Fabrication of High Contact-Density, Flat-Interface Nerve Electrodes for Recording and Stimulation Applications
Summary
This article provides a detailed description on the fabrication process of a high contact-density flat interface nerve electrode (FINE). This electrode is optimized for recording and stimulating neural activity selectively within peripheral nerves.
Abstract
Many attempts have been made to manufacture multi-contact nerve cuff electrodes that are safe, robust and reliable for long term neuroprosthetic applications. This protocol describes a fabrication technique of a modified cylindrical nerve cuff electrode to meet these criteria. Minimum computer-aided design and manufacturing (CAD and CAM) skills are necessary to consistently produce cuffs with high precision (contact placement 0.51 ± 0.04 mm) and various cuff sizes. The precision in spatially distributing the contacts and the ability to retain a predefined geometry accomplished with this design are two criteria essential to optimize the cuff's interface for selective recording and stimulation. The presented design also maximizes the flexibility in the longitudinal direction while maintaining sufficient rigidity in the transverse direction to reshape the nerve by using materials with different elasticities. The expansion of the cuff's cross sectional area as a result of increasing the pressure inside the cuff was observed to be 25% at 67 mm Hg. This test demonstrates the flexibility of the cuff and its response to nerve swelling post-implant. The stability of the contacts' interface and recording quality were also examined with contacts' impedance and signal-to-noise ratio metrics from a chronically implanted cuff (7.5 months), and observed to be 2.55 ± 0.25 kΩ and 5.10 ± 0.81 dB respectively.
Introduction
Interfacing with the peripheral nervous system (PNS) provides access to highly-processed neural command signals as they travel to different structures within the body. These signals are generated by axons confined within fascicles and surrounded by tightly-jointed perineurium cells. The magnitude of the measurable potentials resulting from the neural activities is affected by the impedance of the various layers within the nerve such as the highly resistive perineurium layer that surrounds the fascicles. Consequently, two interface approaches have been explored depending on the recording location with respect to the perineurium layer, namely intrafascicular and extrafascicular approaches. Intra-fascicular approaches place the electrodes inside the fascicles. Examples of these approaches are the Utah array17, the Longitudinal Intra-fascicular Electrode (LIFE)18, and the transverse intra-fascicular multichannel electrode (TIME)32. These techniques can record selectively from the nerve but have not been shown to reliably retain functionality for long periods of time in vivo, likely due to the size and the compliance of the electrode12.
Extra-fascicular approaches place the contacts around the nerve. The cuff electrodes used in these approaches do not compromise the perineurium nor the epineurium and have been shown to be both a safe and robust means of recording from the peripheral nervous system12. However, extra-fascicular approaches lack the ability to measure single unit activity — compared to intra-fascicular designs. Neuroprosthetic applications that utilize nerve cuff electrodes include activation of the lower extremity, the bladder, the diaphragm, treatment of chronic pain, block of neural conduction, sensory feedback, and recording electroneurograms1. Potential applications to utilize peripheral nerve interfacing include restoring movement to victims of paralysis with functional electrical stimulation, recording motor neuron activity from residual nerves to control powered limb prostheses in amputees, and interfacing with the autonomic nervous system to deliver bio-electronic medicines20.
A design implementation of the cuff electrode is the flat-interface nerve electrode (FINE)21. This design reshapes the nerve into a flat-cross section with larger circumference compared to a round shape. The advantages of this design are increased number of contacts that can be placed on the nerve, and the close proximity of the contacts with the rearranged internal fascicles for selective recording and stimulation. Furthermore, upper and lower extremity nerves in large animals and human can take various shapes and the reshaping generated by the FINE does not distort the natural geometry of the nerve. Recent trials have shown that FINE is capable of restoring sensation in the upper extremity16 and restoring movement in the lower extremity22 with functional electrical stimulation in humans.
The basic structure of a cuff electrode consists of placing several metal contacts on the surface of a nerve segment, and then insulating these contacts along with the nerve segment within a nonconductive cuff. To achieve this basic structure, several designs have been proposed in previous studies including:
(1) Metal contacts embedded into a Dacron mesh. The mesh is then wrapped around the nerve and the resulting cuff shape follows the nerve geometry4, 5.
(2) Split-cylinder designs which use pre-shaped rigid and non-conductive cylinders to fix the contacts around the nerve. The nerve segment that receives this cuff is reshaped into the cuff's internal geometry6–8.
(3) Self-coiling designs where the contacts are enclosed between two insulation layers. The internal layer is fused while stretched with an external un-stretched layer. With different natural resting lengths for the two bonded layers causes the final structure to form a flexible spiral that wraps itself around the nerve. The material used for these layers have typically been polyethylene9 polyimide10, and silicone rubber1.
(4) Uninsulated segments of the lead wires placed against the nerve to serve as the electrode contacts. These leads are either woven into silicone tubing11 or molded in silicone nested cylinders12. A similar principle was used to construct FINEs by arranging and fusing insulated wires to form an array, and then an opening through the insulation is made by stripping a small segment through the middle of these joined wires13. These designs assume a round nerve cross section and conform to this assumed nerve geometry.
(5) Flexible polyimide based electrodes33 with contacts formed by micromachining polyimide structure, and then integrating into stretched silicone sheets to form self-coiling cuffs. This design also assumes a round nerve cross section.
Cuff electrodes should be flexible and self-sizing in order to avoid stretching and compressing the nerve that can cause nerve damage3. Some of the known mechanisms by which cuff electrodes can induce these effects are the transmission of forces from adjacent muscles to the cuff and hence to the nerve, mismatch between the cuff's and nerve's mechanical properties, and the undue tension in the cuff's leads. These safety issues lead to specific set of design constraints on the mechanical flexibility, geometric configuration, and size1. These criteria are particularly challenging in the case of a high contact count FINE because the cuff must be at the same time stiff in the transverse direction to reshape the nerve and flexible in the longitudinal direction to prevent damage as well as accommodating multiple contacts. Self-sizing spiral designs can accommodate multiple contacts cuff14, but the resulting cuff is somewhat rigid. Flexible polyimide design can accommodate a high number of contacts but are prone to delamination. The wire array design13 produces a FINE with flat cross section, but in order to retain this geometry the wires are fused together along the length of the cuff producing stiff faces and sharp edges making then unsuitable for long term implants.
The fabrication technique described in this article produces a high contact density FINE with flexible structure that can be made by hand with consistently high precision. It uses a rigid polymer (Polyether ether ketone (PEEK)) to allow precise placement of the contacts. The PEEK segment maintains a flat cross section at the center of the electrode while remaining flexible in the longitudinal direction along the nerve. This design also minimizes the overall thickness and stiffness of the cuff since the electrode body does not have to be rigid in order to flatten the nerve or secure the contacts.
Protocol
1. Electrode Components Preparation
- Gather four electrode components that require precision cut (laser-cut was used, Please refer to the Materials List) prior to the manufacturing process. These components are (Figure 1):
Contacts array frame: This frame is made out of 125 µm thick Polyether ether ketone (PEEK) sheet. It covers the entire width of the cuff and holds the middle contacts and has serpentine-shaped edges (Figure 1B). The middle contacts are wrapped in the guide channels; hence the exposed width of the contacts is limited by the width of the channels and the spacing is determined by the spacing between the channels.
The middle contacts strips: The middle contacts are formed by wrapping these strips around the contacts array frame (Figure 1B). Cut the strips out of the Platinum/10% Iridium sheet to the width of the guiding channels and add extra length to allow them to be fully folded around the frame. Spot-weld the contact's lead at 0º angle with the strip's major axis.
The reference contacts: Four references are needed. The long dimension of these contacts is slightly shorter than the cuff width to fully contain them inside the cuff. Spot weld each reference contact to a lead at 90º angle with the contact's major axis.
PEEK spacers: Spacers are used to create thinner region on the electrode to allow bending and closing (Figure 1C). All the spacers are made from PEEK (other material could be used) and cut to the length of the electrode. The width of the middle space is equal to the height of the electrode.
2. Contacts Array Preparation
- Clean the components made in step 1 by sonication in ethanol for 2 min at 40 KHz and room temperature, then 2 min in distilled deionized water under the same sonication parameters. Let dry.
- Visually inspect the contacts for any defects like laser-cut residuals or surface deformations.
- Position the contacts one by one under the microscope with the welding spot facing up. Hold the contact with tweezers at approximately 1/3 of length starting from the free end. Elevate the lead to a 45º angle while holding the contact to make the first bend.
- Place the pre-bent contact underneath the array frame with the weld facing up. Hold the frame down with tweezers and elevate the lead to a 45º angle to make a second bend. While Continuing holding the frame down, grab the free end of the contact with tweezers and bend at a 180º angle (fold toward the middle line of the frame).
- Straighten and pull the contact toward operator and then bend at 180º angle (fold to the middle line). The spot welding point should now be enclosed in between the two bent ends.
- Repeat steps 2.3 – 2.5 for the remaining contacts. Make as tight as possible. Alternate the contact leads on each side of the array frame.
3. Cuff Layout Guide
- Create a 2D diagram of the cuff in flat open position.
NOTE: Use any CAD software to produce a true-scale diagram. This diagram will determine the dimensions of the electrode and the placement site for the various electrode components. - Print the 2D diagram on regular printing paper to scale using ordinary printing machine, and then cut out a 5 cm by 5 cm square piece with the drawing located in the center.
- Cut out 5 cm by 5 cm square piece of the thermal transparency sheet (T1) with a scalpel.
- Place the transparency piece T1 on top of the diagram paper, and then place both layers on the base plate with the diagram facing up. Tape them down to the base plate with adhesive tape.
4. Electrode Base Layer and Reference Contacts Placement
- Cut out 5 cm by 5 cm silicone sheet with a scalpel (S1), and then place it on the transparency layer. Start by dropping one corner then slowly lower the rest of the sheet to avoid trapping air bubbles in between T1 and S1 sheets (Figure 2A).
- Mix approximately 2 g of uncured silicone as directed on manufacturer data sheet. Rigorously stir the two parts together with sterilized wooden stirring stick. Place the mix in a vacuum chamber for 3 min. Cycle the vacuum to eliminate the bubbles as they rise to surface. Preheat the isotemp oven at 130 ºC.
Note: Latex gloves can inhibit the curing process of the silicone. Latex gloves also contain sulfur which can leave contaminants on the working surfaces. Using nitrile gloves instead is recommended. - Using the dental pick tool, apply a thin line of uncured silicone along the middle of the spacer segments where they are located on the guiding diagram.
- Place the spacers onto the designated regions, and then press them down against the silicone sheet S1.
- Partially cure the silicone in the isotemp oven for 30 min, let it cool down for 10 min.
- Place the reference contacts onto designated areas. Ensure that the weld points are facing up and contact leads are routed towards the midline of the cuff to exit at the far end. After ensuring correct positioning, press the contacts down onto the silicone layer S1. Deposit uncured silicone into the through-holes.
- Tape down the leads and then fully cure the silicone at 130 ºC for 90 min, or overnight at room temperature (Figure 2B).
5. Center Contacts Array Placement
- Cut out 1.5 cm by 5 cm transparency piece with a scalpel (T2). Tape down the reference leads away from the middle region to prevent them from running underneath the contacts array during the next step.
- Place the contact arrays on the dedicated location with the leads side facing up. Deposit uncured silicone to tack the array in place.
- Place the piece from 5.1 (T2) across the midline of the electrode and over the arrays to hold them down, and then tape the ends while pressing down on the arrays. Manually align the array with the dedicated position. Tape down the leads outside the cuff's perimeter.
- Place the small fixture bar across the center of the electrode and over the transparency segment T2. Clamp it down to the base plate with moderate pressure to press the middle contacts against the base silicone layer S1.
- Fully cure the silicone for 90 min at 130 ºC, or overnight at RT.
6. Embedding the Electrode Components
- Remove the small fixture bar and gently remove the transparent sheet T2 to expose the middle contact arrays. Remove all the tapes that hold the leads for both references and middle contacts (Figure 2C).
- Cut a square piece of the transparency sheet with a scalpel to the same width of the electrode and 5 cm in length (T3), and then cut a square piece of silicone sheet to cover the entire electrode surface (S2).
- Lay the silicone sheet (S2) on top of the transparency piece (T3) and stretch it to remove any waves or irregularities and to eliminate air bubbles from being trapped in between.
- Cut four pieces of silicone tubing; 5 cm long each. Place them on the exit site of the leads as assigned on the guiding diagram. Leave a 2 mm space between the electrode edge and the tubes' edges. While holding down each pair of tubes with tweezers, tape down the tubes starting at 1 mm away from the tube end. Repeat for the other pair.
- Arrange and leads of the middle contacts and the references into bundles, and then pass them through the corresponding tube near the exit sites. Repeat for the other three tubes. (Figure 2D).
- Deposit generous amount of uncured silicone over the entire electrode body.
NOTE: Avoid forming air bubbles during this step by either slowly pouring the uncured silicone from the vacuumed mixing container or injecting it with a syringe. - Place the structure from 6.3 on top of the deposited uncured silicone with the silicone sheet S2 facing down. Align the transparency piece T3 with the electrode while keeping the silicone sheet S2 adhered to it.
- Tape down the transparency piece T3 and then apply pressure to channel out any trapped air bubbles. Place the large fixture bar across the center of the electrode and over the transparency segment T3. Then clamp it down to the base plate with moderate pressure. Fully cure the silicone for 90 min at 130 ºC, or overnight at RT.
7. Shielding Layer Placement (Recommended for Recording Cuffs)
- Remove the large fixture bar and delaminate the transparency piece (T3) with tweezers. Place the shielding sheet in the center of each face of the electrode and apply slight pressure to press them into the electrode. Deposit uncured silicone into the through-holes.
- Partially cure the silicone for 30 min at 130 ºC, and then let it cool completely to room temperature. Place adhesive tape over the outer ends of the electrode and over the closing flanges to prevent adding extra uncured silicone to these segments.
- Repeat steps 6.6 through 6.8.
8. Cutting out the Finished Electrode
- Peel off and cut the excess silicone on top of the adhesive tape added in step 7.2 using scalpel blade, then carefully remove the adhesive tape.
- Cut out windows through the silicone to expose the spacer segments through the S2 layer. Extract the embedded spacer segments with tweezers. This step will leave voids and form flexible single silicone sheet at these regions (originally S1).
- Peel off the excess silicone on top of the adhesive tapes that cover the silicone tubes, and then cut it with scalpel blade to level the tubes with the electrode body.
- Cut around the perimeter of the electrode down to base plate.
- Cut out a triangle between each tubes pair completely through the base plate, and on the outer side following the guiding diagram to shape the leads' exit sites. Remove all the silicone material that was detached from the electrode body during last steps.
9. Exposing Contacts and Shielding Layers
- Cut out windows through the silicone layer S2 that covers the shielding layer. Glide the polypropylene suture filament in between the electrode base (layer S1) and the transparent layer T1 on the base plate to delaminate the finished cuff electrode.
- Flip the electrode such that the center contacts and the Silicone layer S1 are facing up, and then expose them by cutting out windows through the base silicone layer S1. Repeat for the outer reference contacts exposing 1 mm wide segments along the center of the contacts. Ensure that the stabilizing through-holes at the sides of the reference contacts are fully embedded inside the electrode's body.
10. Soldering a Connector to the Leads
- Deposit soldering substance onto the leads and onto the connecter pins separately, and then heat and fuse both parts together with soldering iron.
Note: The DFT lead wires consist of silver core surrounded by an outer layer made out of the Nickel-Cobalt base alloy MP35N. Depositing the solder substance onto these wires requires the use of specialty flux to allow adhering to the wire (please refer to the Materials List).
Representative Results
Recording neural activity was performed with a customized pre-amplifier using super-β input instrumentation amplifier (700 Hz – 7 kHz bandwidth and total gain of 2,000). An example of the fabricated FINE electrode with the presented protocol is shown in Figure 3. Implanting the FINE around the nerve is done by suturing the two free edges together. A demonstration of the cuff's flexibility (Figure 3B) indicates that the cuff flattens the nerve while retaining flexibility in the longitudinal direction.
In addition to the cuff flexibility in the longitudinal direction, the cuff should also be elastic to accommodate nerve swelling, especially at the early healing stages post-implantation. High pressure inside the cuff could constrict blood vessels and occlude blood flow inside the nerve. Consequently, the pressure generated inside the cuff as a result of nerve swelling should not exceed the diastolic blood pressure. Figure 4 shows the response of the assembled cuff to various pressure levels inside the cuff. As the pressure increases, the electrode expands to form a larger cross sectional area. At 67 mm Hg; the electrode expands to 1.25 times its original cross sectional area. This observation can be interpreted as if the cuff size is at least 1.2 times the initial cross sectional area of the nerve, the nerve can expand up to 1.5 its initial cross sectional area while the resulting increase in pressure inside the cuff remains under 67 mm Hg. Therefore the design criterion15, 30, 31 for a nerve cuff electrode to exhibit a cuff-to-nerve cross sectional area ratio of at least 1.5 is satisfied.
The functionality and stability of the manufactured cuff design was examined by implanting it on the sciatic nerve of a dog (Figure 5). The study was approved by CWRU IACUC and ACURO. Three parameters were periodically measured through the chronic implant duration: 1) the signal-to-noise ratio (SNR), 2) the contact impedance and 3) the number of contacts that provide viable recording. The SNR is defined as the ratio of neural activity mean power (red segment) over the mean power of baseline activity (yellow segment). 100 ms moving window was used. Throughout the 7.5-month implant duration, the SNR remained steady with a value of 5.10 ± 0.81 dB (Figure 5B).
The magnitude of contacts' impedance was measured in vivo at 1 kHz and is shown in Figure 5C. These measurements were made using the RHD2000-Series amplifier evaluation system. The impedance was observed to be stable with a mean value of 2.55 ± 0.25 kΩ (33 Trials, 16 contacts (N= 528)). Finally, the number of contacts that became inactive over time is also shown in Figure 5C. The number of inactive contacts remained under 2 for the duration of the implant. The fluctuation in the number of excluded channels resulted mostly from a bad connection between the external connector and the amplifier and regained function during the recording sessions.
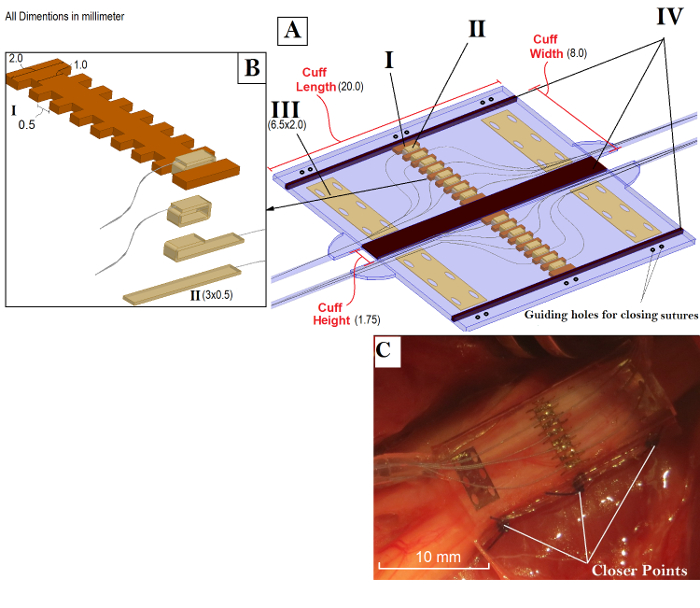
Figure 1: Overview of the FINE and its Components. A) FINE in the open position and the four main building components that require precision cut. These components are: Contacts array frame (I), the middle contacts strips (II), the reference contacts (III), PEEK spacers (IV). The cuff is facing downward with respect to the contacts placement against the nerve. The spacers (IV) are removed after the assembly. B) An expanded view of the center contacts and the steps to fold and fix them around the middle frame. C) Folded configuration of the electrode. Please click here to view a larger version of this figure.
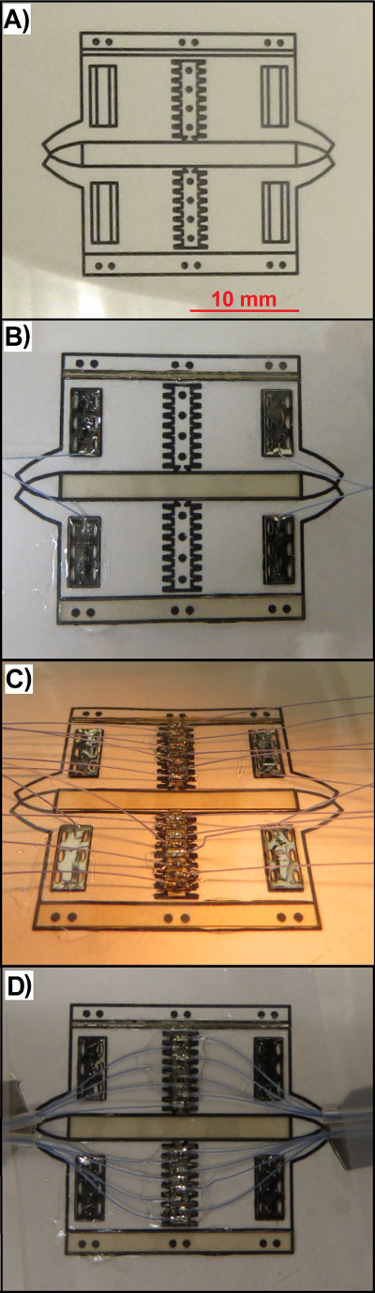
Figure 2: Snapshots of the Electrode during the Fabrication Process. A) The guiding diagram, T1 and S1 stacks at the end of step 4.1. B) Mounting the spacer segments and reference contacts at the end of step 4.7. C) Adhering the center contacts array to S1 sheet at the end of step 6.1. D) Arranging the leads and silicone tube before embedding them inside the electrode body at the end of step 6.5. Please click here to view a larger version of this figure.
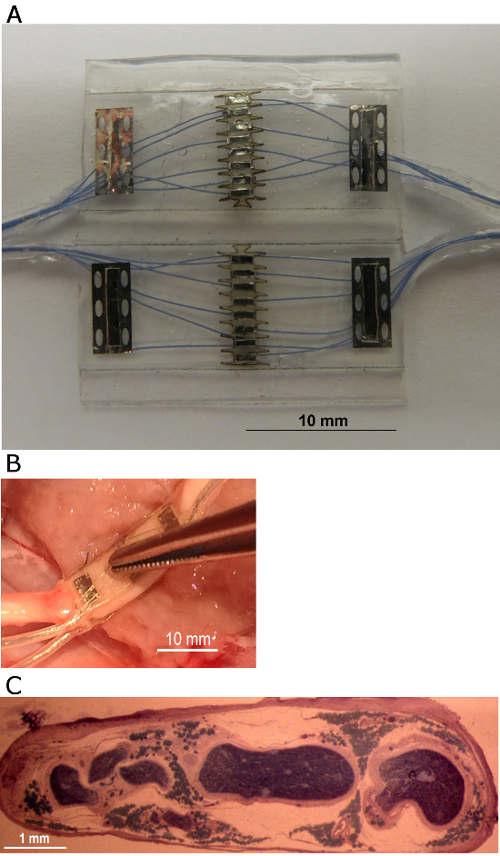
Figure 3: The Nerve Cuff Electrode Described in the Protocol. A) The fabricated 16 -contacts FINE in the open position. The leads are arranged into four bundles of 5 leads per exit site. B) An example of the placement of the cuff around the sciatic nerve in dog. The middle segment of the FINE remained flat in the transverse direction, and the cuff body is flexible in the longitudinal direction. C) A photograph of implanted nerve post mortem showing the flattened cross section and the arrangement of the fascicles after implanting a FINE electrode for 12 weeks. Please click here to view a larger version of this figure.
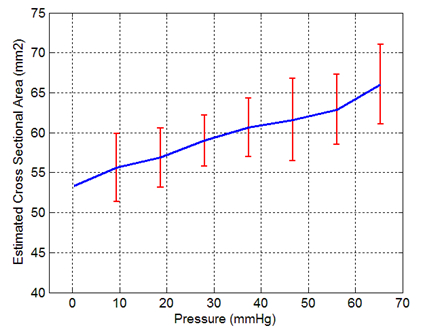
Figure 4: FINE Response to Increasing Internal Pressure. These measurements were made by placing an inflatable elastic chamber inside a closed cuff, and then the pressure was gradually increased by a variable -length water column. The major and minor axes of the cuff's cross section were measured at each pressure level and an elliptic cross section was assumed in order to calculate the cross sectional area (n= 20). The error bars represent the standard deviation.
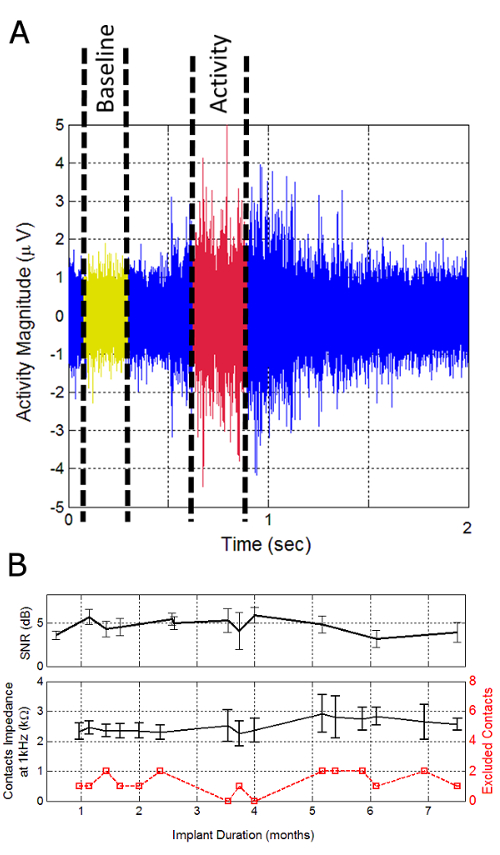
Figure 5: The Evaluation of Cuff Functionality with Chronic Recording of Sciatic Nerve Activity in Dogs. A) A Two seconds example of raw ENG signal recorded at one contact while the animal is voluntarily walking on a treadmill. SNR was defined as the ratio of activity and baseline mean powers. B) Average SNR values were observed during the implant duration. C) Mean value of contacts impedance at 1 kHz (black) and number of non-functional contacts over time (red). 14 of the 16 contacts remained functional throughout the implant duration. The error bars represent the standard deviation. Please click here to view a larger version of this figure.
Discussion
The manufacturing method described in this article requires dexterous and fine movements in order to ensure the quality of the final cuff. The recording contacts must be placed precisely in the middle of the two reference electrodes. This placement has been shown to significantly reduce interferences from surrounding muscles electrical activity27. Any imbalance in the relative position of the contact during the fabrication can degrade the rejection of common mode interfering signals generated outside the cuff. However, with careful technique very little to no noticeable imbalance in the reference contacts was observed.
Several improvements were made to the cuff design to address the failure modes encountered during initial animal trials. These modes and the corresponding improvements are:
Lead breakage: the leads of reference contacts were observed to fail at the welding spot. This failure was attributed to the insufficient strain relief at the site where the lead exits the electrode. This problem was solved by the including a length of reference leads inside the electrode body before exiting.
Closing site Failure: Post-implant cuff opening was observed and attributed to the suture cutting through the silicone. This problem was solved by adding a reinforcement mesh and using softer suture material such as silk to suture the cuff.
Motion artifacts: Large spontaneous artifacts (> 100 µV) were encountered with the first design of the recording cuffs. Similar artifacts were previously reported23 but have not been addressed. These artifacts were found to be triboelectric noise and were attributed to the fact that the two dissimilar nonconductive materials can generate charge along the lead and voltage spikes related to the movement of the lead wires. In particular, the silicone tubing that encloses the contact leads and the leads' insulating material (polytetrafluoroethylene) have different charge affinities, which causes charge transfer between them and into the leads' conductive core forming spikes during movement of the lead. The validation of the nature of these artifacts was made by reconstructing the movement of similar cable structure in normal saline path and similar artifacts were observed. To solve this problem, the insulation material must have charge affinity similar to that of the enclosing tubing material.
Electrode Shielding: A shielding layer (gold metal foil) was also added to the outer faces of the cuff to provide additional EMG reduction28. The foil creates a low-impedance path along the electrode body that shunts interference currents originating outside the cuff.
Connection Failure: It was observed that the transcutaneous connection through the skin was not reliable and caused discontinuity with up to 2 of the 16 contacts (red plot in Figure 5C). Therefore, the connection to the recording device should be improved to enhance the overall interface reliability.
The electrodes produced with this protocol have been implanted in dogs. Some of the materials included in this electrode (e.g., soldering tin, transparency sheet) have not yet been approved for human use. However, the selection of the materials that form the structure of the electrode are included in some FDA approved devices for long term implants (e.g., silicone, PEEK, Platinum/Iridium sheet). Therefore, translating the process into human application only requires careful selection of the tooling materials, and the fabrication under proper clean room conditions.
Three main alternative approaches have been explored to produce multicontact nerve cuff electrodes that can reshape peripheral nerves. First is the hot-knife technique13. It has been shown to be a cost-effective approach to reliably manufacture FINEs with high contact density and high contact placement precision (238 ± 9 µm contact spacing). However, the cuffs produced by this method are stiff and the overall mechanical properties may not suitable for long term implantation. The second approach is laser patterning24. Nd:YaG laser have been used to form the contacts by creating patterns in multi-layered platinum-sputtered PDMS. Although this approach is highly reproducible and yield high precision features (30 µm), the machinery required is very specialized and the long term biocompatibility of the electrodes has not been investigated. The third approach is hand crafted contacts array made of platinum discs or spheres fixed onto silicone rubber25, 26.
This approach does not require expensive equipment and uses highly biocompatible materials. The main drawbacks of this approach are the high tolerance (> 0.5 mm) and the high dependence on human error. The manufacturing procedure described in this protocol yields precise placement of the contacts and is highly reproducible due to the predefined geometry of the fixture frame. The spacing between the middle contacts was measured at 0.51 ± 0.04 mm (n= 70), and the dimensions of the contacts are determined by the tolerance of the laser-cutting machinery.
The FINEs manufactured with this procedure are capable with the appropriate algorithm to detect the location of the fascicles within the nerve and to recover the fascicular signals in freely moving animals without a Faraday cage and with SNR of 5.10 ± 0.81 dB. This design is suitable for nerve stimulation and could be used for selective stimulation using tripolar cuff configuration with minimal artifacts29. This fabrication technique also has the flexibility to produce a variety of cuffs for particular applications such as monopolar stimulation and nerve velocity recording.
Monopolar design can be implemented by removing the four reference contacts while keeping the center contacts. The resulting cuff can then be shorter in length and can be further modified by routing all the leads to exit at one side (one silicone tube pair instead of two). The velocity recording electrode can be implemented by replacing the reference electrodes with four additional contact array frames and then arranging the leads of the extra contacts inside the electrode body toward the opposite exit site.
Divulgaciones
The authors have nothing to disclose.
Acknowledgements
This work was sponsored by the Defense Advanced Research Projects Agency (DARPA) MTO under the auspices of Dr. Jack Judy and Dr. Doug Weber through the Space and Naval Warfare Systems Center, Pacific Grant/Contract No.N66001-12-C-4173. We would like to thank Thomas Eggers for his help in the fabrication process, and Ronald Triolo, Matthew Schiefer, Lee Fisher and Max Freeburg for their contribution in the development of the composite nerve cuff design.
Materials
| Platinum-Iridium foil | Alfa Aesar | 41802 | 90%Platinum Iridium |
| DFT wires | Fort Wayne Metals | 35N LT-DFT-28%Ag | |
| Lead connector | Omnetics Connector Corporation | MCS-27-SS | |
| Silicone sheet | Speciality Silicon Fabricator | 0.005"x12"x12" Silicone Sheet | High durometer, vulcanized |
| Polyether ether ketone (PEEK) sheet | Peek-Optima | 0.005 sheet LT3 grade | |
| polyester stabelizing mesh | Surgicalmesh | PETKM2002 | |
| Silicon tubing (0.04" I.D. 0.085" O.D.) | Silcon Medical/NewAge Industries. | 2810458 | |
| Outer shielding layer | Alfa Aesar, A Johnson Matthey | MFCD00003436 (11391) | Gold foil, 0.004" thick |
| Transparency sheet | APOLLO | APOCG7060 | |
| Ultrasonic bath cleaner | Terra Universal | 2603-00A-220 | |
| Isotemp standard lab oven | Fisher Scientific | 13247637G | |
| Optical microscope | Fisher Scientific | 15-000-101 | |
| Tweezers | Technik | 18049USA (2A-SA) | |
| Surgical blade handles | Aspen Surgical Products | 371031 | |
| Base frame | McMaster-Carr | 9785K411 | |
| Support beam | McMaster-Carr | 9524K359 | |
| Two parts silicone | Nusil | MED 4765 | |
| Soldering Flux | SRA Soldering Products | FLS71 | |
| Tape | 3M Healthcare | 1535-0 (SKUMMM15350H) | Paper, hypoallergenic surgical tape |
| Spot welding machine | Unitek | 125 Power Supply with 101F Welding Head | |
| Laser cutting platform | Universal Laser Systems | PLS6.150D | 150 watts laser |
Referencias
- Naples, G. G., et al. A spiral nerve cuff electrode for peripheral nerve stimulation. Biomed Eng, IEEE Tran. 10, 905-916 (1988).
- Tyler, D. J., Durand, D. M. Functionally selective peripheral nerve stimulation with a flat interface nerve electrode. Neur Sys Rehab Eng., IEEE Trans. 10, 294-303 (2002).
- Navarro, X., et al. A critical review of interfaces with the peripheral nervous system for the control of neuroprostheses and hybrid bionic systems. J Perip Ner Sys. 10, 229-258 (2005).
- Avery, R. E., Wepsic, J. S. Implantable nerve stimulation electrode. U.S. Patent. , (1973).
- Avery, R. E., Wepsic, J. S. Implantable electrodes for the stimulation of the sciatic nerve. U.S. Patent. , (1973).
- Hagfors, N. R. Implantable electrode. U.S. Patent. , (1972).
- Haugland, M. A flexible method for fabrication of nerve cuff electrodes. Eng Med Bio Soc. 1, 359-360 (1996).
- Stein, R. B., et al. Stable long-term recordings from cat peripheral nerves. Brain Res. 128, 21-38 (1977).
- Julien, C., Rossignol, S. Electroneurographic recordings with polymer cuff electrodes in paralyzed cats. J N Sci Meth. 5, 267-272 (1982).
- Van der Puije, P. D., Shelley, R., Loeb, G. E. A self-spiraling thin-film nerve cuff electrode. Can Med Bio Eng Conf. , 186-187 (1993).
- Hoffer, J. A., Loeb, G. E., Pratt, C. A. Single unit conduction velocities from averaged nerve cuff electrode recording in freely moving cats. J N Sci Meth. 4, 211-225 (1981).
- Loeb, G. E., Peck, R. A. Cuff electrodes for chronic stimulation and recording of peripheral nerve activity. J N Sci Meth. 64, 95-103 (1996).
- Wodlinger, B. . Extracting Command Signals from Peripheral Nerve Recordings. , (2011).
- Rozman, J., Zorko, B., Bunc, M. Selective recording of electroneurograms from the sciatic nerve of a dog with multi-electrode spiral cuffs. Jap J Phy. 50, 509-514 (2000).
- Ducker, T. B., Hayes, G. J. Experimental improvements in the use of elastic cuff for peripheral nerve repair. J N Sur. 28, 582-587 (1968).
- Tan, D. W., et al. A neural interface provides long-term stable natural touch perception. S T Med. 6, (2014).
- Branner, A., et al. Long-term stimulation and recording with a penetrating microelectrode array in cat sciatic nerve. Bio Med Eng, IEEE Trans. 1, 146-157 (2004).
- Micera, S., et al. Decoding information from neural signals recorded using intraneural electrodes: toward the development of a neurocontrolled hand prosthesis. P IEEE. 98, 407-417 (2010).
- Kozai, T. D., et al. Ultrasmall implantable composite microelectrodes with bioactive surfaces for chronic neural interfaces. N Mat. 11, 1065-1073 (2012).
- Sinha, G. Charged by GSK investment, battery of electroceuticals advance. Nat Med. 19, 654-654 (2013).
- Tyler, D. J., Durand, D. M. Chronic response of the rat sciatic nerve to the flat interface nerve electrode. A Biom Eng. 31, 633-642 (2003).
- Schiefer, M. A., et al. Selective stimulation of the human femoral nerve with a flat interface nerve electrode. J N Eng. 7, 026006 (2010).
- Edell, D. J. A peripheral nerve information transducer for amputees: long-term multichannel recordings from rabbit peripheral nerves. Bio med Eng, IEEE Trans. 2, 203-214 (1986).
- Schuettler, M., et al. Fabrication of implantable microelectrode arrays by laser cutting of silicone rubber and platinum foil. J N Eng. 2, 121 (2005).
- Pudenz, R. H., Bullara, L. A., Talalla, A. Electrical stimulation of the brain. I. Electrodes and electrode arrays. S Neur. 4, 37-42 (1975).
- Craggs, M. D. . The cortical control of limb prostheses. , 21-27 (1974).
- Struijk, J. J., Thomsen, M. Tripolar nerve cuff recording: stimulus artifact, EMG and the recorded nerve signal. Eng in Med Bio Soc. 2, 1105-1106 (1995).
- Sadeghlo, B., Yoo, P. B. Enhanced electrode design for peripheral nerve recording. N Eng, Int IEEE/EMBS Conf. , 1453-1456 (2013).
- Yoo, P. B., Sahin, M., Durand, D. M. Selective stimulation of the canine hypoglossal nerve using a multi-contact cuff electrode. Ann Bio Med Eng. 32, 511-519 (2004).
- Rydevik, B., Lundborg, G., Bagge, U. Effects of graded compression on intraneural blood flow: An in vivo study on rabbit tibial nerve. J hand Surg. 6, 3-12 (1981).
- Ogata, K., Naito, M. Blood flow of peripheral nerve effects of dissection, stretching and compression. J Hand Sur. 11, 10-14 (1986).
- Boretius, T., et al. A transverse intrafascicular multichannel electrode (TIME) to interface with the peripheral nerve. Bio Sen and Bio Elec. 26, 62-69 (2010).
- Stieglitz, T., Schuettler, M., Meyer, J. U., Micromachined, polyimide-based devices for flexible neural interfaces. Bio Med Micro Dev. 2, 283-294 (2000).

