An In-House-Built and Light-Emitting-Diode-Based Photodynamic Therapy Device for Enhancing Verteporfin Cytotoxicity in a 2D Cell Culture Model
Summary
Here, we describe a novel, simple, and low-cost device to successfully perform in vitro photodynamic therapy (PDT) assays using two-dimensional HeLa cell culture and verteporfin as a photosensitizer.
Abstract
This paper describes a novel, simple, and low-cost device to perform in vitro photodynamic therapy (PDT) assays, named the PhotoACT. The device was built using a set of conventional programmable light-emitting diodes (LEDs), a liquid crystal display (LCD) module, and a light sensor connected to a commercial microcontroller board. The box-based structure of the prototype was made with medium-density fiberboards (MDFs). The internal compartment can simultaneously allocate four cell culture multiwell microplates.
As a proof of concept, we studied the cytotoxic effect of the photosensitizer (PS) verteporfin against the HeLa cell line in two-dimensional (2D) culture. HeLa cells were treated with increasing concentrations of verteporfin for 24 h. The drug-containing supernatant medium was discarded, the adherent cells were washed with phosphate-buffered saline (PBS), and drug-free medium was added. In this study, the effect of verteporfin on cells was examined either without light exposure or after exposure for 1 h to light using red-green-blue (RGB) values of 255, 255, and 255 (average fluence of 49.1 ± 0.6 J/cm2). After 24 h, the cell viability was assessed by the 3-(4,5-dimethyl-2-thiazolyl)-2,5-diphenyltetrazolium bromide (MTT) assay.
Experimental results showed that exposure of cells treated with verteporfin to the light from the device enhances the drug's cytotoxic effect via a mechanism mediated by reactive oxygen species (ROS). In addition, the use of the prototype described in this work was validated by comparing the results with a commercial PDT device. Thus, this LED-based photodynamic therapy prototype represents a good alternative for in vitro studies of PDT.
Introduction
Among the most lethal noncommunicable diseases, cancer represents a global leading cause of premature death. It accounted for nearly 10 million deaths in 2020, representing about one in six deaths worldwide1. Additionally, the multidrug resistance (MDR) phenomenon represents a tremendous public health threat, as approved chemotherapeutic protocols fail to reach remission stages for this clinical condition2. Cancer cells can develop resistance to chemotherapy through several mechanisms; however, the overexpression of some ATP-binding cassette (ABC) transporters – ATP-dependent efflux pumps – is considered the main cause of MDR development within a tumor microenvironment3. In addition to MDR, other cancer complications, such as recurrence and metastasis, reinforce the urgent demand to develop and improve therapeutic approaches to overcome this oncological challenge.
The curative utilization of light has been practiced for centuries4, and photodynamic therapy (PDT) represents a clinically approved therapeutic approach for solid tumors. PDT combines the administration of a photosensitizer (PS) followed by light irradiation to generate reactive oxygen species (ROS) to exert selective cytotoxicity in tumor cells. This therapeutic approach is superior to conventional methods, including surgery, radiation, and chemotherapy5; it is a minimally invasive technique showing lower cytotoxicity in connective tissues6. The light application and PS accumulation directly in the tumor or its microenvironment ensure precise targeting and, consequently, minor, undesirable systemic side effects7 and the possibility of repeated treatment at the same site. Moreover, the cost is lower than that of other approaches. Owing to its promising features, PDT can be considered an appropriate option for both single, especially in the case of inoperable tumors, or adjuvant cancer treatment7, and represents an alternative for MDR related to chemotherapy8,9.
The first report showing a high objective response rate using PDT was described in 1975 in a mouse and rat model10. Since then, studies have been conducted using PDT with positive outcomes7 both in vivo and in vitro with human tumor cell lines in 2D cell culture11,12. Considering the broad applicability of clinically approved PS, regardless of their specific accumulation pathways and wavelength ranges of absorption peaks, the general process is as follows: (i) PS uptake, (ii) peaking of PS concentration at the tumor or its microenvironment, (iii) light application, (iv) PS-light interaction, (v) transfer of PS excited-state energy to either tissue substrate or surrounding oxygen molecules, (vi) ROS production involving singlet oxygen or superoxide anion, (vii) tumor cell death via, essentially, necrosis or apoptosis (direct death), autophagy (cytoprotective mechanism), tissue ischemia (vascular damage), immune modulation, or an overlap of these mechanisms7. In this final stage, the activation of a specific cell death pathway depends on many factors, such as cell characteristics, experimental design and, most importantly, PS intracellular localization and PDT-related targeted damage13.
Verteporfin is a second-generation PS, approved by regulatory agencies for clinical use in Norway and China to treat age-related macular degeneration7. After dose delivery, this prodrug was reported to partially accumulate in mitochondria14 and induce cellular protein tyrosine phosphorylation and DNA fragmentation, leading to tumor cell apoptosis15,16. After 24 h incubation for verteporfin internalization, a PDT protocol using a 690 nm wavelength setup is recommended to achieve effective levels of electromagnetic radiation transfer to adjacent molecules7,17.
Regarding the light source for PDT, the classical diode laser systems are usually expensive, technically complicated, oversized, and thus unportable18,19. As a consequence of its single-wavelength profile, which can also be observed in LED-based PDT equipment, the demand for independent units for each photosensitizer application makes the utilization of diode laser systems even more complex and economically unfeasible20,21. Therefore, the utilization of LED machinery is considered the most promising alternative to solve not only costs22 and maintenance issues, but also to provide high power output and less harmful23 and wider illuminating capability24,25,26,27.
Despite the potential contribution that LED-based equipment can offer to PDT experiments28, most commercial options still possess drawbacks such as a lack of portability, high cost, and complex construction projects and operation29. The main objective of this work was to offer a simple and reliable tool for in vitro PDT assays. This paper describes PhotoACT, an in-house-built LED-based PDT device, which is inexpensive, user-friendly, and portable. As a proof of concept, this device is shown to enhance the cytotoxicity of verteporfin in a 2D cell culture model and, therefore, can be used as a research tool in PDT experiments.
Protocol
NOTE: See the Table of Materials for details related to all materials, reagents, and software used in this protocol.
1. Device construction
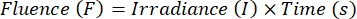
- Saw 3 mm thickn medium-density fiberboards (MDF) to obtain pieces with the dimensions shown in Figure 1A.
NOTE: Use the vector file (Supplemental File 1) for computer numerical control (CNC) cutting. - Build two boxes with the following dimensions (length x width x height ): 330 mm x 235 mm x 225 mm for the bigger boxes, and 300 mm x 220 mm x 150 m for the smaller boxes (Figure 1B).
- Drill the back of the bigger box to install a barrel jack connector. Drill the top of the bigger box andk the top and bottom of the smaller box to provide a passage for electric cables (Figure 1C).
- Paint all the internal surfaces with black ink to promote homogeneous light incidence (Figure 1D).
- Attach, in parallel, three LED tapes with 10 LEDs each at the upper interior surface of the smaller box (Figure 1E).
- Install a brightness sensor at the center of the bottom interior surface of the smaller box (Figure 1F).
- Print the structure of the control unit (Figure 1G) using the 3D printing file (Supplemental File 2).
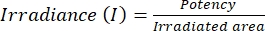
- Install all the components (power button, potentiometers, time/start touchpad, LEDs, brightness sensor, LCD, buzzer, and power supply) at the ports of an ESP32 control board mounted at the control unit interior (Figure 2).
- Upload the programming code (Supplemental File 3, Supplemental File 4, and Supplemental File 5) and run a test to check that all the connections are working (Figure 1H).
- Assemble the boxes and fix them together to avoid gaps, and consequently external light interference and emitted light loss. Attach the mounted control unit to the drilled area at the top of the prototype (Figure 1I).
- Fix a front door of the same material and 330 mm x 225 mm (length x width) dimensions on the bigger box with two small hinges. Also, attach velcro tapes sideways to the bigger box to reinforce the prototype closure (Figure 1J). Install a handle to manipulate the front door of the equipment.
- Attach four rubber foot pads at the bottom of the prototype to ensure more stability during the operations (Figure 1K).
2. Cell lines: cultivation, seeding, and treatment
- Chemicals
- Dissolve the porphyrin in dimethyl sulfoxide (DMSO) to achieve a concentration of 100 mM.
CAUTION: DMSO must be manipulated carefully (handling with the use of personal protective equipment and in a ventilated area). Manipulate both stock and diluted solutions carefully to avoid excessive light exposure.
- Dissolve the porphyrin in dimethyl sulfoxide (DMSO) to achieve a concentration of 100 mM.
- Cell lines
- Cultivate the HeLa cell line in Dulbecco's Modified Eagle's Medium (DMEM) low-glucose medium supplemented with 10% fetal bovine serum and 1% gentamicin.
- Keep the culture flasks in a 5% CO2 cell culture incubator at 37 °C.
- Manage and inspect the cells until they reach 80%-90% confluence.
- Seeding process
- Remove the culture medium from the flask.
- Wash the cell monolayer with PBS.
- Detach the confluent cell culture with trypsin-EDTA (0.5%) 1x for 5 min at 37 °C. Stop the action of trypsin by resuspending the cells with culture medium supplemented with 10% fetal bovine serum and 1% gentamicin.
- Count the resuspended cells with a hemocytometer and seed them into a 96-well plate at 2.0 × 104 cells/well.
- Prepare two plates for dark and light conditions.
- Incubate the plates for 24 h for cell attachment.
- Treatment process
- Remove the medium from both 96-well plates.
- Treat the cells with 100 µL of increasing concentrations of verteporfin (0.045 to 24 µM, serial dilution).
- Incubate the cells with drug treatment for 24 h to allow verteporfin internalization.
- After 24 h, discard the medium containing the drug, wash the monolayer of cells with PBS (100 µL), and add drug-free medium (100 µL).
- Cover one microplate with aluminum foil to protect it from light exposure and incubate it for 24 h. This plate will provide control data for PDT results (dark condition). The other microplate will be utilized on the light exposure condition in the device.
3. Device operation
- Plug the PDT device into the electrical outlet and turn it on by pressing the power button.
- Place the other microplate (light condition) into the PDT device and close the equipment by fastening the front door with the velcro tapes.
- Use the potentiometers to adjust the RGB configuration (a RGB 255, 255, 255 experiment here) and set the color of light emission.
NOTE: Each RGB combination has a specific emission spectrum, which must be adjusted for experiments with different photosensitizers and, consequently, different absorbance curves. - Press the (+)/(-) touchpad to adjust the time configuration (a 60 min experiment here) and set the duration of the assay.
NOTE: The time configuration, in association with the irradiance value, will determine the fluence of the process-the light dose applied in the assay. - Check the setup information at the display.
- Press the Start button to initiate the assay. Ensure that a one-beep buzzer is heard at the beginning of the assay.
- In the course of the experiment, observe real-time information on the display, such as irradiance and time left.
- Do not open the front door or change any configuration during the PDT assay.
- At the end of the assay, wait for a four-beep buzzer and for the electronic system to turn all the LEDs off. Observe a Finished message and the final amount of energy expended-fluence-during the experiment in the display.
NOTE: The fluence final value is calculated using equation (1):
 (1)
(1)
Where F equals to J/cm2 and I equals to mW/cm2 or mJ/s·cm2. The irradiance value considers the potency of the LEDs (emitting source) and the uniformly irradiated area of the dark chamber (660 cm2) (equation [2]):
 (2)
(2)
The theorical irradiance value is shown on the device display throughout the entire PDT assay. At the end of the operation, use equation (3) to calculate the fluence:
Fluence (F) = irradiance (I, constant value) × operation time (s) (3)
4. Cell viability assay
- After the PDT assay, cover the microplate that was exposed to light and incubate for 24 h.
- After the incubation period, remove the culture medium from both plates, wash the monolayer of cells with PBS (100 µL), and add MTT solution (0.5 mg/ml, 100 µL). Incubate both plates-dark and light conditions-for 4 h to allow formazan crystal formation.
- Remove the MTT solution carefully and dissolve the purple crystals with a DMSO/ethanol (1:1) solution.
- After complete dissolution of the crystals, carry out the absorbance measurement using a microplate reader at 595 nm.
NOTE: The device can be used in other important experiments such as ROS-mediated cell death triggered by photosensitizers after light exposure by flow cytometry30.
Representative Results
The final PDT device, named the PhotoACT, included a dark chamber to allocate up to four multiwell microplates, with its upper interior surface equipped with a set of 30 scattered LEDs programmed to emit distinct spectrums of visible light (Figure 3 and Supplemental File 6). The device was built using two associated boxes: an internal box designed as a dark chamber for the PDT assays, and an external box to cover the internal chamber and hold the control unit (Figure 1B). The internal box was painted black (Figure 1D) and composed of a tape model of LED RGB WS2812 (or WS281B) with 30 LEDs and of 1 m length (which was later cut into three pieces) and 9 watts, which holds a built-in processor. This apparatus allowed a more controlled utilization and, consequently, more accurate color emission. The 30 LEDs were equally distributed over the entire upper interior surface of the PDT chamber by three parallel tapes with 10 LEDs each (Figure 1E). A homogeneous light incidence was established due to the low reflectivity of the black interior surfaces and the uniform distribution of LED configuration. A TSL2561 brightness sensor was also incorporated in the bottom center of the internal box to indicate the light incidence and serve as a quality control tool, guaranteeing irradiation uniformity inside the dark chamber (Supplemental Table S1) and monitoring the power of the LED system, which is known to have a certain number of hours of useful life (Figure 1F). The external box is a structure that covers the internal box, composed of six MDF parts, painted gray, and laser-cut for a perfect fit (Figures 1A,B). The control unit was designed using online software31, 3D printed with polylactic acid as a single part using a 3D printer, and painted gray. It holds all the electronics components, including a display, potentiometers, buttons, and a buzzer (Figure 1I and Figure 2).
To enable independent light incidence adjustments, the ESP32 controller board was selected to integrate the control unit (Figure 2). This configuration should allow a USB interface for programming, bluetooth, Wi-Fi, dual core processor, numerous ports, and the ability to communicate with an inter-integrated circuit (I2C), a serial peripheral interface (SPI), and other interfaces. To operate the system, a program was written in C language through an integrated development environment (IDE). The code structure32 is based on FreeRTOS, a free, real-time operational system supported by ESP32 controller board. The referred logic allows independent applications programming, which can be processed by ESP32 in echeloned or parallel approaches, making the project and its maintenance, improvement, and update processes much more versatile and secure.
The interface between the machine and the operator is user-friendly and consisted of a liquid crystal display (LCD), potentiometers, buttons, and a buzzer (Figure 3 and Supplemental File 6). The small, 16 mm x 2 mm (columns vs. lines) LCD had a built-in HD44780 controller with an I2C communication protocol, which confers the ease of installation and transmission versatility, respectively. The preliminary setup includes RGB and time adjustments by the operator. The light magnitude and color configuration can be adjusted using the potentiometers, which modify the intensity (0 to 255) of the three basic color components-RGB. These adjustments can result in several color compositions addressed in the international RGB colors table33. Each RGB composition owns a specific wavelength, which must be adjusted according to the PS used in the PDT experiment; the absorbance curve of the PS and the wavelength of the irradiation must be overlapped for the photoactivation to occur satisfactorily (Supplemental Figure S1). Along the process, the operation status with the time left and light incidence information can be accessed on the LCD.
At the end of the programmed time, the electronics system turned all the LEDs off, emitted an audible warning, and showed on the display the total amount of energy per area (J/cm²), which was calculated by multiplying the constant value of irradiance by the operation time in seconds. This digital model presented a broad range of detection levels (limits between 0.1 and 40,000+ lux), an I2C interface, and a low intensity of electric current (0.5 mA and 15 µA in operation and standby status, respectively).
As a proof of concept, the device was used to enhance the cytotoxic effect of verteporfin in 2D HeLa cell culture after light exposure of 1 h (49.1 ± 0.6 J/cm2). As shown in Figure 4A, the GI50 value was 3.1 µM for the light condition and 13.8 µM for the dark condition. Thus, the 4.4-fold shift comparing the conditions validated the use of verteporfin as a PS and the applicability of PhotoACT to PDT assays. To validate the use of the prototype described in this work, a commercial PDT device was used under the same experimental conditions, including a PS, cells, and fluence, and the results compared. As shown in Figure 4B, both devices photoactivated verteporfin equally, enhancing the cytotoxic effect. These results confirmed the applicability of this in house-built PDT device (Figure 4A,B). Finally, the ROS-mediated cell death triggered by verteporfin after light exposure was confirmed by flow cytometry using DCFDA assay (Figure 4C,D).
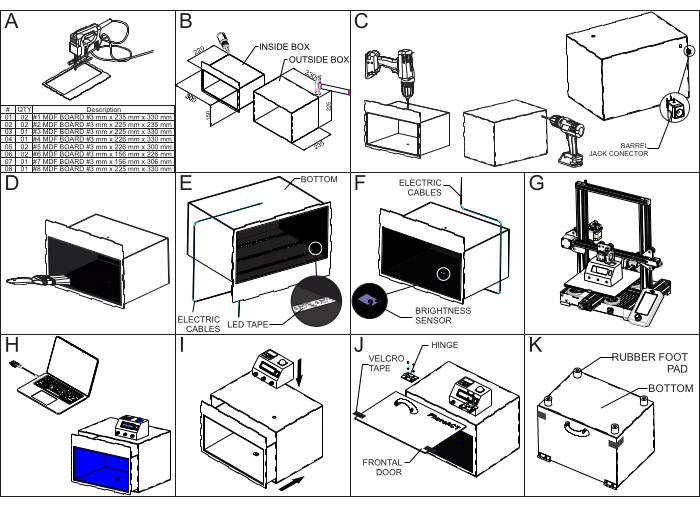
Figure 1: PhotoACT construction and assembly instructions. Detailed illustration of the construction of, drilling, painting, mounting, and accessorizing components into the device. The panel shows a step-by-step guide to build the device. Abbreviation: LED = light-emitting diode. Please click here to view a larger version of this figure.
Figure 2: The control unit construction and electronic installation instructions. Zoomed-in view drawing of exploded control unit and detailed scheme of electronic connections at ESP32 controller board ports with connections and components used in the prototype. Please click here to view a larger version of this figure.
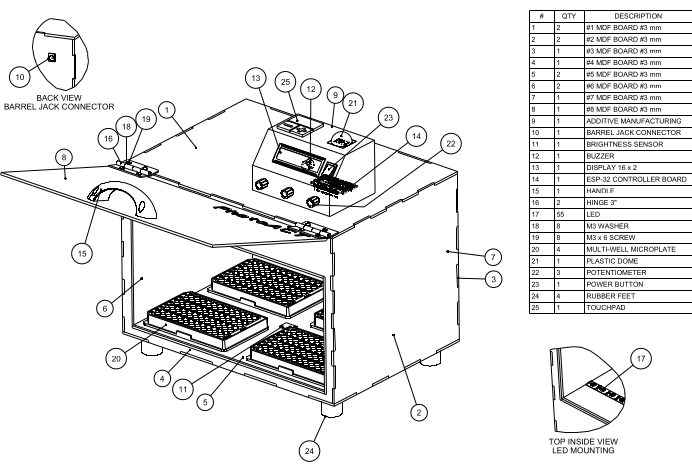
Figure 3: PhotoACT representation. Assembly drawing of the final product design with bill of materials, labelling balloons, and detailed view of the upper interior LEDs. The figure allows to identify parts and components of the prototype. Abbreviations: MDF = medium-density fiberboard; LED = light-emitting diode. Please click here to view a larger version of this figure.
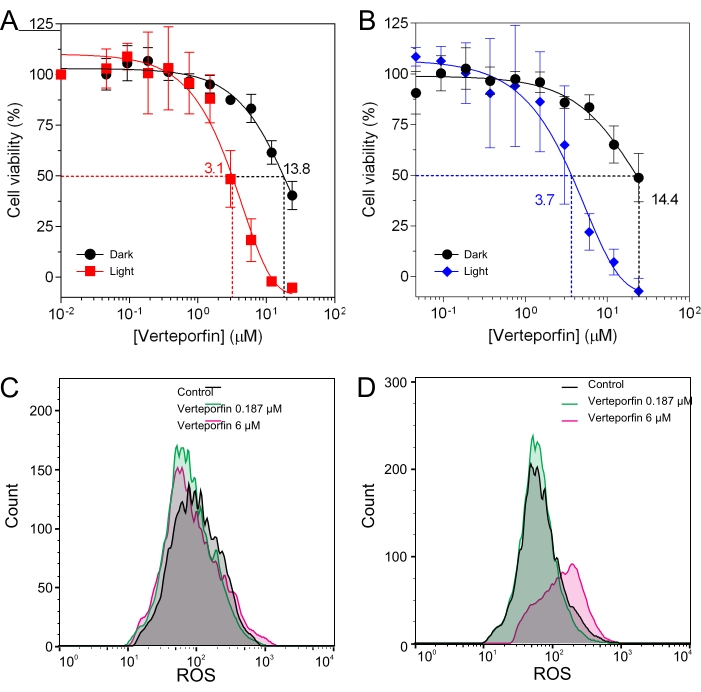
Figure 4: In vitro phototoxicity of verteporfin and ROS generation. (A,B) Cell viability assay performed using the MTT method: the assays were conducted to evaluate the cytotoxic profile of the photosensitizer verteporfin at different concentrations.HeLa cells were treated for 24 h with different concentrations of verteporfin (0.045-24 µM), exposed to light (PhotoACT (A) or commercial PDT equipment (B)) or dark conditions, and then subjected to the MTT assay. Both conditions showed a decreased cell viability at higher concentrations of verteporfin, but the light exposure-obtained from PDT assays-enhanced the cytotoxic profile of the PS, which implies that PDT enhances the cytotoxicity of verteporfin. The viability curves were fitted using GraphPad Prism 6 software. (C,D) HeLa cells were treated for 24 h with low and high concentrations of verteporfin (0.187 µM and 6 µM) and then exposed to light (PhotoACT) or dark conditions. Intracellular ROS levels were measured after irradiation by flow cytometry using DCFDA probe (incubation for 30 min at 1 µM). A right shift among the histograms implied higher fluorescence intensity because of a higher intracellular accumulation of DCF, and thus, greater ROS levels. The results showed no relevant difference in ROS levels in the dark condition (C) but showed a dose-response increase in ROS levels after verteporfin photoactivation (D). Abbreviations: ROS = reactive oxygen species; DCF = 2',7'-dichlorofluorescein; DCFDA = 2',7'-dichlorohydrofluorescein diacetate. Please click here to view a larger version of this figure.
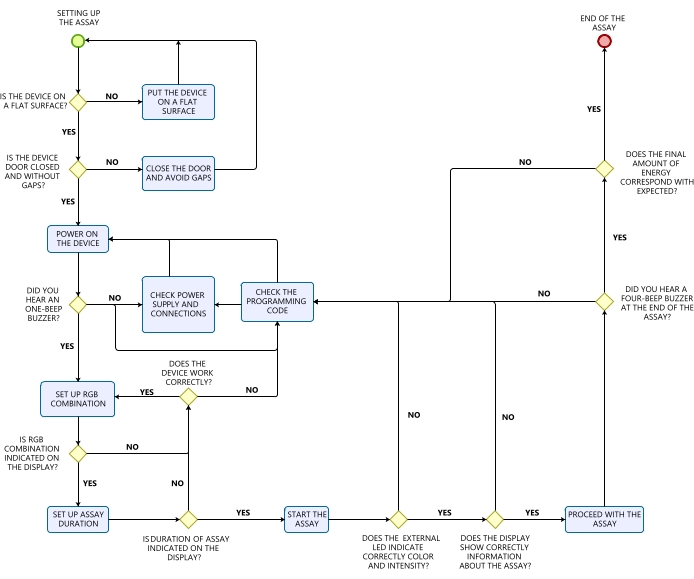
Figure 5: The device's decision flowchart: preliminary setup and operation troubleshooting. Please click here to view a larger version of this figure.
Supplemental Figure S1: Overlap between the absorbance curve of verteporfin and the LED emission spectrum of the device. Absorption spectrum of verteporfin with its specific absorbance peaks (x,y') and LED emission spectrum of RGB 255, 255, 255-white color (3,700K-5,000K CCT) utilized to photoactivate the photosensitizer (x,y''). The overlap between the different absorbance peaks of verteporfin and the white irradiating light corroborates the photoactivation of the photosensitizer, which was also confirmed by the biological results. Please click here to download this File.
Supplemental Table S1: Irradiation uniformity tests. Instant luminosity (lumen) measured by the brightness sensor at different points of the irradiated area. The presented results show no expressive variation, which attest the uniform irradiation of the device. Please click here to download this File.
Supplemental File 1: Vector file for cutting. Drawing (DWG) file for MDF board cutting. The file must be used for computer numerical control (CNC) cutting. Please click here to download this File.
Supplemental File 2: 3D printing file of the unit control's. Stereolithography (STL) file to 3D print the control unit of the device. Please click here to download this File.
Supplemental File 3: C programming code. Programming code developed in C language for configuring the control unit of the equipment. Please click here to download this File.
Supplemental File 4: INO programming code. Programming code developed in INO language for configuring the control unit of the equipment. Please click here to download this File.
Supplemental File 5: Compilation instructions. Markdown (MD) "READ ME" file with additional instructions for programming code compilation. Please click here to download this File.
Supplemental File 6: Design model of the device. Preview of the Standard for the Exchange of Product Data (STEP) tridimensional model file for general visualization of the prototype. Please click here to download this File.
Discussion
The final PhotoACT device was convenient to construct with commercially available, low-cost components at a total cost of less than $50. Additional advantages include low maintenance demands, the capacity to irradiate multiple types of culture plates, the simultaneous use of up to four units per assay, low weight (2 kg)/size (44 cm3) that allows portability, accurate and reproducible irradiation (data not shown), and a user-friendly and simple setup interface that does not require connection to computers or other machines.
Certain critical steps of both construction and operation protocols gave rise to improvement opportunities during project conception. As a PDT chamber requires homogeneous light emission and consistent energy measurement, the internal and external boxes were sealed to avoid both exterior light interference and emitted light loss. Additional velcro tapes were fixed sideways on the frontal door to reinforce the chamber closure and ensure uninterrupted experiments. A representative LED was installed at the control unit to certify the required RGB configuration, indicating the color and intensity of the emitted light during the assay. Finally, the programming code underwent several upgrades to refine instant density measurements and final amounts of energy evaluations, endorsing reproducibility and mathematical consistency. Some other major details that require extra attention include: (i) homogeneous distribution of LEDs and central positioning of the brightness sensor to obtain representative and balanced results, (ii) installation of all components according to the electronic diagram (Figure 2) and programming code (Supplemental File 3, Supplemental File 4, and Supplemental File 5) to ensure correct operation, and (iii) the setup (keeping the same RGB and time configuration) before running an experiment to ensure consistent replicates with reliable results. Although the RGB system provides multiple visible color compositions with specific wavelengths, non-visible light experiments would require specific protocol upgrades. A decision flowchart is presented in Figure 5 to provide a systematic problem-solving approach to find and correct problems or errors during the operation.
Designed to meet the demands of in vitro experimentation with validated results obtained with the therapeutic activation of verteporfin to induce cytotoxicity in 2D HeLa cells (Figure 4), the PhotoACT can be recommended for universities, schools, industries, and other research centers. This device should extend the benefits of PDT to scientific research exploring the mechanism of action of photosensitizers and their clinical applications.
Offenlegungen
The authors have nothing to disclose.
Acknowledgements
We thank Arthur Henrique Gomes de Oliveira and Lucas Julian Cruz Gomes for helping with the filming process. This project was supported by the Brazilian Research Council (CNPq, grant numbers 400953/2016-1-404286/2021-6) and Fundação Araucária-PPSUS 2020/2021 (SUS2020131000003). This study was also financed in part by Coordenação de Aperfeiçoamento de Pessoal de Nível Superior-Brasil (CAPES)-Finance Code 001.
Materials
| 0.5% Trypsin-EDTA (10x) | Gibco | 15400054 | Mammalian cell culture dissociation reagent |
| 3D printer | Flashforge | Finder model | |
| 96-well plates | Non-sterile, polystyrene, and high-binding surface plates with flat bottom wells used for 2D cell culture | ||
| Arduino | |||
| Brightness sensor | TSL2561 model with 0.1-40.000+ lux detection levels and I2C interface | ||
| Buttons | |||
| Buzzer | |||
| Cell culture Flasks | Sterile, polystyrene, rectangular bottom flask with Tissue Culture (TC)-treated surface, canted neck and vent cap (sizes) | ||
| Centrifuge Tubes | Sterile, polypropylene tubes with 15/50 mL capacity used for cell culture dilution at seeding step of the assay | ||
| CO2 Incubator | |||
| Controller board | ESP32 | ||
| Design Software | Trimble | SketchUp | |
| DMEM High Glucose | Gibco | 11965092 | DMEM (Dulbecco's Modified Eagle Medium) is a widely used basal medium for supporting the growth of many different mammalian cells. |
| DMSO | Sigma-Aldrich | D4540-500ML | Dimethyl sulfoxide, ≥99.5% (GC), suitable for plant cell culture |
| Fetal Bovine Serum | Gibco | 12657029 | FBS provides the best value by delivering consistency of cell growth over time and passages. |
| Gentamicin (50 mg/mL) | Gibco | 15750060 | Water-soluble antibiotic drug originally purified from the fungus Micromonospora purpurea. Gentamicin acts by preventing cell culture contamination |
| Hemocytometer | Neubauer patterned chamber used for cell counting at seeding step of the assay | ||
| Inverted Laboratory Microscope | Leica | DM IL LED | |
| Laminar Flow Hood | Cabin designed to protect the working environment from contaminants by maintaining a constant, unidirectional flow of HEPA-filtered air over the work area. Used at several steps of cell cultivation and treatment procedures | ||
| LCD display | |||
| LED RGB WS2812 | 5050 RGB SMD model with a built-in processor. Tape with 30 LEDs, 1 meter length and 9 watts | ||
| MDF fiberboards | 3mm thickness medium-density fiberboards | ||
| Microcentrifuge Tubes | Sterile, polypropylene tubes with safety lid and 1.5/2.0 mL capacity. Convenient tools for manipulating small volumes at treatment step of the assay | ||
| Microplate reader | ThermoFischer | Multiskan FC Microplate Photometer designed to detect a broad wavelength range of absorbance (340-850 nm). The equipment was used to evaluate cell viability after MTT incubation. | |
| MTT Reagent | Invitrogen | M6494 | 3-(4,5-Dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide. Used for cell viability assays |
| Operational System | Real Time Engineers ltd. | FreeRTOS | |
| P10 micripipette | Non-electronic, single-channel, 1-10 μL capacity | ||
| P1000 micropipette | Non-electronic, single-channel, 10-1000 μL capacity | ||
| P200 micropipette | Non-electronic, single-channel, 20-200 μL capacity | ||
| PDT Equipment | LumaCare | Model LC-122 | |
| Phosphate-Buffered Saline pH 7.4 | Gibco | 10010031 | Balanced salt formulation used for washing cells during cultivation and assay procedures |
| Potentiometers | |||
| Tips | Non-sterile, universal fit, 10/200/1000 μL maximum volumes | ||
| Verteporfin | Sigma-Aldrich | SML0534-5MG | Verteporfin, ≥94% (HPLC) |
Referenzen
- Ferlay, J., et al. International agency for research on cancer. Global Cancer Observatory: Cancer Today. 23 (7), 323-326 (2018).
- Gottesman, M. M., Fojo, T., Bates, S. E. Multidrug resistance in cancer: role of Atp-dependent transporters. Nature Reviews Cancer. 2 (1), 48-58 (2002).
- Szakacs, G., Paterson, J. K., Ludwig, J. A., Boothe-Genthe, C., Gottesman, G. A. Targeting multidrug resistance in cancer. Nature Reviews Drug Discovery. 5 (3), 219-234 (2006).
- Ackroyd, R., Kelty, C., Brown, N., Reed, M. The history of photodetection and photodynamic therapy. Photochemistry and Photobiology. 74 (5), 656-669 (2001).
- Hamblin, M. R. Photodynamic therapy for cancer: what’s past is prologue. Photochemistry and Photobiology. 96 (3), 506-516 (2020).
- Barr, H., et al. The contrasting mechanisms of colonic collagen damage between photodynamic therapy and thermal injury. Photochem Photobiol. 46 (5), 795-800 (1987).
- Algorri, J. F., Ochoa, M., Roldán-Varona, P., Rodríguez-Cobo, L., López-Higuera, J. M. Photodynamic therapy: A compendium of latest reviews. Cancers. 13 (17), 4447 (2021).
- Aniogo, E. C., Plackal, B., George, B. P. A., Abrahamse, H. The role of photodynamic therapy on multidrug resistant breast cancer. Cancer Cell International. 19, 91 (2019).
- Spring, B. Q., Rizvi, I., Xu, N., Hasan, T. The role of photodynamic therapy in overcoming cancer drug resistance. Photochemical & Photobiological Sciences. 14 (8), 1476-1491 (2015).
- Dougherty, T. J., Grindey, G. B., Fiel, R., Weishaupt, K. R., Boyle, D. G. Photoradiation therapy. II. Cure of animal tumors with hematoporphyrin and light. Journal of the National Cancer Institute. 55 (1), 115-121 (1975).
- Etcheverry, M. E., Pasquale, M. A., Garavaglia, M. Photodynamic therapy of HeLa cell cultures by using LED or laser sources. Journal of Photochemistry and Photobiology B: Biology. 160, 271-277 (2016).
- Guo, Q., Dong, B., Nan, F., Guan, D., Zhang, Y. 5-Aminolevulinic acid photodynamic therapy in human cervical cancer via the activation of microRNA-143 and suppression of the Bcl-2/Bax signaling pathway. Molecular Medicine Reports. 14 (1), 544-550 (2016).
- Mroz, P., Yaroslavsky, A., Kharkwal, G. B., Hamblin, M. R. Cell death pathways in photodynamic therapy of cancer. Cancers. 3 (2), 2516-2539 (2011).
- Mahalingam, S. M., Ordaz, J. D., Low, P. S. Targeting of a photosensitizer to the mitochondrion enhances the potency of photodynamic therapy. ACS Omega. 3 (6), 6066-6074 (2018).
- Granville, D. J., Levy, J. G., Hunt, D. W. C. Photodynamic treatment with benzoporphyrin derivative monoacid ring A produces protein tyrosine phosphorylation events and DNA fragmentation in murine P815 cells. Photochemistry and Photobiology. 67 (3), 358-362 (1998).
- Castano, A. P., Demidova, T. N., Hamblin, M. R. Mechanisms in photodynamic therapy: part two – cellular signaling, cell metabolism and modes of cell death. Photodiagnosis Photodynamic Therapy. 2 (1), 1-23 (2014).
- Detty, M. R., Gibson, S. L., Wagner, S. J. Current clinical and preclinical photosensitizers for use in photodynamic therapy. Journal of Medicinal Chemistry. 47 (16), 3897-3915 (2004).
- Allison, R. R. Photodynamic therapy: oncologic horizons. Future Oncology. 10 (1), 123-142 (2014).
- Chepurna, O., et al. Photodynamic therapy with laser scanning mode of tumor irradiation. Optical Fibers and Their Applications 2015. 9816, 323-326 (2015).
- Huang, Z. A review of progress in clinical photodynamic therapy. Technology in Cancer Research and Treatment. 4 (3), 283-293 (2005).
- Chepurna, O., et al. LED-based portable light source for photodynamic therapy. Optics in Health Care and Biomedical Optics. 11190, 109-115 (2019).
- Hasson, O., Wishkerman, A. CultureLED: A 3D printer-based LED illumination cultivation system for multi-well culture plates. HardwareX. 12, 00323 (2022).
- Wu, X., et al. Localised light delivery on melanoma cells using optical microneedles. Biomedical Optics Express. 13 (2), 1045-1060 (2022).
- Erkiert-Polguj, A., Halbina, A., Polak-Pacholczyk, I., Rotsztejn, H. Light-emitting diodes in photodynamic therapy in non-melanoma skin cancers-own observations and literature review. Journal of Cosmetic and Laser Therapy. 18 (2), 105-110 (2016).
- Neupane, J., Ghimire, S., Shakya, S., Chaudhary, L., Shrivastava, V. P. Effect of light emitting diodes in the photodynamic therapy of rheumatoid arthritis. Photodiagnosis and Photodynamic Therapy. 7 (1), 44-49 (2010).
- Lins, E. C., et al. A novel 785-nm laser diode-based system for standardization of cell culture irradiation. Photomedicine and Laser Surgery. 31 (10), 466-473 (2013).
- Hopkins, S. L., et al. An In vitro cell irradiation protocol for testing photopharmaceuticals and the effect of blue, green, and red light on human cancer cell lines. Photochemical and Photobiological Sciences. 15 (5), 644-653 (2016).
- Zhang, K., Waguespack, M., Kercher, E. M., Spring, B. Q. An automated and stable LED array illumination system for multiwell plate cell culture photodynamic therapy experiments. Research Square. , 1-18 (2022).
- Gálvez, E. N., et al. Analysis and evaluation of the operational characteristics of a new photodynamic therapy device. Photodiagnosis and Photodynamic Therapy. 37, 102719 (2022).
- Bretin, L., et al. Photodynamic therapy activity of new human colorectal cancer. Cancers. 11 (10), 1474 (2019).
- . T. SketchUp Available from: https://www.sketchup.com/ (2022)
- LCDR PhotoDynamic Therapy (PDT) Equipment Repository. GitHub, Inc Available from: https://github.com/PhotoDynamicTherapy (2022)
- W3C CSS Color Module Level 3. W3C, Inc Available from: https://www.w3.org/TR/css-color-3/#SRGB (2022)

