Transoral Robotic Total Thyroidectomy and Bilateral Central Regional Lymph Node Dissection for Papillary Thyroid Carcinoma
Summary
The transoral robotic total thyroidectomy and bilateral central regional lymph node dissection using three ports without axillary incision are feasible and safe for early-stage papillary thyroid carcinoma. Here we present the operative techniques of this operation.
Abstract
Currently, the common approaches to thyroid surgery include conventional thyroidectomy, bilateral axillo-breast, axillary, retroauricular, and oral vestibule approaches. Essentially, various approaches to thyroid surgery only move the traditional surgical incision to a more concealed position but still leave scars on the body surface. Among them, thyroid surgery via the oral vestibule approach can obtain the best cosmetic outcome through the shortest natural cavity. However, in the early time, thyroid surgery via the oral vestibule approach usually requires three incisions in the mouth and one axillary incision. We have introduced a robotic surgical system into thyroidectomy via the oral vestibule approach and successfully completed total thyroidectomy and bilateral central lymph node dissection. During the operation, only three incisions were made at the oral vestibule without an axillary incision. This article aims to present the unique three-port method of robotic thyroidectomy via oral vestibule for the treatment of patients with papillary thyroid cancer.
Introduction
Thyroid surgeons use different surgical approaches (bilateral axillary breast approach1 [Figure 1], axillary approach2 [Figure 2], retroauricular approach3 [Figure 3], etc.) to conceal surgical incisions and achieve scarless thyroid surgery in the neck. However, none of these technologies can completely avoid scars on the patient's skin surface. In all methods, only the oral vestibule approach (Figure 4) can achieve the shortest distance of flap separation, leaving no scar on the whole body surface4,5,6. In recent years, natural mouth endoscopic surgery (NOTES)7has been introduced in oral thyroid surgery.
Thyroid surgery performed through this method can be completed through an endoscope or robotic surgical system. Compared with the endoscopic surgery system for thyroid surgery, this robot system has an enlarged three-dimensional high-definition field of view and a rotatable mechanical wrist capable of intuitive motion, making surgeons more flexible in performing satisfactory surgeries8,9. The benefits of this innovative technology include minimally invasive dissection and channels for both thyroid glands10,11,12. However, oral thyroidectomy often requires an axillary-assisted incision to complete the surgery. To achieve the ultimate cosmetic effect, our surgical team delves into the feasibility of an oral three-port robotic thyroidectomy without an axillary incision for the treatment of early papillary thyroid cancer.
This article introduces the application of a robotic surgical system to complete oral thyroidectomy and bilateral central lymph node dissection. Furthermore, the feasibility and safety of this approach have been demonstrated by successfully completing a three-port robotic thyroidectomy without axillary incision and central regional lymph node dissection.
Protocol
This study follows the guidelines of the Army Medical University's Human Research Ethics Committee. All patients mentioned in the study signed informed consent forms.
1. Preoperative preparation
- After successful nasotracheal intubation, place the patient supine with the head and neck into hyperextension.
- Let the eyes close naturally. Apply eye ointment and cover the area from the top of the brow bone to the nasal flanks with an appropriate eye patch or surgical patch to prevent disinfectant, blood, and other fluids from flowing into the eyes.
- Fill both external ear canals with cotton balls to prevent disinfectant and blood from entering the ear canals and cover the face with a cotton pad folded in half lest the face be crushed by the tracheal intubation.
- Cover the surface of the cotton pad with a non-woven surgical cap up to the nostrils. Apply surgical lamination externally, down to the level of the upper lip, while leaving the area at the foot of the horizontal line of the corners of the mouth uncovered, the lateral sides of the lamination reaching the edge of the sideburns while its upper side flush with the hairline.
- Use a robot surgical system. Place the patient in the supine position. Administer general anesthesia via nasotracheal intubation as per the anesthetist's recommendations.
2. Surgical procedure
- Inject Lidocaine (10 mL) + Ropivacaine (10 mL) + Adrenaline hydrochloride (10 drops) under the oral mucosa.
- Make an incision of approximately 8 mm above the lower lip ligament. Ensure that the incisions on both sides are approximately 8 mm long, between the sharp teeth and the first molar (Figure 5).
- Maintain the CO2 gas pressure at 6 mmHg and the gas flow rate in the 20 mL/min range.
- Dock the robot arm.
- Place Maryland bipolar coagulator into the left trocar, and ultrasonic scalpel into the right trocar, completing the flap freeing.
- Using an ultrasonic scalpel, separate the flap downward to the clavicle and bilaterally to the anterior border of the Sternocleidomastoid muscle.
- Use unipolar curved scissors to separate the white cervical line and part of the banded muscle to expose a portion of the thyroid gland (Figure 6) and use a 25 G syringe to inject approximately 0.1 mL of carbon nanoparticle suspension injection from the neck to the thyroid parenchyma under surgical observation to complete a negative image to illustrate the parathyroid gland (Figure 7).
- Use an ultrasound knife to release the striated muscle and use 4-0 absorbable sutures to suspend the striated muscle sutures, facilitating surgical visualization.
- Inject 1 mL of 2.5 mg/mL indocyanine green intravenously for better visualization and protection of the parathyroid glands. Switch to automatic fluorescence imaging mode for clear visualization of fluorescent parathyroid glands and comparison with non-fluorescent lymph nodes.
- Use an ultrasound knife to disconnect the blood vessels at the upper pole of the thyroid gland while searching for and protecting the parathyroid gland at the upper pole (Figure 8). Use curved bipolar forceps to complete the delicate operation of in situ parathyroid preservation (Figure 9).
- Reveal the laryngeal entry of the recurrent laryngeal nerve (Figure 10). Usually, the recurrent laryngeal nerve can be found more quickly within the triangular area formed by the medial parathyroid gland, thyroid gland, and laryngeal muscles. This area is rich in blood supply. Deal with bleeding and exudate at the entry larynx promptly to secure a straight field of view operation and reduce the difficulty of robotic thyroid surgery.
- Use the smoke evacuation device (mastoid suction device12; Figure 11) to remove the exudate and blood during the mass resection, maintaining the cleanness of the lens and the definition of the image of the local surgical area, ensuring accurate exposure and protection of recurrent laryngeal nerve during the surgery. Then, conduct the prophylactic unilateral central neck dissection.
- Perform a contralateral hemithyroidectomy with ipsilateral central lymph node prophylactic dissection in the same manner.
- Place all excised tissues in a specimen bag and remove them. Rinse the wound with saline.
- Place a negative pressure drainage tube into the thyroid bed through the cervical puncture hole. Use 4-0 absorbable barbed sutures to continuously suture the strap muscles. Use absorbable threads for the suturing of the oral incisions.
Representative Results
The average operative time was ~253 min (minimum time: 205 min, maximum time: 300 min), with an average blood loss of ~20 mL (minimum blood loss: 10 mL, maximum blood loss: 50 mL). The drain was removed until the drainage fell to less than 30 mL/day, and the patients were discharged 2-3 days postoperatively. Figure 12 shows the follow-up images of the 4 patients 1-month post-surgery. The images show that there are no surgical scars on the body of the patients. The clinical data of 4 patients are shown in Table 1.
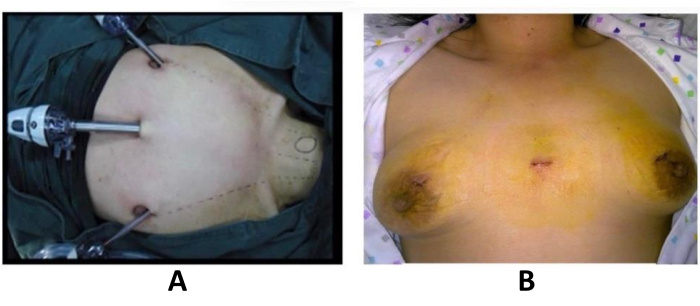
Figure 1: Bilateral axillo-breast approach. (A) Intraoperative image (B) Postoperative image. Please click here to view a larger version of this figure.

Figure 2: Transaxillary approach. Postoperative image. Please click here to view a larger version of this figure.

Figure 3: Retroauricular approach. (A) Intraoperative image. (B) Postoperative image Please click here to view a larger version of this figure.
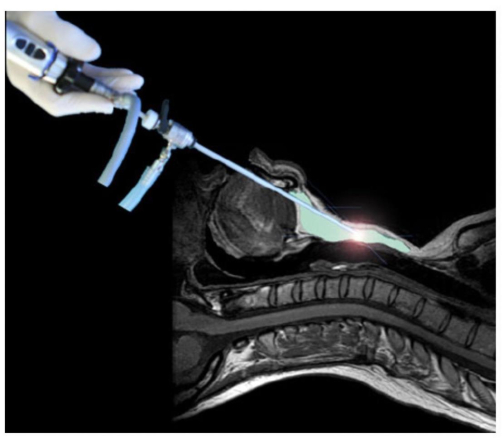
Figure 4: Schematic diagram of the oral vestibular approach hierarchy. Please click here to view a larger version of this figure.

Figure 5: Placement of trocars. Three 8 mm trocars are placed in the position of the oral vestibule. Please click here to view a larger version of this figure.
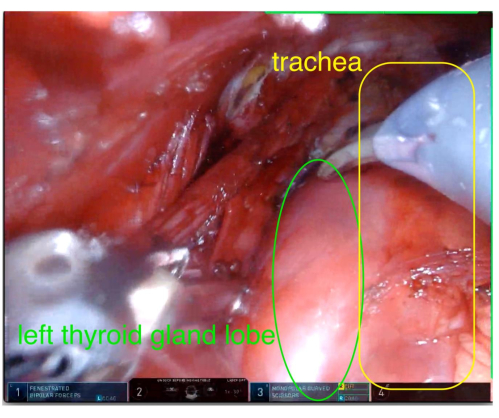
Figure 6: Exposing the left thyroid gland lobe. Separate the muscles to expose the left thyroid gland lobe. Please click here to view a larger version of this figure.
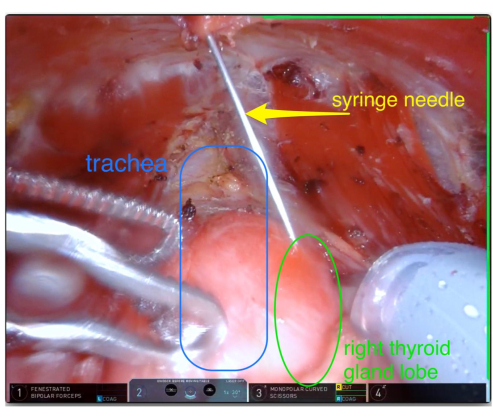
Figure 7: Carbon nanoparticle injection. Injecting carbon nanoparticle suspension into the right thyroid gland lobe to complete a negative image illustrating the parathyroid gland. Please click here to view a larger version of this figure.
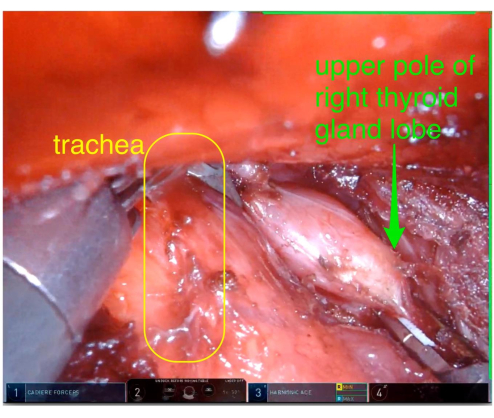
Figure 8: Dissecting the right thyroid gland lobe. Dissecting the upper pole of the right thyroid gland lobe using an ultrasound knife. Please click here to view a larger version of this figure.
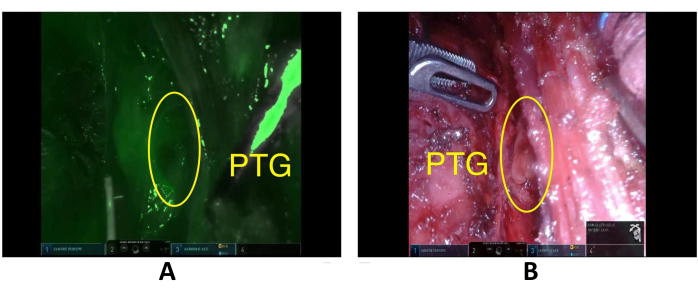
Figure 9: Preserved parathyroid gland. A preserved parathyroid gland seen in situ (the left side is a view in fluorescence mode, with significant interference from surrounding tissues and poor contrast) during the surgical procedure. Please click here to view a larger version of this figure.
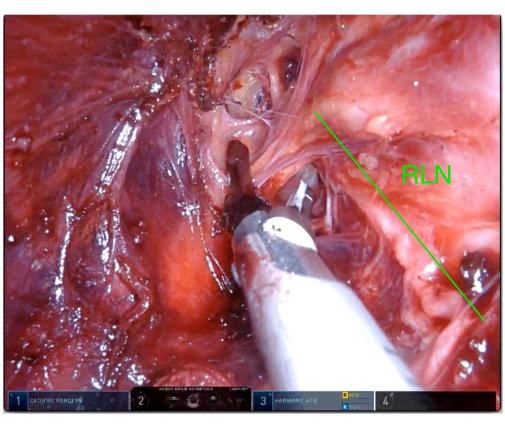
Figure 10: Tissue removal. Separating and cutting off the tissue outside the left recurrent laryngeal nerve using an ultrasonic scalpel. Please click here to view a larger version of this figure.
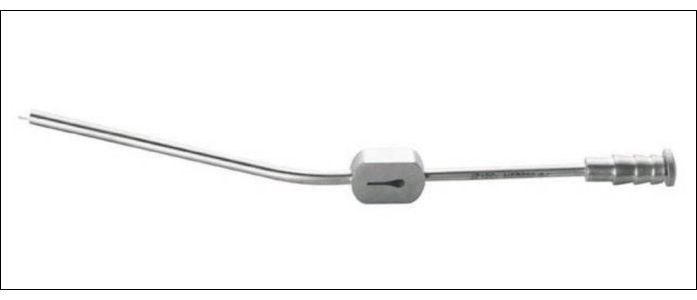
Figure 11: Smoke exhaust device. The smoke exhaust device (mastoid aspirator) used for removing the exudate and blood during the surgery. Please click here to view a larger version of this figure.
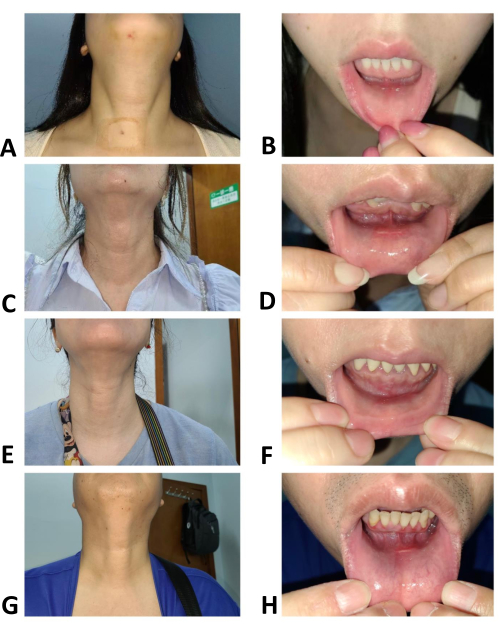
Figure 12: Follow-up photos of the 4 patients showing no scars on the body surface. (A) Patient 1's neck appearance at 1 month after surgery. (B) Patient 1's oral vestibular incision at 1 month after surgery. (C) Patient 2's neck appearance 1 month after surgery. (D) Patient 2's oral vestibular incision at 1 month after surgery. (E) Patient 3's neck appearance at 1 month after surgery. (F) Patient 4's oral vestibular incision at 1 month after surgery. (G) Patient 4's neck appearance at 1 month after surgery. (H) Patient 4's oral vestibular incision 1 month after surgery. Please click here to view a larger version of this figure.
Table 1: Clinical data of 4 patients. The clinical details of the 4 patients who underwent surgery are listed in the table. Please click here to download this Table.
Discussion
Some scholars have reported transoral robotic thyroid surgery. In Kim’s series of TORT studies, the authors used four robotic arms on’s automated platforms to perform the TORT procedure. A fourth arm was used via a transaxillary incision primarily for traction of the strap muscles, and this access was also used to extract specimens and place drains when needed13,14.
In this three-port robot approach, one transverse incision of about 8 mm is located above the lower lip ligament, and a longitudinal incision about 8 mm long on both sides is located between the canine and the first molar. After the establishment of the gas space, the white line of the neck is separated, exposing part of the thyroid gland. Then the injection of nano carbon suspension is utilized for staining and negative development of the thyroid gland. The suture is then used to suspend the shoulder belt muscle to help reveal the thyroid surgery area. Compared with unilateral thyroidectomy, total thyroidectomy has more than doubled the risk of recurrent laryngeal nerve injury. Therefore, it is particularly important to locate, separate and protect the recurrent laryngeal nerve. Usually, the recurrent laryngeal nerve can be found more quickly within the triangular area formed by the medial parathyroid gland, thyroid gland, and laryngeal muscles. In the process of operation in this area, the key step to protect the recurrent laryngeal nerve is to timely deal with the bleeding in the operation field and the smoke generated by the energy equipment. The use of a smoke evacuation device (mastoid suction device) can suck up exudate and blood around the gauze for mass resection, maintaining the cleanness of the lens and the definition of the image of the local surgical area, ensuring the accurate exposure and protection of recurrent laryngeal nerve during the surgery. After the operation, the specimen can be cut into the bag through the central vestibular incision. In this technique, the oral vestibular incision, about 8 mm long, can be slightly expanded when taking out the specimen. Generally speaking, T1 tumors can be successfully removed. However, no further attempt has been made at tumors greater than or equal to T215,16. It may be easier to remove them through the axillary incision. In addition, if the patient’s chin has been injured and scar tissue exists, it will be relatively difficult to take out the specimen. In addition, if necessary, a small drainage tube can be placed to poke out from the skin in front of the neck without leaving obvious scars on the skin.
Through the above technical improvements, the axillary robotic arm becomes unnecessary. In this way, transoral robotic thyroidectomy can completely avoid leaving no scars on the body surface, reducing unnecessary damage and enhancing the surgical safety and treatment effect. In the future, this technology could be applied to patients who need lateral cervical lymph node dissection so as to benefit more patients. However, the specific indications and contraindications still need to be explored.
In conclusion, the three-port transoral robotic thyroidectomy is safe and feasible in carefully selected patients. In the future, this technology can be used for T1 early thyroid cancer patients with a phobia about the defect of physiognomy.
Divulgaciones
The authors have nothing to disclose.
Acknowledgements
Supported by the General project of technology innovation and application development of Chongqing (Grant No. CSTC2019jscx-msxmX0196).
Materials
| 4-0 absorbable sutures | Covidien | VLOCM0023 | Suture the linea alba cervicalis |
| 5-0 Polyglactin braided absorbable suture | Johnson & Johnson | VCP433H | Oral mucosa suture |
| 8 mm Cadiere forceps | Intuitive Surgical, Inc | LOT N10210823 | Clamp tissue |
| 8 mm Harmonic ACE scalpel | Intuitive Surgical, Inc | REF 480275 | Coagulation, expand operating space |
| 8 mm Maryland bipolar forceps | Intuitive Surgical, Inc | LOT K10210830 REF 470172 | Expose the recurrent laryngeal nerve |
| 8 mm Monopolar curved scissors | Intuitive Surgical, Inc | LOT K10211108 REF 470179 | Fine capsular anatomy |
| Carbon Nanoparticles Suspension Injection | Chongqing Laimei Pharmaceutical Co., Ltd | N/A | 1 mL/50 mg; used for tracing regional drainage lymph nodes. |
| Da Vinci Xi Surgical System | Intuitive Surgical, Inc | Xi | Surgical system |
| Endoscopy surgical specimen setrieval bag | Hangzhou Kangji Medical Equipment Co.Ltd. | LOT 22021921 REF 104Y.111 | Remove specimens from air cavity |
| Medical pressure garment | Foshan qiaoke bio technology Co.Ltd. | 20200149 | Pressure dressing of the anterior neck area of the mandible |
Referencias
- Shimazu, K., et al. Endoscopic thyroid surgery through the axillo-bilateral-breast approach. Surgical Laparoscopy, Endoscopy & Percutaneous Techniques. 13 (3), 196-201 (2003).
- Ikeda, Y., Takami, H., Niimi, M., Kan, S., Sasaki, Y., Takayama, J. Endoscopic thyroidectomy by the axillary approach. Surgical Endoscopy. 15 (11), 1362-1364 (2001).
- Alabbas, H., Bu Ali, D., Kandil, E. Robotic retroauricular thyroid surgery. Gland Surgery. 5 (6), 603-606 (2016).
- Witzel, K., von Rahden, B. H. A., Kaminski, C., Stein, H. J. Transoral access for endoscopic thyroid resection. Surgical Endoscopy. 22 (8), 1871-1875 (2008).
- Benhidjeb, T., Wilhelm, T., Harlaar, J., Kleinrensink, G. -. J., Schneider, T. A. J., Stark, M. Natural orifice surgery on thyroid gland: totally transoral video-assisted thyroidectomy (TOVAT): report of first experimental results of a new surgical method. Surgical Endoscopy. 23 (5), 1119-1120 (2009).
- Wilhelm, T., Metzig, A. Video. Endoscopic minimally invasive thyroidectomy: first clinical experience. Surgical Endoscopy. 24 (7), 1757-1758 (2010).
- Park, J. O., Sun, D. I. Transoral endoscopic thyroidectomy: our initial experience using a new endoscopic technique. Surgical Endoscopy. 31 (12), 5436-5443 (2017).
- Clark, J. H., Kim, H. Y., Richmon, J. D. Transoral robotic thyroid surgery. Gland Surgery. 4 (5), 429-434 (2015).
- Richmon, J. D., Pattani, K. M., Benhidjeb, T., Tufano, R. P. Transoral robotic-assisted thyroidectomy: a preclinical feasibility study in 2 cadavers. Head & Neck. 33 (3), 330-333 (2011).
- Wilhelm, T., Metzig, A. Endoscopic minimally invasive thyroidectomy (eMIT): a prospective proof-of-concept study in humans. World Journal of Surgery. 35 (3), 543-551 (2011).
- Nakajo, A., et al. Trans-oral video-assisted neck surgery (TOVANS). A new transoral technique of endoscopic thyroidectomy with gasless premandible approach. Surgical Endoscopy. 27 (4), 1105-1110 (2013).
- Anuwong, A. Transoral endoscopic thyroidectomy vestibular approach: a series of the first 60 human cases. World Journal of Surgery. 40 (3), 491-497 (2016).
- Kim, H. Y., et al. Transoral robotic thyroidectomy: lessons learned from an initial consecutive series of 24 patients. Surgical Endoscopy. 32 (2), 688-694 (2018).
- Kim, H. Y., Park, D., Bertelli, A. A. T. The pros and cons of additional axillary arm for transoral robotic thyroidectomy. World Journal of Otorhinolaryngology – Head and Neck Surgery. 6 (3), 161-164 (2020).
- Park, D., et al. Robotic versus endoscopic transoral thyroidectomy with vestibular approach: A literature review focusing on differential patient suitability. Current Surgery Reports. 10, 133-139 (2022).
- Park, D., et al. Institutional experience of 200 consecutive papillary thyroid carcinoma patients in transoral robotic thyroidectomy surgeries. Head & Neck. 42 (8), 2106-2114 (2020).

