Displacement Analysis of Myocardial Mechanical Deformation (DIAMOND) Reveals Segmental Heterogeneity of Cardiac Function in Embryonic Zebrafish
Summary
The goal of this protocol is to detail a novel method for the assessment of segmental cardiac function in embryonic zebrafish under both physiological and pathological conditions.
Abstract
Zebrafish are increasingly utilized as a model organism for cardiomyopathies and regeneration. Current methods evaluating cardiac function fail to reliably detect segmental mechanics and are not readily feasible in zebrafish. Here we present a semiautomated, open-source method for the quantitative assessment of four-dimensional (4D) segmental cardiac function: displacement analysis of myocardial mechanical deformation (DIAMOND). Transgenic embryonic zebrafish were imaged in vivo using a light-sheet fluorescence microscopy system with 4D cardiac motion synchronization. Acquired 3D digital hearts were reconstructed at end-systole and end-diastole, and the ventricle was manually segmented into binary datasets. Then, the heart was reoriented and isotropically resampled along the true short axis, and the ventricle was evenly divided into eight portions (I–VIII) along the short axis. Due to the different resampling planes and matrices at end-systole and end-diastole, a transformation matrix was applied for image registration to restore the original spatial relationship between the resampled systolic and diastolic image matrices. After image registration, the displacement vector of each segment from end-systole to end-diastole was calculated based on the displacement of mass centroids in three dimensions (3D). DIAMOND shows that basal myocardial segments adjacent to the atrioventricular canal undergo the highest mechanical deformation and are the most susceptible to doxorubicin-induced cardiac injury. Overall, DIAMOND provides novel insights into segmental cardiac mechanics in zebrafish embryos beyond traditional ejection fraction (EF) under both physiological and pathological conditions.
Introduction
Chemotherapy-induced cardiac toxicity and ensuing heart failure are one of the main reasons for chemotherapy discontinuation1. Therefore, cardiac functional assessment plays a crucial role in the identification of cardiac toxicity and, more importantly, in the prediction of early cardiac injury following chemotherapy2. However, current approaches for cardiac functional assessment encounter limitations. Methods such as left ventricular ejection fraction (LVEF) provide only global and often delayed cardiac mechanics after injury3,4. Tissue Doppler imaging provides segmental myocardial deformation information but suffers from significant intraobserver and interobserver variability, in part due to ultrasound beam angle dependency5. Two-dimensional (2D) speckle tracking utilizes the B-mode of echocardiography, which theoretically eliminates the angle dependency, but its accuracy is limited by out-of-plane motion6. Therefore, a rigorous approach for quantifying segmental cardiac function is lacking in both research and clinical settings.
In this context, we developed a 4D quantification method for the analysis of segmental cardiac function that we named displacement analysis of myocardial mechanical deformation (DIAMOND), to determine the displacement vectors of myocardial mass centroids in 3D space. We applied DIAMOND for the in vivo assessment of cardiac function and doxorubicin-induced cardiac toxicity with zebrafish (Danio rerio) as the animal model, chosen due to their regenerating myocardium and highly conserved developmental genes7. We further compared segmental DIAMOND displacement with global ejection fraction (EF) determination and 2D strain following doxorubicin treatment. By integrating DIAMOND displacement with 4D light-sheet fluorescent microscopy (LSFM) acquired rendering of embryonic zebrafish hearts, DIAMOND shows that the basal myocardial segments adjacent to the atrioventricular canal undergo the highest mechanical deformation and are the most susceptible to acute doxorubicin cardiac injury8.
Protocol
All methods described here have been approved by the UCLA Institutional Animal Care and Use Committee (IACUC), and experiments were performed in compliance with protocols approved by the UCLA Office of Animal Research.
1. Breeding Tg(cmlc2:mCherry) zebrafish and collection of embryos
- Follow the housing, breeding, and embryo collection procedures as described in previously established husbandry and breeding practices. For details, see Messerschmidt et al.9.
- Treat the collected embryos with 0.003% 1-phenyl-2-thiourea (PTU) in E3 medium 18 h postfertilization to maintain the transparency of the embryos for LSFM imaging.
2. Doxorubicin treatment to induce cardiac injury
- At 3 days postfertilization (dpf), treat the embryos with doxorubicin at a concentration of 10 μM in E3 fish water medium. After a 24 h treatment to 4 dpf, replace the doxorubicin medium with fresh E3 medium.
CAUTION: Doxorubicin is a chemotherapy medication. Appropriate personal protective equipment (PPE) is required and the waste should be disposed of in biohazard waste containers.
3. Notch pathway modulation
- Treat zebrafish embryos with the Notch pathway inhibitor (2S)-N-[(3,5-difluorophenyl)acetyl]-L-alanyl-2-phenyl]glycine 1,1-dimethylethyl ester (DAPT) at a concentration of 10 μM in E3 fish water medium from 3–6 dpf.
- Microinject the Notch downstream effectors Notch intracellular domain (NICD) and Neuregulin-1 (Nrg-1) mRNA at concentrations of 10 pg/nL and 5 pg/nL, respectively, into the 1-cell stage zebrafish embryos8,10.
NOTE: The microinjection is performed under a microscope with the support of an air pump to accurately control the volume injected. The mRNA microinjection into the cell is done when the fertilized egg is at the first cell stage. For details on the preparation and sequence of the mRNAs, see Chen et al.8. For details on the microinjection and preparation of injection needles, see Rosen et al.10.
4. LSFM imaging and post-imaging synchronization
- For the LSFM imaging techniques and post-imaging synchronization algorithm, see details in previous publications9,11.
NOTE: Briefly, our system utilizes a continuous-wave laser as the illumination source to image all transgenic zebrafish lines. The detection module is composed of two scientific complementary metal-oxide semiconductor (sCMOS) cameras and two sets of filters for dual-channel imaging. The detection module is perpendicularly installed to the illumination plane. Each LSFM frame is acquired within a 20 msec exposure time, while the resolving power in cross section is ~0.65 μm and the step size between consecutive frames is ~2 μm. A 589 nm laser was used to excite mCherry fluorescent signals.
5. Reconstruction of the 3D systolic and diastolic heart
- Open the folder created by the post synchronization algorithm, then open the "Output" folder. Select the middle plane of the heart and load the entire folder into ImageJ. Find the first diastolic and systolic phase and record the frame number.
- Open the "Output/By State" folder and find the folders that have the same numbers as the frame numbers just recorded. Convert the images in the folder into 3D TIFF (tagged image file format) files and name them "diastole.tif" and "systole.tif".
6. Segmentation of the ventricle
- Open the image analyzing software (see Table of Materials). Click File | Open data, and load "diastole.tif" and "systole.tif". Enter the voxel size according to the imaging settings.
NOTE: For the LSFM system used, the typical voxel size is 0.65 µm x 0.65 µm x 2 µm. - Click the "SEGMENTATION" panel and manually segment out the ventricle part of the heart. The built-in "Threshold" tool that can select all the regions above a certain intensity can facilitate this process. The ventricle is the thicker chamber with a stronger fluorescence.
NOTE: Make sure to remove the atrioventricular canal and the outflow tract in the segmented ventricle, because this affects the displacement analysis. - After the segmentation is done, click the "Project" panel. Right click the "diastole.Labels.tif" and "systole.Labels.tif" tabs in the console and click "Export Data as" to save the data as 3D TIFF files.
7. Creation of rectangular parallelepipeds for image registration
- Run "prepImage_1.m" in the programming environment (see Table of Materials). Open "prepImage_1.m", "ImPath" in line 5 so the folder contains the original and segmented TIFF files, and change "slice" in line 4 to the number of slices of the 3D tif files.
- After running the code, it will generate five new 3D TIFF files ("test.tif", "diastole_200.tif", "systole_200.tif", "diaLabel.tif", and "sysLabel200.tif") as well as two new folders ("resample_dia" and "resample_sys").
8. Resample systolic and diastolic 3D hearts along the short axis plane
- Import all five 3D TIFF files into the image analyzing software (see Table of Materials).
NOTE: The voxel size is unchanged. - Go to the MULTIPLANAR panel. Choose "diastole_200.tif" as the primary data. Align the X-axis (the green line in the XY plane) with the vertical long axis of the ventricle, and align the Z-axis (the red line in the YZ plane) with the horizontal long axis of the ventricle.
NOTE: The vertical long axis is determined by finding the longest axis connecting the apex and the outflow tract in the XY plane, and the horizontal long axis is determined by finding the longest axis connecting the apex and the outflow tract in the YZ plane. Rotate the axis by placing the cursor at the end of the axis. - Choose three random points from the oblique YZ plane (the short axis plane) in a counterclockwise manner and record their 3D position coordinates.
NOTE: Make sure the points are chosen in a counterclockwise manner. - Repeat steps 8.2 and 8.3 for "systole_200.tif".
- Click the "PROJECT" panel. Create a "Slice" object for "diastole_200.tif" by right clicking on "diastole_200.tif" and searching for "Slice" object. Left click the Slice object just created, and in the Properties panel | Options, check "Set Plane" and choose three points in "Plane Definition". Enter the coordinates of the three points from step 7.3.
- Repeat step 8.5 for "systole_200.tif".
NOTE: The slice object created should have the name "Slice 2". - Right click "diastole_200.tif" and search for "Resample Transformed Image" and create the object. In the Properties panel, choose "Slice" as the "Reference" and click Apply. This should generate an object named "diastole_200.transformed".
- Right click "diastole_200.transformed" and search for "Resample" and create the object. Choose "Voxel Size" as the "Mode" and change "Voxel Size" to be x = 1, y = 1, and z = 1 in the Properties panel.
- Click "Apply". This should generate an object named "diastole_200.resampled". Right click "diastole_200.resampled" and save it as a 3D TIFF file.
- Repeat the same step for "diaLabel.tif" and "test.tif". Save "diaLabel.resampled" and "test.resampled" as 3D TIFF files. Repeat the same step for "systole_200.tif", "sysLabel.tif", and "test.tif" using "Slice 2" as a reference, and save "systole_200.resampled", "sysLable.resampled", and "test2.resampled" as 3D TIFF files.
NOTE: Make sure there are a total of six TIFF files saved in this step.
9. Division of the resampled heart
- Import all six resampled files from step 8 to ImageJ. Select a slice of "systole_200.resampled" in which the atrioventricular canal is clearly visualized. Record the number of the slice.
- Use the "Image | Transform | Rotate" function of ImageJ so that the atrioventricular canal is vertical. Apply the same rotation to all files. Close all windows and save all changes.
- Move "diastole_200.resampled", "diaLabel.resampled", and "test.resampled" to the "resample_dia" folder, and move "systole_200.resampled", "sysLable.resampled", and "test2.resampled" to the "resample_sys" folder.
- Open "divider_2_8_pieces.m". Change "ImPath" in line 5 and "ImPath" in line 395 to the image directory. Change the variable "Middle" in line 22 and line 411 to the slice numbers where the atrioventricular canal is clearly visualized in "systole_200.resampled" and "diastole_200.resampled".
- Run the code, and in the prompted windows click once at the center of the ventricle and click once at the center of the atrioventricular canal. This needs to be done twice for both systole and diastole images.
10. Registration of systolic and diastolic image matrices
- Open "register_3.m" and change "ImPath" in line 4 to the image folder path. It might take 5–20 min to run this code depending on the computation power of the system.
NOTE: The artificially created rectangular parallelepipeds in step 7 are used for 3D rigid registration that preserves the distance between two points and angles subscribed by three points. When the end-diastole rectangular parallelepiped (red) is registered to the end-systole rectangular parallelepiped (green), the ensuing discrepant 3D location permits the derivation of a unique matrix of rigid transformation consisting of rotation and translation from the end-diastole matrix to the end-systole matrix (Figure 1H). We perform the registration and regularized energy minimization to denoise the matrix after the transformation using an image processing toolbox (see Table of Materials). For a detailed mathematical description, please see Chen et al.8.
11. Output of the displacement vectors
- Open "displacement_4.m" and change "ImPath" in line 4 to the image folder path.
- Run "displacement_4.m", which generates a "vector8.txt" file in the "vectors" folder. Once the "vector8.txt" file is open, there will be an 8 x 4 matrix. Each row of the matrix has four numbers, which are the magnitudes of the X component, Y component, Z component, and the SUM magnitude of the displacement vector of a specific segment of the ventricle.
NOTE: The displacement vector is obtained by calculating the displacement of the mass centroid of each segment in 3D space. We calculate the 3D mass centroid (PS and PD) coordinates (where k indicates the X, Y, or Z coordinate, respectively) of each segment (I-VI) in the segmentation dataset from systole to diastole (Figure 1J). We define the mass centroid
(where k indicates the X, Y, or Z coordinate, respectively) of each segment (I-VI) in the segmentation dataset from systole to diastole (Figure 1J). We define the mass centroid  in 3D space as follows:
in 3D space as follows:
where Cx = X, Cy = Y, and Cz = Z, Mi = the mass of each segment (I ≤ i ≤ VI), m = the number of voxels of each segment, and ρ = the density function as the segmented region is 1 whereas the rest is 0. The L2-norm of the sub-displacement vectors along the X-, Y-, and Z-axes and the sum displacement vector are calculated during the cardiac cycle. There are a total of eight rows in the matrix. The first row and the eighth row contain the atrioventricular canal and are thus ignored in our analysis. Segments I to VI are represented by the second row to the seventh row.
Representative Results
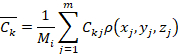
The process by which DIAMOND was developed to assess 3D segmental cardiac function is presented in Figure 1. Following LSFM image acquisition and reconstruction in 3D of the embryonic zebrafish heart (Figure 1A), the true short axis plane was determined as the plane perpendicular to the vertical and horizontal long axes, both of which are determined in a multiplane viewer (Figure 1B). The heart was then resampled along the short axis plane (Figure 1C), and divided into eight equal segments constituted by even angles according to a virtual division line (red dotted line) connecting the center of the endocardial ventricular cavity to the center of the atrioventricular canal (Figure 1E). The 3D depictions of the identified segments are illustrated in a cross-sectional view (Figure 1F) and in comparison with the raw data (Figure 2). Segments VII and VIII were removed from the analysis because they encompass the atrioventricular canal and thus contain less myocardium compared with other segments. The different resampling planes for end-systole (HS) and end-diastole (HD) lead to distinct coordinate systems for end-systolic and end-diastolic matrixes, which need to be registered to restore their original spatial relationship (Figure 1G). The coordinate system of the end-systolic matrix was chosen as the reference for consistency. To determine the transformation matrix (Tm) from the end-diastolic matrix to the end-systolic matrix, a matrix of three parallelepipeds, which is asymmetrical in 3D and has the same dimension as the original image matrix, was virtually created. The parallelepipeds were resampled twice, first in the short axis plane of the end-systole matrix, and then in the short axis plane of the end-diastole matrix, leading to different transformed parallelepipeds for end-systole (green) and end-diastole (red) (Figure 1H).
The green and red parallelepipeds were then registered together by a rigid body registration algorithm and Tm was calculated and applied to the end-diastole matrix to restore the coordinates (Figure 1I). This process permits subsequent tracking in the 3D space of the displacement vectors of mass centroids from any segment of the ventricle during the cardiac cycle (Figure 1J). DIAMOND displacement of ventricular segments I–VI can be tracked during multiple time points in the cardiac cycle (Figure 1K), which can be simplified for quantitative analysis to two time points ranging from end-systole to end-diastole (Figure 1L). The segments generated by DIAMOND can be visualized in Figure 2, where each color represent one cardiac segment.
With DIAMOND, we uncovered segmental heterogeneity of cardiac function and susceptibility to doxorubicin-induced myocardial injury in zebrafish. Following a 24 h treatment with 10 µM doxorubicin from 3–4 dpf (Figure 3A), we compared DIAMOND displacement of ventricular segments between control and chemotherapy-treated groups (Figure 3B) and 48 h after treatment (Figure 3C). All DIAMOND figures follow the same graphical pattern as the resampled ventricles along the short axis (Figure 1E). The data are presented as percentages by normalizing the L2-norm of the displacement vector to the inner perimeter of the heart, with the X (green), Y (blue), and Z components (orange) illustrated as their weighted contributions. At 4 dpf, the average L2-norm of the segmental displacement vectors in control fish ranged from 6.6–11.3 µm, or 3.8–6.6% after normalization. Our results indicate that under control conditions, the basal segments I and VI undergo the largest displacements and are the ones most susceptible to doxorubicin induced cardiac injury (Figure 3B, 29% decrease from 6.6–4.7%, n = 10 control and n = 8 doxorubicin, p < 0.01). At 6 dpf, the average L2-norm of the segmental displacement vectors in the control fish ranged from 6.8–14 µm, or 3.9–8% after normalization. At 6 dpf, the basal segments I and VI recovered DIAMOND displacement to control levels, suggesting segmental regeneration (Figure 3C, n = 10 control and n = 8 doxorubicin). In parallel, a worsening in 2D basal strain from -53 to -38% was observed at 4 dpf following doxorubicin treatment, followed by a return to control levels at 6 dpf, corroborating the DIAMOND displacement results (Figure 3D, 3E). A parallel decrease in global ejection fraction in response to doxorubicin at 4 dpf with recovery at 6 dpf was also observed (Figure 3F, 3G).
We next applied DIAMOND during doxorubicin treatment and Notch pathway modulation using the Notch inhibitor DAPT and rescue using Notch downstream effectors NICD and NRG1 mRNA (Figure 4A). NICD and NRG1 mRNA microinjection rescued the decrease in DIAMOND displacement and EF after acute chemotherapy-induced injury at 4 dpf (Figure 4B, 4D). Exposure to the Notch inhibitor DAPT together with doxorubicin led to a more diffuse decrease in DIAMOND displacement, in addition to the basal segments I and VI (Figure 4B). Moreover, inhibition of the Notch pathway after chemo-induced injury further hindered the recovery of DIAMOND displacement of the basal segments and EF at 6 dpf. The inhibition was rescued by the Notch downstream effectors NICD and NRG1 (Figure 4C, 4E).

Figure 1: 4D DIAMOND displacement development. (A) Raw images were captured by light-sheet fluorescent microscopy. (B and C) Reconstructed 3D heart was resampled along the true short axis plane view. (D) Schematic illustration of embryonic zebrafish heart. (E and F) 2D and 3D illustrations of the division of the ventricle into eight segments excluding segments VII and VIII. (G) The different coordinate systems of end-systole and end-diastole after resampling. (H) A group of rectangular parallelepipeds was created for the generation of a transformation matrix (Tm). (I) Registered end-systolic and end-diastolic coordinate systems by applying Tm. (J) Displacement vector of the segmental mass centroid from end-systole to end-diastole. (K) DIAMOND displacement of ventricular segments I–VI tracked during multiple time points in the cardiac cycle. (L) DIAMOND displacement of ventricular segments I–VI from end-systole to end-diastole. This figure from Chen et al.8 is reproduced with permission from the American Society for Clinical Investigation (ASCI). Please click here to view a larger version of this figure.
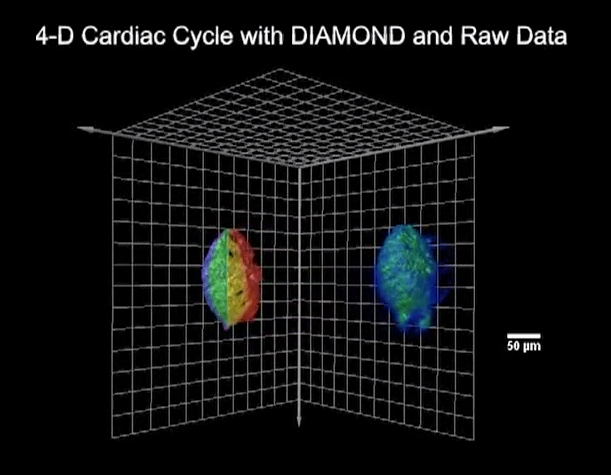
Figure 2: DIAMOND segmentation of the embryonic zebrafish heart compared with raw data in 3D. The embryonic zebrafish heart was divided into six segments (volumes) depicted here in different colors for the calculation of DIAMOND displacements (left). The displacement vector of each segment computed by DIAMOND represents its segmental cardiac function. The atrium and outflow tract were removed during segmentation. Scale bar = 50 µm. Please click here to view a larger version of this figure.
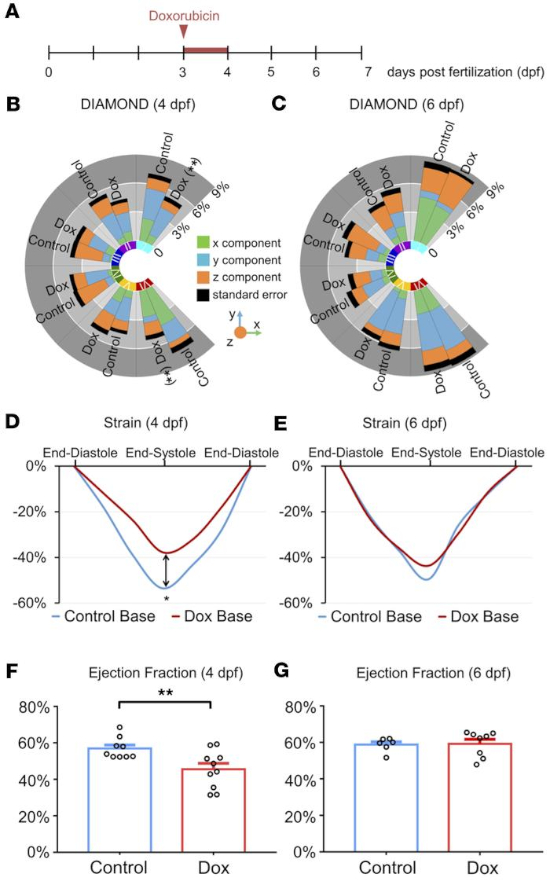
Figure 3: DIAMOND unravels the segmental heterogeneity in cardiac function and susceptibility to chemotherapy-induced injury. (A) Experimental schedule of doxorubicin treatment. (B and C) Segmental comparison of DIAMOND displacement vectors normalized to the inner myocardial perimeter between control and doxorubicin-treated groups at 4 and 6 dpf (t tests, **p < 0.01, n = 8–10 per group). (D and E) Assessment of strain in the ventricular base depicting a similar injury and regeneration pattern as the DIAMOND displacement vectors (*p < 0.05, n = 6–8 per group). (F and G) Decrease in ejection fraction in response to doxorubicin at 4 dpf with recovery at 6 dpf, following a pattern similar to segmental DIAMOND displacements at the global ventricular level (t tests, **p < 0.01, error bars SEM, n = 6–10 per group). This figure from Chen et al.8 is reproduced with permission from the ASCI. Please click here to view a larger version of this figure.

Figure 4: DIAMOND mechanics for assessment of Notch-mediated myocardial recovery following doxorubicin-induced injury. (A) Experimental schedule. (B and C) NICD and NRG1 Notch downstream effectors rescued the reduction of DIAMOND displacement in segments I and VI at 4 dpf. At 6 dpf, inhibition of Notch signaling by DAPT impaired the restoration of segmental cardiac function (ANOVA, **p < 0.01 Dox vs. control; †p < 0.05, ††p < 0.01, Dox + DAPT vs. control, n = 6–10 per group). (D and E) Ejection fraction corroborates DIAMOND mechanics at the global level (ANOVA, *p < 0.05, **p < 0.01, error bars SEM, n = 5–11 per group). This figure from Chen et al.8 is reproduced with permission from the ASCI. Please click here to view a larger version of this figure.
Discussion
A rigorous strategy for quantification of segmental myocardial function is critical to assess cardiac mechanics beyond traditional EF, known to be an insensitive and delayed indicator of myocardial injury1,4,12. Hence, there has been a growing interest in markers of early myocardial changes, and a growing body of literature supports myocardial deformation parameters as an early indicator to forecast ventricular dysfunction4,13. Echocardiographic measurement of left ventricular (LV) strain provides an established method of myocardial deformation measurement13. However, tissue Doppler-based strain imaging suffers from a number of shortcomings due to angle dependency and intraobserver and interobserver variability14. Speckle tracking echocardiography (STE) can resolve angle-independent 2D and 3D tissue deformation, but the accuracy of 2D speckle tracking is affected by through-plane motion6, while 3D speckle tracking requires superior spatial resolution to resolve the positive ultrasound interference patterns (speckles) in 3D and high temporal resolution to track the speckles between frames15. In the present protocol, we describe DIAMOND displacement as a novel myocardial deformation parameter for in vivo quantification of 4D segmental cardiac function in zebrafish. Compared with EF and 2D strain as reference standards, DIAMOND provides additional segmental deformation information without being affected by through-plane motion. By integrating DIAMOND with 4D LSFM, our technique can assess the displacement vector of a heart segment 20–30 µm in width, which is currently impossible for even the most advanced 3D STE system, which has millimeter-range resolution16.
To apply DIAMOND, it is critical to have a comprehensive understanding of the anatomical structure of the embryonic zebrafish heart. During image segmentation, it is essential that the atrioventricular canal and the outflow tract are correctly identified and segmented out from the rest of the myocardium when the user is performing step 6 in the protocol. Furthermore, the horizontal and the vertical long axes of the ventricle must be accurately determined in order to derive the true short axis plane for image resampling in step 8.
The major rate limiting factor of applying DIAMOND is the manual segmentation of the ventricle, which becomes time-consuming when multiple phases during the cardiac cycle may need to be evaluated. With the advancement of machine learning and neural networks, an automated cardiac segmentation method17,18,19,20 could be integrated with DIAMOND to provide monitoring of segmental cardiac function throughout the entire cardiac cycle. Further applications of DIAMOND also include the integration with echocardiography, micro-CT, or micro-MRI, suitable in larger animal models for the multiscale assessment of cardiac injury and regeneration21. However, the method will first require adaptation to the presence of myocardial fibers leading to more complex cardiac deformation including torsion in mammals22,23.
Overall, DIAMOND provides a novel method to evaluate segmental cardiac function in embryonic zebrafish under both physiological and pathological conditions and may be used as a platform for high-throughput in vivo screening of pathways associated with chemotherapy-induced cardiac toxicity.
Offenlegungen
The authors have nothing to disclose.
Acknowledgements
The present work was funded by American Heart Association grants 16SDG30910007 and 18CDA34110338, and by National Institutes of Health grants HL083015, HL111437, HL118650, and HL129727.
Materials
| Amira6 | FEI | Image analyzing software | |
| DAPT | Millipore Sigma | D5942-5MG | |
| Doxorubicin hydrochloride | Millipore Sigma | D1515-10MG | |
| Ethyl 3-aminobenzoate methanesulfonate | Millipore Sigma | E10521-10G | Tricaine |
| MATLAB | MathWorks | Programming environment | |
| MATLAB Image Processing Toolbox | MathWorks | Image processing toolbox |
Referenzen
- Ewer, M. S., Ewer, S. M. Cardiotoxicity of anticancer treatments. Nature Reviews Cardiology. 12 (9), 547-558 (2015).
- Thavendiranathan, P., Wintersperger Bernd, J., Scott, F. D., Thomas D, M. H. Cardiac MRI in the Assessment of Cardiac Injury and Toxicity From Cancer Chemotherapy. Circulation: Cardiovascular Imaging. 6 (6), 1080-1091 (2013).
- Mickoleit, M., et al. High-resolution reconstruction of the beating zebrafish heart. Nature Methods. 11 (9), 919-922 (2014).
- Thavendiranathan, P., et al. Use of Myocardial Strain Imaging by Echocardiography for the Early Detection of Cardiotoxicity in Patients During and After Cancer Chemotherapy. A Systematic Review. 63 (25), 2751-2768 (2014).
- Collier, P., Phelan, D., Klein, A. A Test in Context: Myocardial Strain Measured by Speckle-Tracking Echocardiography. Journal of the American College of Cardiology. 69 (8), 1043-1056 (2017).
- Hanekom, L., Cho, G. Y., Leano, R., Jeffriess, L., Marwick, T. H. Comparison of two-dimensional speckle and tissue Doppler strain measurement during dobutamine stress echocardiography: an angiographic correlation. European Heart Journal. 28 (14), 1765-1772 (2007).
- Poss, K. D., Wilson, L. G., Keating, M. T. Heart regeneration in zebrafish. Science. 298 (5601), 2188-2190 (2002).
- Chen, J., et al. Displacement analysis of myocardial mechanical deformation (DIAMOND) reveals segmental susceptibility to doxorubicin-induced injury and regeneration. JCI Insight. 4 (8), e125362 (2019).
- Messerschmidt, V., et al. Light-sheet Fluorescence Microscopy to Capture 4-Dimensional Images of the Effects of Modulating Shear Stress on the Developing Zebrafish Heart. Journal of Visualized Experiments. (138), e57763 (2018).
- Rosen, J. N., Sweeney, M. F., Mably, J. D. Microinjection of Zebrafish Embryos to Analyze Gene Function. Journal of Visualized Experiments. (25), e1115 (2009).
- Lee, J., et al. 4-Dimensional light-sheet microscopy to elucidate shear stress modulation of cardiac trabeculation. The Journal of Clinical Investigation. 126 (5), 1679-1690 (2016).
- Lenneman, C. G., Sawyer, D. B. Cardio-Oncology: An Update on Cardiotoxicity of Cancer-Related Treatment. Circulation Research. 118 (6), 1008-1020 (2016).
- Geyer, H., et al. Assessment of Myocardial Mechanics Using Speckle Tracking Echocardiography: Fundamentals and Clinical Applications. Journal of the American Society of Echocardiography. 23 (4), 351-369 (2010).
- Castro, P. L., Greenberg, N. L., Drinko, J., Garcia, M. J., Thomas, J. D. Potential pitfalls of strain rate imaging: angle dependency. Biomedical Sciences Instrumentation. 36, 197-202 (2000).
- Seo, Y., Ishizu, T., Aonuma, K. Current Status of 3Dimensional Speckle Tracking Echocardiography: A Review from Our Experiences. Journal of Cardiovascular Ultrasound. 22 (2), 49-57 (2014).
- Amzulescu, M. S., et al. Improvements of Myocardial Deformation Assessment by Three-Dimensional Speckle-Tracking versus Two-Dimensional Speckle-Tracking Revealed by Cardiac Magnetic Resonance Tagging. Journal of the American Society of Echocardiography. 31 (9), 1021-1033 (2018).
- Wolterink, J. M., Leiner, T., Viergever, M. A., Išgum, I., Zuluaga, M. A., et al. . Reconstruction, Segmentation, and Analysis of Medical Images. , 95-102 (2016).
- Avendi, M. R., Kheradvar, A., Jafarkhani, H. A combined deep-learning and deformable-model approach to fully automatic segmentation of the left ventricle in cardiac MRI. Medical Image Analysis. 30, 108-119 (2016).
- Packard, R. R. S., et al. Automated Segmentation of Light-Sheet Fluorescent Imaging to Characterize Experimental Doxorubicin-Induced Cardiac Injury and Repair. Scientific Reports. 7 (1), 8603 (2017).
- Jay Kuo, C. C., Chen, Y. On data-driven Saak transform. Journal of Visual Communication and Image Representation. 50, 237-246 (2018).
- Natarajan, N., et al. Complement Receptor C5aR1 Plays an Evolutionarily Conserved Role in Successful Cardiac Regeneration. Circulation. 137 (20), 2152-2165 (2018).
- Zhukov, L., Barr, A. H. . IEEE Visualization VIS 2003. , 597-602 (2003).
- Nielles-Vallespin, S., et al. In vivo diffusion tensor MRI of the human heart: Reproducibility of breath-hold and navigator-based approaches. Magnetic Resonance in Medicine. 70 (2), 454-465 (2013).

