Use of a Foot-Induced Digitally Controlled Resistance Device for Functional Magnetic Resonance Imaging Evaluation in Patients with Foot Paresis
Summary
Chronic stroke patients’ insured rehabilitation is generally time limited. Imaging-based study of brain activity from walking-related motor tasks can lead to establishing biomarkers to measure improved outcomes and justify extending tailored therapy. A novel, magnetic resonance-compatible, variable-resistance foot motion device and a protocol for use during functional magnetic resonance imaging are presented.
Abstract
Neurological deficits from a stroke can result in long-term motor disabilities, including those that affect walking gait. However, extensive rehabilitation following stroke is typically time limited. Establishing predictive biomarkers to identify patients who may meaningfully benefit from additional physical therapy and demonstrate improvement is important to improve the patients' quality of life. Detection of neuroplastic remodeling of the affected region and changes in the activity patterns excited while performing suitable motor tasks could have valuable implications for chronic stroke recovery. This protocol describes the use of a digitally controlled, magnetic resonance-compatible foot-induced robotic device (MR_COFID) to present a personalized foot-motor task involving trajectory following to stroke-affected subjects with gait impairment during functional magnetic resonance imaging (fMRI). In the task, foot flexion is performed against bi-directional resistive forces, which are tuned to the subject's strength in both the dorsiflexion and plantar flexion directions, while following a visual metronome. fMRI non-invasively uses endogenous deoxyhemoglobin as a contrast agent to detect blood oxygenation level-dependent (BOLD) changes between the active and resting periods during testing. Repeated periodic testing can detect therapy-related changes in excitation patterns during task performance. The use of this technique provides data to identify and measure biomarkers that may indicate the likelihood of an individual benefitting from rehabilitation beyond that which is currently provided to stroke patients.
Introduction
The use of quantitative metrics derived from functional and structural brain imaging may be more useful and effective for tracking progress and predicting the outcomes of stroke therapy than assessing clinical scores, and these quantitative metrics could be useful in designing and improving individualized therapy plans1,2. Developing effective, personalized strategies that relate motor training to a measurable reorganization of neural activity and/or improvements in motor function remains challenging. In prior work, insights have been developed regarding how functional neuroimaging methods and brain mapping in patients affected by chronic stroke can show such changes3,4,5,6,7,8. The examination of brain function in relation to hand-grip performance (which is key to patient self-sufficiency and quality of life) has led to the expectation that this technique could also be applied to gait-related foot motion control through the evaluation of the corresponding topographic patterns of neural activity and the recovery of function. It has been posited that the incorporation of MRI-based functional maps of injury may help to characterize neurological deficits more precisely than clinical evaluations9 and that using robotic devices is more effective for brain recovery than conventional paradigms10. Functional maps can provide insight into which parts of a system are functioning, thereby providing information that is not evident from clinical observations11. Success in foot motion and strength rehabilitation with MRI for stroke patients will facilitate the development of personalized treatment strategies based on MRI metrics for a broader population with other neurological conditions.
In the work presented here, the use of the MR-compatible foot-induced robotic device (MR_COFID or foot device) during fMRI scanning is described to examine the effects of post-stroke motor skill training on brain function. The motivation for the development of this controlled-resistance foot device was the critical unmet need for foot-motion rehabilitation in stroke patients. Constructing a system suitable both for home- and office-based training and for the MR-based monitoring of the responses to training activities creates a unified approach that addresses prior limitations in terms of both training and evaluation.
The MR_COFID (Figure 1A) is an adaptation of the prior magnetic resonance-compatible hand-induced robotic device (MR_CHIRODv2)8,12, which employed an electro-rheological fluid (ERF) actuator to provide dynamically controlled, resistive force in response to a subject grasping and squeezing its handle mechanism. The ERF actuator (Figure 1B) is a fluid-filled, bi-directional piston in which the ERF on one side of the piston is forced by piston motion to flow between a pair of electrodes in a channel, which returns the fluid to the other side of the piston. When a high voltage (HV) is applied to the electrodes, particles in the non-conductive, silicone oil align and mechanically bind to each other, thus increasing the viscosity of the fluid and the device's resistance to motion. In the hand-grip device, the actuator is directly coupled to the grip handles, to a load cell to measure the applied force, and to an optical encoder to measure the displacement of the handle. The new foot device transforms the linear action of the grip device into the angular displacement of the foot in dorsiflexion and plantar flexion using a crank slider mechanism (Figure 1C). The resistance force from the ERF actuator is converted nearly in proportion to the resistance torque about the ankle joint. The pedal's crank motion is symmetrical about the vector perpendicular to the main actuator axis, thus taking advantage of the approximation that the crank angle and its sine are nearly equal for small angles. As only resistive forces can be exerted by ERF, the system is inherently safe; the actuator cannot actively push or pull the foot, and the force falls to zero when the subject stops moving. The maximum plantar flexion of the foot device is 35° and the maximum dorsiflexion is 18°. These values are within the range of motion of the foot during normal gait and non-weight-bearing conditions13,14, are nearly the same as the values used in other research15, and were found during preliminary testing to meet or exceed the stroke subjects' ranges of motion on their injury-affected side and to allow for the maximization of the available resistive forces via the linear-angular transmission mechanism. The original grip device and the additional foot motion mechanism were constructed from non-ferrous materials (plastic, aluminum, brass) for MR safety.
The ERF actuator employs variable electrical, rather than magnetic, fields to alter the fluid viscosity and is, thus, unaffected by the magnetic fields of the MR scanner. The ERF actuator is enclosed within a cylindrical copper shell that is connected to the shield conductor of the coaxial HV cable; this cable is, in turn, grounded to the penetration panel of the MR scanner's Faraday cage. This prevents potential radio frequency noise from the variable voltage applied to the actuator from affecting the scanner and prevents the variable magnetic fields of the scanner from inducing currents in the cables, which could change the ERF viscosity. The HV cable continues outside of the penetration panel to the HV amplifier. Coaxial MHV (miniature high voltage) connectors are used, which provide additional safety when carrying voltages up to 4 kV (Figure 2).
The separate cables from the optical encoder and the load cell have shields that are also grounded to the penetration panel, thus preventing their signals (particularly the digital signals from the encoder channels) from affecting either the scanner or the small voltage load cell output. The shielded and grounded cables outside the penetration panel carry signals to the data acquisition (DAQ) module. The output of the load cell, which uses a temperature-compensated Wheatstone bridge, is amplified by an instrumentation amplifier attached to the analog input terminals of the DAQ, providing a 1,000x amplification factor.
The DAQ module runs firmware using the Lua scripting language (Supplemental Coding File 1). The script loaded onto the DAQ module runs at a loop rate of 500 Hz, and the module reads the encoder and amplified load cell signal, converts the sensor readings to length and force values, and stores them in memory registers for access and logging by an m-file user interface (UI; Figure 3) on the host laptop (Supplemental Coding File 2). The host laptop sends target force values for dorsiflexion and plantar flexion, closed-loop controller parameters, and encoder-reset commands to additional memory registers on the DAQ module when needed. The DAQ script runs a control loop that detects the pedal motion direction to determine which force to exert: dorsiflexion or plantar flexion. It then calculates an output voltage proportional to the difference between the measured and target force values, bounded by 0 V and 4 V, which is the allowable input range of the HV amplifier. The ERF responds to the magnitude of the applied electric field; reversing the voltage does not reduce the viscosity below that of the unenergized (no electric field) fluid, so the DAQ output is limited to a minimum of 0 V. The DAQ quantizes (12 bit resolution) and samples (500 Hz) the analog voltages, resulting in a stair-step output to the HV amplifier that can cause high-frequency components in the HV output due to the rapid changes at each step. The HV amplifier has small and large signal bandwidths of 35 kHz and 8 kHz, respectively, so to reduce the possibility that RF noise detectable by the scanner is generated, the DAQ output uses a first-order RC filter with a −3 dB frequency at approximately 900 Hz, so higher frequencies are almost eliminated. In addition, the foot device is positioned outside the bore of the scanner near the foot of the bed, further minimizing any interaction between the device sensors, the actuator, and the scanner. The amplifier, with a gain of 1,000 V/V and a peak output of 4 kV, generates fields across the ERF gap up to 4 kV/mm; although ERF fluid's breakdown voltage is not reported by the vendor, viscosity and other parameters are described up to this level. The ERF cylinder can exert slightly more than 200 N of force when fully energized and being moved at the target speed. The moment arm length where the connecting rod joins the pedal is 56 mm, resulting in a maximum torque of approximately 11.2 Nm. This is more than sufficient for subjects with foot paresis; however, it can be overpowered by strong, healthy subjects. The hardware components are listed in the Table of Materials.
The use of the foot device builds on the training and testing paradigms developed with earlier hand-grip devices3,4,5,6,7,8,16 and other work11,17,18. At the time of publication, this device was used with chronic stroke subjects with foot-related deficits to study therapy-driven neuroplastic changes via both MR imaging and quantitative performance evaluations.
As described in the protocol below, the subjects undergoing scanning lie supine on the scanner bed, and their heads are immobilized within the scanner's head coil and positioned at the isocenter of the scanner. The foot device is positioned and locked in place such that the subject's tested leg is straight, and their foot is strapped into the device's corresponding pedal. In this manner, bending at the ankle does not cause pushing or pulling against the device, which could shift the head's position within the coil. A mirror frame is positioned in front of the subject's eyes, allowing them to view a projection screen that displays instructions and visual cues for the motor task.
During the task, the subject views either a "+" sign during rest periods or a visual metronome during testing, in which one circle moves up and down on the screen (target), and another circle is displayed that moves under the control of the device's foot pedal position (cursor; Figure 4). Subjects are asked to closely follow the motion of the target. The target speed is determined so that the unenergized viscous reaction force of the device (the viscous forces increase with increasing speed) is low enough for any subject to overcome it, with increased forces applied under computer control.
Robotics are easily deployed, applicable across various motor impairments, have high measurement reliability, and have the capacity to deliver high-intensity training10. This ERF-based device delivers digitally controlled resistance force to the subject, and this device is MR-safe when coupled with non-ferrous/non-magnetic components, as well as MR-compatible due to the use of grounded and shielded electronics12. It has advantages relative to related devices in that it is portable and relatively simple to use, meaning it can be used both in clinical environments and at home, where regular therapy can be performed without the costs related to travel or the clinical facility. The device can produce computer-controlled, time-varying resistance in plantar flexion and dorsiflexion to facilitate the creation of patient-specific rehabilitation routines and, thus, addresses a gap in the field of commercially available rehabilitation devices.
Other research devices do exist but were unsuitable for the present research for various reasons. Some devices are static, measuring forces applied isometrically19 rather than over the subject's range of motion (RoM). Elastic-based devices apply increasing force with increasing displacement, rather than constant resistance over the RoM, and must be manually adjusted to change the force levels20,21,22. The use of fixed weights and gravitational loading15,23 does not allow for the computerized control of the loads or different loads for plantar flexion and dorsiflexion. Pneumatic devices24,25,26 allow for force variations between tests and a constant force across the RoM; however, the valves would need to be placed at a distance from the scanner, so generally, this device would not be able to switch between plantar flexion and dorsiflexion forces quickly when changing the foot direction and would not have the frequency response capabilities of ERF actuators. Electromagnetic motors can be used27 in the scanner environment but only by extending the mechanism far enough to maintain MR safety and compatibility, which limits the portability and increases the risk of accidents should any of the motor components be brought too close to the bore. Hydraulics28 can be bidirectional at different force levels but have challenges similar to the use of electromagnetic motors in that the compressor/driver (typically not MR-compatible) must be distant from the bore, thus limiting portability and frequency response. Hydraulics have been combined with ERF systems29 so that the system can back-drive the end effector (foot or grip device) and provide isometric resistance; however, this capability was not required for the present research and was added at the cost of using non-MR-compatible hydraulic motors.
The foot device provides a combination of features that enable the following: precise and consistent therapeutic foot-control exercises for extended periods; the measurement of the subject's current motor performance capability and adjustment of the task difficulty as rehabilitation proceeds; real-time control and independent adjustment of the applied force in both plantar flexion and dorsiflexion; remote control and adjustment of the resistance force without interruptions for manual adjustment; and MR safety and compatibility.
Protocol
All the experiments were approved by the Institutional Review Board at Massachusetts General Hospital and performed as approved at the Athinoula A. Martinos Center for Biomedical Imaging. Subject consent for the use and sharing of de-identified data was obtained.
NOTE: In the current study, the inclusion criteria were as follows: (1) right or left hemiparesis with residual leg movement from an ischemic/MCA stroke incurred ≥6 months earlier; (2) a Functional Ambulation Category (FAC) score30 of 4-5 (subject ambulates with an assistant to navigate stairs/uneven surfaces or without the help of an assistant); (3) a National Institutes of Health Stroke Scale (NIHSS)31 score of 5-14 (mild/moderate); (4) the ability to stand for 5 min and walk 10 m; (5) aged 18-80 years old. Following initial testing, an additional criterion was included, which involved verifying that the subjects could move the pedal through at least 5° of motion with the paretic foot. Data were collected on demographics, stroke risk factors, the duration of physical/occupational therapy, the length of the hospital stay during the acute stage, medication use, intercurrent infections, and complications.
1. Subject screening and preparation
- During recruitment, meet with the potential subjects, and test their ability to move the device's pedals with their paretic foot.
- Check the fit of each subject's foot in the device's foot pedals. For subjects with smaller feet, test the fit of their feet when wearing sneakers or similar footwear that are MR-safe.
- Subjects who cannot exert sufficient force to move the pedal through at least a 5° range of motion with the device un-energized should be excluded from the study.
- Prior to arrival, instruct the subjects to bring the tested footwear if this was determined to be necessary during the pre-screening. Record the subject information, and obtain informed consent according to the institutional protocol.
- On each testing day, screen the subjects for contraindications as specified by the MR facility policy. Obtain signed waivers in cases of subjects with tattoos with the potential for irritation and/or burning sensations and any other facility-specific waivers.
- Instruct the subject to change into a facility-approved gown/pants and to wait to be called into the scanner room. Store the subject's belongings as per facility policy. If determined to be needed, instruct the subject to put on the footwear.
2. Setup of the controlled-resistance foot device
NOTE: It is recommended that the completion of steps 2.1-2.3 occurs prior to the subject's arrival.
- Setup in the MRI support room
- Place the HV amplifier unit with the attached DAQ module on the floor close to the penetration panel. Plug the AC power cord into the wall outlet, plug the HV coaxial cable into the HV amplifier terminals and into the MHV coaxial plug on the penetration panel, and plug the sensor cable into the corresponding plug on the penetration panel. Turn on the main power switch of the HV amplifier.
- Plug the USB B plug of the USB cable into the DAQ module and the USB A plug of the cable into the USB repeater cable. Lay the USB repeater cable out from the MRI support room to the MRI control room, and fasten the cable to the floor using adhesive tape as necessary to prevent dislodgement by staff or subject ambulation about the facility.
- Activate scanner room projector.
- Setup in the MRI control room
- Place the foot-device host laptop adjacent to the MRI scanner interface, plug in the power supply, and power up the laptop. Start the MATLAB application, and load the user interface (UI) program.
- Plug the MRI scanner button box/trigger signal USB cable, the scanner room projector cable, and the USB repeater cable into the laptop.
- If not previously set up, adjust the laptop monitor settings so that the main window is extended onto the projector screen to the right of the main laptop window. Move the mouse pointer off the right side of the main laptop window, and confirm that it moves into the field of view of the projector screen. Move the mouse pointer back to the main window.
NOTE: The trigger signal and projector cable formats may differ between facilities. Video adapters or similar units may be necessary.
- Setup in the scanner room
- Verify that the scanner table is fully outside of the scanner bore and lowered completely.
- Mount a head coil into its corresponding slot on the scanner table. Remove the top section of the coil, and place it to the side. Cover the scanner table cushions and the lower section of the head coil with a hospital bed sheet.
- Mount the projector screen into the bore at the opposite end from the scanner table.
- Insert two pairs of brass mounting screws into the coil mounting slots toward the foot end of the scanner table, and place the foot device between the screw pairs. Loosely attach plastic retaining brackets to the screws and alignment holes in the base plate of the foot device (Figure 1A).
- Attach the sensor and HV cables to the plugs on the penetration panel. Ensure the cables are not looped around the table or otherwise at risk of pinching or tangling when the table is moved into the scanner bore. Ensure that the sensor and HV cables are extended without loops between the foot device and the penetration panel.
- Start the UI program in the control room (run the m-file script), and verify that communications have been established between the host laptop and the DAQ module by observing the confirmation message in the UI (Figure 3).
- Accept the default force level proportions on the initial UI dialog by clicking on the OK button. Wait for confirmation dialogs to appear and dismiss themselves and for the initial force and displacement live graph window to appear.
- Ensure that, while one staff member moves the pedal of the foot device through its range of motion and another staff member observes the force and displacement traces, the displacement trace moves from −35° to +18° and back and that the force trace shows positive forces for motions in the dorsiflexion direction, negative forces for motions in the plantar flexion direction, and returns to zero at rest. This confirms the function of the sensors, DAQ module, HV amplifier, and ERF actuator (Figure 3A).
- If the signals appear normal, click on 继续 on the live graph window, and then the Shutdown button on the confirmation dialog. If not, check the cable connections and power connections, and redo the setup steps as necessary.
- Subject and foot device alignment
- Escort the subject from the waiting room into the scanner room. Perform metal screening as per facility policy to check for unreported objects or implants. Provide the subject with protective ear plugs.
- Instruct the subject to sit on the table and then to lie supine with their head nestled in the lower section of the head coil. Provide assistance as needed. Fit padding between the subject's head and the walls of the head coil to ensure that head motion is prevented during imaging.
- Instruct the subject to straighten their legs. Move the foot device toward/away from the subject until their heels (or the heels of their shoes) rest in the foot seats of the foot device. Adjust further to align the main pivot of the pedals with the subject's ankles.
- Fasten the foot device in place using the plastic retaining brackets and plastic wing nuts.
- Instruct the subject to remove the foot not being tested from its pedal and rest it slightly proximal from the foot device. Support the non-tested leg with pillows as necessary. Fasten the tested foot into its foot device pedal with hook-and-loop retaining straps, ensuring the ball of the subject's foot (or the front of the subject's shoe) is in contact with the pedal.
NOTE: In the current study, with the non-control (stroke) subjects, the stroke-affected foot was tested first. After the testing of the affected foot was complete, that foot was removed from the pedal, and the non-affected foot was mounted in the corresponding pedal using the same process as in step 2.4.5. - Provide a squeeze-bulb alarm device to the subject, instruct them to squeeze the bulb to test it, and remind the subject that, at any time, they may squeeze the bulb to communicate with the technicians.
- Raise the MR table to full height so the subject can see the projection screen through the mirror assembly.
- Install the upper section of the head coil, and mount the viewing mirror assembly over the head coil. Verify that the subject can see the projector screen clearly in the mirror.
3. Subject strength testing
- Restart the UI. Accept the default force level proportions, or adjust them if required by the study protocol, and click on the OK button as above. When the force/displacement traces have appeared, instruct the subject to move the tested foot as far as possible in the dorsiflexion direction and return to full plantar flexion three times. Verify that the displacement and force traces appear normal as above. This establishes the range of motion for testing, which may be less than that of the full range of the foot device (Figure 3A).
- If the results are acceptable, click on 继续 on the live graph window and Yes – Proceed on the confirmation dialog; click on No-Retry if the subject did not follow the flexion instructions correctly; or click on Go to Shut down if there are other problems, and troubleshoot as necessary.
- When presented with the date/time confirmation dialog, click on Yes – Proceed on the dialog, or click on other options if a different filename or shutdown is desired.
- Instruct the subject to move their tested foot to full plantar flexion, and click on OK on the confirmation dialog. An instruction/metronome window will appear (labeled in Figure 3). Using the mouse, drag this window into the field of view of the projection screen, and click on OK to confirm that this has been completed.
- Verify that the instructions for the subject are displayed on the projector. Verify that the subject's foot remains in full plantar flexion, and click on OK on the corresponding dialog. The UI graph changes to the dynamometer display with indications of the resistance force set points.
- The visual metronome described above appears on the projection screen with a solid, target circle moving up or down on the screen at a constant speed and an open circular cursor controlled by the foot device pedal position. Instruct the subject to move their foot to cause the cursor to follow the motion of the target closely. If the subject can successfully move through their full range of motion while following the target, click on (Fd, Fp) + 10 on the live graph to increase the force set points for both dorsiflexion and plantar flexion (Figure 3B).
- Observe whether the subject continues to track the metronome motion accurately.
- If so, click on (Fd, Fp) + 10 again to increase both the force set points. If dorsiflexion cannot be completed but plantar flexion continues to follow the target motion, click on (Fd, Fp) – 10 once and click on Fp + 10 twice to reduce the dorsiflexion resistance force by one step and increase the plantar resistance by one step.
- If the dorsiflexion force has been set but the subject can no longer track the metronome in plantar-flexion, click on Fp – 10 once, and then click on 继续 in the live graph window. The current force levels are used by the UI program as reference points for the proportionally reduced forces applied during the testing phase.
- If the plantar flexion force set point has reached the maximum setting of the foot device, press 继续 in the live graph, and proceed.
NOTE: Step 3.7.3 generally occurs for control subjects with normal leg strength and for the unaffected limb in stroke subjects due to them exceeding the capabilities of the device, which is designed to focus on the strength in the affected limb. - Record the force set points (shown on the right of the force trace plot) for future reference. Click on Yes – Proceed to continue, No – Test Again to repeat, or Shutdown if there are other problems. Instruct the subject to move the tested foot to full plantar displacement and then to relax.
- Review the use of the squeeze bulb, the scanning sequence, and the task with the subject, and answer any questions the subject may have prior to the initiation of the scans.
- Instruct the subject to close their eyes during this step. Use the scanner's landmarking laser line to locate the head coil/subject's head position. Move the table to center the subject's head within the scanner bore. Have the staff leave the scanner room and close the door.
4. Running the MRI scan session and foot device task
- Perform facility-specific registration of the subject, and load the scan protocol. Notify the subject that the anatomical scan sequence will begin and that they may relax during this portion of the protocol, and instruct them to squeeze the bulb to verify their understanding. Initiate the anatomical scan, and wait for completion.
- As directed by the dialog window provided by the UI, notify the subject that the fMRI and foot-device portion of the study will begin, and instruct them that they should ensure that their foot under testing is in full plantar flexion, that they should return their foot to full plantar flexion when a fixation cross appears on the screen, and that they should follow the visual metronome when it appears. Click on OK on the instruction dialog.
- Follow the instruction that directs the operator to prepare the scanner control computer to initiate the fMRI portion of the protocol. Click on OK in the instruction dialog window, and start the fMRI sequence. The UI program automatically sends the desired force settings to the DAQ module.
NOTE: In the current study, the visual metronome task was performed three times each for the stroke-affected and unaffected limbs at force levels of 60%, 40%, and 20% of the maximum levels set in step 3.7. The force levels are updated automatically for each repetition of the test. - The subject views their instructions displayed on the projector screen. A "+" sign (fixation cross) appears, during which, as previously instructed, the subject rests.
- The visual metronome target is displayed with the solid circle moving up and down at constant speed. As previously instructed, the subject moves their tested foot in dorsiflexion and plantar flexion to cause the open circular cursor to track the target.
NOTE: In the current study, the rest (fixation cross) and active (metronome) phases were of equal length, and the cycle was repeated seven times. During the metronome phase, there were two cycles of dorsiflexion and plantar flexion through the range of motion. These parameters may be adjusted in the UI script for other studies. Each fMRI/metronome phase lasted approximately 5 min 40 s. - Repeat step 4.4 and step 4.5 for a total of seven cycles, after which the fixation cross is displayed and the subject rests.
- Repeat steps 4.2-4.6 for a total of three cycles.
- Enter the MRI scanner room, and switch the foot mounted in the foot device as per step 2.4.5. Repeat protocol section 3 for the second foot.
- Repeat protocol section 4, bypassing step 4.1 and step 4.8 (registration, anatomical scan, switching foot).
- Notify the subject that the DTI portion of the scan will commence and that they may relax during this phase of the study, and instruct them to squeeze the bulb to confirm their understanding. Initiate the DTI scan, and wait for completion.
5. Post-test operations
- Move the table and subject out of the scanner bore, and lower the table. Remove the mirror assembly, the upper head coil section, and the padding about the subject's head. The ear protection may be discarded at this time.
- Assist the subject to a sitting position and to move to the changing area if necessary. The subject may now change back into their regular clothing.
- Talk to the subject, address any post-test questions they may have, arrange the scheduling of future appointments, and complete the stipend payment forms prior to the subject's departure.
- Disassemble and pack the hardware, and unmount the ankle device from the scanner table. Detach the HV and sensor cables from the penetration panel. Detach the button box and monitor cables from the host laptop. Pack the ankle device and supporting hardware into carry cases.
- Perform facility-specific sanitation of the scanner table and relevant work surfaces and equipment.
- Extract the data from temporary folders on the scanner system for offline analysis. Perform log-out procedures.
Representative Results
The results described here relate to the MR compatibility of the foot device, an analysis of typical functional scan results, and notes on the foot device.
The foot device was evaluated for MR safety by the staff of the Athinoula A. Martinos Center and tested for MR compatibility in a 3 T MRI scanner. For phantom tests using a cylinder containing a solution of 1.24 g of NiSO4·6H2O and 2.62 g of NaCl per 1,000 g of H2O, the foot device was attached to the scanner table ~85 cm from the end of the bore, near the 500 mT line, in approximately the position necessary for the pedal pivot to be aligned with a subject's ankle joint with their legs extended. Images of the phantom tests were captured using the same scan sequences used for the subject fMRI imaging (with generalized auto-calibrating partially parallel acquisition [GRAPPA] used for increased spatial resolution and BOLD [blood oxygenation level dependent] sensitivity). These tests were carried out both with the device in place but inactive and with the device active with one of the authors moving the pedals to simulate subject activity and HV amplifier excitation under the control of the DAQ module. Ten images were selected from the scans under each condition.
Regions of interest (ROIs) drawn at the image edge and in the center (Figure 5) were used to calculate the background noise and signal, respectively; the signal means in each location were stable across the runs, as they deviated by <0.2% from the central mean over all 10 acquisitions under each condition. There was no statistical difference (P = 0.1215, two-sample t-test, 10 repetitions/condition) in the ratio between the central and background signals for the phantom test with the inactive foot device (30.24 ± 2.31, dimensionless; Figure 5Aa) and the phantom test with the active foot device (27.94 ± 3.76; Figure 5Ab). This suggests that neither the HV activity nor the sensor signals had any effect on the MR images.
Images acquired with six volunteers who lay in the scanner and performed the task in a similar way to the subjects showed that the foot device did not affect the signal-to-noise ratio (SNR) or the image quality (Figure 5Ba,Bb, without and with the device active, respectively).
Typical activations in the M1 and SMA (supplementary motor area) for a control subject were superimposed onto atlas images to show the t-statistic value related to motion activity relative to the resting state with the ankle device passive (Figure 5Bd) and active (Figure 5Be). The differences in the shape and t-values were affected by differences in the applied force during motion activity and the variation in the brain's normal activity at different time points. The tracking of such images over time during and after training provides data to identify changes in the stroke-affected brain.
The force and displacement sensors were also not sensitive to static or the time-varying magnetic fields of the scanner. Recordings were collected with the foot device in place on the MR table both with the fMRI sequence active and with the foot device in a non-MR laboratory environment, and these recordings were indistinguishable (steady encoder values in both cases, ≤1 bit noise in the force recordings).
Design of the controlled-resistance foot device
The previously reported MR_CHIROD v2 hand-grip device3,4,5,6,7,8 provides the base mechanism for the foot device, which converts the linear grip response of the hand-grip device into the angular pedal motion about the subject's ankle joint via a crank-slider mechanism. The foot device can be mounted to the MRI bed's coil-mounting tracks to provide a solid platform that is position-adjustable to fit the subject's height. The pedals have restraining straps to hold the foot in place during plantar flexion and dorsiflexion. Spacers or footwear offset the subject's foot from the base surface of the pedal and the heel restraint to ensure the ankle's center of rotation is aligned with the pedal's axis. This minimizes the axial leg movement, thus preventing the translation of the motion to the subject's head during the scan and the appearance of brain excitation unrelated to foot motion. The coupled left and right pedals allow the use of the device with patients affected by a stroke on either side of the brain. During testing, the knee on the untested side is bent and supported by pads to keep the untested foot away from the unused pedal. The earlier hand-grip device and the new components of the MR_COFID (foot device) are assembled from non-ferrous metal and plastic components, and the devices use shielded electronics. The device was evaluated for MR safety at the Athinoula A. Martinos Center and tested for MR compatibility, with no issues observed on the phantom imaging. The force and displacement sensors were not sensitive to static or the time-varying magnetic fields of the scanner.
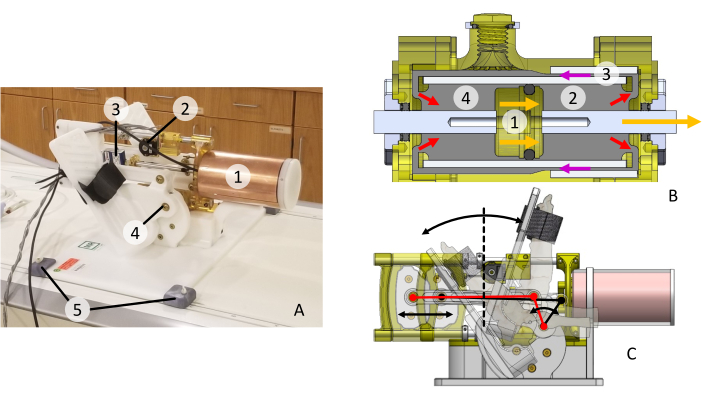
Figure 1: MR-COFID device. (A) 1: Electro-rheological fluid (ERF) cylinder, Faraday cage; 2: optical encoder; 3: load cell; 4: pedal and pivot; 5: retaining brackets. (B) ERF cylinder details: 1: piston and shaft; 2: ER fluid under pressure; 3: HV field gap; 4: ER fluid return. Flow and pressures reverse for the return stroke. (C) Pedal rotation about the ankle axis; transmission linkage for the transformation of the linear ERF force to the angular ankle torque. Please click here to view a larger version of this figure.
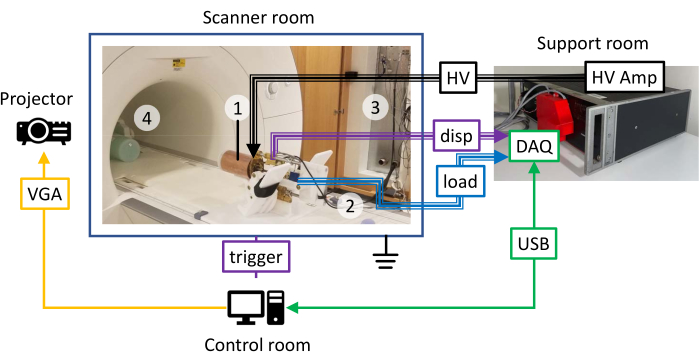
Figure 2: Schematic of the foot device setup in the scanner, control, and support rooms. (1) Faraday cage about the ERF cylinder, (2) shielded cables for the HV supply, and (3) encoder and load cell cables with shields grounded to the penetration panel of the MRI scanner. (4) Cylindrical phantom in the head coil at the scanner isocenter. Please click here to view a larger version of this figure.
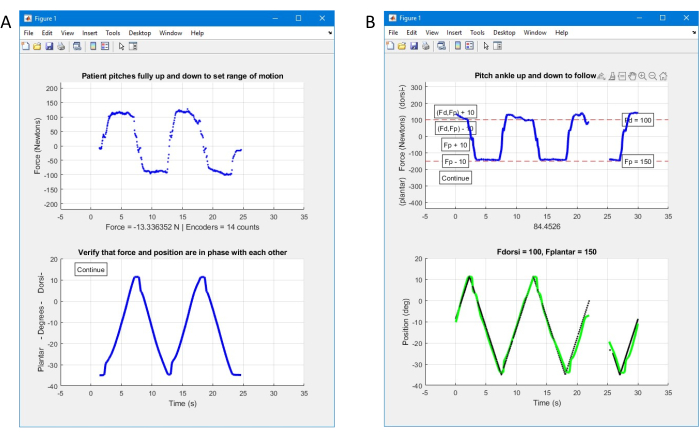
Figure 3: Operator interface. (A) Initial interface to verify the device operation and measure the subject's range of motion. (B) Second interface to establish the subject's strength level in dorsiflexion and plantar flexion. Please click here to view a larger version of this figure.
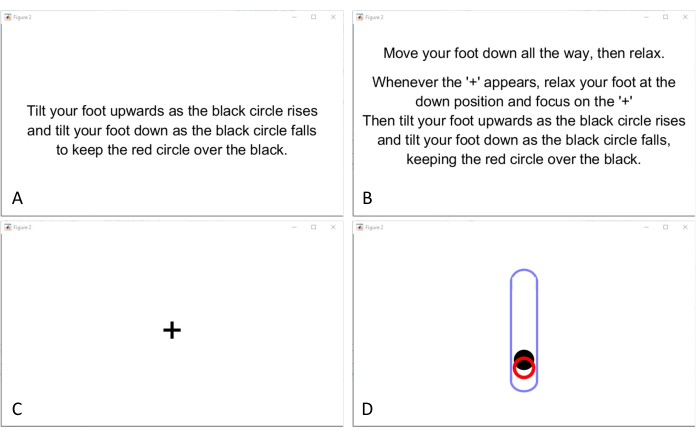
Figure 4: Instructions, fixation cross, and visual metronome displayed to the subject. (A) Instructions displayed during the range-of-motion testing. (B) Instructions prior to each phase of testing during the fMRI scanning. (C) Fixation cross displayed during the resting phases. (D) Visual metronome: a closed circle (target) moves up and down in an oval frame while the subject controls an open circle (cursor) by foot flexion to follow the target. Please click here to view a larger version of this figure.
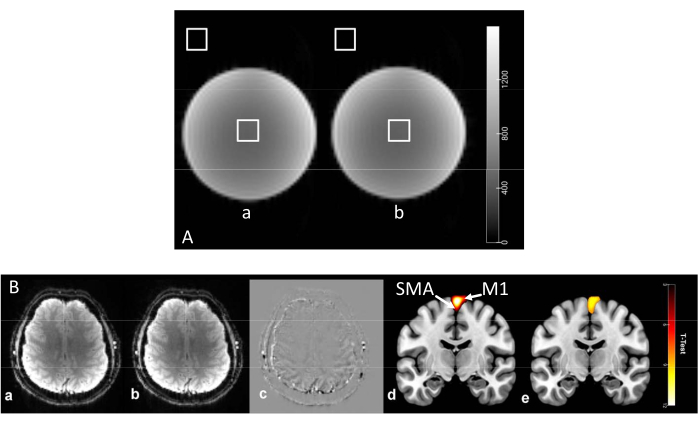
Figure 5: Phantom and subject imaging. (A) Phantom imaging results (a) without and (b) with the foot device active and with the analysis of ROIs within the phantom and at the scan periphery. (B) The operation of the foot robot does not affect the EPI human images or activations. (a) Control without the foot robot in the scanner room. (b) Continuous stepping with the foot robot in the scanner room. (c) Image in (b) minus the image in (a). Activations, including in M1 and SMA (arrows) (d) with the ankle device inactive and (e) energized at 60% of the subject's maximum force. The t-statistic values are shown (color bar), indicating statistically significant excitation of the brain during motion versus excitation when resting, superimposed on atlas images. Please click here to view a larger version of this figure.
Supplemental Coding File 1: Foot for Jove.lua – Lua script firmware uploaded to the DAQ module. Please click here to download this File.
Supplemental Coding File 2: FootDevice_forJove.m – m-file script for the operator interface and the displays for the subjects. The auxiliary function file is provided in Supplemental Coding File 3. Please click here to download this File.
Supplemental Coding File 3: ShutdownLabJackIfAbort.m – m-file auxiliary function used Please click here to download this File.
Discussion
Critical steps
The pre-testing of a subject's ability to generate at least minimal motion of the foot pedal with their paretic foot is crucial. An FAC score of 4 or 5 and the ability to stand for a minimal period reflect a subject's combined ability between their unaffected and paretic limbs and do not reflect the ability to move the paretic foot alone. In the current study, a primary goal was the stimulation of neuroplastic changes about the region of the injury through intensive therapy involving the affected foot, as well as the examination of excitation in the brain. Subjects who cannot generate at least the required level of force and move the pedal will be unable to follow the visual metronome or participate in the associated training paradigm — a gamified therapy session in which a video avatar moves through an undulating cave while avoiding collisions with the walls.
In protocol step 2.4, the subject's foot is fastened into the pedal, and the foot device is positioned after the subject's head has already been stabilized within the head coil. It is important to provide offsetting padding underneath the sole and behind the heel of the foot and/or shoe so that the subject's axis of ankle motion is aligned with the main pivot of the foot device. If this has not been achieved with reasonable accuracy, when the subject flexes their foot up and down, their straightened leg will be pushed and pulled, which will transmit to the subject's head, potentially causing head motion and producing motion artifacts in the fMRI scans.
Limitations
As mentioned above, one of the limitations of this iteration of the device is that there is a minimum resistance force requirement, which prevents subjects with a certain level of severe paresis from operating the device with the single affected limb. Studies and therapy that do not have the single-limb restriction may employ both pedals simultaneously, so assistance can be provided by the unaffected limb. The attempt to exert effort with the affected limb combined with the physical motion enabled by the assisting limb may have benefits, but this effect was outside the scope of the study under which the foot device was initially developed. This limitation may be addressed in a future version of the device, either through the replacement of the current ERF with one that has a lower unenergized viscosity or through redesigning the ERF piston and cylinder. This would increase the dynamic force range and allow more seriously disabled subjects to participate in studies and benefit from therapy with the device's successors.
While the foot device was only used to generate constant force resistance for a given motion in the current study, this is not a limitation of the device. The UI can be reprogrammed to present more complex target-tracking tasks than a simple visual metronome, and/or the resistance force can be continuously or unexpectedly altered, meaning the subject would need to adjust to follow the trajectory. The training game mentioned above makes limited use of more complex paths (under uniform forces) and allows the user to select between up and down branches at various times to help maintain interest during extended training sessions. Future research may establish that more complex stimuli may engender more rapid neuronal remodeling and recovery of function.
Importance
A variety of factors can result in ankle disabilities and negatively affect daily life, including obesity, excessive or limited physical activity, aging, congenital pathologies, injuries, etc. Among them, neurological disabilities caused by strokes or spinal injuries have the most lengthy and challenging rehabilitation. Conventional rehabilitation protocols require an intensive exercise program using resistance bands, foam rollers, and spin boards. These simple devices cannot provide the quantitative information needed for monitoring the rehabilitation process and the customization of therapy. Additionally, they cannot deliver high-dosage and high-intensity therapy consistently. Many foot motion rehabilitation robots have been developed to overcome these limitations with different architectures and design features, including active orthoses, exoskeletons, and platform-based robots32.
Among the existing MR-compatible foot-motion devices, few are rehabilitation-oriented. Some devices provide low-force and high-frequency stimuli on a small surface of the sole of the foot to elicit brain activation rather than to support realistic functional rehabilitation33,34. Others focus on measuring kinematics or force without providing sufficient or predefined resistance19,35,36,37,38,39. A few MRI-compatible rehabilitation-capable systems for providing walking-related resistance are either pneumatic25,40 or use elastic bands21. The present foot device employs a dynamically adjustable type of actuation using electrorheological fluids, which can change their viscosity in response to the applied electric fields. As shown with the precursor hand-grip device, compared to the other actuation technologies, ERFs allow fast, accurate, and strong resistance combined in a compact and portable design41,42,43.
Traditional rehabilitation typically depends on repetitive task-oriented practice at the intensity and duration necessary to reach a plateau in the reacquired ability. Thus, a patient's ability to achieve a positive recovery outcome depends on either the patient's initial intrinsic motivation or the extrinsic/intrinsic motivational abilities of a proficient therapist. Post-stroke clinical monitoring is laborious and imprecise. Insurance coverage for physiotherapy is limited to 150 consecutive days for a first stroke44, and patients who do not respond well to early treatments are generally not expected to improve45. Experience with imaging-monitored, robotically delivered training using the hand-grip device suggests that the physiotherapy window for stroke patients may never close3,5,6,8,46. Imaging-derived metrics may be better than clinical assessments as predictors of potential therapeutic success and may provide information to guide improved and individualized therapy planning. The data obtained suggest that training-acquired motor improvements persist long-term3. This line of work has the potential to bring about a paradigm shift in stroke healthcare and to renew hope for chronic stroke patients.
As neuroplasticity was detected from outcome predictors based on the results with the robotic hand-grip device3,8,46,47,48, the development of a similar MR-compatible foot-induced robotic device (MR_COFID) was proposed. After gripping, foot use is a critical target for rehabilitation because stroke-induced foot dysfunction causes stumbles and falls49. The deliverables of this work may improve chronic stroke outcomes, reduce costs through accelerated rehabilitation and lower burdens of care following rehabilitation, and improve patients' quality of life. Exploring the potential to deliver scalable and effective rehabilitation training via innovative approaches will become increasingly important in the face of predictably shrinking healthcare budgets and unforeseen events such as the current pandemic.
Disclosures
The authors have nothing to disclose.
Acknowledgements
This work was supported by a grant from the National Institute of Neurological Disorders and Stroke (Grant number 1R01NS105875-01A1) of the National Institutes of Health to A. Aria Tzika. This work was performed at the Athinoula A. Martinos Center for Biomedical Imaging. We wish to thank Director Dr. Bruce R. Rosen, M.D., Ph.D. and members of the Martinos Center staff, and Dr. Michael Moskowitz, M.D., for their advice and support. Lastly, we thank Virtumed, LLC for the manufacture of the device.
Materials
| 3T MRI scanner | Siemens Medical Solutions USA, Inc., Malvern, PA | Magnetom Skyra | https://www.siemens-healthineers.com/en-us/magnetic-resonance-imaging/3t-mri-scanner/magnetom-skyra |
| Data acquisition unit (DAQ) | LabJack Corp., Lakewood, CO | T4 | https://labjack.com/news/labjack-t4 |
| High voltage amplifier | Trek, Inc., Lockport, NY | Model 609C-6 | https://www.manualsdir.com/manuals/268654/trek-609e-6-high-voltage-power-amplifier.html?page=2&original=1 |
| Matlab | The Mathworks, Ltd., Natick, MA | n/a | https://www.mathworks.com/ |
| USB repeater cable | Tripp Lite, Chicago, IL | U026-10M | https://assets.tripplite.com/product-pdfs/en/u02610m.pdf |
References
- Stinear, C. M., Ward, N. S. How useful is imaging in predicting outcomes in stroke rehabilitation. International Journal of Stroke. 8 (1), 33-37 (2013).
- Heiss, W. D. Contribution of neuro-imaging for prediction of functional recovery after ischemic stroke. Cerebrovascular Diseases. 44 (5-6), 266-276 (2017).
- Astrakas, L. G., et al. Improving motor function after chronic stroke by interactive gaming with a redesigned MR-compatible hand training device. Experimental and Therapeutic. 21 (3), 245 (2021).
- Astrakas, L. G., Li, S., Elbach, S., Tzika, A. A. The severity of sensorimotor tracts degeneration may predict motor performance in chronic stroke patients, while brain structural network dysfunction may not. Frontiers in Neurology. 13, 813763 (2022).
- Astrakas, L. G., et al. Peak activation shifts in the sensorimotor cortex of chronic stroke patients following robot-assisted rehabilitation therapy. The Open Neuroimaging Journal. 14 (1), 8-15 (2021).
- Mintzopoulos, D., et al. Connectivity alterations assessed by combining fMRI and MR-compatible hand robots in chronic stroke. NeuroImage. 47, T90-T97 (2009).
- Mintzopoulos, D., et al. fMRI of rehabilitation in chronic stroke using MR-compatible robots. Proceedings of the International Society for Magnetic Resonance in Medicine. 16, 3285 (2008).
- Mintzopoulos, D., et al. Functional MRI of rehabilitation in chronic stroke patients using novel MR-compatible hand robots. The Open Neuroimaging Journal. 2 (1), 94-101 (2008).
- Crafton, K. R., Mark, A. N., Cramer, S. C. Improved understanding of cortical injury by incorporating measures of functional anatomy. Brain. 126 (7), 1650-1659 (2003).
- Huang, V. S., Krakauer, J. W. Robotic neurorehabilitation: A computational motor learning perspective. Journal of Neuroengineering and Rehabilitation. 6 (1), 5 (2009).
- Carey, L. M., Seitz, R. J. Functional neuroimaging in stroke recovery and neurorehabilitation: Conceptual issues and perspectives. International Journal of Stroke. 2 (4), 245-264 (2007).
- Khanicheh, A., Mintzopoulos, D., Weinberg, B., Tzika, A. A., Mavroidis, C. MR_CHIROD v.2: Magnetic resonance compatible smart hand rehabilitation device for brain imaging. IEEE Transactions on Neural Systems and Rehabilitation Engineering. 16 (1), 91-98 (2008).
- Baggett, B. D., Young, G. Ankle joint dorsiflexion. Establishment of a normal range. Journal of the American Podiatric Medical Association. 83 (5), 251-254 (1993).
- de Asla, R. J., Wan, L., Rubash, H. E., Li, G. Six DOF in vivo kinematics of the ankle joint complex: Application of a combined dual-orthogonal fluoroscopic and magnetic resonance imaging technique. Journal of Orthopaedic Research. 24 (5), 1019-1027 (2006).
- Hosseini Ghomi, R., Bredella, M. A., Thomas, B. J., Miller, K. K., Torriani, M. Modular MR-compatible lower leg exercise device for whole-body scanners. Skeletal Radiology. 40 (10), 1349-1354 (2011).
- Ottensmeyer, M. P., Li, S., De Novi, G., Tzika, A. A. Functional MRI in conjunction with a novel MRI-compatible hand-induced robotic device to evaluate rehabilitation of individuals recovering from hand grip deficits. Journal of Visualized Experiments. (153), e59420 (2019).
- Carey, J. R., et al. fMRI analysis of ankle movement tracking training in subject with stroke. Experimental Brain Research. 154 (3), 281-290 (2004).
- Dong, Y., Dobkin, B. H., Cen, S. Y., Wu, A. D., Winstein, C. J. Motor cortex activation during treatment may predict therapeutic gains in paretic hand function after stroke. Stroke. 37 (6), 1552-1555 (2006).
- Newton, J. M., et al. Reliable assessment of lower limb motor representations with fMRI: Use of a novel MR compatible device for real-time monitoring of ankle, knee and hip torques. NeuroImage. 43 (1), 136-146 (2008).
- Francescato, M. P., Cettolo, V. Two-pedal ergometer for in vivo MRS studies of human calf muscles. Magnetic Resonance in Medicine. 46 (5), 1000-1005 (2001).
- Doolittle, J. D., et al. Evaluating a novel MR-compatible foot pedal device for unipedal and bipedal motion: Test-retest reliability of evoked brain activity. Human Brain Mapping. 42 (1), 128-138 (2021).
- Naimon, N. D., et al. A low-cost Mr compatible ergometer to assess post-exercise phosphocreatine recovery kinetics. Journal of Magnetism and Magnetic Materials. 30 (3), 281-289 (2017).
- Raymer, G. H., Allman, B. L., Rice, C. L., Marsh, G. D., Thompson, R. T. Characteristics of a MR-compatible ankle exercise ergometer for a 3.0 T head-only MR scanner. Medical Engineering & Physics. 28 (5), 489-494 (2006).
- Meyerspeer, M., Krssak, M., Kemp, G. J., Roden, M., Moser, E. Dynamic interleaved 1H/31P STEAM MRS at 3 Tesla using a pneumatic force-controlled plantar flexion exercise rig. Journal of Magnetism and Magnetic Materials. 18 (5), 257-262 (2005).
- Hollnagel, C., et al. Brain activity during stepping: A novel MRI-compatible device. Journal of Neuroscience Methods. 201 (1), 124-130 (2011).
- Quistorff, B., Nielsen, S., Thomsen, C., Jensen, K. E., Henriksen, O. A simple calf muscle ergometer for use in a standard whole-body MR scanner. Magnetic Resonance in Medicine. 13 (3), 444-449 (1990).
- Ryschon, T. W., et al. A multimode dynamometer for in vivo MRS studies of human skeletal muscle. Journal of Applied Physiology. 79 (6), 2139-2147 (1995).
- Sinha, S., Shin, D. D., Hodgson, J. A., Kinugasa, R., Edgerton, V. R. Computer-controlled, MR-compatible foot-pedal device to study dynamics of the muscle tendon complex under isometric, concentric, and eccentric contractions. Journal of Magnetic Resonance Imaging. 36 (2), 498-504 (2012).
- Unluhisarcikli, O., et al. A robotic hand rehabilitation system with interactive gaming using novel electro-rheological fluid based actuators. Proceedings of 2010 IEEE International Conference on Robotics and Automation. IEEE. , 1846-1851 (2010).
- Mehrholz, J., Wagner, K., Rutte, K., Meiner, D., Pohl, M. Predictive validity and responsiveness of the Functional Ambulation Category in hemiparetic patients after stroke. Archives of Physical Medicine and Rehabilitation. 88 (10), 1314-1319 (2007).
- Lyden, P., et al. Underlying structure of the National Institutes of Health Stroke Scale: Results of a factor analysis. Stroke. 30 (11), 2347-2354 (1999).
- Alvarez-Perez, M. G., Garcia-Murillo, M. A., Cervantes-Sanchez, J. J. Robot-assisted ankle rehabilitation: a review. Disability and Rehabilitation: Assistive Technology. 15 (4), 394-408 (2020).
- Hao, Y., et al. Novel MRI-compatible tactile stimulator for cortical mapping of foot sole pressure stimuli with fMRI. Magnetic Resonance in Medicine. 69 (4), 1194-1199 (2013).
- Gallasch, E., et al. Contact force- and amplitude-controllable vibrating probe for somatosensory mapping of plantar afferences with fMRI. Journal of Magnetic Resonance Imaging. 24 (5), 1177-1182 (2006).
- Noble, J. W., Eng, J. J., Boyd, L. A. Bilateral motor tasks involve more brain regions and higher neural activation than unilateral tasks: An fMRI study. Experimental Brain Research. 232 (9), 2785-2795 (2014).
- Martinez, M., et al. MRI-compatible device for examining brain activation related to stepping. IEEE Transactions on Medical Imaging. 33 (5), 1044-1053 (2014).
- Trinastic, J. P., et al. An fMRI study of the differences in brain activity during active ankle dorsiflexion and plantarflexion. Brain Imaging and Behavior. 4 (2), 121-131 (2010).
- de Lima-Pardini, A. C., et al. An fMRI-compatible force measurement system for the evaluation of the neural correlates of step initiation. Scientific Reports. 7 (1), 43088 (2017).
- Promjunyakul, N. O., Schmit, B. D., Schindler-Ivens, S. M. A novel fMRI paradigm suggests that pedaling-related brain activation is altered after stroke. Frontiers in Human Neuroscience. 9, 324 (2015).
- Zhang, T., et al. An MRI-compatible foot-sole stimulation system enabling characterization of the brain response to walking-related tactile stimuli. Frontiers in Neuroscience. 13, 1075 (2019).
- Khanicheh, A., et al. MR compatible ERF-based robotic device for hand rehabilitation after stroke. Proceedings of the International Society for Magnetic Resonance in Medicine. 13, 1110 (2005).
- Khanicheh, A., Mintzopoulos, D., Weinberg, B., Tzika, A. A., Mavroidis, C. MR_CHIROD v.2: A fMRI compatible mechatronic hand rehabilitation device. Proceedings of the 2007 IEEE 10th International Conference on Rehabilitation Robotics. , 883-889 (2007).
- Mintzopoulos, D., et al. On-line brain mapping using fMRI and a magnetic resonance compatible hand-induced robotic device (MR_CHIROD). Proceedings of the International Society for Magnetic Resonance in Medicine. 15, 3330 (2007).
- Inpatient Rehabilitation Care. Medicare Available from: https://www.medicare.gov/coverage/inpatient-rehabilitation-care (2023)
- Benjamin, E. J., et al. Heart disease and stroke statistics-2017 update: A report from the American Heart Association. Circulation. 135 (10), e146 (2017).
- Astrakas, L. G., Naqvi, S. H., Kateb, B., Tzika, A. A. Functional MRI using robotic MRI compatible devices for monitoring rehabilitation from chronic stroke in the molecular medicine era (Review). International Journal of Molecular Medicine. 29 (6), 963-973 (2012).
- Lazaridou, A., et al. Diffusion tensor and volumetric magnetic resonance imaging using an MR-compatible hand-induced robotic device suggests training-induced neuroplasticity in patients with chronic stroke. International Journal of Molecular Medicine. 32 (5), 995-1000 (2013).
- Lazaridou, A., et al. fMRI as a molecular imaging procedure for the functional reorganization of motor systems in chronic stroke. Molecular Medicine Reports. 8 (3), 775-779 (2013).
- Hyndman, D., Ashburn, A., Stack, E. Fall events among people with stroke living in the community: circumstances of falls and characteristics of fallers. Archives of Physical Medicine and Rehabilitation. 83 (2), 165-170 (2002).

.
