography-vmg-assess-muscles-effort/ (2019)
- Donovan-Hall, M. K., Burridge, J., Dibb, B., Ellis-Hill, C., Rushton, D. The views of people with spinal cord injury about the use of functional electrical stimulation. Artificial Organs. 35 (3), 204-211 (2011).
- Kagaya, H., et al. Restoration and analysis of standing-up in complete paraplegia utilizing functional electrical stimulation. Archives of Physical Medicine and Rehabilitation. 76 (9), 876-881 (1995).
- Jeon, W., Hsiao, H. Y., Griffin, L. Effects of different initial foot positions on kinematics, muscle activation patterns, and postural control during a sit-to-stand in younger and older adults. Journal of Biomechanics. 117, 110251 (2021).
- Nadeau, S., Desjardins, P., Briere, A., Roy, G., Gravel, D. A chair with a platform setup to measure the forces under each thigh when sitting, rising from a chair and sitting down. Medical & Biological Engineering & Computing. 46 (3), 299-306 (2008).
- Lee, S. K., Lee, S. Y. The effects of changing angle and height of toilet seat on movements and ground reaction forces in the feet during sit-to-stand. Journal of Exercise Rehabilitation. 12 (5), 438-441 (2016).
- Camargos, A. C. R., Rodrigues-de-Paula-Goulart, F., Teixeira-Salmela, L. F. The effects of foot position on the performance of the sit-to-stand movement with chronic stroke subjects. Archives of Physical Medicine and Rehabilitation. 90 (2), 314-319 (2009).
- Beck, T. W., et al. Comparison of Fourier and wavelet transform procedures for examining the mechanomyographic and electromyographic frequency domain responses during fatiguing isokinetic muscle actions of the biceps brachii. Journal of Electromyography and Kinesiology. 15 (2), 190-199 (2015).
- Lee, M. Y., Lee, H. Y. Analysis for Sit-to-Stand performance according to the angle of knee flexion in individuals with hemiparesis. Journal of Physical Therapy Science. 25 (12), 1583-1585 (2013).
- Chang, S. R., Kobetic, R., Triolo, R. J. Understanding stand-to-sit maneuver: Implications for motor system neuroprostheses after paralysis. Journal of Rehabilitation Research and Development. 51 (9), 1339-1351 (2014).
- Woods, B., Subramanian, M., Shafti, A., Faisal, A. A. Mechanomyography based closed-loop functional electrical stimulation cycling system. 2018 7th IEEE International Conference on Biomedical Robotics and Biomechatronics (Biorob. , (2018).
- Wessell, N., Khalil, J., Zavatsky, J., Ghacham, W., Bartol, S. Verification of nerve decompression using mechanomyography. Spine Journal. 16 (6), 679-686 (2016).
- Britton, E., Harris, N., Turton, A. An exploratory randomized controlled trial of assisted practice for improving sit-to-stand in stroke patients in the hospital setting. Clinical Rehabilitation. 22 (5), 458-468 (2008).

