Orthotopic Injection of Breast Cancer Cells into the Mice Mammary Fat Pad
Summary
Here, we present a protocol to implant breast cancer cells into the mammary fat pad in a simple, less invasive, and easy-to-handle way, and this mouse orthotopic breast cancer model with a proper mammary fat pad environment can be used to investigate various aspects of cancer.
Abstract
A proper animal model is crucial for a better understanding of diseases. Animal models established by different methods (subcutaneous injections, xenografts, genetic manipulation, chemical reagents induction, etc.) have various pathological characters and play important roles in investigating certain aspects of diseases. Although no single model can totally mimic the whole human disease progression, orthotopic organs disease models with a proper stromal environment play an irreplaceable role in understanding diseases and screening for potential drugs. In this article, we describe how to implant breast cancer cells into the mammary fat pad in a simple, less invasive, and easy-to-handle way, and follow the metastasis to distant organs. With the proper features of primary tumor growth, breast and nipple pathological changes, and a high occurrence of other organs' metastasis, this model maximumly mimics human breast cancer progression. Primary tumor growth in situ, long-distant metastasis, and the tumor microenvironment of breast cancer can be investigated by using this model.
Introduction
Breast cancer is the leading cause of female mortality worldwide. With its progressively increasing incidence, breast cancer has become a serious challenge to public health1. Murine cancer models are good bridges between preclinical and clinical studies, and a good mimic murine disease model will increase the accuracy of research on disease and medicine.
Primary tumor growth starts the progress of malignant disease, while metastasis and complications are the main causes of death and poor life qualities in most cancer patients. Several murine models are used to mimic the pathology of human breast cancer2,3,4. Xenograft models are widely used for cancer study to understand the pathological characters and to screen drugs for safety and efficacy5,6,7. Genetically engineered mice (GEM) are generated to mimic human breast cancer by targeting certain oncogenes or tumor suppressor genes8. GEM have a relatively simple and uniformed background to understand the role of genes in cancerous progress; however, the artificial environment and background are limited to investigate the metastasis pathology and related therapies9. Human cancer cells, although with human pathological features, can only be implanted in immune-deficient mice, and the insufficiency of the tumor-host immune interaction may lead to biased results10.
Where the solid tumor initiates has a direct influence on the biological and pathological characters of the disease11,12,13. Since cancerous progress is the complicated outcome of interactions among tumor cells, stromal cells, immunology cells, inflammatory cells, growth factors, and proteases, primary tumors implanted in situ will provide better insight and mimic the cancerous process more accurately than tumors induced by chemical agents or a subcutaneous injection of tumor cells. Chemical agents used to induce tumors may be harmful to researchers and environment and are even forbidden in some countries. Because of the absence of a mammary fat pad environment, the pathological progress of a subcutaneous injection may differ with that in real breast cancer patients, whose cancer originates and irritates from the mammary fat pad. The disadvantages of subcutaneous injections encourage the use of orthotopic models to study tumor growth. In earlier research, highly metastatic MDA-MB-231 tumors, developed after seven orthotopic transplantations, indicated the importance of the injection location14. Recently, the orthotopic implantation of breast cancer cells into the mammary fat pad with surgery was reported15,16. With the mammary pad environment, the tumor growth and the migration into distant organs cover the entire process of breast cancer at pathologically relevant sites, which makes this model a miniature of the progress of human diseases. However, after the surgery, the skin automatically attempts to heal itself, which may bring the potential risk of interfering with the normal breast cancer origination and bias the results.
We have compared some breast cancer models and established a minimally invasive orthotopic model to investigate the potential effect of drugs on breast cancer progression17,18. In this study, a video protocol on how to orthotopically inject breast cancer cells into the mammary fat pad in a simple, less invasive way is presented. This orthotopic injection method without surgery is advantageous in many ways. First, the operation is simple and rapid, about 1 minute per mouse. Second, with primary tumor foci starting at the right pathological sites, it covers the whole tumorigenic process of breast cancer progression from the tumor growth to other organs metastasis, which provides a good experimental animal model for studying the interaction of tumor cells and tumor microenvironment. Besides, it can be a valuable model to estimate the treatment effects at all stages of breast cancer. The goal of this method is to provide an animal model to maximumly mimic human breast cancer progression.
Protocol
Animal experiments were conducted in accordance with the Provision and General Recommendation of Chinese Experimental Animal Administration Legislation and were approved by the Institution of Animal Care and Use Committee of Capital Medical University (Ref no. AEEI-2014-052). Female Balb/c mice aged 6 to 8 weeks were used.
1. Preparation of the Cells and Animals
- One day before the operation, shave the hair around the fourth nipples to expose the operating area.
- Use one hand to hold the mouse tightly at the back to make sure the mouse will not move freely, turn up the mouse to expose its belly to the operator, and then use another hand to shave the fur around the fourth nipples with an electronic shaver.
- Put a thin layer of hair removal cream around the nipples for 30 – 60 s, clean away the cream with distilled water, and then dry the mouse with soft paper.
- On the day of the operation, collect murine breast cancer cells (4T1-luc2), count the cell number, and adjust the cell density to 2 x 105 cells/mL in phosphate-buffered saline (PBS) in sterile microcentrifuge tubes and keep them on ice. For each mouse, 1 x 104 cells/50 µL in a 1-mL syringe is prepared.
2. Orthotopic Injection
- Anesthesia of mice
- Induce anesthesia. Put the mice in a closed transparent container and turn on 2% isoflurane gas to anesthetize the mice for about 5 min, till they all lie down and fall asleep.
- Maintain anesthesia. Transfer the mice from the container to individual anesthesia masks, put some vet ointment on their eyes to avoid dryness, keep the mice supinely with their nipples exposed to the operator, and let them continue to inhale isoflurane gas for a few minutes until the injection has been performed.
- Confirm the success of anesthesia by the lack of a toe pinch withdrawal reflex.
- Apply ophthalmic ointment to the eyes of the mice to prevent eye dryness.
Note: According to the container size and the number of individual anesthesia masks available, a group of mice can be anesthetized together and injected one by one under individual anesthesia.
- Performance of the injection
- Use one hand to tent up the skin around the fourth nipple with tweezers, to set up an uplifted “tunnel” for the syringe to follow. Use the other hand to hold the syringe with the needle turned upwards to enter the skin subcutaneously at 5 – 10 mm from nipple; then, follow the “tunnel” until the needle tip comes close to the nipple, carefully move the needle tip up into the mammary fat pad till the needle eye comes under the nipple tip, discard the tweezers, and inject the cells slowly.
- Turn around the needle a little and retract the syringe slowly; use a cotton swab to press the needle wound for 10 – 20 s to make sure there is no fluid seepage.
- Observe the fourth nipple to confirm a successful injection: one white transparent flat sphere with the nipple as the center can be observed (Figure 1).
- Keep the mice anesthetized for another minute to avoid letting the mice recover and move too quickly, which will cause the injection wound to open and the tumor cells to leak out.
3. Analysis of the Tumor Growth and Metastasis
Note: Primary tumors are identified as transparent or blister-like bumps after injections, and as spherical or ellipsoid solid lumps with the nipple a few days later. Tumor growth is evaluated by tumor volume and tumor bioluminescence.
- To establish the tumor volume, hold the mouse with one hand. Expose its belly to the operator and use the other hand to caliper the tumor length (L) and width (W). Calculate the tumor volume (V) as follows.
V = (L x W2)/2 - To capture the tumor bioluminescence, inject 150 mg/kg D-luciferin at the back of the mouse’s neck, 10 min before imaging. Anesthetize the mice with 2% isoflurane gas for 5 min and transfer them to individual anesthesia masks to let them inhale isoflurane gas for 5 min longer. Following the manufacturer’s instructions, capture bioluminescence images of the primary tumor and metastasis, with auto exposure time, medium binning, and f/stop at 1.
4. Harvesting of the Primary Tumor and Metastasis Organs for Analysis
Note: When achieving the purpose of this experiment, or reaching the humane endpoint, the primary tumor can be harvested for further study. In this study, tumors are removed at 4 to 5 weeks after the injection, when the tumor volume reaches about 800 mm3. The lungs are removed at week 8.
- Harvesting of the primary tumor
- Perform the surgery in a sterile hood to maintain a sterile atmosphere. Anesthetize the animals by isoflurane. Confirm the success of anesthesia by the lack of toe pinch withdrawal reflexes. Apply ophthalmic ointment to the eyes of the mice to prevent them from drying out.
- Dissociate the tumor from the skin with scissors, dropwise painkiller (1 mg/mL tramadol, 1 drop of about 50 µL per mouse) to relieve postoperative pain.
- Stitch the skin with a surgical suture, cut off excess suture, drape off the incision.
- Cut the primary tumor in half with a scalpel, put 1/2 of the tumor into 4% paraformaldehyde for further hematoxylin and eosin (H&E) staining and immunohistochemistry, and immediately freeze the other 1/2 with liquid nitrogen for western blotting or an RNA isolation study later.
- After suturing, warm the mice with a lamp till they recover, keep the mice in single cages until fully recovered. Continuously administer 10 mg/kg tramadol with an oral gavage for 3 d after the surgery.
- Harvesting of metastasis organs
- Euthanize the mice with an overdose of pentobarbital, open their chests with scissors, gently take out the lungs, and wash them with PBS. Lung metastasis foci can be identified as white transparent bumps which are morphologically different and distinguishable from normal pink lung tissue.
- Put the lungs into 4% paraformaldehyde to verify the metastasis by H&E staining.
Representative Results
After a successful injection, one white transparent flat sphere with the nipple as the out-surface round center can be observed (Figure 1). Primary tumor growth can be measured by tumor volume and living tumor cell bioluminescence (Figure 2). Both the tumor volume and the total flux increased during the experiment before resection. At an early stage, metastasis cannot be found because no secondary tumor has happened or the strong bioluminescent signals of the primary tumor obstruct the detection of small metastasis foci with weak signals. After resection, the bioluminescent signal from the metastatic foci of distant organs can be detected and analyzed. The morphology of both the primary breast tumor and the lung sections were studied with H&E staining, while angiogenesis was investigated by staining the tumor with vessel marker CD31 for microvessel density (MVD) (Figure 3).
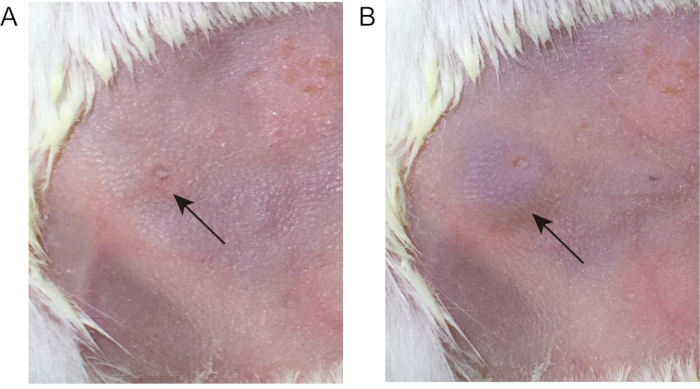
Figure 1: Pictures before and after the orthotopic injection at the mammary fat pad of female Balb/c mice. The operation was performed, and the pictures were taken while the mice were under isoflurane anesthesia. A, before injection, B, after injection.
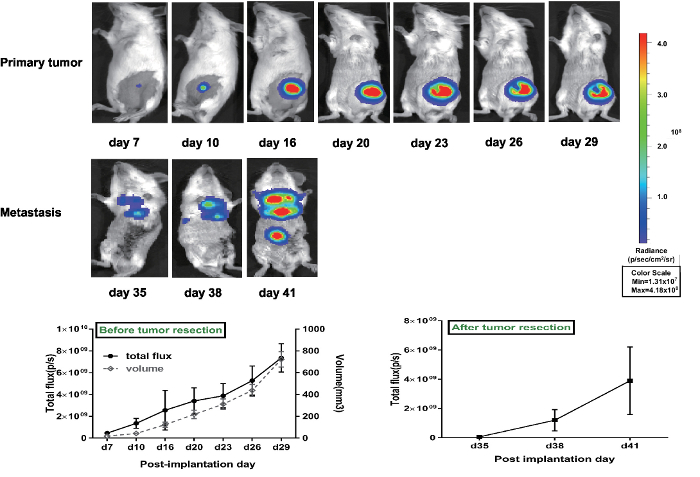
Figure 2: Volume and total flux of the primary tumor were measured from 7 days after the implantation. The cell suspension implantation generated an increased primary tumor both in volume, which was visualized and determined using calipers, and in total flux, which was measured by the Spectrum system. The figure shows bioluminescent images of primary tumors and metastasis observed at various time points after day 7 of implantation. p/s = photons/second. This figure has been modified from Zhang et al.17. Please click here to view a larger version of this figure.
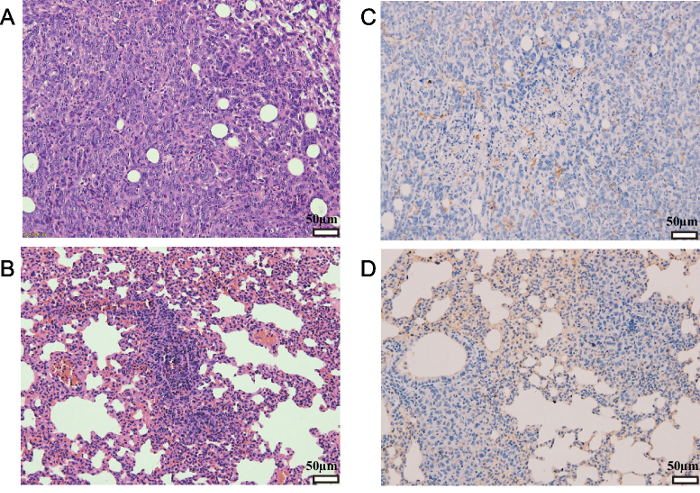
Figure 3: H&E staining and immunohistochemical staining analysis of primary tumors and lung metastasis. Tissues were fixed in 4% paraformaldehyde, embedded in paraffin, and stained. (A and B) Sections were stained with hematoxylin and eosin (H&E). (C and D) Sections were stained with antiCD31 antibody. Brownish staining indicated CD31+ vessels. Panels A and C present primary tumor tissue, panels B and D present lung metastasis. CD = cluster of differentiation. The magnification used = 200X. The scale bar = 50 µm. This figure has been modified from Zhang et al.17. Please click here to view a larger version of this figure.
Discussion
The cells used in this study are 4T1-luc2, murine triple-negative breast cancer cells with luciferase labeling, which are a useful tool for investing antitumor and antimetastatic effects of drugs due to their highly invasive nature2,19. Luciferases, stable to the next cell generation, are used to indicate the living tumor cells, both at the mammary gland and at other distant organs20. In some cases, hypoxia and nutrient deficiency within the tumor result in a decrease in the bioluminescent signal, and the volume of the primary tumor is not inconsistent with the bioluminescent signal at a later stage of tumor progression. The technique of the cellular orthotopic injection (COI) of cell suspensions can also be performed with other breast cancer cell lines, such as human cells MDA-MB-231 (unpublished data). In this study, with the mammary gland as its environment, it is a proper animal model to study tumor microenvironment, crossing talking between tumor cells and stromal cells. During the tumor progress, in some mice, the nipple can ulcerate, scab, grow red granulation tissue, flatten, or even disappear, similar to what happens in human nipples during breast cancer. Mice may experience discomfort with ulcerations; humane care should be taken. More nipple change has been found in mice using this COI technique than with the micro-invasive surgery technique. The surgical orthotopic implantation (SOI) of histologically intact human tumor tissue, compared with the cellular orthotopic injection (COI) of cell suspensions, shows higher malignant cancers in the bladder, lung, stomach, kidney, and colon21 that mimic what is seen in patients22.
With a high incidence of metastasis, especially lung metastasis, the murine breast cancer model established in this study is a good syngeneic cancer model to explore the spontaneous migration and invasion, compared with an artificial metastasis model, such as a tail vein injection. The tumor cell activities and characters also play important roles in metastasis. Other cell lines, such as human breast cancer cell MCF-7, even implanted by an orthotopic injection at the mammary fat pad of immune-deficient Balb/c mice, have a lower metastatic ability. With the modification of cells or mice, such as the over-expression or down-expression of a certain gene, this technology can be applied in more research fields.
The crucial operation of this injection is to carefully and slowly move up the needle tip, from subcutaneous into the mammary fat pad. When the syringe tip comes close to the nipple, the operator will feel insistence from the tissue. Since the mouse gland is very small, only a little more pressure is needed to let the syringe tip pass through the insistence. Too much pressure will result in the tip passing through the gland and breaking the skin, which results in a failure of the injection. Logarithmic-phase cells, a single-cell suspension, the standard operation protocol (SOP), and skilled operators are all required to reduce the variation among mice. Tumor cell behavior is important for the formation and the repeatable of tumor models. Harvest logarithmic-phase cells when they grow to about 80% – 90% confluence; too low or too high cell densities will interfere with the tumor model and result in variations between experiments. The single-cell suspension is also important since cell clumps result in miscalculations of the cell number. Trypsin, an EDTA solution, or other appropriate methods are chosen to detach the cells according to the experiment aims and the targets the researcher is interested in. Dependent on the syringe scale and cell density, the injection volume could vary from 25 to 100 µL. The amount of 1 x 104 to 1 x 106 cells is commonly used to irritate tumor growth according to different cell types. Trypan blue staining is used to distinguish viable cells from dead ones. More than 95% cell viability is regarded as a good situation to induce a rapid tumor growth and metastasis in vivo. These are also suitable for any other tumor models when preparing tumor cells. To correctly caliper the primary tumor size and get an accurate bioluminescent signal, the fur around the nipple should be removed again once it grows back. When the primary tumor grows to a large mass and its bioluminescent signal is too strong for researchers to observe other organ metastases (e.g., lung metastasis), cover it with black electrical tape before bioluminescence images are taken, or remove it by surgery. A painkiller can be used for post-surgical pain.
Successful inoculation can result in lung metastasis: with an occurrence rate of more than 90%, metastatic foci at non-injected breasts, bone, or lymph nodes are quite common, while celiac metastasis is rare. The secondary tumors are a translucent mass and can be distinguished from the surrounding normal tissues. An imprecise application of the injection can lead to experimental errors in tumor size and shape and metastasis locations. Any leakage from the flat sphere after the injection will reduce the tumor size, any leakage from the mammary gland into the "tunnel" will result in a long cylindrical tumor which will obstruct the determination of the tumor volume when we use a digital caliper to measure it. Subcutaneous injections around the mammary fat pad seldom lead to lung metastasis and are not suitable for distant metastasis-associated study. To make the inoculation stable and reduce the risk of leakage, Matrigel can be used when suspending tumor cells. However, Matrigel is not a single solvent, it is regarded as a kind of extracellular matrix (ECM), and some types of gel even contain factors which may interfere with the experiments. In the experiment aimed at tumor microenvironment, ECM, crossing talking among tumor cells or with stromal cells, it is better to avoid using Matrigel. For injected cells with the luciferase tag D-luciferin, the substrate of luciferase is injected to bind the living tumor cells in mice. In this study, the dynamics of bioluminescence in vivo suggested that at 10 minutes after D-luciferin injection, the bioluminescent signal reach the peak and can be stable for about 10 – 15 minutes (varying between different mice), whether with an intraperitoneal injection or a subcutaneous injection. Considering the tested drug is injected intraperitoneally, to avoid the interaction of the tested drug with D-luciferin and to reduce the peritoneal irritation, a subcutaneous injection is suggested.
In conclusion, the orthotopic injection of breast cancer cells outlined in this paper is a very useful and powerful tool in studying the pathology and progression of breast cancer. It is easy to handle and can be performed quickly. The primary tumor originates at the mammary gland with a high occurrence of metastasis, which maximumly mimics the pathophysiological process of human breast carcinoma.
Divulgaciones
The authors have nothing to disclose.
Acknowledgements
The authors would like to thank the National Natural Science Foundation of China (grant no. 81873111, 81673924, 81774039, 81503517), the Beijing Natural Science Foundation (grant no. 7172095, 7162084, 7162083), and the Xu Xia Foundation of the Beijing Hospital of Traditional Chinese Medicine (grant no, xx201701). We thank Prof. Chang-Zhen Liu, from Experimental Research Center, China Academy of Chinese Medical Sciences, for bioluminescent images.
Materials
| anesthesia machine | Midmark Corporation, Dayton, OH, USA | Matrx VMS | anesthesia |
| In-Vivo Imaging System | PerkinElmer | IVIS Spectrum | used for bioluminescence detecion |
| isoflurane | Hebei yipin chemical reagents company | O21400 | anesthesia |
| 1 ml syringe | Becton,Dickinson and Company | A257 | cell injection |
| digital caliper | Shang Hai Shen Han Measuring Tools Co., Ltd. | S-H | volume measurement |
| tramadol | Mundipharma company | – | pain killer |
| D-luciferin | Gold Biotechnology Inc. | LUCK-1G | used for bioluminescence detecion |
| The primary antibody against cluster of differentiation (CD) 31 | Abcam | ab28364 | used for MVD detection |
| hematoxylin and eosin staining kit | Beijing Zhong Shan Jinqiao Biotechnology Co., Ltd. | ZLI-9615 | histology |
| hair removal cream | Veet | – | hair removal cream |
| Carbomer Eye Gel | Dr.GerhardMannChem-Pharm.FabrikGmbH | – | ophthalmic ointment |
| sewing needle | Shanghai Pudong Jinhuan Medical Products Co., Ltd. | 17U0302J | suture |
Referencias
- Torre, L. A., et al. Global cancer statistics. CA: A Cancer Journal for Clinicians. 65 (2), 87-108 (2012).
- Rashid, O. M., Takabe, K. Animal models for exploring the pharmacokinetics of breast cancer therapies. Expert Opinion on Drug Metabolism & Toxicology. 11 (2), 221-230 (2015).
- Wagner, K. U. Models of breast cancer: quo vadis, animal modeling. Breast Cancer Research. 6 (1), 31-38 (2004).
- Horas, K., Zheng, Y., Zhou, H., Seibel, M. J. Animal models for breast cancer metastasis to bone: opportunities and limitations. Cancer Investigation. 33 (9), 459-468 (2015).
- Kawaguchi, T., Foster, B. A., Young, J., Takabe, K. Current Update of Patient-Derived Xenograft Model for Translational Breast Cancer Research. Journal of Mammary Gland Biology and Neoplasia. 22 (2), 131-139 (2017).
- Wright, L. E., et al. Murine models of breast cancer bone metastasis. BoneKEy Reports. 5, 804 (2016).
- Cassidy, J. W., Batra, A. S., Greenwood, W., Bruna, A. Patient-derived tumour xenografts for breast cancer drug discovery. Endocrine-Related Cancer. 23 (12), T259-T270 (2016).
- Stiedl, P., Grabner, B., Zboray, K., Bogner, E., Casanova, E. Modeling cancer using genetically engineered mice. Methods in Molecular Biology. 1267, 3-18 (2015).
- Menezes, M. E., et al. Genetically engineered mice as experimental tools to dissect the critical events in breast cancer. Advances in Cancer Research. 121, 331-382 (2014).
- Talmadge, J. E., Singh, R. K., Fidler, I. J., Raz, A. Murine models to evaluate novel and conventional therapeutic strategies for cancer. The American Journal of Pathology. 170 (3), 793-804 (2007).
- Spaw, M., Anant, S., Thomas, S. M. Stromal contributions to the carcinogenic process. Molecular Carcinogenesis. 56 (4), 1199-1213 (2017).
- Joyce, J. A., Pollard, J. W. Microenvironmental regulation of metastasis. Nature Reviews Cancer. 9 (4), 239-252 (2009).
- Hanahan, D., Weinberg, R. A. Hallmarks of cancer: the next generation. Cell. 144 (5), 646-674 (2011).
- Yano, S., et al. Tumor-targeting adenovirus OBP-401 inhibits primary and metastatic tumor growth of triple-negative breast cancer in orthotopic nude-mouse models. Oncotarget. 7 (51), 85273-85282 (2016).
- Kocaturk, B., Versteeg, H. H. Orthotopic injection of breast cancer cells into the mammary fat pad of mice to study tumor growth. Journal of Visualized Experiments. (96), e51967 (2015).
- Tavera-Mendoza, L. E., Brown, M. A less invasive method for orthotopic injection of breast cancer cells into the mouse mammary gland. Lab Animal. 51 (1), 85-88 (2017).
- Zhang, Y., et al. Establishment of a murine breast tumor model by subcutaneous or orthotopic implantation. Oncology Letters. 15 (5), 6233-6240 (2018).
- Zhang, Y., et al. Gubenyiliu II Inhibits Breast Tumor Growth and Metastasis Associated with Decreased Heparanase Expression and Phosphorylation of ERK and AKT Pathways. Molecules. 22 (5), (2017).
- Kwon, Y. S., Lee, K. S., Chun, S. Y., Jang, T. J., Nam, K. S. Suppressive effects of a proton beam on tumor growth and lung metastasis through the inhibition of metastatic gene expression in 4T1 orthotopic breast cancer model. International Journal of Oncology. 49 (1), 336-342 (2016).
- Kalra, J., et al. Validating the use of a luciferase labeled breast cancer cell line, MDA435LCC6, as a means to monitor tumor progression and to assess the therapeutic activity of an established anticancer drug, docetaxel (Dt) alone or in combination with the ILK inhibitor, QLT0267. Cancer Biology & Therapy. 11 (9), 826-838 (2011).
- Hoffman, R. M. Orthotopic metastatic mouse models for anticancer drug discovery and evaluation: a bridge to the clinic. Investigational New Drugs. 17 (4), 343-359 (1999).
- Hoffman, R. M. Patient-derived orthotopic xenografts: better mimic of metastasis than subcutaneous xenografts. Nature Reviews Cancer. 15, 451 (2015).

