Real-time Imaging of Myeloid Cells Dynamics in ApcMin/+ Intestinal Tumors by Spinning Disk Confocal Microscopy
Summary
By using transgenic reporter mice and injectable fluorescent labels, long-term intravital spinning disk confocal microscopy enables direct visualization of myeloid cell behavior into intestinal adenoma in the ApcMin/+ colorectal cancer model.
Abstract
Myeloid cells are the most abundant immune cells within tumors and have been shown to promote tumor progression. Modern intravital imaging techniques enable the observation of live cellular behavior inside the organ but can be challenging in some types of cancer due to organ and tumor accessibility such as intestine. Direct observation of intestinal tumors has not been previously reported. A surgical procedure described here allows direct observation of myeloid cell dynamics within the intestinal tumors in live mice by using transgenic fluorescent reporter mice and injectable tracers or antibodies. For this purpose, a four-color, multi-region, micro-lensed spinning disk confocal microscope that allows long-term continuous imaging with rapid image acquisition has been used. ApcMin/+ mice that develop multiple adenomas in the small intestine are crossed with c-fms-EGFP mice to visualize myeloid cells and with ACTB-ECFP mice to visualize intestinal epithelial cells of the crypts. Procedures for labeling different tumor components, such as blood vessels and neutrophils, and the procedure for positioning the tumor for imaging through the serosal surface are also described. Time-lapse movies compiled from several hours of imaging allow the analysis of myeloid cell behavior in situ in the intestinal microenvironment.
Introduction
Overwhelming evidence now demonstrates that the tumor microenvironment, consisting of heterogeneous cell populations, including fibroblasts, endothelial cells, immune and inflammatory cells, extracellular matrix, and soluble factors, plays a crucial role in the initiation and progression of solid tumors by contributing to almost all hallmarks of cancer1. Indeed, during tumor progression, there are constant dynamic interactions between transformed cancer cells and stromal cells that evolve to generate a microenvironment favorable to malignancy2. Among the immune cells that infiltrate the tumor microenvironment, myeloid cells are the most abundant3. Consisting of tumor-associated macrophages (TAM), myeloid-derived suppressor cells (MDSCs), dendritic cells (DC) and neutrophils (PMNs), myeloid cells are recruited from bone marrow and progressively infiltrate tumors, releasing cytokines, growth factors and proteases which can promote tumor growth and spread4. The crosstalk between cancer cells and myeloid cells is complex but dynamic. Thus the understanding of the nature of their interactions is crucial for determining why these cells promote cancer progression instead of participating in an anti-tumor immune response, and may help to find new targets to control it.
Direct observation by intravital microscopy provides information on cell dynamics within the tissues of live mice5. A four-color, multi-region, micro-lensed spinning disk confocal system was designed to study stromal cells within mammary tumors6. This approach enables long-term continuous imaging and includes several advantages such as (a) rapid images acquisition to minimize motion artifacts, (b) long-term anesthesia, (c) four color acquisition to follow different cell types, (d) fluorescent labeling of different tumoral components, and (e) observation of different tumor microenvironments within the same mouse to avoid mouse to mouse variability7-9. With this technology, different cell behaviors have been reported in the mammary tumor virus (MMTV) promoter-driven polyoma middle T oncogene (PyMT) model that displays progressive stages of tumorigenesis. Regulatory T-lymphocytes (Tregs, visualized by the Foxp3EGFP transgene) migrate preferentially in proximity to blood vessels whereas DCs (CD11c-DTR-EGFP), carcinoma-associated fibroblasts (Fsp1+/+-EGFP) and myeloid cells (c-fms-EGFP) exhibit higher motility at the tumor periphery than within the tumor mass. In the condition of acute systemic hypoxia, cells migrated differently: Tregs stop migrating in contrast to myeloid cells that continue to move6. In addition, in the same mouse model, it has been shown that doxorubicin sensitivity changes with tumor stage, drug distribution is related to drug response, and doxorubicin treatment leads to CCR2-dependent recruitment of myeloid cells to tumors. Thus, live imaging can also be used to gain insights into drug responses in situ and the biology of chemoresistance10,11.
Adenomatous polyposis coli (Apc) gene mutations commonly occur in human colorectal adenomas and carcinomas12 and mutation of a single copy of the Apc gene results in familial adenomatous polyposis (FAP), which confers an extremely high risk for colon cancer13. The mouse strain ApcMin/+ carries a truncation mutation at codon 850 of the Apc gene and spontaneously develops multiple intestinal adenomas all over the small intestine14-16. Long-term intravital imaging of the intestine is challenging because of the invasiveness of the procedure, since opening the peritoneal cavity is necessary for access to the intestine. Short-term live imaging studies have been previously published on healthy intestine17,18, but long-term direct observation of intestinal tumors has not been reported. A surgical procedure has been designed and refined to visualize tumors through the serosal surface of the intestine, using the intravital spinning disk microscopy system previously used to image breast tumors6,10. In this paper, a protocol is described that allows one to follow the behavior of myeloid cells within the tumors in the small intestine by using ApcMin/+ mice.
Protocol
NOTE: All animal experiments were conducted in accordance with procedures approved by the Institutional Animal Care and Use Committee (IACUC), UCSF. All the imaging experiments were non-survival procedures and the animals were euthanized immediately following the end of image acquisition.
1. Generation of Mice
NOTE: ApcMin/+ mice, carrying a mutation on the Apc gene, spontaneously develop 50-100 adenomas in the small intestine.
- Cross ApcMin/+ mice with the ACTB-ECFP line, which expresses ECFP under the actin promoter, and further with the c-fms-EGFP line, which expresses EGFP under the c-fms promoter to detect the myeloid cells. Heterozygous animals for ACTB-ECFP and c-fms-EGFP are used to detect fluorescence.
- Use mice at 3-4 months of age to image clearly detectable adenomas.
2. Preparation of Materials Before Surgery
NOTE: The details of the microscope set-up have been previously described6,7.
- Microscope
- Turn on the heating blanket. Turn on the argon laser for 488 nm excitation and the solid-state 405 nm, 561 nm, and 640 nm lasers. Turn on the microscope, the spinning disk control unit, the AOTF, the laser control unit, and the camera controller.
- Open the microscope shutter, which turns the LED red. Turn on the computer and camera software.
- Imaging Platform
- Ensure that the stage insert is clean. Otherwise, clean with soap and water and then dry.
- Take two coverslips and use lab tape to secure them on the insert. Place the insert on the stage and clean it with alcohol wipes.
- Using lab tape, attach the heating blanket to the right side of the stage.
- Verify the integrity of the rubber diaphragm on the nose cone and change it if necessary. Position and fix the nose cone for isoflurane anesthesia delivery to the animal by using gauze and lab tape.
- Isoflurane Anesthesia System
- Refill the isoflurane tank.
- Turn on the vacuum and adjust to 1.2 L/min.
- Add distilled water to the nebulizer and connect the nebulizer to the isoflurane system.
- Turn on the oxygen analyzer and connect it to the isoflurane system. Turn on the oxygen tank and ensure that the oxygen analyzer shows 100%. Adjust the O2 flow to 0.2 L/min.
- Turn on the nitrogen tank and adjust the flow at 0.8 L/min. Ensure that the oxygen analyzer shows 21%.
- Preparation of Surgery Tools and Platform
- Clean 2 pairs of dissection forceps and scissors with soap and water.
- Turn on the hot bead sterilizer and let it reach 250 °C. Sterilize the surgery tools for 30 sec. Let them cool off.
- Place a lab soaker on the surgery bench.
- Use a Styrofoam lid as a surgical platform. Cover with a piece of lab soaker. Prepare a second piece of lab soaker to change after shaving the mouse.
- Place the nose cone with the line of anesthesia on the covered Styrofoam lid, and attach it to the Styrofoam lid (not on the lab soaker) with some tape and use two needles on both sides of the nose cone to keep it in place.
- Assemble betadine, alcohol wipes, sterile gauze, super glue, microscope slides, electric shaver, and 4 pieces of lab tape.
3. Preparation of Injections
- Under the hood, prepare an insulin syringe (28 G x ½ in) with 7 µl of stock AF647-conjugated Ly-6G (Gr1) antibody (1 mg/ml) into 100 µl of 2,000 kDa rhodamine-dextran (4 mg/ml) for retro-orbital injection. Retro-orbital injection is recommended in ApcMin/+ mice since anemia that develops in these animals makes the tail veins difficult to detect through the skin.
- Prepare a second insulin syringe with 1 mg/kg atropine diluted into 150 µl PBS for subcutaneous (s.c.) injection before imaging to dampen peristaltic movements of the intestine.
4. Preparation of the Intestine for Imaging
- Verify that the anesthesia line to the induction chamber is open, and the lines to the surgical table and microscope are closed.
- Transfer the animal to the anesthesia chamber. Close the anesthesia chamber and turn on the isoflurane to 4% (with 21% O2).
- When the mouse breathes deeply and slowly (after 5-6 min), transfer it to the surgical stage on its flank and inject the Gr1 antibody solution and/or dextran solution retro-orbitally.
- Open the anesthesia line linked to the surgical platform. Close the line to the anesthesia chamber and put the mouse on its back with its nose in the anesthesia cone.
- Reduce the isoflurane concentration from 4% to 2.5%.
- Verify that the mouse is well anesthetized by pinching its footpad and testing the corneal reflex.
- Add ophthalmic lubricating ointment on eyes to prevent dryness while under anesthesia.
- Secure the limbs of the mouse to the surgical stage by adding lab tape.
- Remove the hair from the ventral surface by using an electric shaver. Also remove the hair from the left hind limb to position the oximeter before acquisition. Remove the lab soaker from the surgical stage and replace with a clean one to avoid hair contamination.
- Disinfect the ventral surface with alcohol wipes and betadine.
- Inject the atropine solution (from 3.2) s.c. in one flank of the mouse.
- Make a 1 cm ventral midline incision through the skin and the peritoneum by using scissors and one pair of forceps. Carefully pull out 3-4 cm of intestine and identify one or several tumors to image.
- Take a glass microscope slide and position a loop of the intestine on it with a tumor at the top.
- Add some super glue to a few locations along the intestine to attach it to the slide. Wait one min for the glue to dry. Use a marker to draw a line on the slide pointing to the tumor in order to facilitate its localization with the confocal.
5. Positioning the Mouse on the Stage and Preparation for Image Acquisition
- Remove lab tape from the limbs.
- Open the anesthesia line to the microscope stage and close the one to the surgical platform.
- Transfer the mouse carefully to the microscope stage with its ventral side down and its nose in the nose cone. Secure the anesthesia line with some lab tape.
- Re-position the mouse and/or the slide in order to have the intestine in the center of one of the cover-slipped windows. Gently tape down the slide with lab tape.
- Attach the oximeter probe to the left limb of the mouse to follow its heart and respiratory rate and arterial oxygen saturation levels.
- Cover the mouse with the heating blanket to avoid hypothermia.
- Decrease the isoflurane concentration from 2.5% to 1-1.5% for imaging.
6. Acquisition of Images by Using µManager Software
- Increase CSUX speed to 2,500 rpm to improve the image quality in the Configuration Settings.
- Use the Objective dropdown menu to choose 10X 0.5 NA or 20X 0.75 NA Fluar lens objective.
- Choose the laser 405 nm from Color dropdown menu.
- Click on Live and adjust the focus with the microscope.
- Click on Auto to automatically adjust maximum and minimum pixel intensities of the display image based on the extreme pixel values in the image. A histogram of display image's pixel intensities is presented in the graph in the lower part of the Main Window.
- Adjust the camera exposure in the Piper Control Panel window by changing the number of clocks (One clock is 33.333 msec).
- If the signal is too bright with the lowest exposure, decrease laser intensity using the microscope control unit.
- Check the signal intensity for 488 nm, 561 nm and 640 nm laser lines. Adjust laser intensity with the laser’s own control unit (488 nm and 561 nm) or the microscope control unit.
- In the Multi D Acquisition window, check the Time points box and type in number of time points and desired time interval.
- Check the Z-stacks box, choose “relative Z” and define Z-start and Z-end relative to the current position.
NOTE: For 10X or 20X objective, start with 3 Z planes, 8 µm or 4 µm apart respectively. - Check the Multiple positions (XY) box for imaging several locations, then click Edit position list, mark 4 to 6 different positions.
- Check the Channels box and add channels from New and select lasers lines from the dropdown menu and type in exposure for each channel (in multiples of 33.333 msec).
- Check Save images in the “Multi D acquisition” window.
- Select a folder and all the images acquired will be automatically saved in this folder with the name prefix given.
NOTE: Each continuous acquisition will be saved in a separate subfolder as individual tiff files for each Z slice in each color at each time point. - Save all the settings by clicking Save settings in the Multi D Acquisition window.
- Click Acquire in the Multi-dimensional Acquisition window to start acquisition.
- If the oximeter probe is not used or stops working well (when pulse is not stable or hard to detect), check the efficiency of anesthesia every 15 min during the imaging procedure by pinching the footpad and checking the corneal reflex. Adjust the anesthesia if the mouse is responsive to these stimuli.
- After acquisition, euthanize the mouse by increasing the isoflurane concentration to 5%. When no breathing movements are detectable, remove the mouse from the stage and perform a cervical dislocation.
7. Analysis of Images by Using Imaris Software
- Conversion to .ims Files (Supplementary Figure 1A)
- Open the camera software, click on File then Batch Converter.
- Click on Add files and choose the first file of the first position. Repeat for each position.
- For each file uploaded, click on Settings and verify that the settings “t” for Time, “c” for Channels and “z” for Z-stacks appear in that order.
- Save in the desired folder. Browse and create a new file as converted.
- Click on Set for all and Start.
- Adjustments (Supplementary Figure 1B)
- Go into the specific Converted folder and open the first file.
- In Display Adjustment window, adjust the background signal cutoff by modifying the Min number for each channel if necessary.
- If necessary, adjust the signal intensity by modifying the Max number (the lower the Max number, the higher the intensity of the signal).
NOTE: Adjustments of the signal intensity/contrast enable the highlight of a cell behavior or a compartment in order to have a nicer visualization. It does not change the result itself. - Click on Edit and Image Properties.
- Change the x, y, and z values (for a 10X objective, x and y = 0.712, z = 8 µm; for a 20X objective : x and y = 0.36, z = 4 µm).
- Click on All Equidistant to adjust time points. Add the start date and start time of the acquisition. Add the end date and end time of the acquisition (Supplementary Figure 1C).
- Click on Play button to watch the movie.
- Click Edit and Delete time points to delete blurry images.
- To join two separate acquisitions together into one movie, go to the last time point of the first movie and click on Edit > Add time points to add the second file.
- Saving as a movie (Supplementary Figure 1D)
- Click on Record, choose the .mov extension and a compression factor of 0.
- Click on Save.
Representative Results
By using spinning disk confocal microscopy, non-tumoral and tumoral tissues in the small intestine of ApcMin/+;ACTB-ECFP;c-fms-ECFP mice can be visualized from the serosal surface. After imaging, camera software is used to analyze and adjust the acquisition (Supplementary Figure 1). After intravenous (i.v.) injection of fluorescent 2,000 kDa dextran-rhodamine and a Ly-6G 647 conjugated antibody, blood vessels and PMNs can be detected respectively (Figure 1). Peyer’s patches that are aggregations of lymphoid tissue and full of myeloid cells can be seen easily (Figure 1A). The crypts of the small intestine are surrounded by blood vessels and myeloid cells (Figure 1A and 1B). Tumoral tissue is often more vascularized and more infiltrated by myeloid cells, and the structure of the crypts is less well organized (Figure 1A and 1B) depending on the size of the tumor. Acquisition can be done by using a 10X 0.5 NA (Figure 1A) and 20X 0.75 NA Fluar lenses (Figure 1B) but we obtained the best performance with the 10X 0.5 NA Fluar lens which was bright, allow the acquisition of a large region (676 x 676 µm) and could provide images from up to 70 µm into the tissue. The smooth muscle layer expressing actin-ECFP can sometimes render the focus on the intestinal epithelium difficult (Figure 1B, right panel). Myeloid cells dynamics in tumors can be followed in real time for a few hours as shown in the Animated/Video Figure 2. Whereas neutrophils (Gr1+ cells) circulate in blood vessels and patrol the tissues, other myeloid cells, mostly macrophages, surround the crypts and are less motile (Animated/Video Figure 2).
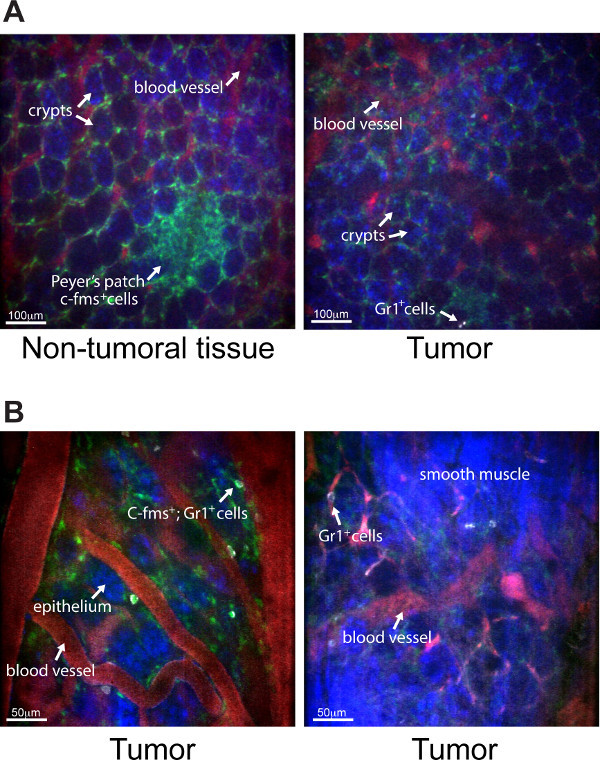
Figure 1. Representative pictures obtained with the spinning disk confocal of non-tumoral and tumoral tissue from ApcMin/+ mice. (A) Four-color pictures (10X Fluar, 0.5 NA lens) of the small intestine epithelium from the serosal surface of ApcMin/+;ACTB-ECFP;cfms-EGFP mouse that received i.v. fluorescent 2,000 kDa dextran-rhodamine (red) and a Ly-6G 647 conjugated antibody (white). The left panel shows the non-tumoral epithelium and the right panel shows a tumor from the same ApcMin/+;ACTB-ECFP;cfms-EGFP mouse. Myeloid cells are green and epithelial cells are blue. A cluster of c-fms+ cells is seen in the non-tumoral intestinal tissue in a Peyer’s patch (white arrow), scale bar = 100 µm. (B) Four-color pictures (20X Fluar, 0.5 NA lens) of the small intestine epithelium from the serosal surface of a ApcMin/+;ACTB-ECFP;cfms-EGFP tumor. In the left panel, several double-positive Gr1+ c-fms+ cells are detected in the tumoral tissue. The right panel shows a picture of the smooth muscle layer expressing actin-ECFP that can render the focus on the intestinal epithelium difficult, scale bar = 50 µm.
Animated/Video Figure 2. Myeloid cell dynamics in a 3 mm adenoma from an ApcMin/+ mouse. Four color time-lapse of the small intestine epithelium (10X Fluar, 0.5 NA lens) from the serosal surface of a ApcMin/+;ACTB-ECFP;cfms-EGFP mouse co-injected with fluorescent 2,000 kDa dextran-rhodamine (red) and a Ly-6G 647 conjugated antibody (white). Myeloid cells are green and epithelial cells are blue. Myeloid cells around the crypts are not moving. Some neutrophils (Gr1+ cells in white) are patrolling in the tissues. This is a 2 hr acquisition and the movie has been sped up 295 times.
Supplementary Figure 1. Screen shots of camera software for acquisition analysis. (A) First, the files need to be converted into .ims extension. (B) Then, display images can be adjusted, such as specific signals can be increased and background decreased. (C) Date and Time need to be adjusted in order to get a real-time movie. (D) The acquisition can be saved as a movie.
Discussion
In this paper, a detailed protocol is described for spinning disk confocal imaging of myeloid cell dynamics in intestinal tumors for several hours in a live animal, imaged from the serosal side of the gut.
To avoid inflammation and to have optimal physiologic conditions, imaging of the intestine has to be done on the intact organ. However, imaging from the serosal side of the intestine is challenging, since the light has to go through different tissue layers such as smooth muscle before reaching the epithelium. Focusing on the epithelium can be difficult in some areas, particularly in the actin-ECFP reporter mice since actin is highly expressed by smooth muscle cells. Although two-photon microscopy has the benefit of deeper tissue penetration as compared to confocal microscopes, we found that the spinning disk confocal microscope is powerful enough to obtain a good visualization of the intestinal epithelial structure. The advantages of spinning disk microscopy include the capacity for very rapid acquisition and unique sensitivity without sacrificing confocal resolution. These qualities allow the observation of dynamic processes even if some time points have to be deleted due to movement artifacts, minimize photodamage, and enable the imaging of relatively weakly fluorescent molecules.
Imaging intestine from the serosal side can also be challenging because of the endogenous peristaltic movements of this organ. In this protocol, a s.c. injection of atropine is given before imaging, and it efficiently decreases the movement. However, it is important to note that peristaltic movement is more extensive in the large intestine, but is not well inhibited by atropine treatment, rendering imaging quite difficult in this part of the gut. The smooth muscle layer in the colon is somewhat more prominent compared to the small intestine and appears to be more contractile. Therefore, it is almost impossible to focus on the epithelium in the actin-ECFP reporter mice. Moreover, in addition to these endogenous movements, organ drifting can occur, but in this case posterior drift correction can be performed by using the camera software.
Another major challenge in invasive imaging experiments is to keep the mouse alive and healthy as long as possible under anesthesia. The intestine is reached by opening the peritoneal cavity. Thus the procedure is more invasive than that used for mammary tumor imaging, which can be done for up to 40 hr because of the integrity of the peritoneum. The maximum acquisition done with the peritoneal cavity opened was 6 hr, but the mouse was still alive with no obvious signs of distress, so even longer acquisition may be feasible.
In this study myeloid cell behavior can be followed and analyzed within the intestinal tumor by using fluorescent reporter mice and also fluorochrome-conjugated tracers or antibodies. This approach can also be used for observing other cell types such as Tregs, dendritic cells or fibroblasts by using Foxp3-EGFP or CD11c-DTR-EGFP, or Fsp1-EGFP reporter mice respectively, as it has been used in the mammary tumor study6. Also, fluorescent antibodies against other cell populations than neutrophils can be injected i.v. In addition, cell behavior can also be analyzed in different conditions, such as hypoxia. Such experiments may give new insights into the behavior of those stroma cells after treatment with chemotherapy or targeted therapy. Finally, this protocol can be used in other mouse models of intestinal cancer and in different stages of tumor progression. ApcMin/+ mice develop intestinal adenomatous polyps only, which do not progress to malignancy because the mice have a shortened lifespan. It will be interesting to study the dynamic of myeloid cells in other intestinal cancer models with more aggressive and invasive tumors such as mice carrying mutations in K-ras19-21or Smad422 genes in addition to the Apc mutation.
Divulgaciones
The authors have nothing to disclose.
Acknowledgements
We would like to thank Ying Yu for ApcMin/+ mice genotyping. This study was supported by funds from INSERM and grants (CA057621 and AI053194) from the National Institutes of Health.
Materials
| Name of Material/ Equipment | Company | Catalog Number | Comments/Description |
| ApcMin/+ mice | Jackson Laboratory | 2020 | |
| ACTB-ECFP mice | Jackson Laboratory | 3773 | |
| cfms-EGFP mice | Jackson Laboratory | 18549 | |
| 2,000 kDa Dextran, rhodamine-conjugated | Invitrogen | D7139 | |
| Isoflurane | Butler Animal Health Supply | 29450 | |
| Nitrogen | UCSF | ||
| Oxygen | UCSF | ||
| 1X PBS | UCSF cell culture facility | ||
| Saline Buffer | UCSF cell culture facility | ||
| Anti-mouse Ly-6G (GR1) antibody AF647 | UCSF Monoclonal antibody core | Stock 1mg/ml. Use at 7ug/mouse | |
| Atropine | LARC UCSF | Use at 1mg/Kg mouse | |
| Alcohol wipes | Becton Dickinson | 326895 | |
| 28G1/2 insulin syringe | Becton Dickinson | 329465 | |
| Remium cover glass | Fisher Scientific | 12-548-5M | 24×50-1 |
| Superfrost plus microscope slides | Fisher Scientific | 12-550-15 | 25x75x1mm |
| Krazy glue | Office Max | 7111555 | |
| Betadine | LARC UCSF | ||
| Heat blanket | Gaymar Industries | ||
| Hot bead sterilizer | Fine Science Tools | 18000-45 | Turn ON 30min before use |
| Cotton tipped apllicators 6-inch | Electron Microscopy Sciences | 72310-10 | |
| Anesthesia system | Summit Anesthesia Support | ||
| Inverted microscope | Carl Zeiss Inc | Zeiss Axiovert 200M | |
| stage insert | Applied Sientific Instrumentation | ||
| Mouse Ox oximeter, software and sensors | Starr Life Sciences | MouseOx | |
| Nebulizer | Summit Anesthesia Support | ||
| Imaris | Bitplane | ||
| mManager | Vale lab, UCSF | Open-source software | |
| ICCD camera | Stanford Photonics | XR-Mega-10EX S-30 | |
| Spinning disk confocal sacan-head | Yokogawa Corporation | CSU-10b |
Referencias
- Hanahan, D., Weinberg, R. A. Hallmarks of cancer: the next generation. Cell. 144 (5), 646-674 (2011).
- Hanahan, D., Coussens, L. M. Accessories to the crime: functions of cells recruited to the tumor microenvironment. Cancer Cell. 21 (3), 309-322 (2012).
- Schouppe, E., De Baetselier, P., Van Ginderachter, J. A., Sarukhan, A. Instruction of myeloid cells by the tumor microenvironment: Open questions on the dynamics and plasticity of different tumor-associated myeloid cell populations. Oncoimmunology. 1 (7), 1135-1145 (2012).
- Egeblad, M., Nakasone, E. S., Werb, Z. Tumors as organs: complex tissues that interface with the entire organism. Dev Cell. 18 (6), 884-901 (2010).
- Lohela, M., Werb, Z. Intravital imaging of stromal cell dynamics in tumors. Curr Opin Genet Dev. 20 (1), 72-78 (2010).
- Egeblad, M., et al. Visualizing stromal cell dynamics in different tumor microenvironments by spinning disk confocal microscopy. Dis Model Mech. 1 (2-3), 155-167 (2008).
- Ewald, A. J., Werb, Z., Egeblad, M. Dynamic long-term in vivo imaging of tumor-stroma interactions in mouse models of breast cancer using spinning-disk confocal microscopy. Cold Spring Harb Protoc. 2011 (2), (2011).
- Ewald, A. J., Werb, Z., Egeblad, M. Monitoring of vital signs for long-term survival of mice under anesthesia. Cold Spring Harb Protoc. 2011 (2), (2011).
- Ewald, A. J., Werb, Z., Egeblad, M. Preparation of mice for long-term intravital imaging of the mammary gland. Cold Spring Harb Protoc. 2011 (2), (2011).
- Nakasone, E. S., Askautrud, H. A., Egeblad, M. Live imaging of drug responses in the tumor microenvironment in mouse models of breast cancer. J Vis Exp. (73), e50088 (2013).
- Nakasone, E. S., et al. Imaging tumor-stroma interactions during chemotherapy reveals contributions of the microenvironment to resistance. Cancer Cell. 21 (4), 488-503 (2012).
- Walther, A., et al. Genetic prognostic and predictive markers in colorectal cancer. Nat Rev Cancer. 9 (7), 489-499 (2009).
- Fearon, E. R. Molecular genetics of colorectal cancer. Annu Rev Pathol. 6, 479-507 (2011).
- Moser, A. R., Pitot, H. C., Dove, W. F. A dominant mutation that predisposes to multiple intestinal neoplasia in the mouse. Science. 247 (4940), 322-324 (1990).
- Su, L. K., et al. Multiple intestinal neoplasia caused by a mutation in the murine homolog of the APC gene. Science. 256 (5057), 668-670 (1992).
- Watson, A. J., et al. Epithelial barrier function in vivo is sustained despite gaps in epithelial layers. Gastroenterology. 129 (3), 902-912 (2005).
- McDole, J. R., et al. Goblet cells deliver luminal antigen to CD103+ dendritic cells in the small intestine. Nature. 483 (7389), 345-349 (2012).
- Xu, C., Shen, Y., Littman, D. R., Dustin, M. L., Velazquez, P. Visualization of mucosal homeostasis via single- and multiphoton intravital fluorescence microscopy. J Leukoc Biol. 92 (3), 413-419 (2012).
- Haigis, K. M., et al. Differential effects of oncogenic K-Ras and N-Ras on proliferation, differentiation and tumor progression in the colon. Nat Genet. 40 (5), 600-608 (2008).
- Sansom, O. J., et al. Loss of Apc allows phenotypic manifestation of the transforming properties of an endogenous K-ras oncogene in vivo. Proc Natl Acad Sci U S A. 103 (38), 14122-14127 (2006).
- Janssen, K. P., et al. APC and oncogenic KRAS are synergistic in enhancing Wnt signaling in intestinal tumor formation and progression. Gastroenterology. 131 (4), 1096-1109 (2006).
- Takaku, K., et al. Intestinal tumorigenesis in compound mutant mice of both Dpc4 (Smad4) and Apc genes. Cell. 92 (5), 645-656 (1998).

