Real-Time In Vitro Migration Assay for Primary Murine CD8+ T Cells
Summary
This protocol providesa method of primary murine T cell isolation and time-lapse microscopy of T cell migration under specific environmental conditions with quantitative analysis.
Abstract
The adaptive immune response is reliant on a T cell's ability to migrate through blood, lymph, and tissue in response to pathogens and foreign bodies. T cell migration is a complex process that requires the coordination of many signal inputs from the environment and local immune cells, including chemokines, chemokine receptors, and adhesion molecules. Furthermore, T cell motility is influenced by dynamic surrounding environmental cues, which can alter activation state, transcriptional landscape, adhesion molecule expression, and more. In vivo, the complexity of these seemingly intertwined factors makes it difficult to distinguish individual signals that contribute to T cell migration. This protocol provides a string of methods from T cell isolation to computer-aided analysis to assess T cell migration in real-time under highly specific environmental conditions. These conditions may help elucidate mechanisms that regulate migration, improving our understanding of T cell kinetics and providing strong mechanistic evidence that is difficult to attain through animal experiments. A deeper understanding of the molecular interactions that impact cell migration is important to develop improved therapeutics.
Introduction
T cells are the major effectors of the adaptive, antigen-specific immune response. On a population level, T cells are heterogeneous, comprised of cellular subsets with distinct specialized functions. Importantly, CD8+ T cells are the main cytolytic effectors of the immune system, which directly eliminate infected or dysfunctional cells1.
Mature CD8+ T cells reside in tissue and circulate through blood and lymphatics in search of antigens. During infection, T cells are presented with antigens in blood or tissue and quickly drain to the spleen or nearest draining lymph node to begin a productive immune response. In either case, T cells become activated, undergo clonal expansion, and leave the lymphatic system to enter the blood, if not already there. During this process, intracellular signaling confers the downregulation of lymphatic homing receptors and the upregulation of numerous integrin and chemokine receptors essential for tissue-specific migration2. Ultimately, the directed migration of T cells to sites of infection is driven by converging environmental signals that include integrin and chemokine signaling.
Chemokines can be broadly categorized into two main classes: (1) homeostatic signals, which are essential for differentiation, survival, and basal function, and (2) inflammatory signals, such as CXCL9, CXCL10, and CCL3, which are required for chemotaxis. Generally, chemokines create a signal gradient that drives directional migration, known as chemotaxis, in addition to activating integrin expression1. Chemotaxis is finely regulated and highly sensitive, with T cells capable of responding to tiny changes in gradient that can lead them toward a specific direction or location.
In addition to these T cell-related factors, migration is also affected by the extracellular matrix (ECM) composition and density. The ECM is made up of a dense network of proteins, including collagen and proteoglycans, which provide the scaffold for adhesive integrin receptors on T cells. Integrins are a diverse family of transmembrane proteins, each with highly specialized binding domains and downstream signaling effects. Dynamic expression of integrin receptors on the surface of a T cell enables quick adaptation to their changing environments3. Importantly, integrins connect the ECM and intracellular cytoskeletal actin networks that work together to generate the propelling force required for T cell movement.
In summary, migration patterns vary based on the immune cell phenotype or environmental signals. These complex biological processes are tightly regulated by the expression of cytokines, chemokines, and integrins on the surface of the T cell, surrounding cells, and the local, infected tissue. In vivo, these migratory mechanisms can be complex and may result from several additive signals4. Due to this complexity, it can be impossible to establish a causal relationship between seemingly interlocked variables. To overcome this, there are several in vitro approaches to study specific aspects of T cell migration such as response to specific chemokine signals and the interaction between T cell integrins and ECM binding proteins. This protocol addresses methods to isolate and activate murine CD8+ T cells, with in vitro migration assays in two-dimensional space and computational analysis tools for analyzing specified T cell migration. These methods are advantageous to the user because they do not require sophisticated materials or devices, as with some other cell migration assays described in the literature. Cell migration data generated with these methods can provide evidence of immune responses in a simplistic manner that enables further, informed investigation in vivo.
Protocol
The animal protocols were approved by the University Committee on Animal Resources at the University of Rochester. The mice in this study were maintained in the pathogen-free space of the University of Rochester animal facility. Male/female C57BL/6 mice, aged 6-12 weeks (15-30 g), were used for the present study. Mouse tissue isolation can be performed on a benchtop with gloves to cover hands and a facemask to cover the nose and mouth, or inside a biosafety cabinet. All cell culture and plate preparation must be performed in a biosafety cabinet. The reagents and equipment used in this study are listed in the Table of Materials.
1. CD8+ T cell purification and activation
- Preparation of materials
- For the negative selection of CD8+ T cells: Prepare a negative selection medium from the supernatant of hybridoma cell lines GK1.5 and M5/114 antibodies, which produce anti-CD4 and anti-MHCII, respectively. Mix the supernatant at a 1:1 ratio, filter it, and store it at 4 °C for future use (>0.5 µg of each antibody/million total cells). Alternatively, commercial CD8+ T cell isolation kits are available.
- For activation of T cells: Add 500 µL of CD3 (10 µg/mL) and CD28 (16 µg/mL) antibodies in 1x DPBS (without calcium and magnesium) to a non-tissue culture (TC) treated 24-well plate and store overnight at 4 °C to ensure plate binding.
NOTE: Antibodies and proteins coat non-TC-treated culture plates/dishes better than regular TC-treated ones, so non-TC-treated culture plates are used for T cell generation.
- Prepare a 10 cm culture dish (or equivalent) by placing a 70 µm cell strainer into the dish and dispense 2 mL of R9 medium into the filter (R9 medium: RPMI 1640x supplemented with 10% FBS, 1% antibiotic-antimycotic, 20 mM HEPES buffer, 1% MEM non-essential amino acids, 50 µM β-mercaptoethanol).
- Obtain a mouse with appropriate genetic background, sex, age, and weight as determined by the experimental design.
- Euthanize the mouse using CO2 followed by cervical dislocation, or appropriate euthanasia strategies as defined by local animal care and use protocols and approved by the institution.
- Place the mouse in a supine posture, stretch all four limbs perpendicular to the body, and pin footpads to a dissection board using mouse dissection T pins, or equivalent. Make a superficial, central incision through the cutaneous layer on the ventral lower abdomen with mouse surgical dissection scissors and cut straight up to the chin (~8 cm). Separate the skin from the peritoneal lining to expose lymph nodes. Stretch the skin perpendicularly away from the trunk and pin it down5.
- Gently excise the cervical, axial, brachial, and inguinal lymph nodes bilaterally using blunt forceps (or the preferred type from a standard mouse surgical dissection kit). Transfer to the cell strainer prepared in step 1.2.
- Open the peritoneum and remove the spleen. Transfer to the cell strainer prepared in step 1.2.
- Dispose of the mouse carcass in the appropriate biohazard receptacle.
- Prepare a single-cell suspension of the secondary lymphoid tissues by mechanical disruption over the 70 µm cell strainer with 2 mL of R9 medium from step 1.2 by twisting the tissue disruption tool one-half turn clockwise and counterclockwise repeatedly.
NOTE: The plunger end of a luer-lock syringe, either 3 mL or 10 mL, works well to crush and homogenize the tissue. Alternative materials can be used at the user's discretion. - Wash the cells, syringe end, strainer, and culture dish with 7 mL of medium, ensuring the strainer remains upright to prevent the transfer of larger pieces of tissue or cellular aggregates that may be present into the single-cell suspension.
- Transfer the cell suspension to a 15 mL conical tube.
- Pellet the cells at 270 x g at room temperature (20 °C) for 5 min and decant the supernatant.
- Add 500 µL of lysing buffer for 1 min to remove red blood cells. Dilute with 9.5 mL of R9 medium and spin at 270 x g (20 °C) for 5 min. Decant the supernatant.
- Resuspend the pellet in 10 mL of the previously prepared negative selection medium containing anti-MHCII and anti-CD4 (step 1.1.1). Rock at room temperature (20 °C) for 30 min.
- Pellet the cells at 270 x g for 5 min and decant the supernatant. Wash 3x with 10 mL of R9 medium.
- Simultaneously, in a 15 mL conical tube, wash 200 µL of sheep anti-rat IgG beads in 7 mL of medium. Place the tube on a magnet, remove the medium, and repeat the wash step twice. Resuspend the beads in 7 mL of R9 medium.
- Pellet the cells at 270 x g (20 °C) for 5 min, decant the supernatant, and then resuspend the pellet in 7 mL of bead suspension from step 1.13. Rock at room temperature (20 °C) for 45 min.
- Enrich CD8+ T cells by magnetic bead depletion. Place the conical tube directly on the magnet without a lid for 3 min to remove antibody/bead-bound cells. CD8+ cells should be retained. With the tube still in the magnet, collect the cell suspension using a serological pipet or equivalent and transfer it to a new 15 mL tube. Centrifuge at 270 x g (20 °C) for 5 min and wash 3x in medium.
- Wash the pre-coated activation plate (step 1.1.2) with 1x DPBS twice without directly pipetting on the bottom surface of the plate.
- Optional: Perform a live/dead lymphocyte separation to remove dead cells.
- Transfer cells to a 15 mL conical tube. Gently add 2 mL of lymphocyte separation media to the bottom of the cell suspension. Centrifuge at 900 x g for 10 min (at room temperature) at low acceleration and deceleration.
NOTE: Live cells will separate at the interface of medium and separation media (middle white layer). Dead cells will pellet at the bottom of the tube and may be discarded at the end. - Transfer the middle layer containing live lymphocytes to a new tube and centrifuge at 270 x g for 5 min at room temperature. Decant the supernatant.
- Transfer cells to a 15 mL conical tube. Gently add 2 mL of lymphocyte separation media to the bottom of the cell suspension. Centrifuge at 900 x g for 10 min (at room temperature) at low acceleration and deceleration.
- Resuspend the pellet in 12 mL of medium with 10 U/mL recombinant mouse IL-2. Plate 1 mL per well in a non-TC treated 24-well plate and transfer to 37 °C overnight.
2. Lifting the activated CD8+ T cells
- Visualize cells using a standard benchtop light microscope, using the 4x or 10x objective.
NOTE: Activated T cells will appear larger and round or elongated compared to inactivated T cells and should have dense clusters of cells throughout the well. - To lift the activated cells, disrupt the cells with a 1 mL pipette, making sure to mix well at the edges of the plate. Transfer cells to a new 15 mL conical tube.
NOTE: Activated cells are stickier and require more vigorous pipetting. - Wash the wells with 1 mL of R9 medium to remove any remaining cells. Repeat once more if needed. Centrifuge the cells at 270 x g (20 °C) for 5 min. Discard the supernatant.
- Perform a live/dead lymphocyte separation to remove dead cells as in steps 1.17-1.18.
- Maintain T cells by live/dead cell removal every 3-4 days in R9 medium with IL-2 in a non-TC 6-well plate.
NOTE: T cells proliferate better in wells of small dimension during early activation, possibly due to T cell-T cell contacts or T cell-derived soluble factors that help their activation. Rapid T cell proliferation causes the culture medium to yellow within 24-48 h post-culture. At this point, lift the cells and transfer them to a larger well (uncoated, non-TC 6-well plate) with sufficient fresh culture medium to feed the cells (typically 5 mL per well). Replace depleted medium with fresh whenever indicated by yellow medium color change, or every 3-4 days.
3. Preparation of glass dish
- Prepare glass cell migration chambers or plates by coating with 300 µL/cm2 Protein A (0.1 mg/mL) overnight at 4 °C, wash twice with 1x DPBS by dispensing onto the dish and decanting before moving to the next step.
- Coat the migration chamber or plate with 300 µL/cm2 recombinant mouse ICAM-1 or VCAM-1 Fc chimera (0.1-2.75 mg/mL) together with a recombinant mouse chemokine (0.1-10 µg/mL) for 2-3 h at room temperature. Other integrin ligands such as fibronectin, mouse collagen IV, and mouse E-cadherin are rendered to directly coat the chamber at 2.5-10 µg/mL overnight at 4 °C.
- Wash chambers twice with 1x DPBS by dispensing onto the dish and decanting immediately after before adding cells.
NOTE: T cells can migrate differently in different concentrations of integrin ligands and chemokines depending on the status of activation, differentiation, sensitization, and priming. Assaying cell migration in multiple different concentrations is strongly suggested.
- Wash chambers twice with 1x DPBS by dispensing onto the dish and decanting immediately after before adding cells.
- Plate the adherent cells on glass-coated plates 24 h prior to the start of imaging if co-culturing T cells with other cells, such as cancer cells, to measure T cell killing of cancer cells in a real-time manner.
4. Preparation of cells
- Optional: Stain T cells and adherent cells with cell tracker dye of choice at 1 µg/mL per 1 x 107 cells in 1x DPBS for 15 min at 37 °C, or according to the manufacturer's protocol.
- Count cells using a hemocytometer or equivalent.
- Plate 1 x 105 CD8+ T cells (or desired amount) in Leibovitz's L-15 medium supplemented with 1-5 g/L glucose in a 37 °C chamber.
NOTE: L-15 medium is formulated for use without a CO2-sodium bicarbonate system. It is buffered using free basic amino acids, phosphate buffers, and galactose to maintain pH levels. - Optional: Perform integrin blocking.
- Preincubate T cells with a blocking antibody to an integrin (1-10 µg/mL, anti-mouse CD11a (M17/4), anti-mouse CD18 (M18/2), anti-mouse VLA-4 (9C10) for 10 min and allow to crawl in the presence of the same antibody.
5. Time-lapse microscopy
- Perform video microscopy.
- For T cells, acquire brightfield and fluorescent images every 10-60 s for 10-60 min, or desired acquisition settings.
NOTE: T cell migration is temperature-sensitive, and the optimal temperature for mouse T cell migration is 37 °C. The temperature control system that this protocol uses consists of an enclosed and insulated microscope deck with an attached heating system. The imaging chamber sits on the imaging deck. The perimeter of this chamber has a well filled with distilled water that allows consistent heat and humidity during imaging. The microwell is positioned at the center of the imaging chamber.
6. Software-assisted analysis of T cell migration
- Use the Volocity software to assess T cell migration.
- Open Volocity and create a new image sequence.
- Select and move all time-lapse video microscopy movies to the blue area in Volocity.
- Adjust brightness and contrast using the contrast enhancement tool to the researcher's desired settings.
- Check image sizes: 0.325 µm for 20x, 0.65 µm for 10x.
- Sequence: set timepoints (ex: 81 images if taking an image every 15 s for 20 min, 4 per min).
- Uncheck all timepoints in the measurement tab.
- Find objects using intensity-slide the bar so it is just right of the peak.
- Exclude objects by size: all cells that are smaller than 10 µm diameter and greater than 100 µm to exclude cell debris or non-cellular particles. Exclude T cells that are migrating for less than 20% of the recording time (which can vary depending on the definition by each investigator).
- Ignore static objects (check box).
- Automatically join broken tracts (check box).
- Set the shortest path to no more than 20 µm.
- The track of a cell migration is the line connecting the location of the same cell over time. Ensure that the tracking algorithm is tracking by detecting where individual objects are detected by segmentation in each frame, and the objects are matched across frames.
- Save a new protocol by choosing Measurements > Save Protocol > Name New Protocol.
- Click on measure all timepoints in the measurement tab.
- Sort tracks by timespan, high to low.
- Record track ID numbers for all cells with good tracks as defined by the investigator. After automatic cell tracking, manual evaluation of each cell track is necessary to exclude falsely identified or broken tracks. Exclude cells with bad tracks.
- Export the file as comma-separated text and transfer data to the desired analysis software.
NOTE: Basic parameters: Velocity (µm/min), displacement (net movement, µm), track length (total path length, µm), and meandering index (MI; net displacement/track length. MI = 1 indicates a completely straight linear track).
- Perform manual tracking using Image J.
- Open plugins and select tracking and manual tracking. Set the parameters – time intervals, x/y calibration (pixel size), and z calibration (in manual tracking mode). Start individual cell tracking by clicking on add track, selecting one cell at the first time point, and continuing it through all time points. Next, click on End track. Repeat it for all the cells of interest.
NOTE: Trackmate, another tool for cell tracking, is an automatic tracking software available via the ImageJ plugin.
- Open plugins and select tracking and manual tracking. Set the parameters – time intervals, x/y calibration (pixel size), and z calibration (in manual tracking mode). Start individual cell tracking by clicking on add track, selecting one cell at the first time point, and continuing it through all time points. Next, click on End track. Repeat it for all the cells of interest.
Representative Results
Confirmation of T cell activation can be achieved by flow cytometry, looking for increased expression of CD69 and CD44, which are canonical markers of activation in murine T cells6. Additionally, the purity of the T cell population can be determined by flow cytometry for CD3+ CD8+ T cells. This method yields >90 % CD8+ T cell population.
T cell migration can be assessed with software-assisted cell tracking programs that are both reproducible and tunable to fit the investigator's needs. Some basic parameters used to determine experimental effects include cellular velocity (migration length per a given time to determine how fast a cell moves), displacement (migration distance, a straight line from the starting point to the endpoint, to determine how far a cell migrates), track length (migration distance, the total length of migration path, to determine how far a cell migrates), and meandering index (MI is between 0 and 1 to determine the straightness of migration, 1 = straight). These parameters are employed to evaluate migratory differences in naïve and activated CD8+ T cells crawling along ICAM-1 coated glass with CXCL12 (Figure 1). Increased average velocity, displacement, and meandering index were observed in activated CD8+ T cells compared to naïve, indicating that activated T cells have increased migration capability. Similarly, the impact of different chemokines on cellular migration patterns can be elucidated with these methods. For example, activated CD8+ T cells exhibit increased migration in the presence of CXCL12, but not CCL2 or CCL22, and migration increases in a dose-dependent manner to a saturating concentration (Figure 2). Furthermore, software-assisted cell tracking enables the characterization of individual cell migration, which allows an understanding of the effects of individual ligands on T cell behavior. Representative cell tracks can be seen in Figure 3.
Taken together, these data support the efficacy of the current methods by confirming that we can (1) track cell migration on an individual cell basis, and (2) distinguish differences in migration of CD8+ T cells based on activation status and in the presence of different chemokines and adhesion molecules. This assay is a critical step in dissecting complex signaling mechanisms and informing focused in vivo experiments that can further address the biological contributions of specific signals in a cell type-specific manner.
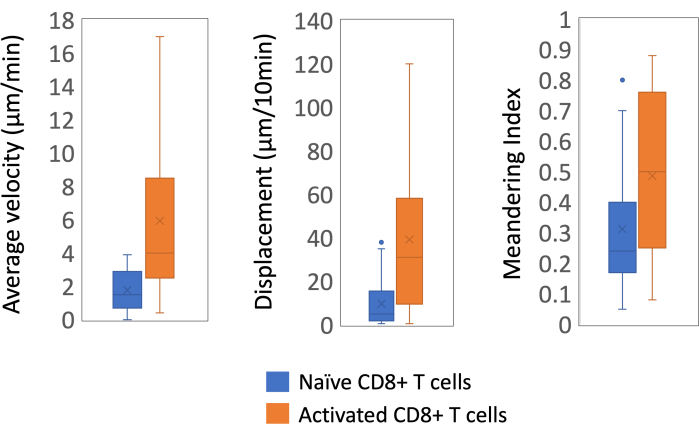
Figure 1: In vitro assays for naïve and activated CD8+ T cell migration. Naïve or CD3/CD28-activated mouse CD8+ T cells were allowed to migrate on ICAM-1 plus CXCL12 for 10 min. Velocity, displacement, and meandering index of the cell migration were analyzed using time-lapse microscopy and Volocity. Each group has 36 individual T cells (mean ± SEM). Please click here to view a larger version of this figure.
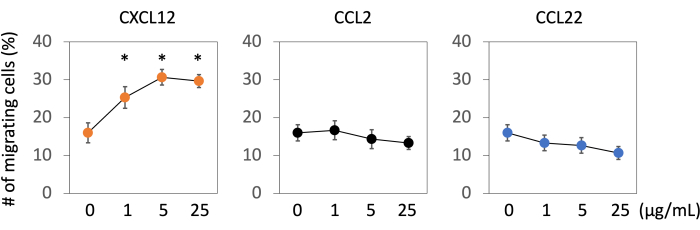
Figure 2: In vitro assays for chemokine-dependent migration of activated CD8+ T cells. CD3/CD28-activated mouse CD8+ T cells were allowed to migrate on ICAM-1 plus an indicated chemokine. The ratios of the number of cells crawling more than 50 µm for 20 min (percentage of total) were determined in a field of view. A single assay analyzed >10 cells (n = 3 assays per group mean ± SEM). Unpaired t-test, *p< 0.05 compared with control. Please click here to view a larger version of this figure.
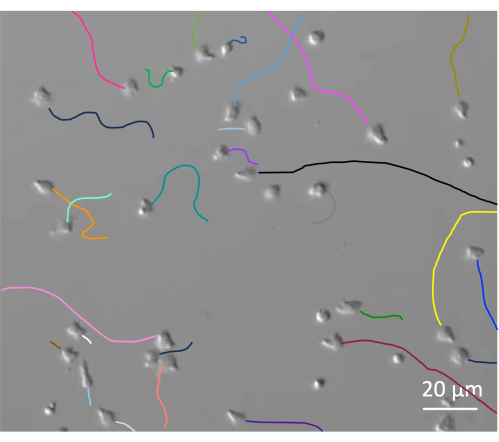
Figure 3: Migratory tracks of activated CD8+ T cells on ICAM-1 plus CXCL12 for 20 min. Each colored line indicates the migratory track of each T cell in a direction from the point of the cell to the opposite. In this particular assay, 24 out of 38 cells migrated in a significant length (at least the distance of their cell width by our definition). T cells migrated in different lengths of distances, indicating each cell was in a different status of activation or priming. All the migrating cells moved in different directions under the condition that the surface was uniformly coated. Please click here to view a larger version of this figure.
Discussion
Understanding the biological impact of converging signals in vivo is challenging and not easy to interpret. The protocols presented herein provide a reasonable method to understand T cell migration in highly defined and biologically relevant conditions. These conditions can be specified based on the investigator's discretion, and the protocols can be modified to fit the needs of various T cell populations, activation status, and cell phenotype. Furthermore, many ligands and receptors can be interrogated through these defined antibody-blocking7,8 and ligand-coated glass procedures8,9,10. This technique has also been a critical platform to develop engineered immune cells11,12.
Important steps in the protocol include the isolation of secondary lymphoid tissue, activation of the T cells, coating of the glass imaging dishes, and data analysis. To the inexperienced eye, lymph nodes embedded in tissue can be difficult to identify and extract. This can be overcome with practice. Once T cells have been isolated and purified, the activation step results in sticky cells that, if not lifted properly, can result in low yield. This can be avoided with generous and careful washing of the wells. Glass dishes must be properly coated with the ligand of interest and washed before the addition of cells. This will ensure that a robust layer of protein is available for cells to adhere to, while also ensuring that excess reagent does not disrupt the biology. Protein A-glass surface binding and Fc-Protein A binding in the physiological pH and salt concentration are strong enough to resist being washed off when gently pouring and decanting buffer. Residual proteins, if any, in the medium do not cause any toxicity, even though they might disturb cell interaction with bound ligands if unbound ones are in high concentrations. We rule out this possibility by rinsing the coated glass a couple of times. Finally, many user-friendly commercial and non-commercial software exist that allow researchers to detect even subtle differences in cellular behaviors and morphologies. The importance of reassuring the analyzed results manually to exclude errors that the software could make cannot be overstated.
Methods for T cell purification and activation can be modified to fit the needs of the researcher to obtain the proper cell state and phenotype to recapitulate in vivo observations. Various cell types and states can be used to address different mechanisms of infection and immune response7,8,9,10,11,13, including addressing naïve and memory T cell behavior and various aspects of the memory response, such as priming and recruitment, in tissue-specific conditions14. This method can be used for co-culture with different cell types to understand cellular interactions further, including cell-cell contact times and duration7,9, antigen presentation9,13, and target cell killing6. Additional reporters and labels can be used to assess subcellular structures7, granules15, apoptosis6, and more.
The protocol is an excellent tool to guide additional in vivo experiments based on observations in simplified and highly defined conditions. While in vitro assessment of cell motility can be highly reductive, it is an important step in breaking down complex biological activities. With the results of these experiments, investigators can approach in vivo work in a more physiologically relevant and targeted way.
The simplicity of this method also represents its major limitation; though representative of in vivo activities, all results can be further confirmed using intra-vital multiphoton microscopy, for example. The method described herein is one of the simplest that is fully available to research labs with a brightfield microscope and/or epifluorescence microscope with a digital camera integrated into the microscope system or separately put on the scope's objective. On the other hand, there are more options for advanced analysis of in vitro immune cell migration. First, immune cells are often driven by chemokine gradients in the biological system. Analysis of immune cell behaviors under chemokine gradients can be attained in several ways. One simple method is to use a specially designed slide (see Table of Materials). This channeled well system, when its bottom coated with integrin ligands, enables analysis of immune cell migration under static chemokine gradient. Other simple assays for immune cell chemotaxis include time-lapse microscopy of cell migration to a micropipette tip that releases chemokines16, under agarose assay17, and Zigmond chamber18. For more sophisticated migration assay under controlled chemokine gradients, customized slides with microfluidic gradient generators are required19,20. Second, immune cells can migrate in unique physical conditions using different mechanisms, sometimes without using integrin-dependent adhesion to ligands. The in vitro migration assay in one-dimension can be done with or without integrin ligand coating and reproduces motility of immune cells in capillary vessels21,22. Another option is cell migration assay in three-dimensional space23,24 to investigate mechanisms underlying interstitial migration of cells25,26. Overall, we have outlined simple, reproducible, and reliable methods to study dynamic cellular migration events.
Disclosures
The authors have nothing to disclose.
Acknowledgements
We thank previous and current members of the Kim Lab who have contributed to the development of these protocols over time. Representative data were made possible by P01 AI102851/AI/NIAID NIH HHS/United States and P01 HL018208/HL/NHLBI NIH HHS/United States. This publication was made possible in part by Grant Number T32 GM135134 from the Institutional Ruth L. Kirschstein National Research Service Award.
Materials
| 10 cm dish | Corning | 353003 | or equivalent |
| 15 mL conical tube | ThermoFisher | 339650 | or equivalent |
| 1x DPBS | Gibco | 14190144 | without calcium and without magnesium |
| 6 well plate non-TC treated | Corning | 3736 | or equivalent |
| 70 µm cell strainer | FisherScientific | 352350 | or equivalent |
| ACK lysing buffer | ThermoFisher | A1049201 | or equivalent |
| Allegra 6KR centrifuge | ThermoScientific | sorvall 16R with tx400 3655 rotor and bucket | or equivalent |
| Beta mercaptoethanol | Sigma | M3148 | or equivalent |
| CellTrace Violet | ThermoFisher | C34571 | Or equivalent |
| Centrifuge | ThermoScientific | Sorvall ST 16R | or equivalent |
| Collagen (IV) | Corning | 354233 | or equivalent |
| DeltaT culture dish .17 mm thick glass clear | Bioptechs | 04200417C | |
| Dynabeads Sheep anti-Rat IgG | Invitrogen | 11035 | |
| DynaMag 15 Magnet | ThermoFisher Scientific | 12301D | or equivalent |
| Easy sep mouse T cell isolation kit | Stem Cell | 19851 | |
| FBS | SigmaAldrich | F2442-500ML | or equivalent |
| Fibronectin | SigmaAldrich | 10838039001 | or equivalent |
| Fiji | http://fiji.sc/ | weblink | |
| Filter cubes | Nikon or Olympus | ||
| GK1.5 | ATCC | TIB-207 | |
| HEPES | ThermoFisher | 15630080 | or equivalent |
| HQ CCD camera | CoolSNAP | or equivalent | |
| ImageJ | http://imagej.nih.gov/ij/h | weblink | |
| ImageJ automatic tracking plug in | http://imagej.net/TrackMate | weblink | |
| ImageJ manual tracking plug in | https://imagej.nih.gov/ij/plugins/track/track.html | weblink | |
| L-15 | Various | See Materials | Medium Recipe: Leibovitz’s L-15 medium without phenol red (Gibco) supplemented with 1-5 g/L glucose |
| Liebovitz's L-15 medium, no phenol red | ThermoFisher | 21083027 | |
| Luer Lok disposable syringe | Fisher Scientific | 14-955-459 | or equivalent |
| Lymphocyte separation medium | Corning | 25-072-CI | or equivalent |
| M5/114 | ATCC | TIB-120 | |
| MEM Non-Essential Amino Acids | ThermoFisher | 11140050 | or equivalent |
| Microscope heating system | Okolab | okolab.com | Custom designs available |
| Millicell EZ slide | Millipore | C86024 | |
| Mojosort mouse CD8+ Naïve T cell isolation kit | Biolegend | 480043 | |
| Mouse E-cadherin | R&D systems | 8875-EC-050 | or equivalent |
| Mouse surgical dissection kit | Fisher Scientific | 13-820-096 | or equivalent |
| NIS elements | Nikon | Software | |
| non-TC 24wp | Corning | 353047 | or equivalent |
| Penicillin-streptomycin | ThermoFisher | 15140122 | or equivalent |
| Protein A | ThermoFisher Scientific | or equivalent | |
| R9 | Various | See Materials | Medium Recipe: RPMI 1640x supplemented with 10 % FBS, 1 % antibiotic-antimycotic (Gibco), 20 mM HEPES buffer (Gibco), 1 % MEM Non-Essential Amino Acids (Gibco), 50 μM β-mercaptoethanol (Sigma-Aldrich) |
| Recombinant mouse ICAM-1 Fc chimera | R&D systems | 796-IC-050 | or equivalent |
| Recombinant Mouse IL2 | Biolegend | 575410 | or equivalent |
| RPMI 1640x | ThermoFisher | 11875093 | or equivalent |
| T pins | Fisher Scientific | S99385 | or equivalent |
| TE2000-U microscope | Nikon | or equivalent | |
| Various recombinant mouse chemokine | R&D systems | or equivalent | |
| VCAM-1 Fc chimera | R&D systems | 643-VM-050 | or equivalent |
| Volocity | PerkinElmer | Software |
References
- Sun, L., Su, Y., Jiao, A., Wang, X., Zhang, B. T cells in health and disease. Signal Transduct Target Ther. 8 (1), 235 (2023).
- Fowell, D. J., Kim, M. The spatio-temporal control of effector T cell migration. Nat Rev Immunol. 21 (9), 582-596 (2021).
- Tabdanov, E. D., et al. Engineering t cells to enhance 3d migration through structurally and mechanically complex tumor microenvironments. Nat Commun. 12 (1), 2815 (2021).
- Kameritsch, P., Renkawitz, J. Principles of leukocyte migration strategies. Trends Cell Biol. 30 (10), 818-832 (2020).
- Flaherty, S., Reynolds, J. M. Mouse naive CD4+ T cell isolation and in vitro differentiation into t cell subsets. J Vis Exp. (98), e52739 (2015).
- Sailer, C. J., et al. Pd-1(hi) CAR-T cells provide superior protection against solid tumors. Front Immunol. 14, 1187850 (2023).
- Lim, K., Hyun, Y. M., Lambert-Emo, K., Topham, D. J., Kim, M. Visualization of integrin mac-1 in vivo. J Immunol Methods. 426, 120-127 (2015).
- Lim, K., et al. Neutrophil trails guide influenza-specific CD8+ T cells in the airways. Science. 349, 4352 (2015).
- Lim, K., et al. In situ neutrophil efferocytosis shapes T cell immunity to influenza infection. Nat Immunol. 21 (9), 1046-1057 (2020).
- Reilly, E. C., et al. T(rm) integrins CD103 and CD49a differentially support adherence and motility after resolution of influenza virus infection. Proc Natl Acad Sci U S A. 117 (22), 12306-12314 (2020).
- Amitrano, A. M., et al. Optical control of CD8(+) T cell metabolism and effector functions. Front Immunol. 12, 666231 (2021).
- Xu, Y., et al. Optogenetic control of chemokine receptor signal and t-cell migration. Proc Natl Acad Sci U S A. 111 (17), 6371-6376 (2014).
- Capece, T., et al. A novel intracellular pool of IFA-1 is critical for asymmetric CD8(+) T cell activation and differentiation. J Cell Biol. 216 (11), 3817-3829 (2017).
- Hirai, T., Whitley, S. K., Kaplan, D. H. Migration and function of memory CD8(+) T cells in skin. J Invest Dermatol. 140 (4), 748-755 (2020).
- Mouchacca, P., Schmitt-Verhulst, A. M., Boyer, C. Visualization of cytolytic T cell differentiation and granule exocytosis with T cells from mice expressing active fluorescent granzyme B. PLoS One. 8 (6), e67239 (2013).
- Nuzzi, P. A., Lokuta, M. A., Huttenlocher, A. Analysis of neutrophil chemotaxis. Methods Mol Biol. 370, 23-36 (2007).
- Heit, B., Tavener, S., Raharjo, E., Kubes, P. An intracellular signaling hierarchy determines direction of migration in opposing chemotactic gradients. J Cell Biol. 159 (1), 91-102 (2002).
- Zigmond, S. H. Ability of polymorphonuclear leukocytes to orient in gradients of chemotactic factors. J Cell Biol. 75 (2), 606-616 (1977).
- Jowhar, D., Wright, G., Samson, P. C., Wikswo, J. P., Janetopoulos, C. Open access microfluidic device for the study of cell migration during chemotaxis. Integr Biol (Camb). 2 (11-12), 648-658 (2010).
- Sai, J., Walker, G., Wikswo, J., Richmond, A. The IL sequence in the LLKIL motif in CXCR2 is required for full ligand-induced activation of Erk, Akt, and chemotaxis in HL60 cells. J Biol Chem. 281 (47), 35931-35941 (2006).
- Choi, Y., Sunkara, V., Lee, Y., Cho, Y. K. Exhausted mature dendritic cells exhibit a slower and less persistent random motility but retain chemotaxis against ccl19. Lab Chip. 22 (2), 377-386 (2022).
- Harding, M. G., Zhang, K., Conly, J., Kubes, P. Neutrophil crawling in capillaries: A novel immune response to staphylococcus aureus. PLoS Pathog. 10 (10), e1004379 (2014).
- Rommerswinkel, N., Niggemann, B., Keil, S., Zanker, K. S., Dittmar, T. Analysis of cell migration within a three-dimensional collagen matrix. J Vis Exp. (92), e51963 (2014).
- Wu, P. H., Giri, A., Sun, S. X., Wirtz, D. Three-dimensional cell migration does not follow a random walk. Proc Natl Acad Sci U S A. 111 (11), 3949-3954 (2014).
- Lammermann, T., et al. Rapid leukocyte migration by integrin-independent flowing and squeezing. Nature. 453 (7191), 51-55 (2008).
- Overstreet, M. G., et al. Inflammation-induced interstitial migration of effector CD4(+) T cells is dependent on integrin αv. Nat Immunol. 14 (9), 949-958 (2013).

