A Fluorescence-based Lymphocyte Assay Suitable for High-throughput Screening of Small Molecules
Summary
We present in the current study a novel fluorescence-based assay using lymphocytes derived from a transgenic mouse. This assay is suitable for high-throughput screening (HTS) of small molecules endowed with the capacity of either inhibiting or promoting lymphocyte activation.
Abstract
High-throughput screening (HTS) is currently the mainstay for the identification of chemical entities capable of modulating biochemical reactions or cellular processes. With the advancement of biotechnologies and the high translational potential of small molecules, a number of innovative approaches in drug discovery have evolved, which explains the resurgent interest in the use of HTS. The oncology field is currently the most active research area for drug screening, with no major breakthrough made for the identification of new immunomodulatory compounds targeting transplantation-related complications or autoimmune ailments. Here, we present a novel in vitro murine fluorescent-based lymphocyte assay easily adapted for the identification of new immunomodulatory compounds. This assay uses T or B cells derived from a transgenic mouse, in which the Nur77 promoter drives GFP expression upon T- or B-cell receptor stimulation. As the GFP intensity reflects the activation/transcriptional activity of the target cell, our assay defines a novel tool to study the effect of given compound(s) on cellular/biological responses. For instance, a primary screening was performed using 4,398 compounds in the absence of a "target hypothesis", which led to the identification of 160 potential hits displaying immunomodulatory activities. Thus, the use of this assay is suitable for drug discovery programs exploring large chemical libraries prior to further in vitro/in vivo validation studies.
Introduction
High throughput screening (HTS) is a proven strategy widely adopted for the identification of new therapeutic molecules or for the repositioning of FDA-approved drugs in new medical indications.1 So far, the achieved HTS success can be measured by the plethora of previously discovered drugs. For instance, the tyrosine kinase inhibitor lapatinib used for the treatment of breast cancer, sitagliptin; a dipeptidyl peptidase-4 (DPP-4) inhibitor used as an anti-hyperglycemic drug, and the oral Bcr-Abl tyrosine kinase inhibitor dasatinib used for the treatment of chronic myelogenous leukemia represent few examples of a long list of approved drugs originally discovered by HTS.2 Although the productivity of the pharmaceutical industry has lately suffered from a lack in the discovery of new chemical entities, the likelihood of successful drug discovery can be improved through an increase in the number of pre-clinical candidates displaying modulatory biological/biochemical properties. Accordingly, the development of new HTS assays adapted for phenotypic screening could offer the potential to provide important pharmacological tools for the discovery of new drug hits.3,4,5,6 Furthermore, HTS can now be performed at a faster pace due to significant technological transformations in recent years including custom-designed flexible robotic installations, novel read-out technologies and extensive miniaturization.2,7 Among the factors contributing to the growing interest in the use of phenotypic screening (aka forward pharmacology) is the perception that focusing on functional effects rather than oversimplified reductionist assumptions regarding molecular targets (target-based screening/biochemical reactions) is more likely to show clinical efficacy. Thus, phenotypic screening holds the promise to uncover new potentially therapeutic compounds and molecular pathways of currently untreatable diseases.2
To properly identify inhibitors or activators for a given molecular target or cellular function, a highly sensitive and reliable assay is required in order to differentiate between bona fide hits and false positives. So, what makes a good assay? The quality of a given assay must be first judged by the signal-to-noise ratio (reflected through a Z factor).8 Second, the targeted effect or the goal of the screen should be clearly established. For example, functional cell-based approaches can offer significant advantages for receptor screening as opposed to an assay specifically designed to assess ligand-receptor binding. The reason for this is that the latter approach cannot differentiate between agonist and antagonist ligands.9 In contrast, a cell-based approach is likely to be more effective as receptor function can be directly assessed in a biological phenotype (proliferation, cell cycle arrest, apoptosis, and/or differentiation). However, it must be noted that biochemical assays can provide significant advantages over phenotypic assays as they infringe on a specific intracellular target. A well-optimized biochemical assay will generally have less data scatter than a phenotypic screening while simplifying afterwards investigations related to the drug molecular mechanism of action. However, the major drawback of target-based or biochemical assays is the chance of amplifying the rate of false positive hits that may affect non-specific targets when tested in a biological system (loss of the specificity originally studied in the biochemical assay).10 Although a well-established cut-off point between negative and positive hits can minimize the number of false positives in the primary screening, the use of a physiologically relevant system mimicking the native cellular environment such as intact cells, whole tissue or whole animal remains the core of the assay design pendulum. Therefore, phenotypic screening enables lead discovery with desirable biological/phenotypic effects for diseases with no identified drug targets without having prior knowledge of the compound's activity or mode of action.11
The herein study concerns the development and testing of an optimized and reproducible phenotypic screening based on two important components: a commercially available mouse model and a clustered sub-family of chemical compounds. With respect to the animal model, the assay relies on the use of lymphocytes derived from a mouse strain (Nur77GFP) harboring a bacterial artificial chromosome containing a cassette in which the expression of the green fluorescent protein (GFP) is driven by the Nur77 promoter.12 The hallmark of this stimulation is based on the fact that Nur77 is an immediate early gene up-regulated following T-cell receptor (TCR) or B-cell receptor (BCR) stimulation.12 As for the screening method itself, an approach was used to help avoiding the screening of trivial analogues while minimizing the time needed to assess a large chemical library (>105 compounds). To do so, a database of chemical compounds selected by medicinal chemists using virtual screening tools was exploited to identify topologically similar compounds using known active seed structures as references. This approach allowed us to screen 4,398 compounds representing an overall library of over 136,000 chemical entities.
Protocol
All animal protocols were approved by the Animal Care Committee of Université de Montréal. Mice were euthanized by gradual inhalation of CO2 until no vital signs were observed followed by cervical dislocation. The procedure was carried out by a certified person to ensure that animals were euthanized in a humane manner and according to the recommendations of the Canadian Council on Animal Care.
1. Preparation of Splenocyte Medium and Flow-cytometry Buffer
- Perform all steps under a 70% ethanol-cleaned biological hood.
- Remove 70 mL of pre-warmed Roswell Park Memorial Institute (RPMI) 1640 1x medium (commercially available and supplied in filtered 500 ml volume sterile bottles) and place in a sterile tube. The removed medium will be used later in the protocol.
- Supplement the remaining 430 mL of RPMI 1640 1x with 50 ml inactivated fetal bovine serum (FBS), 5 mL penicillin/streptomycin, 5 mL HEPES, 5 ml non-essential amino acids, 5 mL sodium pyruvate, and 0.05 mL filtered (1M) 2-mercaptoethanol.
NOTE: Pre-warm splenocyte medium using a water bath set at 37 ºC to avoid heat shocking cells. This is important to avoid induction of cellular apoptosis. - To prepare the flow-cytometry buffer, add 2 mL of FBS to 98 ml phosphate buffered saline (PBS) and keep refrigerated until use (preferably within three days).
2. Generation of Splenocyte Cell Suspension from Nur77GFP Mouse Spleens
- Aseptically isolate the spleen from a 6-8 week old female Nur77GFP mouse.
- To achieve this, work under sterile hood. Soak the sacrificed mouse fur, scissors and forceps in 70% ethanol.
- Lay the mouse on its right side, cut the skin and muscles in the upper left abdominal quadrant. Inspect the incision area to visibly locate the spleen then cut it out. Keep the spleen in splenocyte medium on ice until ready to perform the next step.
- Place the spleen(s) in a 10 cm2 cell culture petri dish containing 5 ml of pre-warmed splenocyte medium.
- Mash the spleen using a sterile syringe plunger until the solution is turbid. A spleen collagen matrix should remain by the end of the procedure.
- Following extensive mashing in splenocyte medium, collect the cell suspension and pass it through a 70 µm cell strainer placed on a 50 mL tube to filter-out any debris or clots.
- Centrifuge at 500 x g for 5 min. After discarding the supernatant, re-suspend the cell pellet in 2-3 mL of in-house produced or commercial red blood cell lysis buffer. Following pipetting (2-3 times) let the suspension rest for 20-30 s.
- Add 5 mL of PBS or a suitable buffer of choice then centrifuge the cell suspension for 5 min at 500 x g.
- Remove the supernatant (should be red in color as it contains lysed red blood cells) and re-suspend the cell pellet in 2 ml of splenocyte medium.
- Using a hemocytometer, count the number of cells stained with trypan blue to differentiate between live and dead (necrotic) cells.
3. T-cell Isolation from the Splenocyte Cell Suspension
- Centrifuge the cell suspension for 5 min at 500 x g. Re-suspend the cells in serum-free RPMI medium (50 ml from step 1.3) to obtain a cellular concentration of 10 x 106 cells/mL.
- Transfer the cells to a 5 mL polystyrene tube and set aside a 100 µL aliquot of splenocytes for purity assessment/comparison at the end of the purification step.
- Add normal rat serum to the cell suspension at 50 µL/mL followed by T cell isolation antibody cocktail (50 µL/mL).
- Mix the cell suspension and let it rest for 10 min. This step allows the antibody cocktail to bind all unwanted cells.
- Add the streptavidin rapid spheres (magnetic beads) for 2.5 min, then bring the volume to 2.5 mL using the serum-free medium.
- Place the tube in a cell isolation magnet for 3 min.
- Transfer the T cell suspension into a new polystyrene tube by holding the magnet and pouring out the solution in one move.
NOTE: The isolated suspension contains the purified T cells. All unwanted cells are held on the side of the tube bound to the magnetic streptavidin beads. - Count the isolated T cells using trypan blue and a hemocytometer.
NOTE: At this step the purity of the isolated T cells can be verified (optional) by analyzing the percentage of CD3+ events before and after T cell isolation by flow-cytometry.13- Briefly, centrifuge 1 ml of splenocyte cell suspension at 500 x g. Discard the supernatant and suspend the cells in flow-cytometry buffer at a concentration of 1 x 106 cells/mL.
- Add fluorescent-tagged anti-mouse CD3 antibody at a concentration of 1:100. Incubate at 4 °C for 30 min. Wash once, centrifuge and re-suspend in flow-cytometry buffer (400 µL) for analysis by flow-cytometry.
4. B-cell Isolation from the Splenocyte Cell Suspension
- Follow the same protocol as described for T cells (steps 3.1-3.8) but using a B-cell isolation kit. For purity assessment, use the CD19 antibody instead of the CD3 antibody.13
- For purity assessment (optional), use the CD19 antibody instead of the CD3 antibody. Centrifuge 1 mL of splenocyte cell suspension at 500 x g. Discard the supernatant and suspend the cells in flow-cytometry buffer at a concentration of 1 x 106 cells/ml.
- Add fluorescent tagged anti-mouse CD19 antibody at a concentration of 1:100 and incubate at 4 °C for 30 min. Wash once, centrifuge and re-suspend in flow-cytometry buffer (400 µL) for analysis by flow-cytometry.
5. T-cell Activation and the Induction of GFP Expression
- Seed the T cells, in suspension, into a round-bottomed 96-well plate at a concentration of 2.5 x 105 cells/well.
- Add recombinant interleukin (IL)-7 at 2 ng/mL and CD3/CD28 magnetic beads (25 µL/106 cells). Keep a portion of the T cells untreated with beads to serve as a negative control for later measurements that representing non-activated T cells.
- Twelve hours later, harvest the T cells from the 96-well plate by gently pipetting the cell suspension in each well up and down to break any bead-cell complex/aggregates. Collect the suspension from all wells into a 5 mL polystyrene tube.
- Place the tube containing the suspension inside the same cell isolation magnet used previously for purification of T or B cells and allow it to rest for 5 min.
- Transfer the T cell suspension into a new polystyrene tube by holding the magnet and pouring out the solution in one move.
- Centrifuge the cells at 500 x g for 5 min. Re-suspend the cells in fresh splenocyte medium to get a concentration of 2 x 106 cells/mL.
- Assess GFP expression intensity by flow-cytometry (optional for quality control) at 12 to 24 h post-stimulation in comparison with non-activated T cells.12
NOTE: The GFP fluorescence is intrinsic to the Nur77GFP T cells and is manifested upon successful activation of the TCR.12 - For assessment of viability and activation (optional) by microscopy, stain the activated cells with Hoechst 30 min prior to analysis at a concentration of 0.2 µg/ml. Add adequate volume of the cell suspension to a cover slide or to a well of a flat-bottomed black-sided 384-well plate and examine under fluorescence microscope to assess living cells. Dead cells will not retain nuclear staining.14
6. B-cell Activation and the Induction of GFP Expression
- Using a T-25 culture flask, re-suspend the isolated B cells at 1 x 106 cells/mL.
- Add anti-mouse IgG/IgM (H+L) at 10 µL/mL and recombinant CD40L at a concentration of 200 ng/mL. Keep a portion of the B cells untreated to serve as a negative control for later measurements (representing non-activated B cells).
- Assess GFP expression intensity by flow-cytometry at 12 or 24 h post-stimulation in comparison with non-activated B cells.
NOTE: The GFP fluorescence is intrinsic to the Nur77GFP B cells and is manifested upon successful activation of the BCR.12 - For assessment of viability and activation (optional) by microscopy, stain the activated cells with Hoechst 30 min prior to analysis at a concentration of 0.2 µg/mL. Add adequate volume of the cell suspension to a cover slide or to a well of a flat-bottomed black-sided 384-well plate and examine under a fluorescence microscope to assess living cells. Dead cells will not retain nuclear staining.14
7. High Throughput Screening of Small Molecules
- Prepare a cell suspension at 2 x 106 cells/mL of the activated T or B cells (magnetic beads or antibodies/CD40L) or non-activated groups.
- Plate 75,000 cells/well in a 384-well plate (volume of 40 µL). Use a flat-bottomed black-sided 384-well plate or a microscope cover slide for viability and activation assessment by fluorescent microscopy (optional quality control step prior to HTS) using Hoechst stain (refer to steps 5.8 and 6.4 for details).14
- Manually or using an automated system, add the drugs of choice (dissolved in 0.5% DMSO) to each well.
- Add the vehicle (DMSO) to positive (activated) and negative (non-activated) control wells. Adjust DMSO concentration to a maximum of 0.5%.
- Incubate the plates for 24 h (or incubation time of choice) at 37 ºC and 5% CO2.
- On the day of the screening, dilute the Hoechst 33342 stain solution (1:3,333; for e.g. add 10 µL to the cells in the 384-well plates to generate a total volume to 50 µL). Stain 30 min before GFP analysis by adding Hoechst solution to achieve a concentration of 0.2 µg/mL.
- Gently pipette the cells up and down to obtain a homogenous distribution in each well.
NOTE: This step is important in case of dispensing the drugs (step 7.3) using an automated system as the cells tend to accumulate at one side of the well, opposite to the direction of the flow. - Spin the plates at 45 x g for 3 min at room temperature.
- Leave the plates to rest for 15 min at room temperature.
- Perform plate(s) read-outs, using the automated confocal high content screening (HCS) system.15 Load the plate to the machine. Set the objective at 40X or higher magnification. Use camera #4 for Hoechst (UV lamp) and camera #1 for GFP (laser 488). Set up the machine to read 6-10 fields per well. Adjust the machine to do two sequential readings per field at 488 nm (to read GFP) and UV light (to read Hoechst). Set the objective at 40X or higher magnification.
NOTE: The system is a computerized microscope that does not require any adjustments. The focal distance, the intensity of the incident light and the time of exposure are all setup automatically by the machine.
Representative Results
Design of the HTS assay
Two important factors were taken into consideration when designing the herein fluorescent assay. First, we needed to replicate a physiological condition in which T- or B cell activation would represent an ailment (e.g. graft-versus-host disease). Second, the assessment of cellular activation should be performed using a sensitive and quantitative method. Fluorescence is nowadays one of the primary choice for HTS read-outs as it corresponds to these needs.10,16 As a robust GFP read-out can be obtained following Nur77GFP-derived T or B cell stimulation both in vitro or in vivo,12 our assay exploited this strategy to differentiate between non-activated and activated cells as a working model for the identification of immunomodulatory compounds.
Originally, the design of our assay was based on GFP assessment by flow-cytometry using unfractionated stimulated splenocytes. In this case, both non-activated/activated T and B cells are stained with anti-CD3 or anti-CD19, respectively prior to GFP assessment. As shown in Figure 1A, T cells (CD3+ cells) represent approximately 30% of a given mouse spleen. At steady state, the GFP level was in the range of 10% (most likely due to post-thymic selection through the TCR during development or homeostatic stimulation in the periphery). Following TCR stimulation using the CD3/CD28 beads, a five to six-fold increase in the percentage of GFP expression (57% instead of 10%) was detected in CD3+ T cells (Figure 1A–B). Likewise, B cells (CD19+ cells) represent 50-55% of total splenocytes and their basal GFP expression is comparable to non-activated T cells (e.g. ~10%, Figure 1C). Interestingly, however, BCR stimulation using anti-mouse IgG/IgM and recombinant CD40L triggered a trivial increase in GFP expression (33% instead of 12%, Figure 1C–D). As GFP expression is a key element for assessing the pharmacological effect of screened small molecules on activated T or B cells, optimizing its intensity is central for the sensitivity and success of the screening.
Assessment of GFP expression using purified T or B cells
Although T and B cell stimulation can be achieved directly using unfractionated splenocytes, the GFP expression intensity was not sensitive enough for the screening especially if read-outs are to be performed by microscopy. In order to improve the cellular response, T cells were first purified by magnetic beads using a commercially available kit (Figure 2A). As previously shown using unfractionated splenocytes, 10% of isolated CD3+ T cells were GFP positive (basal expression). In this context, T cell stimulation using the CD3/CD28 beads significantly improved their GFP response (Figure 2A–2B, 86% as opposed to 57% when unfractionated splenocytes were used). Similar improvements were obtained with B cells (Figure 2C–2D, 80% instead of 33%). These results clearly demonstrate that the use of purified T and B cells maximizes GFP expression, which is suitable for the proposed phenotypic screening.
Schematic diagram of the designed HTS assay
Overall, the assay can be sub-divided into four major sections (Figure 3). In the case of T cells for example, a splenocytes cell suspension is prepared in order to purify T cells (steps 1-3) followed by a 12 h stimulation step in vitro using CD3/CD28 beads (steps 4-5). Activated T cells are then plated and cultured for 24 h with the small molecules of choice in 384-well plates (steps 6-7) before the assessment of GFP and Hoechst intensities using the automated HCS system. The same assay could be used for B cells with modifications performed at steps 4-5. Briefly, B cells can be stimulated with anti-mouse IgG/IgM and recombinant CD40L instead of beads. As these components are used in their soluble form (e.g. not linked to beads), B cells can be incubated for 12 h then simply washed prior to plating in 384-well plates for the screening process.
Efficient T-cell survival is primordial for the success of the HTS study. Accordingly, two limiting factors may impede the quality of the assay and should be taken into consideration. First, murine T cells are highly susceptible to apoptosis following in vitro stimulation.17 Second, all tested compounds are diluted in a DMSO solution, which might add a second stress factor. To minimize cell loss, recombinant IL-7 (2 ng/ml) was supplemented to T cells upon TCR stimulation at steps 4-5. This homeostatic cytokine supports proliferation and enhances T-cell survival through the expression of anti-apoptotic molecules such as Bcl-2, Bcl-xL and Mcl-1.18,19,20,21,22
Primary high throughput screening of 4,398 compounds reveals several activators and inhibitors of T cell activation
A high throughput screening was carried out by plating 75,000 of non-activated (negative control) or activated T cells (positive control) as displayed in Figure 4. To ensure high reproducibility, the assay was conducted several times with an obtained Z factor of 0.87 (Figure 5A). Using the HCS system, the observed GFP expression of stimulated T cells was 20 times higher than unstimulated T cells allowing the generation of a ''window of action'' zone where GFP inhibitory compounds could be easily detected (Figure 5A). This is shown in the figure in terms of the number of fluorescent cells divided by the total number of cells in the scanned fields. In the example shown in Figure 5A, the screening of 320 compounds unveiled three compounds (pointed-out by red arrows) capable of inhibiting GFP expression by 1.5-2.5 folds. In this example, the positive control value was 0.44 ±0.02 and the negative control was 0.02 ±0.00.
The screening of a total of 4398 compounds (Z factor of 0.85) was then conducted. The compounds were selected by medicinal chemists as seed/representative compounds based on their chemical structure representing an overall chemical library containing 136,000 entities (Figure 5B). At the end of the assay, analysis of GFP inhibition identified compounds capable of either inhibiting (positive deviators) or enhancing GFP expression (negative deviators).
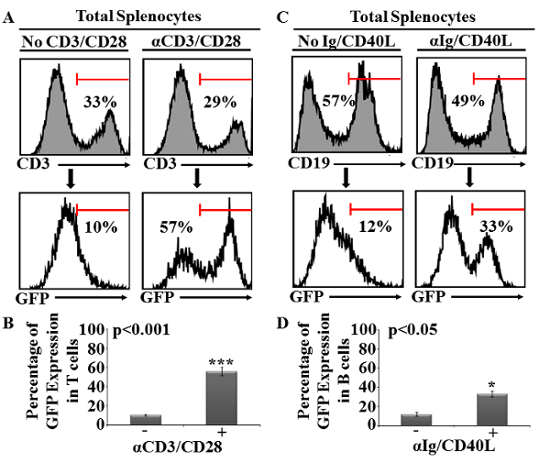
Figure 1: Analysis of T- and B-cell GFP expression following TCR or BCR activation conducted on unfractionated splenocytes. (A) Representative flow-cytometry analysis of T cells stained with an anti-CD3 antibody using splenocytes in the absence (top left panel) or presence of CD3/CD28 beads (top right panel). GFP expression for both T-cell groups are displayed at the bottom. (B) Percentage of GFP expression obtained by flow-cytometry analysis of T cells. Error bars represents mean ± SD. (C) Similar to (A) except that splenocytes were activated using anti-mouse IgG/IgM and recombinant CD40L then stained for CD19. (D) Percentage of GFP expression obtained by flow-cytometry analysis of B cells. Error bars represents mean ± SD. All shown experiments were repeated at least three times (n = 5/group; *P <0.05 and ***P <0.001). Please click here to view a larger version of this figure.
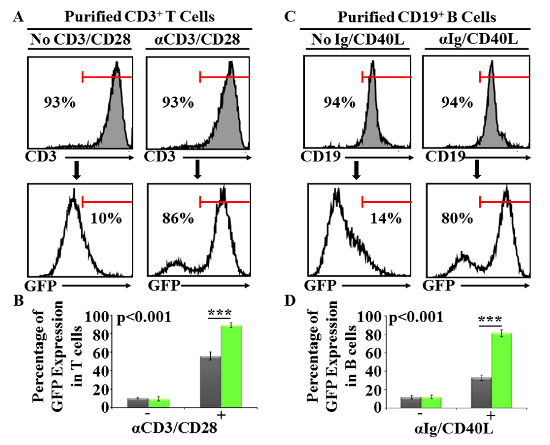
Figure 2: Analysis of GFP expression using purified T or B cells following TCR or BCR activation respectively. (A) Representative flow-cytometry analysis of purified T cells stained with an anti-CD3 antibody. For GFP induction, purified T cells were stimulated using CD3/CD28 beads (top right panel). Non-activated control T cells are shown at the top left panel. GFP expression of both non-activated and activated T cells is displayed at the bottom. (B) Percentage of GFP expression obtained by flow-cytometry analysis of T cells. Error bars represents mean ± SD. (C) Similar to (A) except that the purity of B cells was assessed by CD19 staining and activated using anti-mouse IgG/IgM and recombinant CD40L. (D) Percentage of GFP expression obtained by flow-cytometry analysis of B cells. Error bars represents mean ± SD. All shown experiments were repeated at least three times (n = 5/group and ***P <0.001). Please click here to view a larger version of this figure.
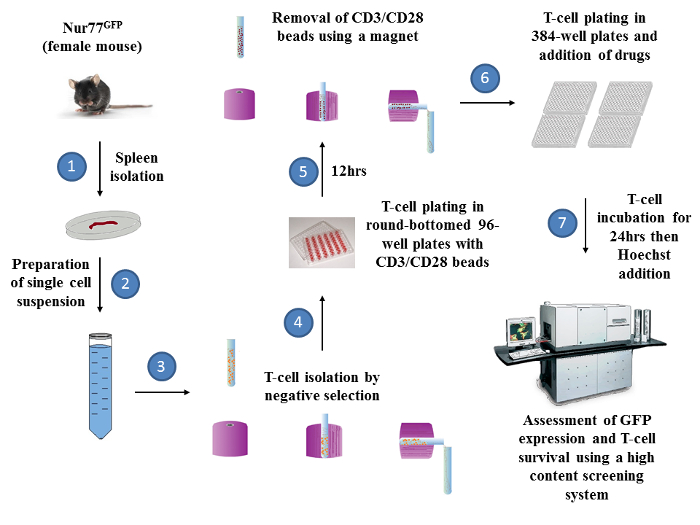
Figure 3: Overall schematic diagram representing the steps of the phenotypic screening. There are 7 major steps required to prepare the HTS assay. A female Nur77GFP mouse is sacrificed to isolate its spleen (Step 1). Following the generation of a splenocytes cell suspension (Step 2), T cells are negatively isolated (by depletion of unwanted cells) using a commercially available kit (step 3). Isolated T cells are then incubated with recombinant IL-7 in the absence or presence of CD3/CD28 beads in round-bottomed 96-well plate at 37 ºC (step 4). Twelve hours later (step 5), T cells are pipetted several times to dislodge any aggregates prior to beads removal using the same cell isolation magnet used originally for T-cell purification. Isolated T cells are then seeded in 384-well plates (75 000 cells/well, step 6) with the compounds for another 24 h (step 7). The following day, incubated cells are stained with Hoechst 30 min prior to analysis by the HCS system (step 8). The same set-up could be followed-up for the preparation of a B cell-based assay except that step 4 and 5 are to be replaced by a simple wash as the stimulators are added in soluble forms. Please click here to view a larger version of this figure.
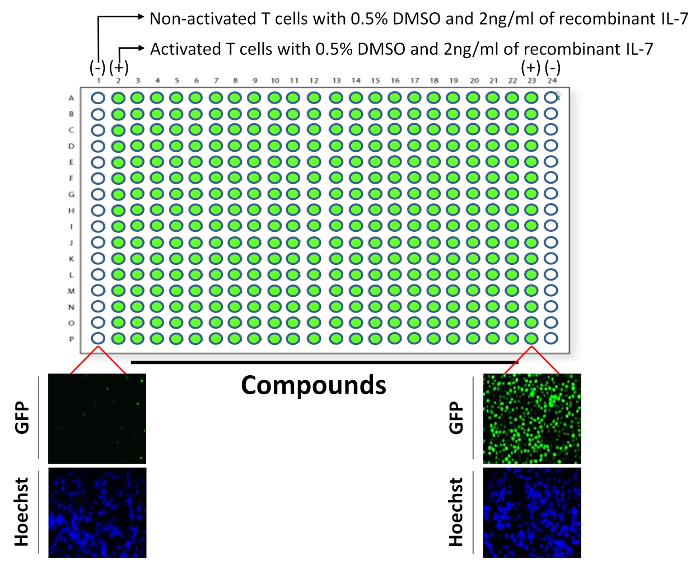
Figure 4: Layout for the plating of T cells in a 384-well plates. Each plate used in the assay contained three groups. In the first group, wells were loaded with non-activated T cells (negative control for GFP on each sides of the plate; wells A1-P1 and A24-P24), whereas the second group contained activated T cells without drugs (positive control for GFP; wells A2-P2 and A23-P23). All remaining wells containing activated T cells supplemented with the chemical entities used in the screening. All wells contained 0.5% DMSO. Examples for the GFP and Hoechst signals are shown for non-activated and activated T cells. Please click here to view a larger version of this figure.
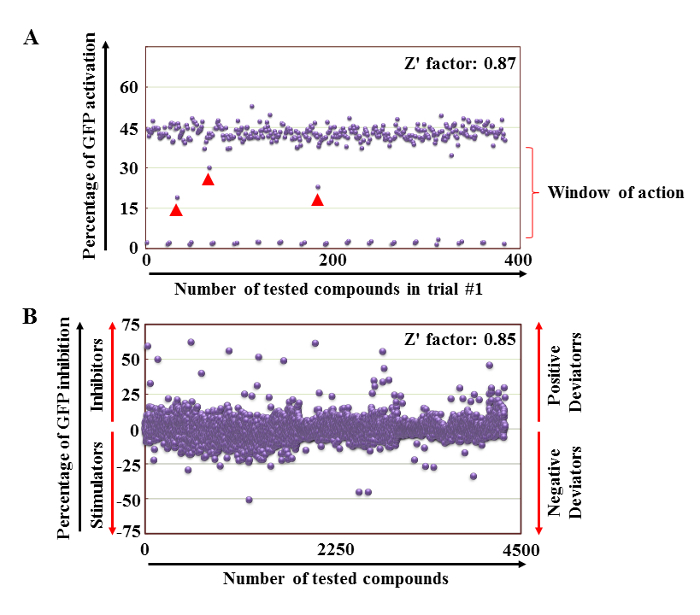
Figure 5: Primary phenotypic screening. (A) Representative example of a primary screening performed on 320 compounds. Non-activated T cells are almost GFP null in contrast to TCR-stimulated T cells, which display 20-fold higher GFP expression. (B) Cumulative data of all compounds screened using the assay. The GFP expression demonstrates compounds displaying inhibitory action whereas other compounds were behaving as T cell stimulators. Please click here to view a larger version of this figure.
Discussion
Several read-out methods have been exploited for the development of sensitive and reliable HTS assays. These include colorimetric, luminescent or fluorescent methods. Although colorimetric methods are simple to set-up, they require multiple additions of chemicals, which may interfere or disrupt the cells being tested.23 In addition, they do not permit dynamic assessment of a biological response as the pharmacological effect is assessed at a specific endpoint. Furthermore, this method may require expensive robotic arms if automated HTS is used. These factors make colorimetric read-outs less compatible with the objective of HTS due to their cumbersome requirements and low sensitivity.23 Although luminescence has been proposed as an alternative to colorimetric assays, the application of these luminescent tests in HTS is usually limited due to the requirement of cell lysis. Even though other non-lysis protocols were developed, the intensity of the bioluminescence signal can be impeded by many factors such as luciferin absorption, availability of co-factors, pH, and transparency of culture media or buffer, causing discrepancies between detected bioluminescence signals and actual changes in cellular activity.24 Hence, most assays rely on fluorescence methods. In fact, fluorescent-based assays were initially developed using small, highly-fluorescent organic molecules capable of monitoring a variety of cellular processes upon cell activation. In sum, fluorescent assays have higher sensitivity and can be easily adapted for phenotypic measurements during HTS.23
The developed fluorescent-based HTS assay presented here has three major advantages. First, it is highly reliable, reproducible and has been adopted for the screening of compounds capable of modulating two different primary cells (T and B lymphocytes) using the same stimulation/read-out concept. For example, the primary screening of 4,398 compounds, which was completed over five different runs displayed a consistent activation-induced GFP signal with minimal intra and inter-assay variabilities (<5% and <15%, respectively for T cell assay). Second, the assay uses a commercially available transgenic mouse model. Usually, the design of a fluorescence-based assay requires the genetic engineering of primary cells or a cell line of interest in order to display a fluorescent signal upon stimulation. Although this approach generates a precious laboratory tool, it is generally not readily available to the scientific community. To bypass this limitation, T and B cells were isolated from the Nur77GFP transgenic mice. The advantage of these lymphocytes is their ability to express GFP within 24 h upon TCR or BCR stimulation. Therefore, screening drugs capable of modulating the transcriptional machinery driving GFP expression or the overall cellular response represents an appealing approach. Third, supplementing T cells with CD3/CD28 beads in their initial activation phase requires the removal of these beads prior to GFP assessment. This is important if microscopy is used for analyzing T cell activation/inhibition as leaving the beads will otherwise mask the GFP signal. If flow-cytometry is used instead for the analysis, beads could be left in the wells (unless it specifically creates additional confounding limitation(s) to the assay) as the specific population of interest can be gated using both forward and side scatters.
The initial objective was to design a screening assay with minimal cellular handling. Under this context, the activation of T or B cells using unfractionated splenocytes stimulated with beads or soluble antibodies/recombinant CD40L respectively was limited as a great proportion of lymphocytes remained GFP negative (Figure 1). As this step is critical for the success of the assay, the protocol was modified to purify T or B cells using commercially available kits to increase the percentage GFP-expressing cells. This approach significantly improved the activation outcome of both cell populations. Although another method of choice can be used for T and B cell isolation if deemed necessary, the proposed approach is: i) highly reproducible, ii) easily adapted to assess the purity of the isolated population by flow-cytometry prior to HTS, iii) and time efficient as the purification step is relatively short (~30 min) and can be performed with minimal preparation. However, it must be noted that the assay presented in this study is based on the use of mouse primary cells. Secondary (for confirmation purposes) and tertiary (final validation on the target of interest) assays should be conducted following the primary screen to validate the identified hits. Although it could be easily adapted to a variety of different cell lines, the pharmacological effect of identified hits needs further validation on other species (e.g. human cells – example of tertiary assay) as there are no possible ways to predict sustained effects among species. In sum, this assay is valuable for the identification of new potential hits and/or molecular targets with possible extrapolation of results from in vitro/animal tests to humans.
Even though the designed assay can be exploited for both T and B cells, one advantage is conferred to the specific use of T cells in this case. TCR activation usually requires dual stimulation conferred through a primary (e.g. anti-CD3 or anti-TCR) and a secondary co-activating (e.g. anti-CD28) signal.25,26 Interestingly, both anti-CD3 and anti-CD28 antibodies can be purchased directly linked onto the surface of magnetic beads, and can be removed from the cell suspension using a standard magnet before adding the chemical compounds to be tested in the screening. As a library with unknown chemical entities is being used, retaining activated T cells free of molecules bound to their TCR complex may minimize any possible interference between the tested compounds and those bound to the TCR binding grooves.27 In addition, removing the stimulating agent following T cell activation mimics physiological situations as opposed to working with T cells subjected to a sustained supraphysiological TCR activation. The latter situation can be problematic as it might override the pharmacological effect of a given compound especially if it was used at small concentrations in the screening. As there are no commercially available beads exerting the same effect on B cells, it would be interesting to perform a HTS in the future testing whether the continuous presence of the stimulus on B cells limits the performance of the assay.
Divulgaciones
The authors have nothing to disclose.
Acknowledgements
This work was supported by the Merck Frosst Start-up funds provided by Université de Montréal. We would like to thank Drs Jean Duchaine and Dominic Salois from the High-throughput platform at the Institute for Research in Immunology and Cancer for their discussion, comments and feedbacks. Moutih Rafei holds a Fonds de la Recherche en Santé du Québec Junior 1 Award.
Materials
| Nur77GFP mice | The Jackson Laboratory | Mouse strain No. 016617 | An in house colony was established at our animal facility |
| 96 wells-U culture plates, sterile | VWR International | 10062-902 | T-cell activation using the magnetic beads |
| 70µm cell strainer, sterile | Corning Inc. | 352350 | Generation of splenocytes cell suspension |
| 5 ml polystyrene round bottom tubes, sterile | Corning Inc. | 352058 | Generation of splenocytes cell suspension |
| 50 ml polypropylene conical bottom tubes, sterile | VWR International | 89039-656 | Generation of splenocytes cell suspension |
| 10 ml syringe without needle, sterile | Becton, Dickinson and Company | 305482 | To mash the spleen |
| T-25 culture flask | Greiner Bio-One | 690 175 | To incudabte B cells during activation |
| 5 ml cell culture dish, sterile | Greiner Bio-One | 627 160 | To mash the spleen |
| Penicillin- Streptomycin (10,000 U/mL) | WISENT Inc. | 450-200-EL | Component of the splenocyte media |
| RPMI 1600 with sodium bicarbonate and L- glutamine | WISENT Inc. | 350-002-CL | Component of the splenocyte media |
| MEM non-essential amino acids | WISENT Inc. | 321-010-EL | Component of the splenocyte media |
| HEPES free acid 1 M | WISENT Inc. | 330-050-EL | Component of the splenocyte media |
| Sodium pyruvate solution (100mM) | WISENT Inc. | 600-110-EL | Component of the splenocyte media |
| Fetal Bovine Serum (FBS) | WISENT Inc. | 080-910 | Component of the splenocyte media and flow-cytometry buffer |
| Phosphate buffered saline (PBS) | WISENT Inc. | 311-010-CL | Component of flow-cytometry buffer |
| 2-Mercaptoethanol (55mM) | Thermo Fisher Scientific | 21985-023 | Component of the splenocyte media |
| T- Cells isolation kit | Stemcell Technologies | 19851 | To isolate T cells |
| B- Cells isolation kit | Stemcell Technologies | 19854 | To isolate B cells |
| Mouse T-Activator CD3/CD28 superparamagnetic beads | Thermo Fisher Scientific | 11452D | To activate T cells |
| Cell isolation magnet | Stemcell Technologies | 18000 | To isolate T cells and remove the magnetic beads |
| AffiniPure F(ab')2 Fragment Goat Anti-Mouse IgG + IgM (H+L) | Jackson ImmunoResearch Laboratories, Inc. | 115-006-068 | To stimulate B cells |
| Recombinant Murine IL-7 | Peprotech | 217-17 | To support T-cell survival during activation |
| Recombinant CD40L | R&D Systems | 8230-CL/CF | To stimulate B cells |
| Anti-mouse CD3 antibody | BD Pharmingen | 561799 | To stain T cells for flow-cytometry |
| Anti-mouse CD19 antibody | BD Pharmingen | 553786 | To stain B cells for flow-cytometry |
| Biomed FXp | PerkinElmer Inc. | A31842 | To re-suspend cells after 24 hours incubation |
| Opera Phenix High Content Screening System | PerkinElmer Inc. | HH14000000 | To analyze GFP/Hoechst signal |
Referencias
- Swinney, D. C., Anthony, J. How were new medicines discovered. Nat Rev Drug Discov. 10 (7), 507-519 (2011).
- Macarron, R., et al. Impact of high-throughput screening in biomedical research. Nat Rev Drug Discov. 10 (3), 188-195 (2011).
- Lokey, R. S. Forward chemical genetics: progress and obstacles on the path to a new pharmacopoeia. Curr Opin Chem Biol. 7 (1), 91-96 (2003).
- Hall, S. E. Chemoproteomics-driven drug discovery: addressing high attrition rates. Drug Discov Today. 11 (11-12), 495-502 (2006).
- Pruss, R. M. Phenotypic screening strategies for neurodegenerative diseases: a pathway to discover novel drug candidates and potential disease targets or mechanisms. CNS Neurol Disord Drug Targets. 9 (6), 693-700 (2010).
- St Onge, R., Schlecht, U., Scharfe, C., Evangelista, M. Forward chemical genetics in yeast for discovery of chemical probes targeting metabolism. Molecules. 17 (11), 13098-13115 (2012).
- Houston, J. G., Banks, M. N., Binnie, A., Brenner, S., O’Connell, J., Petrillo, E. W. Case study: impact of technology investment on lead discovery at Bristol-Myers Squibb. Drug Discov Today. 13 (1-2), 44-51 (2008).
- Zhang, J. H., Chung, T. D., Oldenburg, K. R. A Simple Statistical Parameter for Use in Evaluation and Validation of High Throughput Screening Assays. J Biomol Screen. 4 (2), 67-73 (1999).
- Walters, W. P., Namchuk, M. Designing screens: how to make your hits a hit. Nat Rev Drug Discov. 2 (4), 259-266 (2003).
- Zheng, W., Thorne, N., McKew, J. C. Phenotypic screens as a renewed approach for drug discovery. Drug Discov Today. 18 (21-22), 1067-1073 (2013).
- Malo, N., Hanley, J. A., Cerquozzi, S., Pelletier, J., Nadon, R. Statistical practice in high-throughput screening data analysis. Nat Biotechnol. 24 (2), 167-175 (2006).
- Moran, A. E., et al. T cell receptor signal strength in Treg and iNKT cell development demonstrated by a novel fluorescent reporter mouse. J Exp Med. 208 (6), 1279-1289 (2011).
- Kovacic, N., Müthing, J., Marusic, A. Immunohistological and Flow Cytometric Analysis of Glycosphingolipid Expression in Mouse Lymphoid Tissues. J Histochem Cytochem. 48, 1677-1689 (2000).
- Shapiro, H. M. Flow cytometric estimation of DNA and RNA content in intact cells stained with hoechst 33342 and pyronin Y. Cytometry. 2, 143-150 (1981).
- Zanella, F., Lorens, J. B., Link, W. High content screening: seeing is believing. Trends Biotechnol. 28 (5), 237-245 (2010).
- An, W. F. Fluorescence-based assays. Methods Mol Biol. 486, 97-107 (2009).
- Kishimoto, H., Sprent, J. Strong TCR ligation without costimulation causes rapid onset of Fas-dependent apoptosis of naive murine CD4+ T cells. J Immunol. 163 (4), 1817-1826 (1999).
- Schluns, K. S., Kieper, W. C., Jameson, S. C., Lefrancois, L. Interleukin-7 mediates the homeostasis of naive and memory CD8 T cells in vivo. Nat Immunol. 1 (5), 426-432 (2000).
- Jiang, Q., et al. Cell biology of IL-7, a key lymphotrophin. Cytokine Growth Factor Rev. 16 (4-5), 513-533 (2005).
- Koenen, P., et al. Mutually exclusive regulation of T cell survival by IL-7R and antigen receptor-induced signals. Nat Commun. 4, 1735 (2013).
- Vella, A., Teague, T. K., Ihle, J., Kappler, J., Marrack, P. Interleukin 4 (IL-4) or IL-7 prevents the death of resting T cells: stat6 is probably not required for the effect of IL-4. J Exp Med. 186 (2), 325-330 (1997).
- Hawkins, C. J., Vaux, D. L. The role of the Bcl-2 family of apoptosis regulatory proteins in the immune system. Semin Immunol. 9 (1), 25-33 (1997).
- Sumantran, V. N. Cellular chemosensitivity assays: an overview. Methods Mol Biol. 731, 219-236 (2011).
- Huh, S., et al. A cell-based system for screening hair growth-promoting agents. Arch Dermatol Res. 301 (5), 381-385 (2009).
- Weiss, A. TCR signal transduction: opening the black box. J Immunol. 183 (8), 4821-4827 (2009).
- Noel, P. J., Boise, L. H., Green, J. M., Thompson, C. B. CD28 costimulation prevents cell death during primary T cell activation. J Immunol. 157 (2), 636-642 (1996).
- Michels, A. W., et al. Structure-based selection of small molecules to alter allele-specific MHC class II antigen presentation. J Immunol. 187 (11), 5921-5930 (2011).

