The Development of Lyophilized Loop-mediated Isothermal Amplification Reagents for the Detection of Coxiella burnetii
Summary
We described here a simple loop-mediated isothermal amplification (LAMP) method using lyophilized reagents for the detection of C. burnetii in patient samples.
Abstract
Coxiella burnetii, the agent causing Q fever, is an obligate intracellular bacterium. PCR based diagnostic assays have been developed for detecting C. burnetii DNA in cell cultures and clinical samples. PCR requires specialized equipment and extensive end user training, and therefore, it is not suitable for routine work especially in a resource-constrained area. We have developed a loop-mediated isothermal amplification (LAMP) assay to detect the presence of C. burnetii in patient samples. This method is performed at a single temperature around 60 °C in a water bath or heating block. The sensitivity of this LAMP assay is very similar to PCR with a detection limit of about 25 copies per reaction. This report describes the preparation of the reaction using lyophilized reagents and visualization of results using hydroxynaphthol blue (HNB) or a UV lamp with fluorescent intercalating dye in the reaction. The LAMP reagents were lyophilized and stored at room temperature (RT) for one month without loss of detection sensitivity. This LAMP assay is particularly robust because the reaction mixture preparation does not involve complex steps. This method is ideal for use in resource-limited settings where Q fever is endemic.
Introduction
The small Gram-negative bacterium Coxiella burnetii is the causative agent of Q fever, which is a worldwide zoonosis. Due to Q fever's worldwide distribution and the high infectivity of C. burnetii, US military and civilian personnel deployed overseas are at risk of being infected in the endemic areas.
Q fever manifests in two forms: acute and chronic infections. Acute Q-fever presents itself with flu-like symptoms, hepatitis, or pneumonia, and is usually a self-limiting disease with a low mortality rate. Chronic Q-fever, while less prevalent, often results in endocarditis, which has a much higher mortality rate if left untreated1,2. Therefore, early diagnosis to guide an appropriate treatment is critical for patient care. Polymerase chain reaction (PCR) and quantitative real time PCR (qPCR) assays have been developed for detecting C. burnetii DNA in cell cultures and clinical samples3-5. Both PCR and qPCR are costly and often not readily available in resource-constrained areas for routine work.
Originally described by Notomi6, loop-mediated isothermal amplification (LAMP) offers an alternative DNA amplification method. LAMP uses Bst DNA polymerase for strand displacement DNA synthesis along with specially designed primer sets that recognize at least six independent regions of the target gene. The most significant advantage of LAMP is that amplification occurs under isothermal conditions. Therefore, only a water bath, heating block or an incubator is required. This method has been used to detect several rickettsial pathogens7-9. Visualization of amplified DNA products by gel electrophoresis is the most accurate method which can differentiate true positives from false positives due to nonspecific amplification. However the procedures involved in gel electrophoresis are not practical for resource-limited areas. Several alternative methods were developed to detect the reaction products. These alternative, such as turbidity derived from magnesium pyrophosphate formation10 or using a fluorescent intercalating dye to be visualized under UV light11,12 are more favorable than running a gel. The LAMP reagents were stable for one month when stored at 25 °C and 37 °C, which are ambient temperatures in tropical and sub-tropical countries where Q fever is endemic13.
A LAMP assay was developed in our laboratory to detect the presence of C. burnetii in plasma samples14. Here we describe a simple protocol for the preparation of the LAMP reaction mixture from the lyophilized reagents. The lyophilized reagents are stable for one month when stored at RT. When combined with an easy visualization method, this is an ideal method to use for detecting C. burnetii in a resource-limited setting.
Protocol
1. Prepare Plasmid DNA Dilutions as Standard for LAMP Reaction
- Use a spectrophotometer to measure the optical density (O.D.) at 260 nm to determine the plasmid (containing target gene IS1111a of C. burnetii RSA 493) DNA concentration. An O.D.260 of 1 equates to 50 µg/µl of DNA.
- Convert the amount of plasmid DNA into the copy number. Since the size of the plasmid is 6,330 bp, the molecular weight of this plasmid is 4.1 x 106 g (6,330 bp x 649 g/bp). The DNA concentration of the plasmid is 34.2 ng/µl (as determined from step 1.1). 1 µl of this DNA sample contains 34.2 ng of plasmid DNA, equating to 5 x 109 copies (34.2 x 10-9 g / 4.1 x 106 g x 6.02 x 1023) of DNA.
- Add 10 µl of plasmid DNA (5 x 109 copies/µl) to 90 µl of water for a 10-fold dilution to make a DNA sample of 5 x 108 copies/µl.
- Repeat step 1.3 to prepare DNA samples of 5 x 107, 5 x 106, 5 x 105, 5 x 104, 5 x 103, 5 x 102, 5 x 101, and 5 x 100 copies/µl .
2. Prepare DNA Template from Samples for LAMP Reaction
- Perform DNA extraction from human plasma samples using a commercial DNA mini kit according to manufacturer's protocol. Use a total of 200 µl sample for extraction and elute extracted DNA in a 20 µl volume.
3. Prepare 2x LAMP Reaction Buffer
- Mix 200 µl of 10x Pol Buffer, 320 µl of 5 M trimethylglycine, 12 µl of 1 M MgSO4, 280 µl of dNTP mixture (10 mM each) and 188 µl of water to make 1 ml of 2x LAMP buffer. Mix by pulse-vortexing for 10 sec.
4. Perform Standard LAMP Reaction
- Mix 12.5 µl of 2x LAMP buffer (as prepared in step 3; 40 mM Tris-HCl (pH 8.8), 20 mM KCl, 16 mM MgSO4, 20 mM (NH4)2SO4, 0.2% Triton X-100, 1.6 M trimethylglycine, 1.4 mM dNTP mixture), 1.2 µl of primer mix, 1 µl of Bst DNA polymerase (8 U/µl), and 5.3 µl of water to make reaction mixture (20 µl) in a 0.2 ml PCR tube.
- Add 5 µl of DNA (from step 1 or 2) to the 20 µl reaction mixture and mix well.
- Close tube and incubate at 60 °C for 60 min in a water bath or heating block. This is the optimal reaction temperature determined previously.
- Add 5 µl of 10x gel loading buffer to terminate the reaction.
- Load 5 µl of reaction products to a 2% agarose gel stained with intercalating nucleic acid stain.
- Run gel at 100 V for 35 min in 1x TBE buffer.
- Visualize the results by UV light.
5. Perform LAMP Reaction with Reconstituted Reagents
- Mix 125 µl of 10x Pol Buffer, 200 µl of 5 M trimethylglycine, 7.5 µl of 1 M MgSO4, 667.5 µl of water to make 1 ml of reconstitution buffer. Mix by pulse-vortexing for 10 sec.
- Remove tubes which contain the lyophilized reagents from the sealed aluminum foil bag. Do not use the tubes if the aluminum foil bag is not sealed or if it is damaged.
- Add 20 µl of reconstitution buffer into each tube to re-suspend lyophilized reagents.
- Mix by pipetting buffer up and down 5 times. Take a look to make sure the lyophilized reagents are completely re-suspended. The white powder should disappear in the tube.
- Add 5 µl of DNA template (from step 1 or 2) to the reconstituted reagents and mix well.
- Close tube and incubate at 60 °C for 60 min in a water bath or heating block.
- Add 5 µl of 10x gel loading buffer to terminate the reaction.
- Load 5 µl of reaction products to a 2% agarose gel stained with intercalating nucleic acid stain.
- Run gel at 100 V for 35 min in 1x TBE buffer.
- Visualize the results by UV light.
6. Perform LAMP Reaction with Reconstitution Buffer Containing HNB or Fluorescent Intercalating Dye
- Mix 125 µl of 10x Pol Buffer, 200 µl of 5 M trimethylglycine, 7.5 µl of 1 M MgSO4, 7.5 µl of 20 mM HNB (or 12.5 µl of 100x fluorescent intercalating dye) and 660 µl (or 655 µl) of water to make 1 ml of reconstitution buffer. Mix by pulse-vortexing for 10 sec.
- Use the reconstituted buffer prepared in section 6 to repeat the steps 5.2 – 5.6.
- Visualize the results by the naked eye (reaction containing HNB) or a UV light (reaction containing fluorescent intercalating dye).
7. Perform Real-time LAMP Reaction with Tube Scanner
- Add 5 µl DNA to the reconstituted reagents containing fluorescent intercalating dye, close tube and insert it to the tube scanner.
- Set incubation temperature at 60 °C. Measure the fluorescence at 520 nm for 60 min.
Representative Results
The lyophilized LAMP reagents inside the 0.2 ml tube contains Bst DNA polymerase, primers, and dNTPs. 20 µl of reconstitution buffer is used to re-suspend the lyophilized reagents. Figure 1 shows the LAMP reaction results on agarose gels with freshly prepared reagents and lyophilized reagents. The lyophilized reagent does not reduce its activity. LAMP reactions prepared by both reagents can detect 25 copies of DNA template. Figure 2 shows the detection of the reaction products with HNB or fluorescent intercalating dye present in the reaction. Addition of HNB to the reaction produces a visual color change from purple to blue with 25, 50 and 100 copies of DNA template present in the reactions. The inclusion of fluorescent intercalating dye in the reaction shows a strong fluorescence signal with UV light when 25, 50, and 100 copies of DNA templates are present. A tube scanner was used in this study for real-time detection. This machine can perform 8 reactions simultaneously. Figure 3 shows using the tube scanner to monitor the fluorescence signals in real-time with fluorescent intercalating dye presence. The fluorescence signals are above baseline after 14, 18, 21, and 23 min with 106, 104, 103, and 100 copies of DNA template in the reactions.
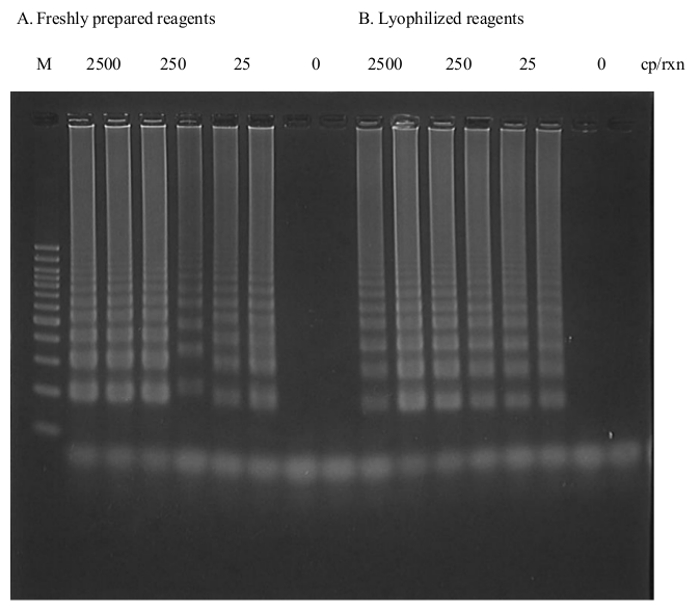
Figure 1. LAMP Results on Agarose Gel with Freshly Prepared Reagents (A) and Lyophilized Reagents (B). Reaction mixtures were incubated at 60 °C for 60 min. (A) Lane 1, 100 bp ladder; Lane 2 – 3, 4 – 5, 6 – 7 and 8 – 9 are reactions with 2.5 x 103, 2.5 x 102, 2.5 x 10, and no copies of plasmid DNA. (B) Lane 10 – 11, 12 – 13, 14 – 15, and 16 – 17 are reactions with 2.5 x 103, 2.5 x 102, 2.5 x 10, and 0 copies of plasmid DNA. Please click here to view a larger version of this figure.
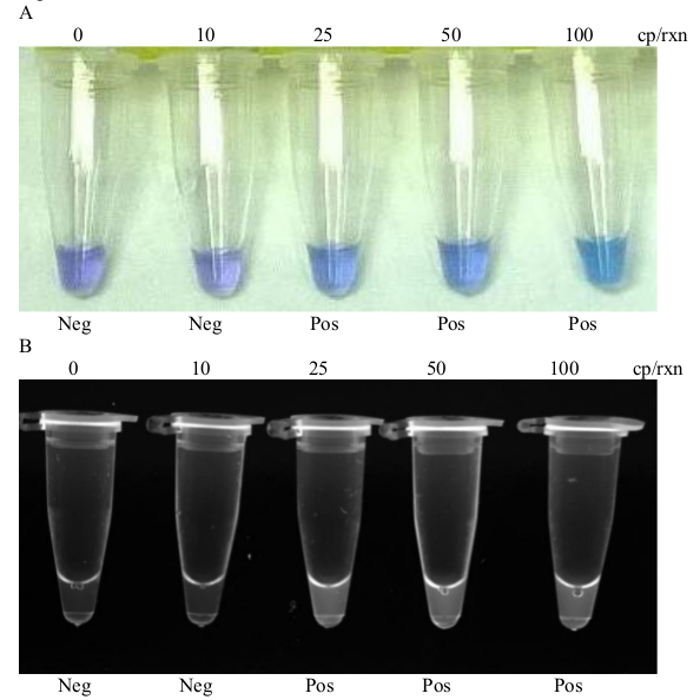
Figure 2. Methods to Detect LAMP Products. HNB (A) or fluorescent intercalating dye (B) were used to detect LAMP products. Reactions were carried out at 60 °C for 60 min. Lane 1 to 5, reactions with 0, 10, 25, 50, and 100 copies of plasmid. Please click here to view a larger version of this figure.
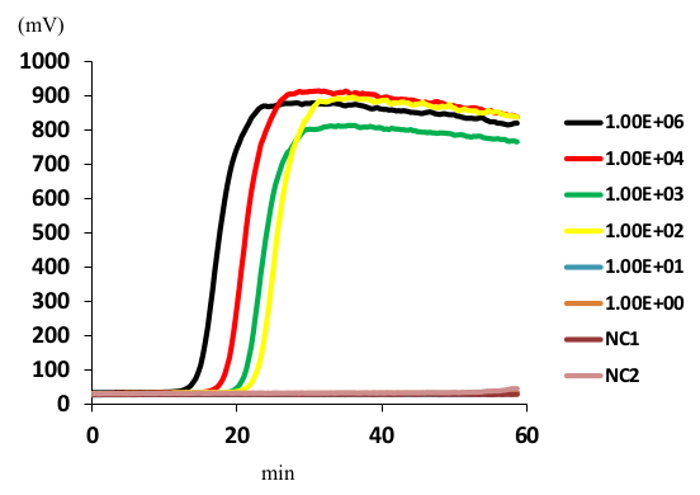
Figure 3. Real-time Detection of LAMP Products. Reactions were carried out at 60 °C for 60 min. Reactions with 106 (black), 104 (red), 103 (green), 100 (yellow), 10 (blue), 1 (orange) and 0 (brown and light brown) copies of plasmid. Three detections were performed independently. They were highly reproducible. Please click here to view a larger version of this figure.
Discussion
Previously, we developed a sensitive and specific LAMP assay targeting the insertion element IS1111a14. The IS1111 element was selected because it is highly conserved among the different strains of C. burnetii and its high number of copies (7 to 110) in the bacteria (Klee 2006). Our results showed that LAMP can detect about 25 copies of the IS1111 element, which may correlate to as little as one chromosomal copy of Coxiella DNA. In this study, Bst DNA polymerase, LAMP primers, and dNTPs were lyophilized and packaged in a zipped aluminum foil bag. The sensitivity of these lyophilized reagents remains at 25 copies; similar to the freshly prepared reagents for at least one month when stored at RT. It is very important to make sure the aluminum foil bag is properly sealed before opening it. Do not use the tubes if the aluminum foil bag is not sealed or if it is damaged. This may cause the rehydration of the lyophilized reagents which leads to the loss of its reactivity. The other critical step is the re-suspension of the lyophilized reagents with reconstitution buffer. The LAMP reaction will not work properly with reagents that are not fully re-suspended. Because of the high salt concentrations of the reaction buffer and high viscosity of the trimethylglycine solution, they cannot be successfully lyophilized with Bst DNA polymerase, LAMP primers, and dNTPs. A special step is required to prepare the reconstitution buffer with those components. Potentially the LAMP reaction can be tested at low salt concentrations with low or no trimethylglycine. If there is a reaction condition that has the same detection sensitivity but with low salt and low trimethylglycine concentration, the lyophilized reagent only needs to be reconstituted with water. This will further simplify the reaction steps.
Recently, Wang et al.15 compared twelve in-house LAMP assays with the commercialized isothermal Master Mix kit and found the in-house assays have false-positive results. In our laboratory, we have developed several LAMP assays for the detection of different bacteria and have never found false-positive results in these in-house assays. Furthermore, in the beginning stages of the development of the LAMP method, the assays were tested with both in-house prepared master mix and commercialized master mix and no difference was observed in the assays' sensitivity and specificity.
Our study also presents several methods that not only can detect the LAMP products without opening the reaction tubes to decrease the likelihood of laboratory cross contamination but also have a shorter process time to read results compare to gel electrophoresis method. The advantage of using these detection methods will greatly enhance our ability to quickly perform the assay and diagnose an individual with C. burnetii infection in resource-limited areas. This will allow rapid and appropriate treatment of acute Q fever and lessen the potential of future chronic infection.
Unlike PCR-based methods where a thermocycler is needed, a heating block, water bath or incubator maintaining a constant temperature around 60 °C is all that is required for the LAMP assay. This makes the assay particularly suitable in resource-limited setting. Unlike the original LAMP assay, Bst DNA polymerase, LAMP primers, and dNTPs need to be stored at -20 °C. These lyophilized reagents can be stored at room temperature which makes it even more useful for a resource-limited setting where Q fever is endemic. The long term stability study of the lyophilized reagents at 4 °C, 25 °C, and 37 °C is currently ongoing. In the future, we would like to demonstrate that this LAMP assay using lyophilized reagents can detect C. burnetii with sensitivity similar to that of PCR in a remote setting.
Disclosures
The authors have nothing to disclose.
Acknowledgements
This research was supported by Naval Medical Research Center, research work unit 6000.RAD1.J.A0310. The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, or the U.S. Government. Wei-Mei Ching is an employee of the U.S. Government. This work was prepared as part of her official duties. Title 17 U.S.C. §105 provides that 'Copyright protection under this title is not available for any work of the United States Government.' Title 17 U.S.C. §101 defines a U.S. Government work as a work prepared by military service member or employee of the U.S. Government as part of that person's official duties.
Materials
| LAMP primers | Eurofins MWG operon | 10 nmol, salt free | Sequence designed by customer |
| Bst DNA polymerase | New England Biolabs | M0275L | 8 units/ml |
| 10X Thermo pol buffer | New England Biolabs | B9004S | |
| dNTP mixture | New England Biolabs | N0447L | 10 mM each |
| Betaine | Sigma-Aldrich | B0300 | 5 M, Trimethylglycine |
| Magnesium Sulfate | Sigma-Aldrich | M3409-1ML | 1 M |
| 10X Bluejuice | Invitrogen | 10816-015 | gel loading buffer |
| SYBR green | Invitrogen | S7585 | 10,000X, visualize products in tubes |
| GelRed | Phenix Research Products | RGB-4103 | 10,000X, visualize products in gels |
| Lyophilized reagents | Gene Reach | ||
| Hydroxynaphthol blue | Fluka | 33936-10G | |
| ESEQuant tube scanner | Qiagen | real-time detection |
References
- Anderson, A., et al. Diagnosis and management of Q fever United States, 2013: recommendations from CDC and the Q Fever Working Group. MMWR Recomm. Rep. 62 (3), 1-30 (2013).
- Rolain, J. M., Boulos, A., Mallet, M. N., Raoult, D. Correlation between ratio of serum doxycycline concentration to MIC and rapid decline of antibody levels during treatment of Q fever endocarditis. Antimicrob. Agents and Chemother. 49 (7), 2673-2676 (2005).
- Fournier, P. E., Raoult, D. Comparison of PCR and serology assays for early diagnosis of acute Q fever. J. Clin. Microbiol. 41 (11), 5094-5098 (2003).
- Schneeberger, P. M., et al. Real-time PCR with serum samples is indispensable for early diagnosis of acute Q fever. Clin. Vaccine Immunol. 17 (2), 286-290 (2010).
- Turra, M., Chang, G., Whybrow, D., Higgins, G., Qiao, M. Diagnosis of acute Q fever by PCR on sera during a recent outbreak in rural South Australia. Ann. N Y Acad. Sci. 1078, 566-569 (2006).
- Notomi, T., et al. Loop-mediated isothermal amplification of DNA. Nucleic Acids Res. 28 (12), (2000).
- Paris, D. H., Blacksell, S. D., Newton, P. N., Day, N. P. Simple, rapid and sensitive detection of Orientia tsutsugamushi. by loo-isothermal DNA amplification. Trans. R. Soc. Trop. Med. Hyg. 102 (12), 1239-1246 (2008).
- Huber, E., et al. Loop-mediated isothermal amplification assay targeting the 47-kDa gene of Orientia tsutsugamushi.: A rapid and sensitive alternative to real-time PCR. J. Med. Microb. Diagn. 1 (112), (2012).
- Pan, L., Zhang, L., Wang, G., Liu, Q. Rapid, sensitive detection of the ompB gene of spotted fever group rickettsiae by loop-mediated isothermal amplification. BMC Infect. Dis. 12 (254), (2012).
- Mori, Y., Nagamine, K., Tomita, N., Notomi, T. Detection of loop-mediated isothermal amplification reaction by turbidity derived from magnesium pyrophosphate formation. Biochem. Biophys. Res. Commun. 289 (1), 150-154 (2001).
- Qiao, Y. M., et al. Loop-mediated isothermal amplification for rapid detection of Bacillus anthracis.spores. Biotechnol. Lett. 29 (12), 1939-1946 (2007).
- Tomita, N., Mori, Y., Kanda, H., Notomi, T. Loop-mediated isothermal amplification (LAMP) of gene sequences and simple visual detection of products. Nat. Protoc. 3 (5), 877-882 (2008).
- Thekisoe, O. M., et al. Stability of Loop-Mediated Isothermal Amplification (LAMP) reagents and its amplification efficiency on crude trypanosome DNA templates. J. Vet. Med. Sci. 71 (4), 471-475 (2009).
- Chen, H. W., Ching, W. M. Development of loop-mediated isothermal amplification assays for rapid and easy detection of Coxiella Burnetii. J. Microbiol Methods. 107, 176-181 (2014).
- Wang, D., et al. A Comparison of In-House Real-Time LAMP Assays with a Commercial Assay for the Detection of Pathogenic Bacteria. Molecules. 20 (6), 9487-9495 (2015).

