An Automated Method for Assessing Visual Acuity in Infants and Toddlers Using an Eye-Tracking System
Summary
In this paper, we present a novel automated method for assessing visual acuity in infants and toddlers by using an eye-tracking system.
Abstract
Visual acuity measurement is an important visual function test to perform in infancy and childhood. However, accurate visual acuity measurement in infants is difficult because of deficiencies in their communication ability. This paper presents a novel automated method to assess visual acuity in children (5-36 months old). This method, the automated acuity card procedure (AACP), uses a webcam for eye tracking and recognizes children’s watching behaviors automatically. A two-choice preferential-looking test is performed when the tested child watches the visual stimuli shown on a high-resolution digital display screen. When the tested child watches the stimuli, their facial pictures are recorded by the webcam. These pictures are used by the set computer program to analyze their watching behavior. With this procedure, the child’s eye movement responses to different stimuli are measured, and their visual acuity is assessed without communication. By comparing the results with grating acuity obtained by Teller Acuity Cards (TACs), AACP performance is deemed comparable to that of TACs.
Introduction
The infantile period is a critical period for visual development. Visual problems that arise early in life can have a significant impact on a child's development. It is important to be able to perform a quantitative visual assessment in infants, which can help detect early vision problems. However, because infants are not cognitively developed or expressive enough to recognize visual acuity chart symbols, such as letters or graphs, measuring their visual acuity is difficult. The current gold standard for infant vision assessment is the acuity card procedure1 based on the preferential looking test2. However, because this method requires experienced testers to judge visual acuity by observing the child's eye movements3,4,5,6, it is limited by the experience of the testers4,5. Therefore, acuity card procedures, such as Teller Acuity Cards (TACs)5,6, remain a subjective method. Thus, there is a need for a method that can quantitatively measure visual acuity in infants and young children, that can be used without the need for verbal communication and that is not limited by requiring experienced testers.
The invention and use of the remote eye tracker enabled an automated acuity measuring system to be developed. In previous studies, eye-tracking methods have been used as a tool for visual function evaluation in children7,8,9,10. A remote eye tracker can be used for gaze tracking and is a substitute for a tester's observation of a child's eye movements. The ACTIVE procedure7 and AVAT procedure10 are fully automated visual acuity tests with a remote eye tracker; they have yielded comparable visual acuity results to the Keeler Acuity Cards test in healthy infants and young children. As opposed to other recent studies, we used a webcam instead of a remote eye tracker to capture the child's gaze. We invented an eye movement data automatic acquisition method based on computer vision. The procedure combined the eye movement acquisition method with the preferential looking technique in assessing visual function in children.
This paper aims to present a novel automated method, which can evaluate visual acuity in young children, called the automated acuity card procedure (AACP). This procedure is particularly useful for infants and younger children who have not yet acquired sufficient communication skills. The key aspect is that visual responses can be quantitated to yield grating acuity in infants and young children. Grating acuity measurement enables the detection of visual pathologies and plays an important role in subsequent medical management.
Protocol
The protocol described here was approved by the Ethical Committee of Peking University First Hospital (PKUFH 2018-223). The procedures adhered to the tenets of the Declaration of Helsinki for research involving human subjects. The study format was described, and informed consent was obtained from the parents of the participants.
1. Preparation of the apparatus
NOTE: The AACP components were set up in a mildly illuminated test room. Drapes were pulled in the room to avoid interference from sunlight. A display system, a recording system, and an analysis system were the three components of the AACP (Figure 1).
- Set up a display system, a 28 inch liquid-crystal display monitor (62.208 cm x 34.992 cm screen, 3840 pixels x 2160 pixels, 0.162 mm/pixel, 30 Hz frame rate). Place the display monitor on a table that can be raised. Linearize the screen luminance by an 8-bit look-up table. Set the luminance at 1 cd/m2, 200 cd/m2, and 400 cd/m2 for black, mid-gray, and white, respectively.
- Place two side panels on either side of the screen to reduce distractions for the children being tested.
- Set up a recording system, a high-definition pro webcam with a resolution of 1080 pixels/30 fps.
NOTE: The webcam records image sequences of testers' behaviors, each cropped at 1280 pixels x 720 pixels. During automated acuity testing, one time-stamped webcam image is obtained every 200 ms for synchronization. - Connect the display monitor and webcam to a computer, the analysis system. Ensure that the webcam is located in the center, directly below the screen, and is able to be adjusted as needed.
NOTE: The monitor and webcam are either integrated with the computer (a laptop or desktop PC) or are separate devices that are then attached to a computer. - Install the AACP procedure software on the computer for the presentation of stimuli and the analysis of eye movements. The AACP procedure software (China National Invention Patents, No. 201910865074.4 and No. 201510919621.4) comprises a stimulus displaying module, a vision testing module, and a testing result processing module.
- Set the visual stimuli as a 12 cm x 12 cm square-wave grating with different period/degree (cpd) spatial frequencies and a contrast ratio of 1.00. Ensure that the stimulus is displayed randomly in the center of the left or right portion of the screen, and that the rest of the screen shows a luminance-matched gray area similar to the TACII.
NOTE: At the detection distance of 55 cm (which is consistent with that of TACII), the stimuli were approximately the same (due to pixel size limitations) as those on printed TACII cards (16 cards, 1/2 octave).
2. Eye-tracking calibration
- Obtain informed consent from the parents, and describe the study format to them.
- Position the child at a distance of 55 cm from the display monitor. Let the child sit alone on a chair or, preferably, on the parent's lap. If the child sits alone, let the parent sit alongside the child.
- Adjust the position of the lifting table and place it with the monitor. Arrange the screen perpendicular to the child's eyes.
- Adjust the position of the webcam to ensure that the child's face is visible in the recording system and to avoid capturing faces other than the child's.
- Prior to starting the procedure, inform the child that they will be watching the screen. Instruct the parent to prompt the child to look at the screen when the child is not paying attention. No specific instructions are necessary during the test.
- Open the AACP procedure software. Type the child's information into the software (name, sex, age).
- Click on the Start button. The software starts the calibration procedure. A graphics interchange format (GIF) image (2.0736 cm x 2.0736 cm, 128 x 128 pixels) appears against the white background in the center of the screen (Figure 2). The image and background music appears simultaneously. This stimulus is presented for at least 3 s. The analysis system simultaneously determines whether the child's line of sight is fixated on the image. If no gaze data are available within 1 min during this presentation, the screen presents another cartoon GIF image. When gaze coordinates are detected within this region, the test procedure starts without the actions of the tester and runs automatically.
3. Testing procedure
- Present the initial grating. The spatial frequencies of the gratings range from 0.33-30.0 cpd in 1/2 octave steps. Determine the initial grating by the child's age, as in the TACII test.
- Present the initial grating for 1,000 ms, which is the length of a trial. Then, present a blank screen for 200 ms. Present the same stimulus again, followed by a blank screen again. Present the grating of the same spatial frequency set three times.
- During execution of the procedure, let the webcam record the child's facial pictures. The software uses these pictures to analyze their watching behavior. The vision testing program checks the eye movement responses with the criteria stated in Table 1 to determine whether the stimulus has been seen (Figure 3).
- Let the testing result processing program present the subsequent stimulus, according to the protocol shown in Figure 411.
- After every three trials, present a GIF image (with background music) as a visual reward to maintain the child's interest. If no gaze data are usable (e.g., if the child turned around or had their eyes closed) within 1 min of the GIF image presentation, stop the test. This test outputs no result.
- After performing steps 3.4 and 3.5, analyze the grating acuity results for the child outputted by the software programs.
Representative Results
The AACP was applied to one group of children11: 155 normally developing infants and toddlers (5 to 36 months old, based on gestational age). In a previously published study, the grating acuity results obtained by the AACP were compared with those obtained by TACII. The results obtained by these two procedures are significantly correlated (r153 = 0.83, p < 0.001). Only 10.32% (16 of 155) of the children's results differed by more than one octave. Among them, eight children were 5-7 months old. Of these 16 children, three had visual acuity results obtained by the AACP that were 1.5-2 octaves over those obtained by TACII. The other 13 children had AACP visual acuity 1.5-2 octaves below TACII visual acuity.
The grating acuity measured by the AACP gradually increased as infant age increased. Figure 5 shows the change in grating acuity measured by the AACP with the change in age in months. From 6 to 12 months, the grating acuity increased by nearly 0.5 octaves. From 12 to 24 months, the grating acuity increased by almost one octave. From 24 to 36 months, the grating acuity increased by nearly 1.5 octaves. The trend of acuity development in this study is consistent with the results of acuity measured by TACII in previous studies12. It is also consistent with the acuity development measured by TACII in the same group of infants11.
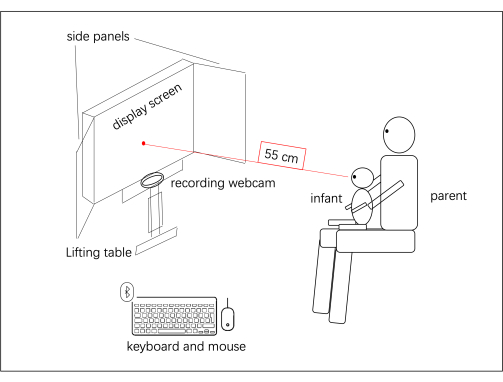
Figure 1: AACP apparatus. The AACP components and the spatial arrangement of their setup in the test room are shown. The infant was seated on a parent's lap and viewed the stimuli binocularly at a distance of 55 cm. Please click here to view a larger version of this figure.
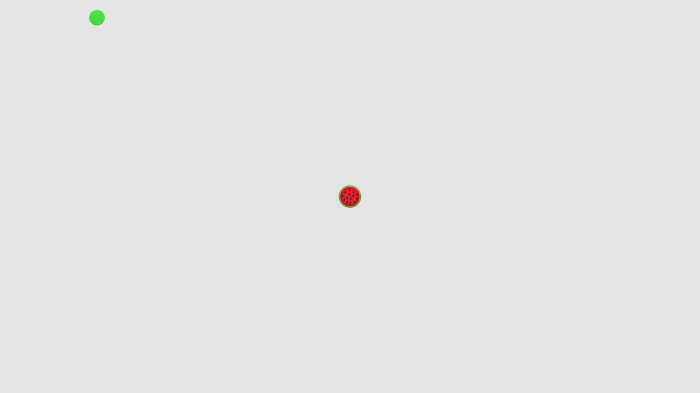
Figure 2: Cartoon stimulus in the calibration procedure. The cartoon stimulus is a GIF image with background music. The stimulus attracts visual attention. When the child's gaze falls within the image area, the dot changes from red to green, and the calibration procedure is performed. This figure has been modified with permission from Wen et al.11. Please click here to view a larger version of this figure.
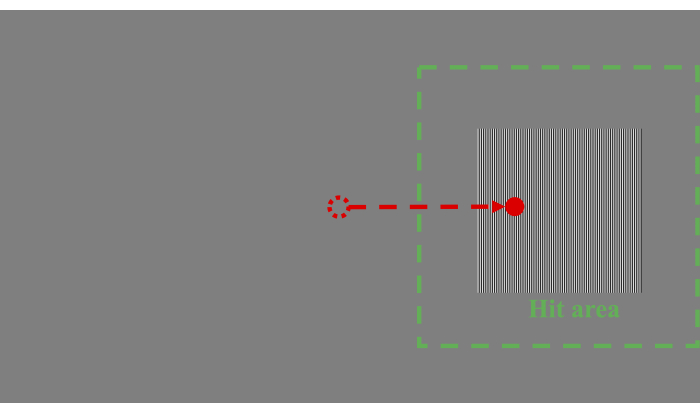
Figure 3: Grating stimulus in the testing procedure. The grating stimulus is a grating of vertical black-and-white stripes presented on a uniform gray background. The gaze point of the participant moving from the center to the green square indicates that the participant has watched the target, which means a "hit". The gaze point of the participant moving from the center to the empty area indicates that the participant did not watch the target, which means a "miss". The green square area has a half-side length based on the distance from the center of the stimulus to the side of the screen (i.e., from the center of the stimulus to the left edge of the screen in this figure). This figure has been modified with permission from Wen et al.11. Please click here to view a larger version of this figure.
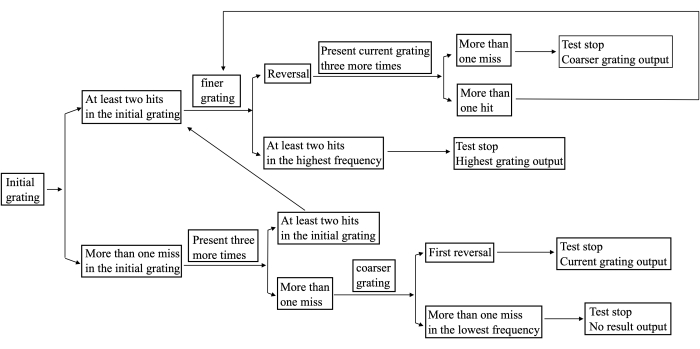
Figure 4: The protocol used in the AACP procedure. This figure has been modified with permission from Wen et al.11. Please click here to view a larger version of this figure.
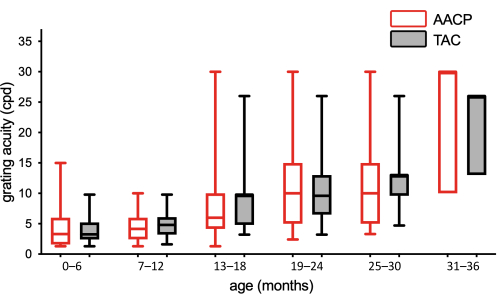
Figure 5: Box plots of grating acuities plotted against age (N = 155). White boxes with red lines and gray boxes with black lines are grating acuities of the AACP and TACII11, respectively, for every 6 months of age. Please click here to view a larger version of this figure.
| Criterion | Verify that the gaze signal: | |||
| Hit | remained in the target area continuously for more than 400 ms of the 1,000 ms target presentation. | |||
| Miss | (1) did not enter the target area within a time window of 1,000 ms. (2) remained in the target area less than 400 ms. | |||
Table 1: Criteria to establish whether a stimulus has been seen.
Discussion
Several studies7,8,9,10 based on the eye-tracking method have shown the value of this method in evaluating infants and young children who have difficulty in verbal communication. However, the number of participants in previous studies is relatively small. Only 30 infants under 12 months of age were tested by the ACTIVE procedure, which was developed by Jones et al.7. The AVAT procedure, which was developed by Vrabic et al.10, tested 35 infants and young children similarly. In the present study, a large sample of 5- to 36-month-old infants and toddlers (N = 155) was tested by the AACP procedure and showed high testability and comparable visual acuity evaluation to TACs. In addition, the use of a webcam instead of a remote eye tracker to follow the child's gaze makes the AACP equipment less expensive and more convenient to access.
When infants grow up, they show increasing interest in the various stimuli in the surrounding environment. Therefore, it is a challenge for them to maintain cooperation during the test. Displaying cartoon images in the center of the screen was designed to attract their attention, which is similar to the ACTIVE procedure7. Every three trials, before changing the grating frequency, a cartoon image was presented as a visual reward to maintain the infant's attention and attract their gaze toward the center of the screen, thus reducing the misjudgment of the procedure caused by the infant's eye gaze shifting to the side. Moreover, two attached screen side panels were used to reduce distractions for infants. In the standard TAC test in laboratory settings13, acuity cards are shown through a rectangular opening on a gray screen that includes attached side panels. We set the screen side panels to reduce the interference of the surrounding environment, but the side panels can be disassembled to adapt to other testing environments.
In the present study, digital stimuli for the AACP and printed stimuli for TACs were square-wave gratings, which have "edge effects". Edge artifacts at the junction of high-frequency gratings and isoluminant background provide potentially additional visual cues for children, which occur in the AACP and TACs14 tests. However, compared with paper-based TACs, digital stimuli are more flexible. Gabor-modulated stimuli will be used in the future to avoid edge effects. The contrast, size, frequency, and other characteristics of digital stimuli are easier to adjust. At the detection distance of 55 cm in this study, the spatial frequencies of the gratings ranged from 0.33 to 30.0 cpd. If a child has very poor visual acuity, such as below 0.33 cpd, their actual visual acuity cannot be detected by the AACP. In further studies, different ranges of frequencies may be set with different detection distances to be applicable to children with more visual conditions.
Another limitation of the existing method is that the duration of a trial, which is 1 s, is too short for some younger infants to distinguish the grating. Among the children whose visual results differed by more than one octave in the AACP and TACs, half were children aged 5-7 months. In future applications, different trial durations may be set to adjust to different participants' ages. At present, the parent can observe the infant's performance during the test. If the infant fails the test due to moving or fatigue, the test can be repeated.
The AACP is a novel eye-tracking method based on webcam data. It can be used to evaluate grating acuity in infants and toddlers, and the results are comparable to the gold standard visual acuity test. By requiring only eye movements as overt indicators of responses, the AACP can be used to measure visual acuity in a fully automated manner. In the future, by changing the types of visual stimulation, the AACP may be used to evaluate other visual information processing functions early in children's development.
Disclosures
The authors have nothing to disclose.
Acknowledgements
This study was supported by Capital's Fund for Health Improvement and Research (No. 2018-2Z-4076) and Peking University First Hospital SEED Research Funds (2019SF31).
Materials
| AACP procedure software | In-house | In-house | The AACP procedure software (China National Invention Patents, No. 201910865074.4 and No. 201510919621.4) comprises a stimulus displaying module, a vision testing module, and a testing result processing module. |
| Computer processor | Intel Corporation, Santa Clara, CA, USA | Intel CORE i7-6500U processor | Analysis system |
| Display monitor | InnoLux Co., Ltd., China | InnoLux M280DGJ-L30 | Display system |
| Webcam | Logitech International S.A., Lausanne, Switzerland | Logitech C920 high-definition pro webcam | Recording system |
References
- Teller, D. Y., McDonald, M. A., Preston, K., Sebris, S. L., Dobson, V. Assessment of visual acuity in infants and children: the acuity card procedure. Developmental Medicine and Child Neurology. 28 (6), 779-789 (1986).
- Teller, D. Y. The forced-choice preferential looking procedure: a psychophysical technique for use with human infants. Infant Behavior and Development. 2, 135-153 (1979).
- Preston, K. L., McDonald, M., Sebris, S. L., Dobson, V., Teller, D. Y. Validation of the acuity card procedure for assessment of infants with ocular disorders. Ophthalmology. 94 (6), 644-653 (1987).
- Mohn, G., vanHof-van Duin, J., Fetter, W. P., de Groot, L., Hage, M. Acuity assessment of non-verbal infants and children: clinical experience with the acuity card procedure. Developmental Medicine and Child Neurology. 30 (2), 232-244 (1988).
- Cavallini, A., et al. Visual acuity in the first two years of life in healthy term newborns: an experience with the teller acuity cards. Functional Neurology. 17 (2), 87-92 (2002).
- Clifford, C. E., Haynes, B. M., Dobson, V. Are norms based on the original teller acuity cards appropriate for use with the new teller acuity cards II. Journal of American Association for Pediatric Ophthalmology and Strabismus. 9 (5), 475-479 (2005).
- Jones, P. R., Kalwarowsky, S., Atkinson, J., Braddick, O. J., Nardini, M. Automated measurement of resolution acuity in infants using remote eye-tracking. Investigative Ophthalmology & Visual Science. 55 (12), 8102-8110 (2014).
- Hathibelagal, A. R., Leat, S. J., Irving, E. L., Nandakumar, K., Eizenman, M. Measuring infant visual acuity with gaze tracker monitored visual fixation. Optometry and Vision Science. 92 (7), 823-833 (2015).
- Barsingerhorn, A. D., Boonstra, F. N., Goossens, J. Saccade latencies during a preferential looking task and objective scoring of grating acuity in children with and without visual impairments. Acta Ophthalmologica. 97 (6), 616-625 (2019).
- Vrabič, N., Juroš, B., Tekavčič Pompe, M. Automated visual acuity evaluation based on preferential looking technique and controlled with remote eye tracking. Ophthalmic Research. 64 (3), 389-397 (2021).
- Wen, J., Yang, B., Li, X., Cui, J., Wang, L. Automated assessment of grating acuity in infants and toddlers using an eye-tracking system. Journal of Vision. 22 (12), 8 (2022).
- Leone, J. F., Mitchell, P., Kifley, A., Rose, K. A. Normative visual acuity in infants and preschool-aged children in Sydney. Acta Ophthalmologica. 92 (7), e521-e529 (2014).
- Clifford-Donaldson, C. E., Haynes, B. M., Dobson, V. Teller Acuity Card norms with and without use of a testing stage. Journal of AAPOS. 10 (6), 547-551 (2006).
- Robinson, J., Moseley, M., Fielder, A. Grating acuity cards-spurious resolution and the edge artifact. Clinical Vision Sciences. 3 (4), 285-288 (1988).

