Particle Image Velocimetry Investigation of Hemodynamics via Aortic Phantom
Summary
The present protocol describes particle image velocimetry (PIV) measurements performed to investigate the sinus flow through the in vitro setup of the transcatheter aortic valve (TAV). The hemodynamic parameters based on velocity are also determined.
Abstract
Aortic valve dysfunction and stroke have recently been reported in transcatheter aortic valve implantation (TAVI) patients. Thrombus in the aortic sinus and neo-sinus due to hemodynamic changes has been suspected. In vitro experiments help investigate the hemodynamic characteristics in the cases where an in vivo assessment proves to be limited. In vitro experiments are also more robust, and the variable parameters are controlled readily. Particle image velocimetry (PIV) is a popular velocimetry method for in vitro studies. It provides a high-resolution velocity field such that even small-scale flow features are observed. The purpose of this study is to show how PIV is used to investigate the flow field in the aortic sinus after TAVI. The in vitro setup of the aortic phantom, TAVI for PIV, and the data acquisition process and post-processing flow analysis are described. The hemodynamic parameters are derived, including the velocity, flow stasis, vortex, vorticity, and particle residence. The results confirm that in vitro experiments and PIV help investigate the hemodynamic features in the aortic sinus.
Introduction
Aortic stenosis is a common disease in older adults, and it is when the aortic valve doesn't open, reducing blood flow. The problem is caused by the thickening or calcification of the aortic valve1. Therefore, it is a necessary treatment to enhance the blood flow and decrease the load on the heart. It is treated by remodeling the aortic valve or replacing it with an artificial valve. This study focuses on transcatheter aortic valve implantation (TAVI), replacing the malfunctioning aortic valve with an artificial one using a catheter.
TAVI has been recommended for patients challenged in surgery, and the mortality has also been low2. Recently, it has been reported that thrombus in patients after TAVI caused valve dysfunction and stroke3,4. Thrombus in the aortic sinus and neo-sinus is suspected, with its cause probably being the changes in the hemodynamics caused by TAVI. It is performed without removing the native leaflets; these leaflets can disturb the sinus flow and elevate the risk of thrombosis5.
It is difficult to determine how blood flow is affected by TAVI and how thrombosis is induced in patients. It is desirable to elucidate the relationship between blood flow and thrombus formation in vivo. However, a lack of practical techniques for measuring blood flow makes this problematic. On the other hand, in vitro techniques have the advantage of allowing one to monitor the changes in the blood flow by limiting the parameters that must be investigated. In vitro setup and particle image velocimetry (PIV) have been used to identify velocity in medical fields6,7,8. Therefore, in vitro and PIV are sufficient for determining the parameters to be reported by mimicking the patient's condition: the heart rate and pressure, viscosity, and sinus geometry, and allowing one to control these parameters.
In this study, in vitro setup and PIV are used to investigate the flow in the aortic sinus after TAVI. The aortic phantom and TAVI for the PIV and the data acquisition process and post-processing flow analysis are described in this protocol. Various hemodynamic parameters are derived, including the velocity, stasis, vortex, vorticity, and particle residence. The results demonstrate that in vitro setup and PIV help investigate the hemodynamic features in the aortic sinus.
Protocol
1. In vitro setup
- Prepare the experimental setup on an optic table, including a piston pump, data acquisition device (DAQ), and a computer with the required system engineering software and a motor controlling software (see Table of Materials) (Figure 1).
NOTE: The piston pump has been previously tested and calibrated and consists of a motor, motor driver, and linear actuator9. - Import the spreadsheet file with the flow rate information to the system engineering software.
NOTE: For example, heart rate is 60 bpm, the maximum flow rate is 20 L/min, cardiac output is 4.8 L/min, and stroke volume is 70 mL. - Set the parameter in systems engineering software, such as DAQ input and output channel; sample clock is 1,000 and feedback iteration is 10.
- Set the parameter in the motor controlling software; lead screw length is 10 mm, analog input and output are 14.5 mm/voltage.
- Install the check valve and resistance valve to the reservoir10.
NOTE: The check valve is connected to the piston pump as an inlet of the system, and the ball valve is connected to the acrylic sinus model as an outlet of the system. - Fix the acrylic sinus model (Figure 2) with a square aluminum bar to the optic table.
NOTE: The dimensions of the acrylic sinus model are presented in Table 1. - Install the pressure gauge (~0-15 psi) to the pressure tap of the acrylic sinus model for receiving a pressure signal from another computer.
NOTE: The pressure taps are located 140 mm from the sinotubular junction (STJ). - Prepare a working fluid by mixing saline and glycerin (see Table of Materials) in a mass ratio of 60:40.
NOTE: A viscometer and a refractometer were used to measure the working fluid's viscosity and refractive index. The viscosity is ~4 cp, the refractive index is 1.45, and the density is 1,100 kg/m3. - Connect the reservoir, piston pump, and the acrylic sinus model with a silicone hose (see Table of Materials).
- Tie the transcatheter aortic valve (TAV) (see Table of Materials) to the native leaflet made by a 3D printer with a thread11.
- Combine the fixed TAV on the native leaflet with the acrylic sinus model.
NOTE: The TAV used here (obtained commercially) has a diameter of 23 mm and 26 mm, and height is 18 mm and 20 mm, respectively12. For TAV (23 mm), the deployment depth and native leaflet length were 1.8 mm and 9 mm, and for TAV (26 mm), it is 2.0 mm and 10 mm, respectively. The inner diameter of the native leaflet was 21 mm, considering the patient's annulus size.
CAUTION: The TAV dries out if not preserved in saline solution. It is kept in the liquid even after being tied to the native leaflet. - Fill the working fluid (step 1.8) in the in vitro system.
CAUTION. Avoid making bubbles on the acrylic sinus model because it affects PIV results.
2. PIV setup
- Locate the laser on another optic table and one-axis rail.
NOTE: The laser is a continuous Nd: YAG laser that emits light with a wavelength of 532 nm and whose power can increase to 10 W (see Table of Materials). The laser sheet passed through optics has a 1 m distance from the acrylic sinus model. - Locate the high-speed camera on a 2-axis traverse and move the traverse.
CAUTION: The high-speed camera is perpendicular to the laser sheet and acrylic sinus model. - Equip the lens to the high-speed camera.
NOTE: The macro lens mounted on the high-speed camera has a focal length of 105 mm, and the aperture is f/2.8. - Seed particle (see Table of Materials) in the reservoir.
NOTE: The particle is a hollow glass sphere with an average diameter of 10 µm and a density of 1,090 kg/m3. The reservoir has a rectangular shape and, the width, length, and height inside are 23 cm, 23 cm, 35 cm, respectively. There is a hole for fastening in the upper part. The lid also had a hole for fastening and a bolt tap to install the bulb pump to apply pressure. - Program an external trigger using an open-source electronic prototypic platform, Arduino (see Table of Materials).
NOTE: When the piston pump moves a predetermined distance, the output of Arduino becomes 1, which is transmitted to the high-speed camera as a trigger to be photographed. - Run the camera controlling software (see Table of Materials), click on Current Session Reference (CSR), and remove the lens cap.
- Turn on the laser, set it to 7 W, and locate the laser sheet to the center of the TAV.
- Take a snapshot and check the particle density and diameter.
NOTE: To reduce errors, confirm that ~8-10 particles are in the interrogation window, with a particle diameter of 2-4 pixels13. - Set the parameters, such as resolution (1280 x 720), random frame rate, exposure time to maximum according to random frame rate in the camera controlling software.
- Click on the Enable button in the motor controlling software at first and click on the Start button in the systems engineering software to operate the piston pump.
- Take a picture and check whether the maximum particle distance is less than 4-6 pixels.
NOTE: This study corresponds to 50% of the interrogation window, which set 16 pixels between velocity vectors. The maximum distance of particles in the interrogation window is limited to 8 pixels. - Repeat step 2.11 to ensure the maximum particle distance within that range by adjusting the frames per second (fps) if it is more than 6 pixels and lowering the fps if it is less than 4 pixels.
3. Investigation of hemodynamics
- Check whether there is leakage from the connection part of the acrylic sinus model or the silicone hose becomes folded.
- Import the excel file having stored flow rate and bpm information in the system engineering software.
NOTE: For example, heart rate is 60 bpm, the maximum flow rate is 20 L/min, cardiac output is 4.8 L/min, stroke volume is 70 mL (Figure 3A). - Confirm the system engineering software parameter, such as DAQ device input and output channel. The sample clock is 1,000, and the feedback iteration is 10.
- Confirm the motor controlling software parameter, e.g., lead screw length is 10 mm, analog input and output are 14.5 mm/voltage.
- Turn on the high-speed camera and run the camera controlling software.
- Click on CSR and remove a lens cap.
- Set the camera controlling software parameters, e.g., the resolution of 1280 x 720, a frame rate of 300 fps, burst period of 200 µs and 150 µs, burst count of 3, and exposure (forced by the burst period).
- Turn on the laser, set it to 7 W, and locate the laser sheet on the center of TAV. Focus on the laser sheet by controlling the lens.
- Adjust the pressure to the reservoir.
NOTE: The mean post-valvular pressure is 100 mmHg while operating the piston pump (Figure 3B,C). - Click on the Enable button in the motor controlling software at first and click on the Start button in the system engineering software to operate the piston pump.
- Wait until the flow rate stabilizes.
NOTE: The flow rate calculates the difference based on the signal from the piston pump and executes negative feedback, so it takes time to wait until it stabilizes. - Check a trigger that works in the Arduino serial plotter.
- Capture particle images for continuous 14 cycles and repeat a total of seven times.
NOTE: The storage capacity of a high-speed camera is related to the resolution and the number of particle images. According to the parameter set in step 3.7, it is possible to take a picture only for 14 cycles at a time.
4. Data processing
- Convert from .cine file to .tiff files using the camera controlling software.
- Calculate the average image for all the particle images over time. Remove the area corresponding to the reflection of the laser at the wall or the TAV by subtracting the average image14.
- Make the mask by separating the areas to be analyzed from those to discard.
NOTE: In this study, two masks were used: one to analyze the sinus region alone and the other to analyze the entire region, which contains the region after STJ. - Perform PIV using the PIVlab, an open-source tool based on MATLAB15 (see Table of Materials).
- Import particle images saved by the time-resolved method or pairwise method.
- Execute contrast limited adaptive histogram equalization (CLAHE)16.
NOTE: CLAHE is a method for image pre-processing. The contrast of the particle image is redistributed so that the laser reflects the increase and decrease in the particle intensity. The particle image is divided by a window with 20 pixels. - Import the mask and apply it to all the particle images.
- Set the multi-pass interrogation window.
NOTE: The interrogation window is decreased from 64 x 64 to 32 x 32 with a 50% overlap. The distance between the two vectors corresponds to 16 pixels. - Execute the cross-correlation13 about the particle image pair converted into the frequency domain using fast Fourier transform (FFT)13.
- Find a peak value using a 2 x 3 Gaussian fit in correlation result.
NOTE: The peak value selected in the Gaussian fitting determined the particle distance.
- Run the smoothing process, which involves the following processes.
- Remove the outliers into a "NaN" using the "isoutlier" built-in function in MATLAB.
- Interpolate a nan to value using the "inpaint_nans" function in MATLAB15.
- Convert from "pixel/frame" to "m/s" according to the frame rate and burst period.
NOTE: The conversion is related to the time interval, determined by the frame rate and burst period. Specifically, the coefficient of the time-resolved method is derived by the frame rate, and that of a pairwise method is derived by the burst period. - Merge the pairwise method and time-resolved method using the weighting factor.
NOTE: The weighting factor depends on the velocity magnitude and has a total value of 1 in each section. If the velocity magnitude exceeds a certain threshold, the factor for the pairwise method is higher than that for the time-resolved method. - Run the "smoothn" function of DCT-PLS using a smoothing factor of 0.5915,17.
NOTE: The "smoothn" and "inpaint_nans" functions are present in the PIVlab.
5. Data analysis
- Load PIV data into MATLAB.
- Extract "u" and "v" components from the PIV data.
- Calculate the velocity field18 (Equation 1, Supplementary File 1).
- Derive hemodynamics parameters using the in-house code and built-in function19.
- Derive the vorticity with MATLAB built-in function "curl"18 (Equation 2, Supplementary File 1).
- Derive the stasis with the in-house code20 (Equation 3, Supplementary File 1).
- Derive the Γ1 with the in-house code21 (Equation 4, Supplementary File 1).
- Derive the particle residence with an in-house code19 (Equation 5, Supplementary File 1).
- Calculate the average and standard deviation of hemodynamics parameters (Table 2).
NOTE: Peak velocity, vorticity, Γ1, and stasis were calculated for a total of 98 cycles. The decay was obtained through exponential fitting to the percentage of particle residence. The decay set 14 cycles as one dataset and calculated the average and standard deviation for seven times.
Representative Results
The velocity fields showed a different sinus flow structure depending on the valve diameter in Figure 4. For TAV (23 mm), the velocity was higher than 0.05 m/s between TAV and STJ from early systole to peak systole that TAV was opened using the forwarding jet. High velocity was then distributed in a narrow range near the stent at late systole. The velocity at diastole was lower than 0.025 m/s, and two vortexes with low velocity appeared. For TAV (26 mm), when the valve opened, high velocity was measured at STJ. In time except for early systole, velocity distribution in sinus was lower than 0.05 m/s. Specifically, the velocity at late systole was lower than at another time. The one-direction vortex, which had an oval shape, is observed above the native leaflet at diastole.
The hemodynamics parameters derived by velocity are shown in Figure 5 and Table 2. The peak velocity in TAV (23 mm) was higher than TAV (26 mm). Stasis was observed in the sinus except for the forwarding jet and becoming into the sinus. The stasis area formed in TAV (23 mm) was broad, but the fraction of stasis was low. The vortex and vorticity at diastole presented something not confirmed in the velocity field. For TAV (23 mm), two similar vortices were noticed above and below the native leaflet. But for TAV (26 mm), the clockwise vortex was not clear; the counterclockwise vortex had an elliptical shape. The vorticity showed that was similar results to the vortex. The positive was near the stent and native leaflet, and the negative was observed in another region.
The percentage and snapshot of particle residence are shown in Figure 6. The snapshots of particle residence showed particle distribution in the sinus region for 2 s, and the percentage of particle residence showed that fraction of remaining particles in the sinus region for 14 s. In Figure 6B, the TAV (26 mm) decreased faster than TAV (23 mm), but both cases were presented that all particles left the sinus region within 6 s. The particles moved out of the region in Figure 6A, but it was not identical in cases. For TAV (23 mm), particles were distributed in the entire sinus region and went out of the plane as the cycle progressed. This did not happen for TAV (26 mm) and showed different aspects. The particles were concentrated near the annulus, which left the sinus region from the bottom of the native leaflet.
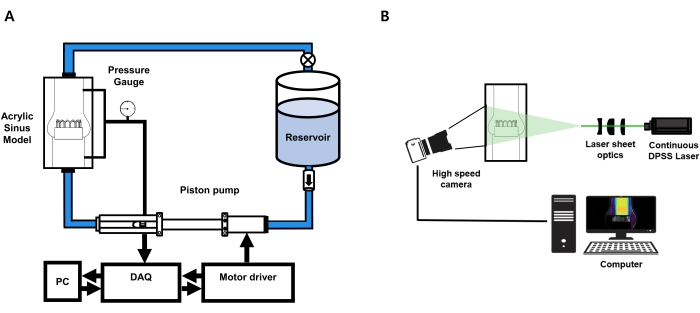
Figure 1: In vitro experimental setup. It consists of a high-speed camera, an acrylic sinus model, a piston pump system, a reservoir, an Arduino, and a computer. It is a closed system and flows only in one direction due to the check valve installed in the reservoir and TAV installed in the acrylic sinus model. Please click here to view a larger version of this figure.
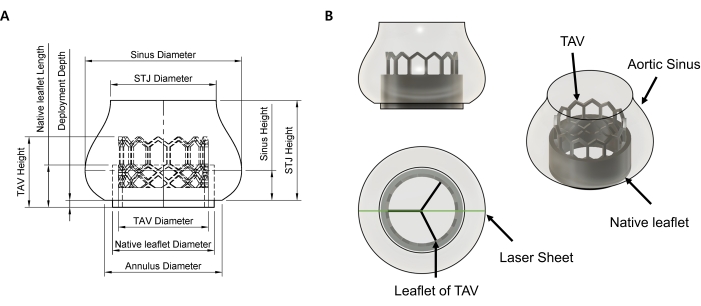
Figure 2: The acrylic sinus model with native leaflet and TAV (23mm). (A) The drawing and naming of the dimensions are listed in Table 1. For both artificial valves, the acrylic sinus model is the same. (B) Modeling about native leaflet and stent of TAV (23 mm). The native leaflet is cylindrical in shape and is not transparent. In modeling, the leaflet of TAV was omitted and only presented stent. TAV; Transcatheter aortic valve, STJ; sinotubular junction. Please click here to view a larger version of this figure.
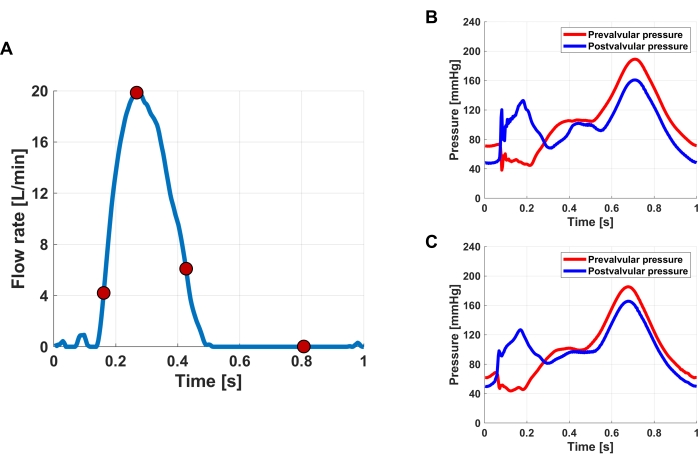
Figure 3: Flow rate and pressure for 1 s. (A) Flow rate is derived by stroke volume for 1 s; maximum flow rate is 20 L/min. The red dot in flow rate is instance time from the left at the early systole, peak systole, late systole, and diastole, respectively. (B) The pressure of TAV (23 mm). (C) The pressure of TAV (26 mm). The blue line is post-valvular pressure, and the red is pre-valvular pressure. Please click here to view a larger version of this figure.
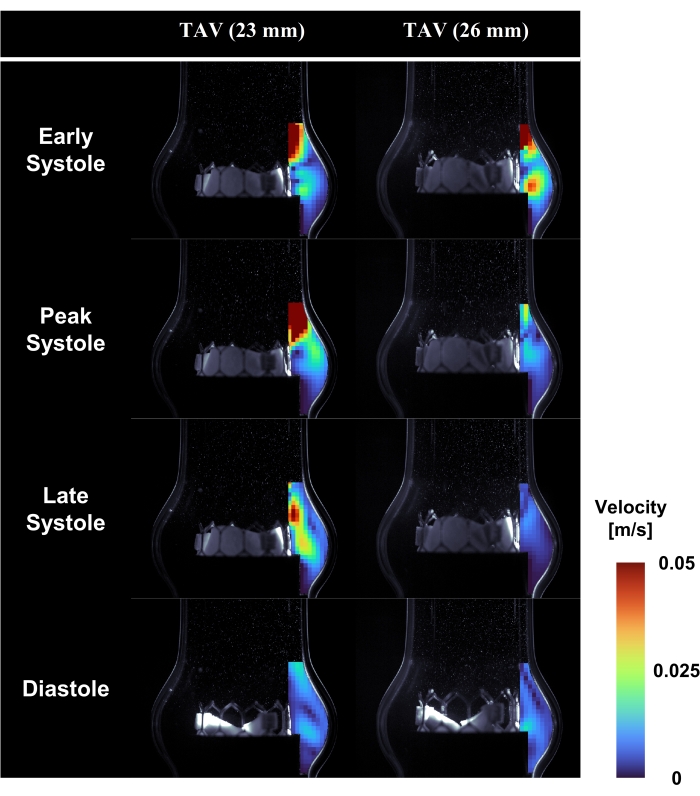
Figure 4: Velocity field in the sinus region. Velocity contour is ranged from 0-0.05 m/s. The left row is the velocity field of TAV (23 mm), and the right row is that of TAV (26 mm). The column is instance time defined at a flow rate. Please click here to view a larger version of this figure.
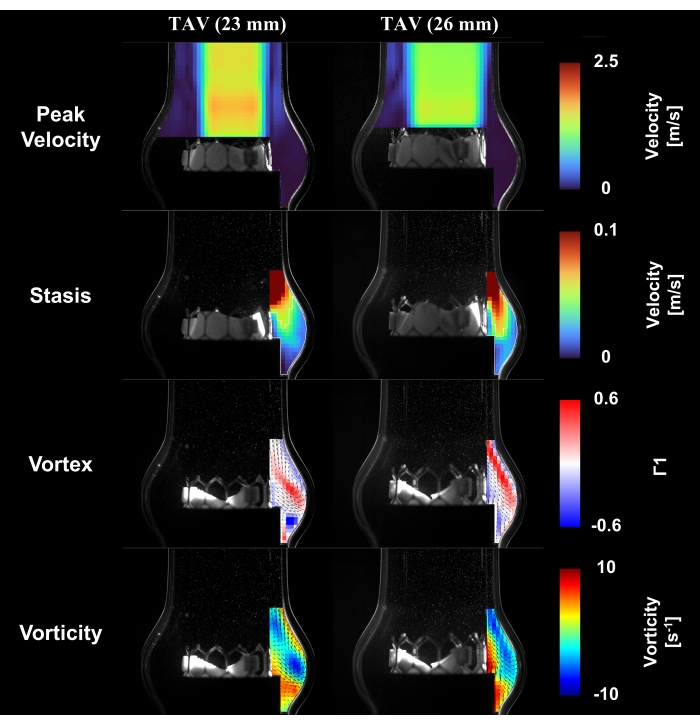
Figure 5: Sinus hemodynamics result. The peak velocity contour is presented at peak systole. Flow stasis is projected for the cycle, and it is that internal region shown by a white line. The vortex and vorticity are represented as velocity vector and contour at diastole. Please click here to view a larger version of this figure.
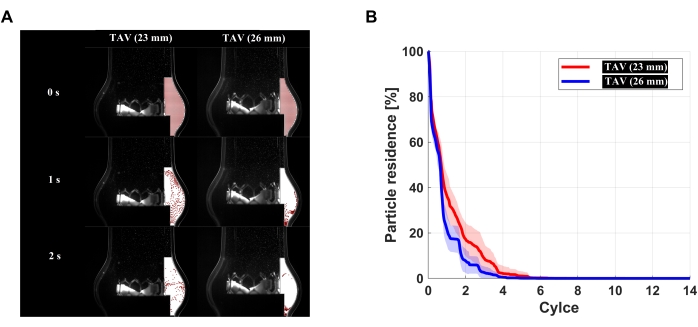
Figure 6: Snapshots and percentage of particle residence. (A) particle residence for 2 s is presented with a white patch indicated sinus region and red circle indicated virtual particles. (B) The percentage of particle residence for 14 s is that the red line is TAV (23 mm), and the blue line is TAV (26 mm). Please click here to view a larger version of this figure.
| Peak velocity (m/s) | Vorticity (s-1) | Vortex | Stasis | Decay | |
| TAV (23 mm) | 1.74 ± 0.03 | 10.13 ± 1.76 | 0.58 ± 0.08 | 0.44 ± 0.13 | -0.95 ± 0.21 |
| TAV (26 mm) | 1.43 ± 0.03 | 7.42 ± 1.16 | 0.33 ± 0.10 | 0.50 ± 0.09 | -1.35 ± 0.28 |
Table 1: Dimensions of acrylic sinus model. All units are in mm.
| Unit (mm) | |||||
| TAV Diameter | TAV Height | Deployment Depth | Native leaflet Length | Native leaflet Diameter | |
| TAV (23 mm) | 23 | 18 | 1.8 | 9 | 26 |
| TAV (26 mm) | 26 | 20 | 2 | 10 | 29 |
| Unit (mm) | |||||
| STJ Diameter | STJ Height | Annulus Diameter | Sinus Diameter | Sinus Height | |
| TAV (23 mm) | 27 | 25.5 | 30 | 40 | 7.65 |
| TAV (26 mm) |
Table 2: Average and standard deviation about sinus hemodynamics parameter.
Supplementary File 1: Equations for data analysis. Please click here to download this File.
Discussion
The sinus flow changed due to different sinus geometry after TAVI. The vortex was formed by the aortic valve opening and the interaction with the forward jet of systole22. In the study of the artificial surgical valve without native leaflets, vortex observed in the sinus region at systole was normal23. This study forms the vortex presented at diastole by reducing the forward jet and coming into the sinus. The sinus flow encountered the native leaflet; as a result, it splits clockwise below the native leaflet and counterclockwise above. It suggests that patients after TAVI are different compared to healthy without thrombosis. So, the sinus flow changed after TAVI, possibly affecting thrombus formation in the sinus.
Thrombosis occurs because red blood cells are destroyed by shear stress, the stagnation flow, and external substances such as the stent of TAV24. In this study, thrombus formed by stagnation flow was considered, which was confirmed by hemodynamics parameters such as flow stasis and particle residence. The native leaflet physically prohibits the sinus flow and limits the sinus region. The sinus flow near the annulus becomes more restricted, increasing stasis. And for the particle residence, particles above the native leaflet quickly exit the region, whereas those below do not. The red blood cell has a small distance, aggregating in the sinus. It was also studied that flow stasis is observed at the bottom of the sinus when there is a native leaflet4. The problem after TAVI is that native leaflet remains, and research is needed to revise so as to inhibit thrombosis.
In vitro experiments and PIV successfully observe the velocity field in the sinus. However, there are still differences from actual patients, and it requires improvement. Firstly, the acrylic sinus model is simplified to allow fabrication at once. The right and left coronary are located on two of the three cusps; the blood goes to the coronary artery ~5% of the total during diastole10,25. One of the limitations of the present in vitro model is that the current model does not mimic physiological properties such as rheology, vascular structure, 3D vessel geometry, etc. Also, the current model does not include coronary flow. The previous studies demonstrated that coronary flow affects sinus flow. Secondly, the current 2D PIV analysis does not include the out-of-plane motion of the flow. Further study with volumetric measurement (e.g., 3D PIV/Particle tracking velocimetry (PTV)) can reveal the complex flow field in the aortic flow. Thirdly, PIV’s accuracy limitations due to individual variations of particle image intensities exist. The out-of-plane motion, even without noise, limits the achievable accuracy26,27. In this study, the accuracy of PIV measurement with subpixel interpolation is ~0.1 pixel, which corresponds to 0.03 m/s at TAV (23 mm) and 0.041 m/s at TAV (26 mm).
Future studies plan to use in vitro experiments and 3D fluid visualization methods to understand sinus hemodynamics. The acrylic sinus model is designed to have a tricuspid with a coronary artery. It will be split by avoiding interference in the sinus region. In this study, the measured area after STJ was also analyzed to confirm whether the velocity field is similar. Although not explained, it is hypothesized that sinus flow affects the leaflet motion of TAV. It is not protruding as a result. The measured area will focus only on the sinus to minimize problems such as blurred particle images by refracted laser. Also, 3D PTV is being prepared to observe the motion of the particle26,27. It will be helpful to understand the principle of thrombosis in the sinus after TAVI.
Disclosures
The authors have nothing to disclose.
Acknowledgements
This research was supported by the Basic Science Research Program of the National Research Foundation of Korea, which is funded by the Ministry of Education (NRF-2021R1I1A3040346 and NRF-2020R1A4A1019475). This study was also supported by 2018 Research Grant (PoINT) from Kangwon National University.
Materials
| 3D Printer | Prusa Research | Original Prusa i3 MK2; FDM printer | |
| Aluminum bar (square) | APSPRO | KHP-3030, KHP-6060 | Dimension: 30 mm x 30 mm, 60 mm x 60 mm |
| Bulb pump | Skyhope | MHL-1 | |
| Camera controlling software | Phantom | PCC 3.4 software | The software controll the high speed camera |
| Check valve | HANJU STEEL PIPE | Check valve; 1/2 inch (15A) | |
| Digital Aqusition device | National Instruments | USB-6001 | |
| Glycerin | ANU Korea | It used for making a working fluid | |
| High-speed camera | Phantom | Phantom VEO 710E-L | |
| Laser | Changchun New Industries Optoelectronics Technology | MGL-W-532; CW Nd:YAG Laser | |
| Linear actuator | THOMSON | PC-40; it converts the rotational motion to lenear motion | |
| Macro lens | Nikon | VR Micro-NIKKOR 105mm, f/1.4 | |
| Motor | KOLLMORGEN | AKM33H-ANCNR-00; DC servo motor | |
| Motor controlling software | KOLLMORGEN | Kollmorgen software; the software controll the motor driver | |
| Motor driver | KOLLMORGEN | AKD-B00606-NBAN-0000 | |
| Open-source electronic prototypic platform | Arduino | A000066 | Arduino Uno R3. It used for making a external trigger |
| Optic table | SMTECH | 1800 (W) x 900 (B) x 800 (H) | |
| Particle | Dantec Dynamics | 80A6011 | Hollow Glass Sphere. Mean diameter:10 µm, Density: 1090 kg/m3 |
| PIVlab | PIVlab | Open source algorithm based on MATLAB https://kr.mathworks.com/matlabcentral/fileexchange/27659-pivlab-particle-image-velocimetry-piv-tool-with-gui |
|
| Pressure gauge | OMEGA | PX309-015A5V. Measurement range: 0~15psi | |
| Refractometer | ATAGO | 2350 | R-5000. Hand held refractometer; measurement range: 1.333-1.520 |
| Resistance valve | HANJU STEEL PIPE | Ball valve; 1/2 inch (15A) | |
| Saline | DAI HAN PHARM | It is used for making a working fluid and for preserving the TAV | |
| Silicone hose | HSW | Inner diameter 26mm, Outter diameter 30mm; Inlet length 5m, Outlet length 1.5m | |
| System enginnering software | National Instruments | LabVIEW software. The software controlls the DAQ. | |
| Transcatheter Aortic Valve, TAV (23 mm) and TAV (26 mm) | Edwards Lifesciences | SAPIEN3 23mm, SAPIEN3 26mm. It is supported by Seoul Asan Medical | |
| Viscosmeter | Brookfiled | DVELV; Measurement range: 1-2×109 cp |
References
- Carabello, B. A., Paulus, W. J. Aortic stenosis. The Lancet. 373 (9667), 956-966 (2009).
- Jakobsen, L., et al. Short-and long-term mortality and stroke risk after transcatheter aortic valve implantation. The American Journal of Cardiology. 121 (1), 78-85 (2018).
- Koo, H. J., et al. Computed tomography features of cuspal thrombosis and subvalvular tissue ingrowth after transcatheter aortic valve implantation. The American Journal of Cardiology. 125 (4), 597-606 (2020).
- Midha, P. A., et al. The fluid mechanics of transcatheter heart valve leaflet thrombosis in the neosinus. Circulation. 136 (17), 1598-1609 (2017).
- Abubakar, H., Ahmed, A. S., Subahi, A., Yassin, A. S. Thrombus in the Right Coronary Sinus of Valsalva Originating From the Left Atrial Appendage Causing Embolic Inferior Wall Myocardial Infarction. Journal of Investigative Medicine High Impact Case Reports. 6, 2324709618792023 (2018).
- Charonko, J., Karri, S., Schmieg, J., Prabhu, S., Vlachos, P. In vitro, time-resolved PIV comparison of the effect of stent design on wall shear stress. Annals of Biomedical Engineering. 37 (7), 1310-1321 (2009).
- Hariharan, P., et al. Inter-laboratory characterization of the velocity field in the FDA blood pump model using particle image velocimetry (PIV). Cardiovascular Engineering and Technology. 9 (4), 623-640 (2018).
- Lim, W., Chew, Y., Chew, T., Low, H. Pulsatile flow studies of a porcine bioprosthetic aortic valve in vitro: PIV measurements and shear-induced blood damage. Journal of Biomechanics. 34 (11), 1417-1427 (2001).
- Kim, J., Lee, Y., Choi, S., Ha, H. Pulsatile flow pump based on an iterative controlled piston pump actuator as an in-vitro cardiovascular flow model. Medical Engineering & Physics. 77, 118-124 (2020).
- Moore, B. L., Dasi, L. P. Coronary flow impacts aortic leaflet mechanics and aortic sinus hemodynamics. Annals of Biomedical Engineering. 43 (9), 2231-2241 (2015).
- Evans, B. . Practical 3D printers: The science and art of 3D printing. , (2012).
- Yudi, M. B., Sharma, S. K., Tang, G. H., Kini, A. Coronary angiography and percutaneous coronary intervention after transcatheter aortic valve replacement. Journal of the American College of Cardiology. 71 (12), 1360-1378 (2018).
- Adrian, R. J., Westerweel, J. . Particle Image Velocimetry. , (2011).
- Deen, N. G., et al. On image pre-processing for PIV of single-and two-phase flows over reflecting objects. Experiments in Fluids. 49 (2), 525-530 (2010).
- Thielicke, W., Stamhuis, E. PIVlab-towards user-friendly, affordable and accurate digital particle image velocimetry in MATLAB. Journal of Open Research Software. 2 (1), (2014).
- Pizer, S. M., et al. Adaptive histogram equalization and its variations. Computer Vision, Graphics, and Image Processing. 39 (3), 355-368 (1987).
- Garcia, D. Robust smoothing of gridded data in one and higher dimensions with missing values. Computational Statistics & Data Analysis. 54 (4), 1167-1178 (2010).
- Elger, D. F., LeBret, B. A., Crowe, C. T., Roberson, J. A. . Engineering Fluid Mechanics. , (2020).
- Raghav, V., Sastry, S., Saikrishnan, N. Experimental assessment of flow fields associated with heart valve prostheses using particle image velocimetry (PIV): recommendations for best practices. Cardiovascular Engineering and Technology. 9 (3), 273-287 (2018).
- Ncho, B., Sadri, V., Ortner, J., Kollapaneni, S., Yoganathan, A. In-Vitro Assessment of the Effects of Transcatheter Aortic Valve Leaflet Design on Neo-Sinus Geometry and Flow. Annals of Biomedical Engineering. 49 (3), 1046-1057 (2021).
- Graftieaux, L., Michard, M., Grosjean, N. Combining PIV, POD and vortex identification algorithms for the study of unsteady turbulent swirling flows. Measurement Science and Technology. 12 (9), 1422 (2001).
- Yap, C. H., Saikrishnan, N., Tamilselvan, G., Yoganathan, A. P. Experimental measurement of dynamic fluid shear stress on the aortic surface of the aortic valve leaflet. Biomechanics and Modeling in Mechanobiology. 11 (1), 171-182 (2012).
- Toninato, R., Salmon, J., Susin, F. M., Ducci, A., Burriesci, G. Physiological vortices in the sinuses of Valsalva: an in vitro approach for bio-prosthetic valves. Journal of Biomechanics. 49 (13), 2635-2643 (2016).
- Raghav, V., Midha, P., Sharma, R., Babaliaros, V., Yoganathan, A. Transcatheter aortic valve thrombosis: a review of potential mechanisms. Journal of the Royal Society Interface. 18 (184), 20210599 (2021).
- Ramanathan, T., Skinner, H. Coronary blood flow. Continuing Education in Anaesthesia, Critical Care & Pain. 5 (2), 61-64 (2005).
- Nobach, H., Bodenschatz, E. Limitations of accuracy in PIV due to individual variations of particle image intensities. Experiments in Fluids. 47 (1), 27-38 (2009).
- Gülan, U., et al. Performance analysis of the transcatheter aortic valve implantation on blood flow hemodynamics: An optical imaging-based in vitro study. Artificial Organs. 43 (10), 282-293 (2019).

