Three-dimensional Navigation-guided, Prone, Single-position, Lateral Lumbar Interbody Fusion Technique
Summary
The single-position, prone, lateral approach allows for both lateral lumbar interbody placement and direct posterior decompression with pedicle screw placement in one position.
Abstract
Lateral interbody fusion provides a significant biomechanical advantage over the traditional transforaminal lumbar interbody fusion due to the large implant size and optimal implant position. However, current methods for lateral interbody cage placement require either a two-staged procedure or a single lateral decubitus position that precludes surgeons from having either full access to the posterior spine for direct decompression or comfortable pedicle screw placement.
Herein is one institution’s experience with 10 cases of a prone single-position approach for simultaneous access to the anterior and posterior lumbar spine. This allows both lateral lumbar interbody cage placement, direct posterior decompression, and pedicle screw placement, all in one position. Three-dimensional (3D) navigation is utilized for increased precision in both approaching the lateral spine and interbody cage placement. The traditional blind psoas muscle tubular dilation was also modified. Tubular retractors and lateral vertebral body retractor pins were used to minimize the risks to the lumbar plexus.
Introduction
First described as extreme lateral interbody fusion (XLIF) in 2006, the lateral lumbar interbody fusion approach (LLIF) utilizes a transpsoas approach to the vertebral body1. The LLIF presents several operative advantages over other traditional approaches. First, the LLIF is one of the least invasive interbody fusion approaches, minimizing perioperative tissue damage and blood loss, as well as postoperative pain and length of hospital stay2,3. The LLIF allows for the placement of larger interbody spacers, which confers a greater likelihood of fusion and greater disc height distraction4,5.
Several LLIF protocols are currently employed, each of which presents limitations. The two-stage approach requires two patient positions for cage placement and posterior screw fixation, respectively. This protocol may increase intraoperative time and anesthetic exposure as the surgeon must wait for patient repositioning between the first and second stages of the procedure. Single-position LLIF variants have also been developed to improve the two-position process. Using a stand-alone LLIF technique forgoes the posterior component of the LLIF surgery and thus negates the need for patient repositioning. However, this technique precludes direct posterior decompression and the added stability of pedicle screw placement. Performing the entire surgery in the lateral position has also been described, but this introduces additional ergonomic challenges for the surgeon6,7.
A prone single-position approach effectively decreases operative time, thus speeding patients’ recovery. Below, the protocol for performing a prone single-position approach for simultaneous access to the anterior and posterior lumbar spine is outlined. Unlike a previously described variation of this approach, 3D navigation is employed to guide both the lateral approach and the interbody cage placement8. Finally, this article includes a case series of the first 10 patients who underwent this prone, lateral lumbar interbody fusion (Pro-LLIF) procedure at the authors’ institution.
Protocol
NOTE: The protocol follows the guidelines of and was approved by the Brigham human research ethics committee.
1. Equipment and positioning
- Use an open Jackson table for the procedure. Ensure the availability of both frameless stereotactic navigation and intraoperative neuromonitoring with lower extremity electromyography (EMGs), which are critical to the success of the case.
NOTE: An open Jackson table allows the abdominal viscera to fall away from the spine during the lateral approach. - Place the patient in the prone position with legs extended. Pay special attention to the hip and/or thigh pads on the side that the interbody spacer will be introduced. If required, shift these pads caudally before the procedure begins if they crowd into the anticipated lateral entry point below the patient's lowest ribs.
2. Initial posterior approach and posterolateral instrumentation
- Expose the posterior elements first via a midline incision over the target levels. Open the fascia in standard fashion, and dissect the paraspinal musculature off the bony elements, including the eventual pedicle screw entry points. Next, place a spinous clamp and have the radiology technician bring in the O-arm to obtain an intraoperative computed tomography scan to allow for stereotactic navigation.
- Next, place pedicle screws at the appropriate levels in a standard fashion with navigation assistance.
NOTE: Doing so at this step ensures that the pedicle screws are placed before the navigation is disturbed, either inadvertently during the case or intentionally by the placement of the interbody cages. Moreover, placement of the screws can aid in the lateral discectomy portion of the case.
3. Lateral approach and interbody cage placement
- Next, start the lateral approach. Using the navigation, mark a skin incision on the flank, positioning it such that it will bring the surgeon perpendicularly across the mid-point of the target disc space (or allow for multiple such trajectories if inserting interbody cages at multiple levels).
- At this point, rotate the patient's bed away for a more comfortable working position for the surgeon (i.e., "airplaning"). Similarly, consider using a sitting stool to drop the surgeon's working angle to allow for a more comfortable approach (Figure 1).
- Make a 2'' to 3'' incision in the patient's flank, parallel to the patient's ribs. Dissect through the subcutaneous fat and external oblique fascia using electrocautery. Next, dissect with a pair of Metzenbaum scissors to spread open the external oblique, internal oblique, and transverse abdominus muscles and gain access to the retroperitoneal space.
- Once the potential retroperitoneal space is encountered, use fingers for blunt dissection of the space to feel the peritoneal cavity pulling away through the force of gravity and then rapidly encounter the bulk of the psoas muscle overlying the spine. Feel the transverse process as a landmark posteriorly. Use fingers for further blunt dissection to separate the retroperitoneal cavity more thoroughly from the lateral spine surface, especially in the cranial-caudal direction to minimize the chance of inadvertently entering the peritoneal cavity in the subsequent steps.
- Next, place a table-mounted, lighted, lateral-access retractor system just superficial to the psoas muscle (Figure 2).
- To enter the psoas, first, use a navigation-guided fenestrated probe to select an optimal entry point and approach angle into the target disc space. Then, place A K-wire through the fenestrated probe into the disc space to secure the access.
- Place sequential dilators over the probe superficial to the psoas muscle until finally, the table-mounted retractor system is brought in and secured.
- Connect the light source to the retractor blades. Then, open the retractor blades in the cranial-caudal and anterior-posterior directions to visualize the surgical area directly.
- Next, dissect the psoas muscle under direct vision using long Panfield 4 and long Kittner dissectors to expose enough disc space to accommodate the width of the cage (generally 18 mm). If required, use EMG monitoring to monitor the lumbosacral space.
NOTE: Under direct vision, the lumbosacral plexus nerves traveling on the surface of the psoas muscle are easily identified and avoided to minimize injury to those nerves. Traversing the psoas in a separate step, under direct vision with the lighted retractor system, allows for greater ability to avoid damage to the lumbosacral plexus.- Once the disc space is fully exposed, place two pairs of pins in the cranial and caudal vertebral bodies to keep the surgical corridor through the psoas muscle open.
NOTE: The pins keep the psoas muscle (and the associated plexus nerves) clear of the surgical corridor, thus providing a comfortable and safe surgical environment. It eliminates the muscle creeping problem commonly encountered with the expandable tubular retractor system (Figure 3).
- Once the disc space is fully exposed, place two pairs of pins in the cranial and caudal vertebral bodies to keep the surgical corridor through the psoas muscle open.
- Ensure that the disc space is adequately exposed in both the cranial-caudal and the anterior-posterior dimensions. Perform an annulotomy with a #15 blade, and perform an initial discectomy using pituitary rongeurs and curettes.
- During this step, break the annulus on the contralateral side using a navigated cobb elevator to release the space and facilitate a larger interbody cage placement and scoliosis correction when needed.
- Insert the navigated cobb elevator into the disc space. Under the navigation guidance, advance the tip of the cobb elevator beyond the contralateral disc border and "pop" it through the contralateral annulus for annulus release.
NOTE: Due to the cobb elevator being navigated, the location of the tip of the cobb elevator can be tracked at all times. Therefore, take care not to violate the annulus on either the anterior or posterior side to protect the great vessels and the thecal sac, respectively.
- Insert the navigated cobb elevator into the disc space. Under the navigation guidance, advance the tip of the cobb elevator beyond the contralateral disc border and "pop" it through the contralateral annulus for annulus release.
- Of note, with simultaneous access to the posterior spine while this is going on, place the pedicle screws in distraction at this time if needed.
NOTE: This not only facilitates entrance into particularly narrow and collapsed disc spaces but also allows for the placement of a larger interbody spacer than would be possible otherwise.
- During this step, break the annulus on the contralateral side using a navigated cobb elevator to release the space and facilitate a larger interbody cage placement and scoliosis correction when needed.
- Afterwards, use sequentially larger navigated shavers and navigated cage trials to prepare the disc space further. Take care to avoid violating the bony endplates. Once an appropriately sized cage trial is determined, insert the corresponding interbody cage (Conduit lateral Interbody cage) with navigation guidance (Figure 4). Before inserting the cage, fill the cage with allograft bone chips or any grafting materials of the surgeon's choice.
- Remove the pins holding back the psoas muscle and achieve hemostasis. At this point, shift the lighted retractor system to another target level if multiple interbody cages are intended to be placed. Otherwise, remove the system and close the muscle, fascia, and skin in a layered fashion.
4. Completion of the posterior portion
- Should further posterior decompression be needed (e.g., laminectomy), perform it at this point.
NOTE: This can also be performed simultaneously during some portions of the lateral procedure if a second qualified operator is available (Figure 1). - Finally, place rods to connect the pedicle screws, decorticate the spine, and place a morselized bone graft in a standard fashion. Routinely place vancomycin powder in the cavity, place wound drains, and use liposomal bupivacaine in the back musculature. Perform the closure in the standard layered fashion, including muscle, fascia, subcutaneous tissues, and skin.
NOTE: Closure can be performed simultaneously with the closure of the lateral incision should it fit with the workflow of the individual case.
Representative Results
Cohort demographics
Ten consecutive patients underwent the Pro-LLIF procedure from August 2020 to February 2021. The eligibility criteria for this procedure were ages 18 and older and symptomatic degenerative spondylosis with spinal instability (spondylolisthesis or degenerative scoliosis) from L2 to L5, requiring interbody fusion. Per the institution's standard of care, all patients had trialed and failed a course of conservative management. The exclusion criteria were patients excluded from operative intervention based on their medical inability to tolerate surgery. In addition, in patients with unfavorable anatomies, especially if the L4-5 disc level is caudal to the top of the iliac crest, it would be difficult to use the Pro-LLIF approach. All operations were performed by the same neurosurgeon (Y.L.).
The initial Pro-LLIF cohort comprised eight female and two male patients. The mean age at the time of surgery was 66 years, with individual ages ranging from 41 to 77 years. Eight patients were current or former smokers, and five patients met the Center for Disease Control's definition of obesity (BMI > 30).
Spondylolisthesis was the most common spinal disease amongst this cohort (five patients). The most common indication for surgery was radiculopathy with low back pain (six patients), followed by radiculopathy alone (three patients). Four patients had undergone prior fusion procedures.
Operative characteristics
The majority of the patients in this cohort (60%) underwent one level of Pro-LLIF (Table 1). The mean total operative time for the Pro-LLIF procedure was 4.5 h (median 4.1 h, range 3.2-6.9 h). The total time under anesthesia averaged 6.5 h (median 5.9 h, range 4.2-9.7 h). The average estimated blood loss during the Pro-LLIF procedure was 240 mL (range 50-650 mL).
Preoperative and postoperative magnetic resonance images (MRIs) of the lumbar spine were used to evaluate the changes in foraminal height, segmental lordosis, lumbar lordosis, and disc height after undergoing Pro-LLIF (Table 2). For some patients, the foraminal height or lumbar lordosis improvement is limited, which might be due to the significant disc space and facet joint stiffness in those patients.
Hospital course, length of stay, and dispensation
Pro-LLIF patients experienced an average length of stay of 3.5 days. One patient required early reoperation to recover a retained surgical drain in the posterior incision. No neurological injury or subsidence was reported for any patient in the immediate postoperative period. Six of the ten patients were discharged to home; the remaining four patients were discharged to rehabilitation facilities.
Follow-up and postoperative clinical evaluation
One-month follow-up data were available for all ten patients. The Odom Criteria's 4-point rating scale was adapted to assess Pro-LLIF surgical outcomes (Table 3). At one month, three patients met the criteria for an "Excellent" rating, and six patients reported symptoms consistent with a "Good" rating. One patient reported similar symptoms post-ProLLIF, earning the patient an Odom rating of "Poor." That patient was a complex lumbar deformity patient who has failed multiple surgeries in the past with the development of severe left leg pain following a previous lumbar fusion surgery at another hospital.
Comparison with a propensity score-matched cohort analysis
Retrospective data were also collected on patients who had undergone oblique lateral interbody fusion (OLIF) procedures at the same institution by the same senior neurosurgeon. Using propensity-score matching, 10 OLIF patients were identified who had undergone comparable levels of lateral interbody fusion and decompression as the Pro-LLIF patients. Student's two-sided, unpaired t-tests with Bonferroni multiple-comparison correction were used to compare the quantitative outcome measures between the Pro-LLIF and OLIF groups. No significant differences in total operative time, total anesthesia time, lengths of stay, and estimated blood loss were identified between the Pro-LLIF and OLIF patients (Figure 5).
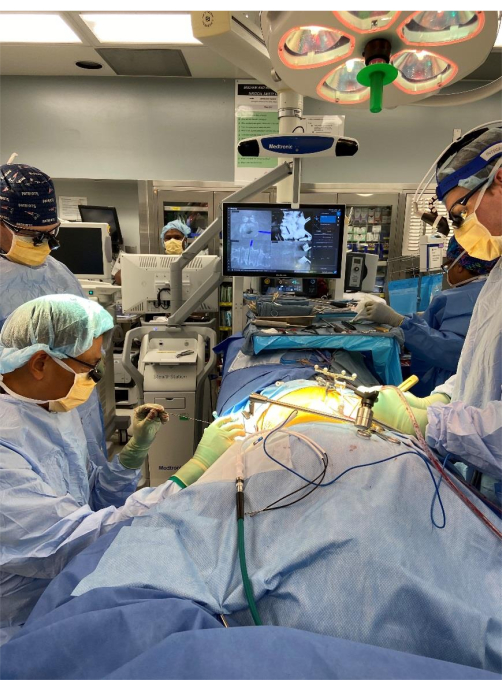
Figure 1: Intraoperative view of single-position pro-LLIF procedure, showing the setup, air-planing of the operative table, and intra-operative navigation and two surgeons performing the lateral and the posterior portions of the surgery simultaneously. Abbreviation: pro-LLIF = prone lateral lumbar interbody fusion. Please click here to view a larger version of this figure.
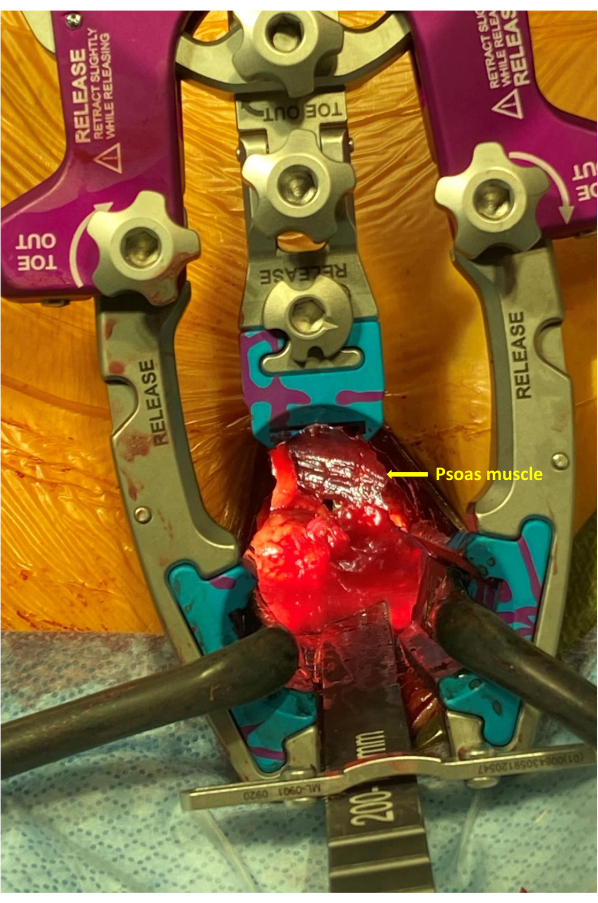
Figure 2: Intra-operative close-up view showing the placement of the expandable retractor system superficial to the psoas muscle in the retroperitoneal space, providing a clear view for direct psoas dissection. Please click here to view a larger version of this figure.
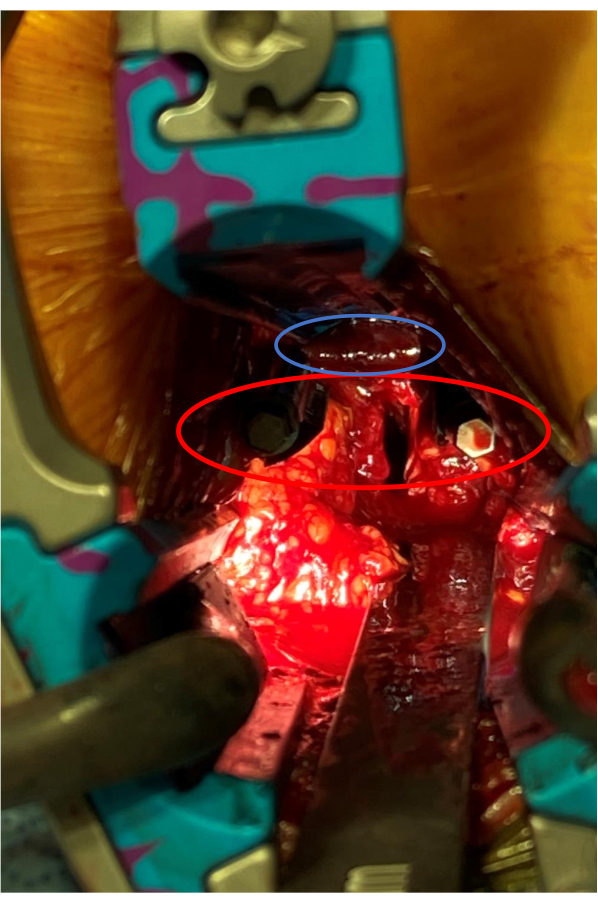
Figure 3: Following direct psoas muscle dissection, separate retractor pins (in red oval) placed in the cranial and caudal vertebral bodies kept the psoas muscle (in blue oval) out of the surgical corridor, allowing easy disc preparation and interbody cage placement. Please click here to view a larger version of this figure.
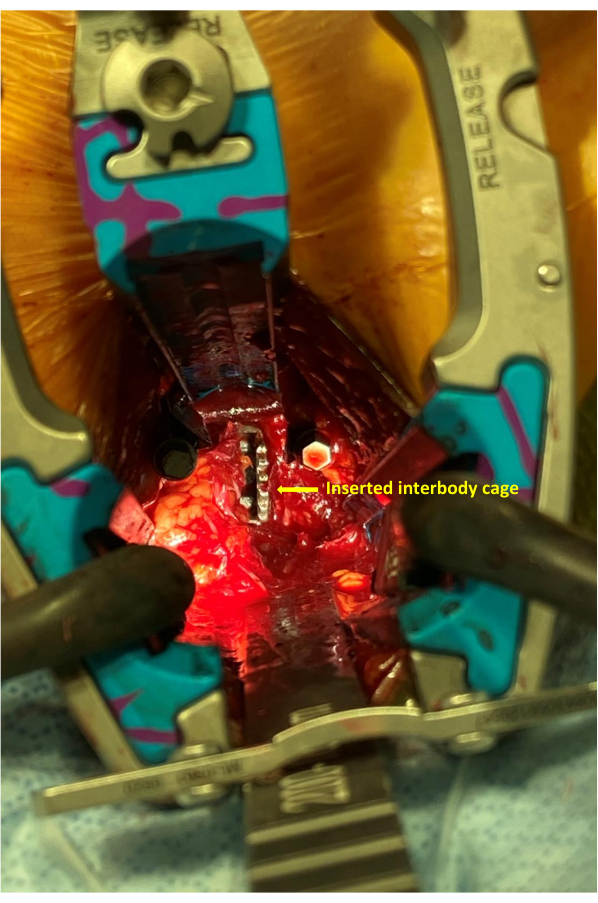
Figure 4: After the disc preparation, the lateral Conduit titanium interbody cage is inserted into the disc space. Please click here to view a larger version of this figure.
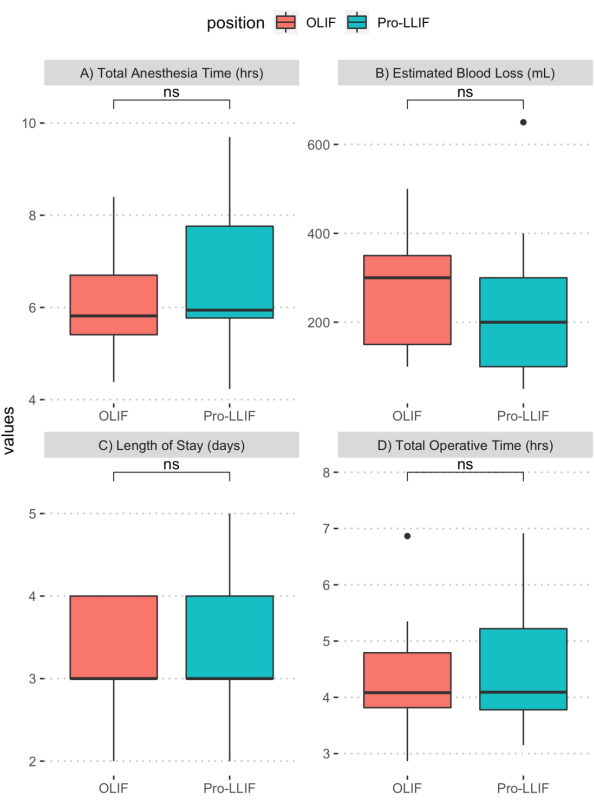
Figure 5: Comparison of operative outcomes between Pro-LLIF and OLIF patients. Student's two-sided, unpaired t-tests were used to compare (A) total anesthesia time (h), (B) estimated blood loss (mL), (C) lengths of stay (days), and (D) total operative time (h). Bonferroni correction was used to adjust for multiple comparisons. No significant difference between the Pro-LLIF and OLIF cohorts was identified for any of the evaluated outcome measures. Abbreviations: pro-LLIF = prone lateral lumbar interbody fusion; OLIF = oblique lateral interbody fusion. Please click here to view a larger version of this figure.
| case | age | sex | BMI | diabetes | smoking | chronic steroids | obesity | asa | Prior fusion | disease | indication | Operated levels | ||||||||||
| 1 | 64 | 0 | 19.92 | 0 | 0 | 0 | 0 | 2 | 1 | spondylolisthesis | radiculopathy/LBP | L2-L3 | ||||||||||
| 2 | 65 | 0 | 40.24 | 0 | 0 | 0 | 1 | 3 | 0 | spondylolisthesis | radiculopathy | L4-L5 | ||||||||||
| 3 | 77 | 0 | 34.72 | 1 | 1 | 1 | 1 | 3 | 1 | Sagittal deformity | radiculopathy.LBP | L2-L4 | ||||||||||
| 4 | 62 | 1 | 35.25 | 0 | 1 | 0 | 1 | 2 | 0 | spondylolisthesis | radiculopathy.LBP | L3-L4 | ||||||||||
| 5 | 68 | 1 | 33.75 | 0 | 1 | 0 | 1 | 2 | 0 | spondylolisthesis | radiculopathy | L3-L5 | ||||||||||
| 6 | 77 | 0 | 23.44 | 1 | 1 | 1 | 0 | 3 | 1 | scoliosis | radiculopathy.LBP | L3-L4 | ||||||||||
| 7 | 41 | 0 | 19.5 | 0 | 1 | 1 | 0 | 2 | 0 | degenerative | radiculopathy | L2-L3 | ||||||||||
| 8 | 72 | 0 | 35.15 | 0 | 1 | 0 | 1 | 3 | 0 | scoliosis | radiculopathy.LBP | L2-L5 | ||||||||||
| 9 | 65 | 0 | 21 | 0 | 0 | 0 | 0 | 2 | 0 | Spondylolisthesis, scoliosis | radiculopathy.LBP | L3-L4 | ||||||||||
| 10 | 74 | 0 | 22 | 0 | 1 | 0 | 0 | 2 | 1 | pseudoarthrosis | LBP | L2-L4 | ||||||||||
Table 1: Pro-LLIF cohort demographics. Basic patient demographics, surgical indications, and operative data for all 10 Pro-LLIF cases of this series. Key: 0 = no, 1 = yes. "ASA" refers to the American Society of Anesthesiologists Physical Status Classification System, which scores patients' health status and the likelihood of surgical and anesthetic comorbidities. ASA score was determined preoperatively by anesthesiology teams at this institution. Abbreviations: pro-LLIF = prone lateral lumbar interbody fusion; ASA = American Society of Anesthesiologists; BMI = body mass index.
| case | Pre-operative foraminal height | Post-operative foraminal height | Pre-operative segmental lordosis | Post-operative segmental lordosis | Pre-operative lumbar lordosis | Post-operative lumbar lordosis | Pre-operative disc height | Post-operative disc height |
| 1 | 18 | 18 | 5 | 16 | 50 | 61 | 8 | 11 |
| 2 | 14 | 20 | 15 | 18 | 30 | 39 | 7 | 15 |
| 3 | 11 | 13 | 5 | 34 | 30 | 45 | 3 | 11 |
| 4 | 21 | 21 | 6 | 20 | 80 | 109 | 12 | 16 |
| 5 | 18 | 23 | 17 | 23 | 28 | 33 | 9 | 10 |
| 6 | 14 | 15 | 4 | 13 | 35 | 50 | 2 | 8 |
| 7 | 13 | 15 | 5 | 10 | 59 | 55 | 2 | 7 |
| 8 | 16 | 15 | 16 | 25 | 40 | 70 | 3 | 10 |
| 9 | 19 | 19 | 4 | 7 | 37 | 39 | 5 | 9 |
| 10 | 19 | 19 | 33 | 23 | 60 | 60 | 12 | 15 |
Table 2: Radiographic evaluation of Pro-LLIF outcomes. Comparison of pre- and postoperative MRIs was used to assess Pro-LLIF's impact on foraminal height, segmental lordosis, lumbar lordosis, and disc height for each patient. Abbreviations: pro-LLIF = prone lateral lumbar interbody fusion; MRIs = magnetic resonance images.
| Outcome | Definition |
| Excellent | All preoperative symptoms relieved; no postoperative symptoms |
| Good | Minimal persistence of preoperative symptoms with minor postoperative symptoms |
| Fair | Relief of some preoperative symptoms with persistence or worsening of others; minor to major postoperative symptoms |
| Poor | Persistence or worsening of all preoperative symptoms; minor to major postoperative symptoms |
Table 3: Odom's criteria (adapted). A 4-point rating scale for assessing clinical outcomes post-PLLIF, adapted from Odom's criteria for cervical spine surgery outcomes. Abbreviation: pro-LLIF = prone lateral lumbar interbody fusion.
Discussion
This study provides a detailed protocol for a prone, single-position, 3D-navigation-guided lateral lumbar interbody fusion (Pro-LLIF). Pro-LLIF permits concurrent access to the anterior and posterior spine and does not require patient repositioning, unlike the two-stage OLIF or XLIF approach9. This single-position approach has been associated with decreased operative time, anesthesia time, and surgical staffing requirements, presenting physical and financial benefits8,9,10.
Critical steps in the pro-LLIF procedure include the following: 1) as this technique is reliant upon stereotactic navigation, obtaining a high-quality interoperative CT and making sure the registration continues to be accurate throughout the case is of the utmost importance. 2) Blunt dissection and separation of the retroperitoneal cavity from the lateral lumbar surface needs to be done thoroughly to make sure no peritoneal membrane is still adherent to the spine surface at the surgical area to avoid inadvertent injury to the peritoneal content. 3) As with all transpsoas approaches, care needs to be taken when traversing the psoas muscle to avoid damage to the lumbosacral plexus. Splitting the psoas muscle carefully under direct vision, in the anterior portion of the muscle, with the aid of intraoperative neuromonitoring, and using pins holding the muscle away from the surgical corridor during disc preparation and cage insertion are keys to avoiding nerve damage. 3) During the lateral disc preparation portion of the procedure, performing not only an ipsilateral annulotomy to enter the disc space, but also a contralateral annulotomy to further release the anterior column is important to maximize the amount of lordosis and correction of scoliosis at each level.
As mentioned in the protocol, this technique can be modified to insert multiple interbody cages through a single incision. Doing so often involves separate retractor positions in the lateral approach as described in the protocol. To limit any inaccuracies in the intraoperative navigation that are caused by the insertion of interbody spacers, we recommend that surgeons place the pedicle screws immediately after obtaining the registration CT scan.
Obtaining an optimal lateral trajectory in the prone position requires several adjustments. First, the incision may be too close to where the patient's body meets the operating room table, specifically around where the supporting hip pad typically sits. This can be avoided by translating the hip pads caudally slightly upon initial positioning. Second, the natural tendency for the surgeon is to operate in a downward trajectory, and sometimes it is difficult to have an accurate perception of an operative trajectory that is parallel to the ground. This can be alleviated with the use of a sitting stool, rolling the patient ("airplaning") away from the surgeon, raising the table height, and most importantly, using intra-operative stereotactic navigation for the optimal surgical trajectory.
As with all lateral approaches, the cranial and caudal limits of this technique are bounded by the ribcage and iliac crest, respectively. Therefore, L5-S1 will not be feasible for this approach. This approach will not be easy for certain patients with potential L4-5-accessing trajectory blocked by the top of the iliac crest. Careful examination of the preoperative AP X-ray is important in determining the feasibility of this surgical approach for the L4-5 level.
Several factors limit the comparison between Pro-LLIF and other established methods of lateral interbody fusion. First, no significant differences in operative timing or outcomes were identified in this study. It is likely that a ten-patient cohort is underpowered for comparative statistics; repeating the presented analyses on an expanded cohort will ameliorate this issue. Another potential confound is the learning curve associated with optimizing, training in, and teaching the new Pro-LLIF procedure. These are the very first 10 Pro-LLIF cases performed in this institute, and surgical nuances are being worked up and optimized over time. For example, we have modified the psoas retraction technique compared to the regular minimally invasive lateral access method.
We added the direct psoas muscle dissection and distraction pin placement above and below the operated disc under direct vision to create the surgical corridor rather than inserting the expandable tube into the psoas muscle. This allows surgeons to be more confident that the lumbar plexus is not being compressed by the expandable tube, and to avoid the issues of "muscle creeping" that is frequently associated with using the expandable tubes. In addition, while all ten Pro-LLIF procedures were performed by the same neurosurgeon, the second operator, anesthesiologists, and surgical staff varied between cases. Increased team experience with Pro-LLIF will likely result in decreased operative time, lengths of stay, and postoperative complication rates. Despite these limitations, the data support the utility and efficacy of the Pro-LLIF approach for patients requiring lumbar interbody fusions from L2 to L5. The single-position, prone, lateral approach provides safe and simultaneous access for lateral interbody cage placement and direct posterior neural decompression and segmental fixation. Efficiency will improve with increased experience with this promising technique.
Divulgaciones
The authors have nothing to disclose.
Acknowledgements
We thank the dedicated work from our nurses and surgical technicians in making the advance of this technique a possibility.
Materials
| CONDUIT Lateral Lumbar Implants | DePuy Synthes | EIT Cellular Titanium Interbody | |
| COUGAR LS Lateral Spreaders | DePuy Synthes | Lateral Spreaders: 6, 8, 10, 12, 16 mm | |
| COUGAR LS Lateral Trials | DePuy Synthes | Parallel Trial, 18 x 6 mm | |
| COUGAR LS Lateral Trials | DePuy Synthes | Lordotic Trials, 18 x 8 mm 18 x 10 mm 18 x 12 mm 18 x 14 mm | |
| DePuy Synthes ATP/Lateral Discetomy Instruments | Avalign Technologies LLC | ||
| Dual Lead Awl Tip Taps 4.35 mm – 10 mm | DePuy Synthes | Navigation Enabled Instruments used with Medtronic StealthStation Navigation System | |
| EXPEDIUM 5.5 System | DePuy Synthes | with VIPER Cortical Fix Screws | |
| EXPEDIUM Driver Shaft T20 5.5 | DePuy Synthes | Navigation Enabled Instruments used with Medtronic StealthStation Navigation System | |
| EXPEDIUM Drive Sleeve 5.5 | DePuy Synthes | Navigation Enabled Instruments used with Medtronic StealthStation Navigation System | |
| Phantom XL3 Lateral Access System | TeDan Surgical Innovations, LLC | Lateral Access retractor (includes dilators and LED Lightsource) | |
| PIPELINE LS LATERAL Fixation Pins | DePuy Synthes | ||
| The R Project, R package version 4.0, MatchIt package | propensity-score matching | ||
| SENTIO MMG Lateral Probe | DePuy Synthes | Lateral Access Probe | |
| SENTIO MMG Stim Clip | DePuy Synthes | attaches to insilated dilators, conducting triggered EMG while rotating 360 degrees | |
| VIPER 2 1.45 mm Guidewire, Sharp | DePuy Synthes | ||
Referencias
- Ozgur, B. M., Aryan, H. E., Pimenta, L., Taylor, W. R. Extreme lateral interbody fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. The Spine Journal. 6 (4), 435-443 (2006).
- Kwon, B., Kim, D. H. Lateral lumbar interbody fusion: indications, outcomes, and complications. Journal of the American Academy of Orthopaedic Surgeons. 24 (2), 96-105 (2016).
- Rodgers, W. B., Gerber, E. J., Patterson, J. Intraoperative and early postoperative complications in extreme lateral interbody fusion: an analysis of 600 cases. Spine. 36 (1), 26-32 (2011).
- Pimenta, L., Turner, A. W. L., Dooley, Z. A., Parikh, R. D., Peterson, M. D. Biomechanics of lateral interbody spacers: going wider for going stiffer. The Scientific World Journal. 2012, 381814 (2012).
- Ploumis, A., et al. Biomechanical comparison of anterior lumbar interbody fusion and transforaminal lumbar interbody fusion. Journal of Spinal Disorders & Techniques. 21 (2), 120-125 (2008).
- Blizzard, D. J., Thomas, J. A. MIS single-position lateral and oblique lateral lumbar interbody fusion and bilateral pedicle screw fixation: feasibility and perioperative results. Spine. 43 (6), 440-446 (2018).
- Ouchida, J., et al. Simultaneous single-position lateral interbody fusion and percutaneous pedicle screw fixation using O-arm-based navigation reduces the occupancy time of the operating room. European Spine Journal. 29 (6), 1277-1286 (2020).
- Lamartina, C., Berjano, P. Prone single-position extreme lateral interbody fusion (Pro-XLIF): preliminary results. European Spine Journal. 29, 6-13 (2020).
- Quiceno, E., et al. Single position spinal surgery for the treatment of grade II spondylolisthesis: A technical note. Journal of Clinical Neuroscience. 65, 145-147 (2019).
- Buckland, A. J., et al. Single position circumferential fusion improves operative efficiency, reduces complications and length of stay compared with traditional circumferential fusion. The Spine Journal. , (2020).

