Passive Administration of Monoclonal Antibodies Against H. capsulatum and Others Fungal Pathogens
Summary
C57BL/6 mice have been used to study Hc pathogenesis and provide the best model. We are exploring the potential benefits of humoral immunity against this fungus and generated several mAbs [to histone H2B and a heat shock protein 60kDa] that we tested for their protective efficacy after intraperitoneal administration.
Abstract
The purpose of the use of this methodology is 1) to advance our capacity to protect individuals with antibody or vaccine for preventing or treating histoplasmosis caused by the fungus Histoplasma capsulatum and 2) to examine the role of virulence factors as target for therapy. To generate mAbs, mice are immunized, the immune responses are assessed using a solid phase ELISA system developed in our laboratory, and the best responder mice are selected for isolation of splenocytes for fusion with hybridoma cells. C57BL/6 mice have been extensively used to study H. capsulatum pathogenesis and provide the best model for obtaining the data required. In order to assess the role of the mAbs in infection, mice are intraperitoneally administered with either mAb to H. capsulatum or isotype matched control mAb and then infected by either intravenous (i.v.), intraperitoneal (i.p.), or intranasal (i.n.) routes. In the scientific literature, efficacy of mAbs for fungal infections in mice relies on mortality as an end point, in conjunction with colony formin units (CFU) assessments at earlier time points. Survival (time to death) studies are necessary as they best represent human disease. Thus, efficacy of our intervention would not adequately be established without survival curves. This is also true for establishing efficacy of vaccine or testing of mutants for virulence. With histoplasmosis, the mice often go from being energetic to dead over several hours. The capacity of an intervention such as the administration of a mAb may initially protect an animal from disease, but the disease can relapse which would not be realized in short CFU experiments. In addition to survival and fungal burden assays, we examine the inflammatory responses to infection (histology, cellular recruitment, cytokine responses). For survival/time to death experiments, the mice are infected and monitored at least twice daily for signs of morbidity. To assess fungal burden, histopathology, and cytokine responses, the mice are euthanized at various times after infection. Animal experiments are performed according to the guidelines of the Institute for Animal Studies of the Albert Einstein College of Medicine.
Protocol
1. Growth of H. Capsulatum
- Prepare a biosafety cabinet for work with the fungus by cleaning the cabinet with 10% bleach followed by 20 min UV irradiation. H. capsulatum in the yeast phase requires Biosafety level (BSL) II practices, while the mould form requires BSLIII. Use yeast form in the following steps.
- Next prepare a 15 ml conical tube with 5 ml of PBS. Harvest a colony of H. capsulatum (strain Hc ATCC G217B) from a BHI blood agar plate [glucose 10 g/L, cysteine 0.1 g/L, penicillin-streptomycin 1% and sheep red blood cells 50 ml/L (Colorado Serum Co., Colorado, USA)] cultivated at 37°C or take an aliquot from frozen yeast stock at -80°C and add it to the PBS. Vortex the cells vigorously and centrifuge for 1100 x g for 10 min at room temperature. Carefully remove the supernatant without disturbing the pellet and add 10mL of fresh PBS. Repeat this procedure three times. Suspend the cells in 5mL of PBS and tranfer to a 50 mL conical tube.
- To disrupt aggregated cells, pass the yeast cell suspension through a 26G1/2 needle using a 10mL syringe 5 times in a biosafety cabinet (using facial protection). To isolate small, uniformly-sized yeast, centrifuge the cells at 55 x g for 1 min at room temperature and then remove the top 1 ml.
- Add the cell suspension to an sterile erlenmeyer flask containing 100 ml of HAM F12 medium (GIBCO) supplemented with 16g/L glucose, 1g/L glutamic acid, 8.4mg/L cystine, 6g/L glutamic acid and then grow the cells at 37° C for 48 h in an incubator with 150rpm shaking.
2. Hybridoma Growth and Purification of Monoclonal Antibodies
- Transfer the selected hybridomas to DMEM medium containing 10% fetal calf serum, 10% NCTC, 1% non-essential amino acids and 1% Penicillin-Streptomycin. Grow the cells in a cell culture flask (Becton Dickenson) for 5-7 days at 37°C/5%CO2.
- Then centrifuge the medium at 1100 x g for 10 min at room temperature and collect all the supernatant without disrupting the pellets.
- Next, purify the cell free supernatant using a protein A/G resin by FPLC.
- The mAb concentration can then be calculated by a capture ELISA (1) using an IgG isotype control as standard (Figure 1B).
3. Histoplasma Capsulatum Inoculum Preparation
- Take a 48 h Histoplasma capsulatum (strain Hc ATCC G217B) yeast phase culture grown in HAM F-12 medium.
- Centrifuge the cells at 1100 x g for 10 min. Discard the supernatant and add fresh PBS.
- Repeat the 3.2 procedure 3 times.
- Pass the yeast cell suspension 5 times through a 26G1/2 needle using a syringe.
- Centrifuge the suspension at 55 x g for 1 min to pellet residual cell clusters. Transfer the supernatant containing the single cell suspension to a new tube.
- Enumerate the single cell suspension using a hematocytometer.
- Adjust the cell concentration in order to achieve 1.25 x 107 yeast (survival) or 5.0 x 106 (CFU, cytokines and histology) in a suspention of <50 μL (Figure 2).
4. Intraperitoneal Administration of the MAbs
- Pick up the mouse by its tail and the scruff of the neck (Fig 3A). Immobilize the mouse by the scruff of its neck as close to theears as possible (make sure to take up enough skin so that the mouse cannotturn its head to bite the person handling it; Figure 3B and 3C).
- Stabilize the tail withthe little finger gently pressed against the palm of the hand (Figure 3D).
- Swab the injection area with 70% ethanol before placing the needle and to aspirate to look for blood before injecting.
- Use the 26G1/2 to piercethe skin and abdominalmuscles to inject the mAb solution containing 500μg (PBS, isotype control antibody or the mAb to be tested, diluted in 1 mL PBS) into thelower left or lower right abdominal quadrant (intraperitoneal cavity),with the animal in the head down position, taking care to avoid the diaphragm andother internal organs (Figure 3E).
- Wait briefly before withdrawing the needleto reduce the likelihood of leakage.
- Wait a minimum of two hours before proceeding to the next step.
5. Mouse Anesthesia and Intranasal Infections
- Prepare the anesthesia using ketamine and xylazine at 100 mg/Kg and 10 mg/Kg, respectively. Perform intraperitoneal administration of PBS, isotype control antibody, or experimental antibody as described in the accompanying written protocol. Wait two hours after mAb injection before anesthetizing the mouse and proceeding with the intranasal infection.
Prepare anesthesia using ketamine and xylazine at 100 mg/Kg and 10 mg/Kg, respectively (7).
- During the 2h waiting period, prepare the Histoplasma capsulum inoculum as described in the accompanying written protocol.
- Proceed according to the itens 5.1 to 5.5. Toe pinch the animals with a tweezer and to verify the absence of reflex and confirm that the anesthesia worked. After anaesthetization, gently suspend the mouse by its front teeth to an nylon or cotton string. Use 2 column stands to tie the strings in order to suspend the animals.
- Slowly administer approximately 50 μl inoculum into a nare using a micropipette while closely monitoring the mouse’s respiration rate. Allow the mouse to rest in this position for 2-5 min after intranasal infection to facilitate the deposition of the yeast into the animal’s lungs (Figure 3F).
- After the mouse has been infected, maintain the mouse in a monitored, warm environment (temperature between 25 and 37°C), carefully utilizing a heat lamp if necessary , until it recovers from the anesthesia. When the mouse awakes, return it to a clean cage with ad libitum access to food and water. The cages are returned to our animal facility and kept in a clean animal room (BLSI).
6. Survival Studies
- Assess infected and mock-infected animals clinically for tachypnea, lethargy, obtundation, and weight loss. The animals should be checked twice daily by laboratory members and daily by Animal Caretakers.
- With murine histoplasmosis, until close to the end of life, there are typically no apparent signs of the infection other than a mild increase in respiration rate. With advanced disease, which usually happens from 10-11 days, the mice become significantly tachypneic and have diminished activity. Typically they rapidly become moribund and expire.
- Distressed animals should be euthanized appropriately with CO2 in a dedicated chamber, Deceased animals should be enumerated daily.
7. CFU Studies, Histology and Cytokines Studies
- Prepare 15 ml conical tubes with 10mL PBS for each organ to be collected.
- Euthanize animals 7 and 14 days after infection with a sublethal inuculum (5.0 x 106) as previously shown and remove the lung, spleen and liver immediately.
- Remove a piece of the organ to be evaluated and perform the fixation in formalin overnight. The sections will be examined under the microscope for pathological evaluation.
- Prepare 50 ml conical tubes with 5mL PBS topped with 70 μm cell strainers for each organ to be homogenized. Macerate each remaining portion of the organs seperately into the 50 mL tubes using sterile 5mL syringe plungers.
- Next, serially dilute organ homogenates (1:100, 1:1000 and 1:5000) and plate 100μL of each dilution on BHI-blood agar plates (2).
- Add protease inhibitor tablets to the homogenates according to the manufacture’s instructions (Roche, Germany).
- Incubate plates at 37°C for up to 14 days and enumerate CFUs.
- Centrifuge the organ homogenates at 4000xg for 10 min and remove organ supernatants, whish will be used in used in the cytokine assays performed by standard methods according to the manufacturer.
8. Monoclonal Antibody Protection Against H. Capsulatum is Dependent on Antibody Specificity and Isotype
- MAb isotype is critical in protection against H. capsulatum, as mice treated with IgG1 or IgG2a mAbs to Hsp60 have significantly prolonged survival compared to control mice receiving an IgG2b mAb to Hsp60 or either an isotype control mAb or PBS (Figure 4).
- Further, in mice that received protective mAbs, there was a significant reduction in the number of pulmonary and splenic CFU at day 7 and decreases of 2 and 2.5 log units of yeast numbers in the lungs at day 14 (Figure 5).
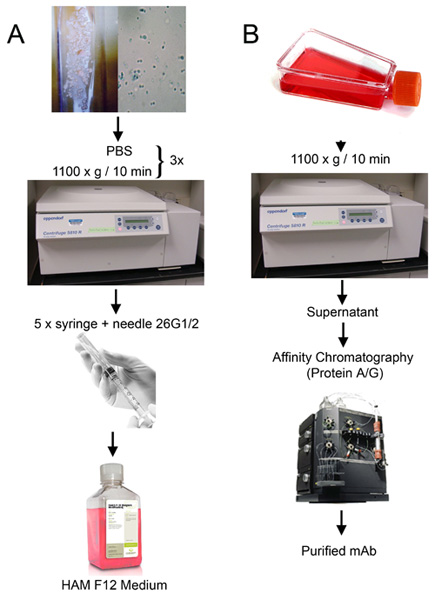
Figure 1: Growth of H. capsulatum and hybridomas. (A) Liquid HAM F-12 culture preparation from a single colony obtained from H. capsulatum grown on a BHI-blood agar plates. (B) Hybridoma growth in cell culture flasks and mAb purification by protein A/G resin using affinity cromatography.
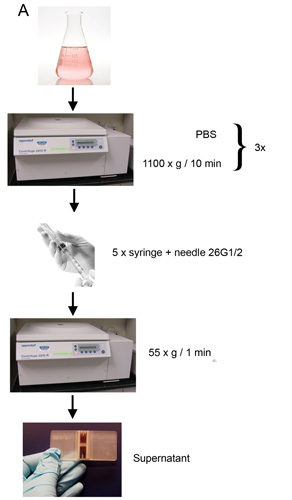
Figure 2: H. capsulatum inoculum preparation for intranasal infection. Cell suspension obtained after H. capsulatum agregates disruption by syringe and centrifugation is enumerated by counting in a hemocytometer. Cell concentration is adjusted to 1.25 x 107 (survival experiments) or 5 x 106 (CFUs, cytokines and histology) in <50 μL.
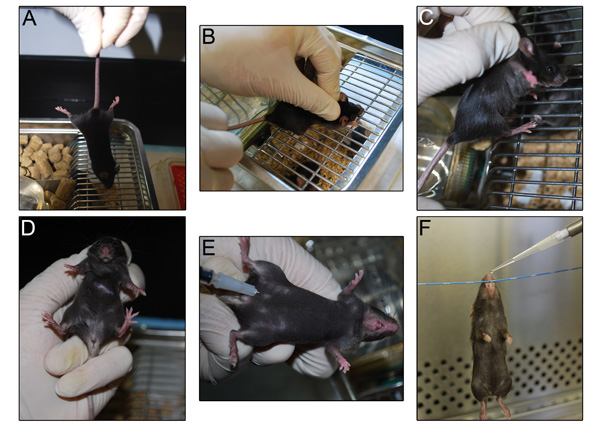
Figure 3: Mouse handling during mAb administration. (A) The mouse is picked up by the tail and (B and C) immobilized by holding the scruff of its neck as close to theears. (D) The tail is held between the little finger and palm. (E) The mAb solution is injected using a 26G1/2 needle. (F) The H. capsulatum inoculum is administered intranasally by gently pipetting the cell suspension into a nare.
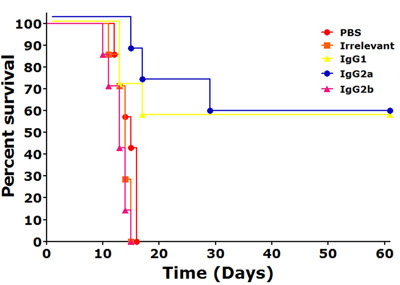
Figure 4: MAbs to Hsp60 can alter the pathogenesis of histoplasmosis. i.p. injections with 500 μg of IgG1 ,or IgG2a mAbs 2 h prior to infection significantly prolonged survival (p<0.05, compared to controls), but an IgG2b mAb.
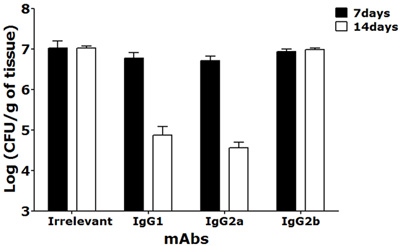
Figure 5: CFU determinations in lungs at 7 and 14 days after a sublethal intranasal challenge with 5×106 Hc yeasts of mice treated i.p. with selected mAbs to Hsp60 or irrelevant mAb showed reduction in fungal burden for IgG1 and IgG2a mAbs treated animals. Black bars represent CFUs at day 7 and white bars 14 days post-infection (*p<0.001 at 7 days and **p<0.001 at 14 days post infection).
Discussion
The protocol presented here demonstrates that mAb’s to H. capsulatum can modify the course of experimental murine histoplasmosis. MAbs to cell surface antigens of pathogens can modify the complex dynamics that occur during the interplay between a host and a pathogen. This study establishes that mAbs mediate protection in a murine model of lethal histoplasmosis when injected intraperitoneally, and it suggests candidate proteins for vaccine development, such as H2B, M antigen (surface catalase)(3) and Hsp60. In vivo, administration of protective mAbs to Hc Hsp60 and H2B reduced organ fungal burden and inflammation and prolonged survival of infected mice.
Although vaccine development for H. capsulatum is an exciting area of research, vaccination may not be effective in immunocompromised individuals, since they cannot necessarily orchestrate an immunoresponse. Hence, it is clear that this population may benefit mostly from passive therapy with mAb to H. capsulatum antigens. Our data suggest that mAbs, especially to Hsp60 or in combination with other mAbs to cell surface antigens, could improve the treatment of patients with histoplasmosis (4, 6). Additionally, combination of a mAb to H. capsulatum with antifungal drug therapy can be synergistic and more effective in protective efficacy. Amphotericin B is the drug of choice and usually used for initial treatment of histoplasmosis. Hence, the addition of mAb to antifungal drug therapy should be considered in future studies. In fact, we have previously demonstrated a synergistic effect of mAbs to H2B and sub-inhibitory concentrations of amphotericin B in our animal model (5). Furthermore, mAbs could be administered prophylactically in outbreaks of histoplasmosis, especially to high-risk individuals, such as individuals with human immunodeficiency virus infection or patients receiving TNF-α inhibitors. Future investigations of protective mAb may reveal additional important insights into the pathogenesis of histoplasmosis and antibody function against H. capsulatum and, perhaps, other intracellular pathogens.
Divulgaciones
The authors have nothing to disclose.
Materials
| Name of Material | Company |
|---|---|
| Biological safety cabinet (BSL2) | |
| 15 mL conical tubes | Falcon, BD |
| HAM F-12 medium | Gibco |
| 37°C shaker | |
| Vortex | |
| 50 mL conical tubes | Falcon, BD |
| 26G1/2 needle | BD |
| 10 mL syringe | BD |
| 250 mL flasks | |
| FPLC (Fast protein liquid chromatography) system | GE Helthcare |
| ELISA reader | BioTek |
| Anesthesia (ketamine and Xylazine) | |
| Column stands | |
| Nylon string | |
| Heat lamp | |
| 70μm cell strainers | Falcon, BD |
| BHI agar plates | Gibco |
Referencias
- Casadevall, A., Mukherjee, J., Scharff, M. D. Monoclonal antibody based ELISAs for cryptococcal polysaccharide. J. Immunol. Methods. 154, 27-35 (1992).
- Guimaraes, A. J., Frases, S., Gomez, F. J., Zancope-Oliveira, R. M., Nosanchuk, J. D. Monoclonal antibodies to heat shock protein 60 alter the pathogenesis of Histoplasma capsulatum. Infect Immun 77. , 1357-1367 (2009).
- Guimaraes, A. J., Hamilton, A. J., de M Guedes, H. L., Nosanchuk, J. D., Zancope-Oliveira, R. M. Biological function and molecular mapping of M antigen in yeast phase of Histoplasma capsulatum. PLoS One. 3, e3449-e3449 (2008).
- Nosanchuk, J. D. Protective antibodies and endemic dimorphic fungi. Curr Mol Med. 5, 435-442 (2005).
- Nosanchuk, J. D., Steenbergen, J. N., Shi, L., Jr, D. e. e. p. e., &, G. S., Casadevall, A. Antibodies to a cell surface histone-like protein protect against Histoplasma capsulatum. J Clin Invest. 112, 1164-1175 (2003).
- Nosanchuk, J. D., Steenbergen, J. N., Shi, L., Deepe, G. S., , ., Casadevall, A. Antibodies to a cell surface histone-like protein protect against Histoplasma capsulatum. J. Clin. Invest. 112, 1164-1175 (2003).
- Smith, W. Responses of laboratory animals to some injectable anaesthetics. Lab Anim. 27, 30-39 (1993).

