Arterial Pouch Microsurgical Bifurcation Aneurysm Model in the Rabbit
Summary
Developing and testing endovascular devices for intracranial aneurysm treatment is still of great importance. Most aneurysm models used today miss either the important characteristics of an arterial degenerated wall or the hemodynamics of a true bifurcation. Therefore, we aimed to design a novel arterial pouch bifurcation model in rabbits.
Abstract
Endovascular treatment for intracranial aneurysms gained importance over the past decades, consequently there is an increased need of testing endovascular devices. Animal models respecting rheological, hemodynamic and aneurysm wall conditions are highly warranted. Therefore, the aim of the present study was to design a novel standardized and reproducible surgical technique to create autologous arterial pouch bifurcation aneurysms with non-modified and modified wall conditions in rabbits.
Bifurcation aneurysms were created by end-to-side anastomosis of the right on the left common carotid artery, both serving as parent arteries for the arterial pouch, which was microsurgically sewn on. Grafts were taken from the proximal right common carotid artery, either for the control (n = 7, immediate autologous re-implantation) or modified (n = 7, incubated with 100 international units elastase for 20 minutes before autologous re-implantation) group. Pouch and parent artery patency were controlled by fluorescence angiography immediately after creation. At follow-up (28 days), all rabbits underwent contrast enhanced magnetic resonance angiography and fluorescence angiography followed by aneurysm harvesting, macroscopic and histological evaluation.
A total of 16 female New Zealand White rabbits were operated upon. Two animals died prematurely. At follow-up, 85.72% of all aneurysms remained patent. Both groups revealed an increase in aneurysm size over time; this was more pronounced in the control group (6.48 ± 1.81 mm3 at time of creation vs. 19.85 ± 6.40 mm3 at follow-up, p = 0.037) than in the modified group (8.03 ± 1.08 mm3 at time of creation vs. 20.29 ± 6.16 mm3 at follow-up, p = 0.054).
Our findings demonstrate the adequacy of this new rabbit model which allows for the creation of bifurcation aneurysms with different wall conditions in a microsurgical approach. Given the excellent long-term patency and the property of aneurysm growth over time, this model may serve as an important tool for preclinical evaluation of novel endovascular therapies.
Introduction
Subarachnoid hemorrhage resulting from intracranial aneurysm (IA) rupture can effectively be controlled by either endovascular or microsurgical occlusion techniques1,2,3,4. Different endovascular therapies, to overcome the main limitation of IA recurrence after coiling, gained importance over the past decades generating an increased need of testing endovascular devices. To test these novel treatment approaches, appropriate animal models that respect rheological properties, hemodynamics and aneurysm wall conditions are highly warranted5,6,7. In this context, clinical as well as preclinical studies have already revealed the important role of aneurysm wall conditions regarding aneurysm rupture and recurrence after occlusion, especially focusing on the loss of mural cells7,8,9.
So far, experimental aneurysms in rabbits have most often been created either by elastase incubated common carotid artery (CCA) stumps or venous pouches sutured into an artificial CCA bifurcation.10,11,12,13,14,15,16 Thus, a true arterial pouch bifurcation model has never been described.
The aim of this study was to design a safe, fast, and standardized technique for microsurgical creation of bifurcation aneurysms with different wall conditions in a rabbit model (Figure 1). This was achieved by suturing non-modified and modified arterial pouches into an artificial created bifurcation of both CCAs.
Protocol
All veterinary care was performed in accordance with the institutional guidelines (all experiments were approved by the Local Committee for Animal Care of the Canton Bern, Switzerland (BE 108/16)) and conducted under supervision of a board-certified veterinarian anesthesiologist. The ARRIVE guidelines and the 3R principles were strictly followed17,18.
NOTE: House all animals at a room temperature of 22‒24 Celsius (°C) and maintain a 12 hours (h) light/dark cycle. Provide free access to water, pellet and ad libitum hay diet every time. Statistical analyses were performed using the non-parametric Wilcoxon-Mann-Whitney-U test. A probability value (p) of ≤ 0.05 was considered significant.
1. Presurgical phase
- Perform a detailed preoperative clinical examination of all rabbits planned for surgery immediately next to a quiet, aseptic operating room maintaining a temperature of 23 ± 3 °C.
- Record the weight of each animal, macroscopically evaluate the mucous membranes, capillary refill time and pulse quality.
- Further on perform cardiac auscultation with a stethoscope and abdominal palpation.
- Based on the clinical findings, attribute an American Society of Anesthesiologists (ASA) classification to each rabbit19. Include only animals with an ASA I score in the study.
- Shave both outer ears with an electric shaver and apply prilocaine-lidocaine cream on both auricular arteries and veins.
- Sedate the rabbit with a combination of 20 milligram (mg)/killogram (kg) of ketamine, 100 mg/kg of dexmedetomidine and 0.3 mg/kg of methadone injected subcutaneously (SC) via a syringe.
- Leave each animal undisturbed for at least 15 min.
- Thereafter, under supplementary oxygenation with 3 liter (l) /minute (min) through a loose face mask and steady monitoring through a pulse oximeter, place a 22 G cannula in the left auricular central artery and another 22 G cannula in the auricular vein of the contralateral ear.
- Shave the surgical field (neck) and inject 0.75% peri-incisional ropivacaine intradermally. Next shave the forehead and prepare to place pediatric electroencephalographic (EEG) sensors.
- Induce general anesthesia with propofol 1-2 mg/kg intravenously (IV) to effect. Then immediately intubate the trachea of all rabbits with a silicone tube (3 millimeter (mm) internal diameter) under capnographic control. Afterwards, transport all rabbits to the operating room, place them in dorsal recumbency and connect the tube to a pediatric circle system.
- Achieve anesthesia deepening and maintenance through isoflurane in oxygen, targeting a maximal end tidal isoflurane concentration of 1.3%.
- Ensure clinical and instrumental monitoring (pulse oximetry, doppler and invasive blood pressure, 3-lead electrocardiogram, EEG, rectal temperature monitoring and inhaled and exhaled gases) until tracheal extubation.
- To maintain hydration, provide Ringer’s lactate at a continuous rate infusion (CRI) of 5 ml/kg/h through the venous access. Always confirm proper anesthesia using toe pinches at an interval of 10 min.
- Disinfect the surgical field using povidone iodine from the manubrium sterni to both jaw angles. Now, perform sterile draping of the surgical field.
- During surgery, provide analgesia with lidocaine at a CRI of 50 microgram (µg)/kg/min and fentanyl at 3‒10 µg/kg/h. Apply spontaneous or assisted ventilation as well as permissive hypercapnia. Perform arterial blood gas analysis at least one time during surgery.
- Treat relevant hypotension (mean arterial pressure < 60 mmHg) with noradrenaline. Prevent hypothermia (rectal temperature ≤ 38 °C) using a heating pad or a heating forced-air warming system.
2. Surgical phase – Step I
- Start the surgery with a median skin incision from the manubrium sterni to the level of the jaw angles/larynx. Sharply dissect the skin and soft tissue with a scalpel, surgical scissors and forceps. Separate the subcutis and the fat pad medially by blunt dissection.
- Enter the anterior upper ridge of the sternocleidomastoid muscle medially on the left side by blunt dissection, using micro forceps and surgical scissors.
- Macroscopically, perform blunt preparation and carefully separate the left CCA from the vagal nerve distally to avoid laryngeal paresis by further using micro forceps and surgical scissors (Figure 2). Note that the bifurcation of the left CCA serves as intraoperative landmark (Figure 3 and Figure 4A). For all the following steps, use a soft tissue spreader to improve surgical visualization.
- After successful preparation and liberation of the left distal CCA from the vagal nerve, administer papaverine (40 mg/ml, 1:1 diluted in 0.9% isotonic sodium chloride solution) locally. Continuously protect all vessel segments with micro swabs followed by further papaverine administration externally. Place the papaverine-soaked left CCA below the autologous muscle tissue to protect the vessel from drying under the light of the operation microscope.
- Switch sides while maximizing the surgeon’s comfort during the operative procedure. Repeat the same surgical procedure on the right side. Dissect the CCA distally and proximally up to the predefined landmarks (carotid bifurcation at the level of the jaw angles/larynx and internal jugular vein; Figure 4A,B). Reinsert a spreader and administer micro swabs and papaverine as described previously.
- Before the ligation of the right proximal CCA, inject heparin (500 international units (IU)/kg) systemically via a venous ear catheter.
- Use a surgical microscope from now on. First, ligate the right proximal CCA with a 4-0 non-absorbable suture directly at the end of the macroscopically visible proximal landmark to avoid any tension on the arterial vessel.
- Secondly, apply a 6-0 non-absorbable ligature exactly 4‒5 mm distally by using a vessel clip for measurement, considering that after cutting distally from the first 4-0 ligature, the resulting arterial pouch will be of standardized length of about 3‒4 mm in every animal (Figure 5A,C).
- After tightening the 6-0 ligature, clamp the right CCA as far distally as possible with a temporary vessel clip (as normally used in cerebral aneurysm surgery) to avoid any endothelial damage and to create a long vessel segment for irrigation in order to prevent thrombogenesis (Figure 5B).
- Now perform a cut distally to the 4-0 non-absorbable ligature. To harvest the arterial pouch (Figure 5C), perform a second cut distally to the 6-0 non-absorbable ligature.
- Clean the arterial pouch meticulously from all soft tissue and measure its length, width and depth (Figure 5C) with a vessel clip. If no further modification is needed, keep the autologous arterial graft in a heparinized solution (500 IU/100 ml in 0.9% isotonic sodium chloride) at room temperature until further use.
3. Arterial pouch degradation
- If an arterial pouch degradation is needed, clean it meticulously of soft tissue and preincubate it with 100 IU of porcine elastase dissolved in 5 ml of Tris-buffer at room temperature on the day of experiment for 20 min. Do not use a brush technique. Incubate the arterial pouch intra- and extra-luminally by using a shaker.
- Before putting the pouch in a heparinized solution of 0.9% isotonic sodium chloride, gently swipe it three times for 3 min with anatomical forceps in 0.9% isotonic sodium chloride solution to wash out the remaining porcine elastase.
- If needed, keep the lumen of the arterial pouch opened up with a microtube made of silicone; meticulously protect the left and right CCA during the whole surgical procedure with wet micro paddings.
4. Surgical phase – Step II
- For further preparation of the CCA, place two round micro swabs directly beneath it to move the artery more superficially. Now, put one micro swab with a purple padding under the left CCA at the distal third for better visualization of the artery.
- Flush the right proximal CCA with a solution of 0.9% isotonic sodium chloride combined with 500 IU of heparin dissolved in 100 ml of 0.9% isotonic sodium chloride. In order to create a tension free anastomosis, place the right CCA under the fat pad/peritracheal musculature by using surgical scissors for tunneling it to the left side. Remove the soft tissue of the artery.
- Now perform a 2 mm fish mouth incision on the proximal side of the right CCA using a micro scissor and forceps.
- Change the side on the operating table. Clip the left distal CCA with another temporary vessel clip followed by the proximal left CCA with two temporary vessel clips. Protect all exposed vessel segments from drying out under the surgical light using wet micro swabs.
- Liberate the distal third of the left CCA completely from soft tissue and perform an arteriotomy. Use surgical micro forceps and gently grab some soft tissue. Now elevate the artery and incise the left distal CCA slowly with a surgical micro scissor. Flush the vessel segments with heparin (500 IU dissolved in 100 ml of 0.9% isotonic sodium chloride solution).
- After performing the arteriotomy with curved micro forceps and micro scissors, enlarge the arteriotomy located at the distal third of the left CCA distally, measuring about 2-fold of the diameter of the right blunt of the carotid artery and the autologous graft. This allows sufficient blood flow into the arterial pouch.
- Take the arterial pouch out of the heparinized saline solution. Place the pouch in the surgical field, where the bifurcation is planned. Start suturing the rear of the right carotid blunt caudally-located with a non-absorbable 9-0 suture, followed by a suture on the cranially-located rear side at the level of the fish mouth incision. Finish sewing the rear from distal to proximal by single stitches.
- While suturing, keep all elastase preincubated pouches moist with continuous irrigation. While suturing the vessel wall of the pouch, use curved surgical micro forceps to gently open up the lumen with its tip. Whenever suturing parts of the left or proximal right CCA, use straight surgical micro forceps. Afterwards, suture the horizontal back side.
- Next suture the horizontal front side, starting at the dome of the aneurysm moving to its base. Afterwards, start with single stitches distally on the front side moving caudally.
- For all steps 4.5‒4.8 while suturing the anastomosis pay attention just to grab the part of the vessel close to the arteriotomy to avoid iatrogenic stenosis. Also, continuously moisten all vessel segments during the whole surgical procedure extraluminally with a syringe filled with heparinized sodium chloride solution (500 IU dissolved in 100 ml of 0.9% isotonic sodium chloride) and protect them with wet micro swabs.
- Before finishing the anastomosis, irrigate the whole complex with heparinized 0.9% isotonic sodium chloride solution intraluminal (500 IU dissolved in 100 ml of 0.9% isotonic sodium chloride). Beware that elastase modified arterial pouches have to be sewn on as quickly as possible because of their strong tendency to dry out and to thrombose. Because of the aggressive behavior of the residual elastase concentration in the pouch regarding digesting circumferential vessels, proceed fast with the surgery to re-perfuse the vessel complex quickly.
- Remove all temporary vascular clamps stepwise.
- Remove the distal clamp from the left CCA. Accept minor bleeding and staunch it by gently imprinting micro swabs on the anastomosis. Afterwards, remove the clamp of the right CCA, press gently with micro swab and forceps to avoid thrombus formation.
- If needed, replace the temporary vascular clips to provide enough coagulation. Afterwards, relieve both vessel clips from the left side proximally. If needed in any step, replace clips to allow coagulation or to perform re-stitching.
- At this stage perform fluorescence angiography of the vessel complex (Figure 6 and Figure 7).
NOTE: Fluorescence angiography is performed by administering 1 ml of fluorescein IV, using 2 bandpass filters, a smartphone with video camera, and a bicycle spotlight. This procedure has been already described elsewhere20,21,22. - Lastly, close the operative situs. Readapt and gently suture the fat pad with a 3-0 resorbable suture with single nodes to protect the anastomosis. Close subcutis and skin in the same fashion.
5. Postsurgical phase
- Discontinue the isoflurane and systemic analgesia administration at the end of the surgery and provide tracheal extubation as soon as the swallowing reflex has returned.
- Administer 0.5 mg/kg of meloxicam IV, 10 mg/kg aspirin (ASS) IV, 100 µg of vitamin B12 SC and 20 mg/kg of clamoxyl IV.
- Provide supplementary oxygenation and active warming until the rabbits have spontaneously regained sternal recumbency.
- Perform postoperative follow-up and animal care four times a day for the first three days, in accordance to the guidelines for the assessment and management of pain in rodents and rabbits23,24.
- Administer post-operative analgesia via a fentanyl patch (12 µg/h) applied on the outer ear, meloxicam once a day SC for three days and methadone as rescue therapy SC, according with the score sheet for pain evaluation. Administer 250 IU/kg low-molecular heparin (LMH) subcutaneously for three days in all rabbits.
Representative Results
Following a pilot series of seven animals, totally 16 animals were included in the experimental protocol. Two animals died prematurely and were therefore excluded from the final analysis (12.5% mortality). Calculated on 14 animals, immediate aneurysm patency rate during fluorescence angiography was 71.43% in both, the control and modified group. Four aneurysms had to be reopened with consecutive thrombus evacuation and after a repeated fluorescence angiography there was a documented patency in all cases (100%). Aneurysm patency rate in MR- and fluorescence-angiography was 85.72% in the control and 85.72% in the elastase modified group at follow-up after 28 days (two animals showed complete parent artery and aneurysm thrombosis and therefore were excluded from further analysis). Partial thrombosis was observed by analyzing three-dimensional reconstructions of the MR-imaging (Figure 9) in 3 out of the 12 remaining cases. Both groups demonstrated an increase in aneurysm size over time; control group: 6.48 ± 1.81 mm3 at time of creation vs. 19.85 ± 6.40 mm3 at follow-up, p = 0.037 (all statistical tests were performed using the non-parametric Wilcoxon-Mann-Whitney-U test); modified group: 8.03 ± 1.08 mm3 at the time of creation vs. 20.29 ± 6.16 mm3 at follow-up, p = 0.054), showing no significance between both growth rates (p = 0.87). There was no postoperative aneurysm-related hemorrhage. Average duration of the surgical procedure for the control group was 164 ± 10 min (range, 122‒187 min) compared to 201 ± 13 min (range, 158‒250 min) for the modified group. An average of 24 ± 1 interrupted sutures (range, 21‒26) was needed to create aneurysms in the control group, 25 ± 2 (range, 18‒28) stitches in the elastase group. Figure 8 and Figure 9 show histological characteristics as well as CE-3D-MRA morphometric measurements of bifurcation aneurysms on day 28.
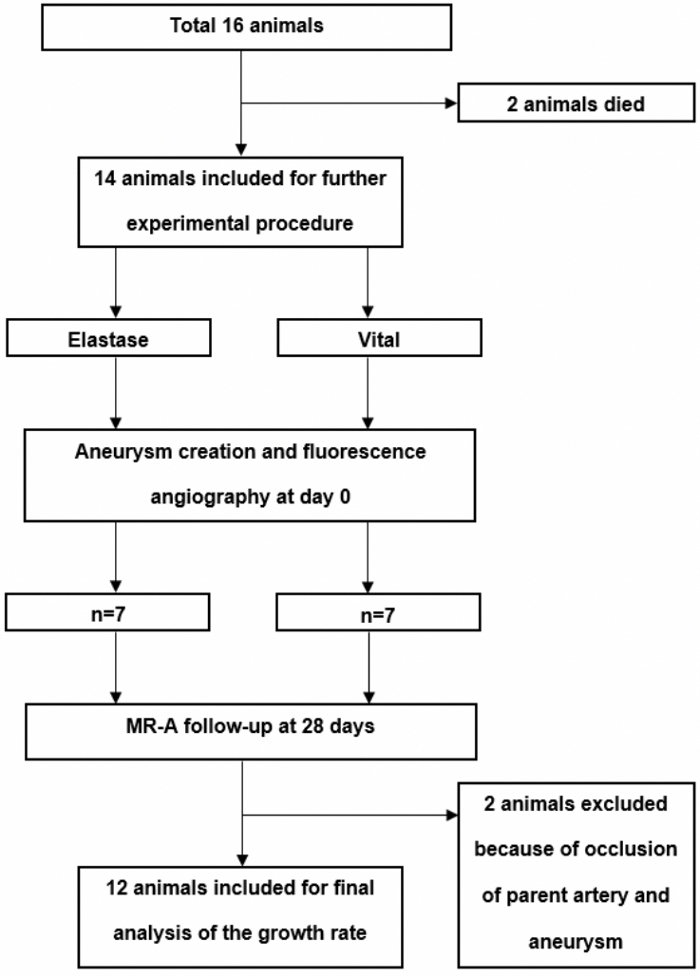
Figure 1: Flow chart of the experimental setting.
In total, after a piloting phase of seven animals, 16 animals were operated and either randomized to control group or elastase pretreatment. Two animals died in the early postoperative course. Please click here to view a larger version of this figure.
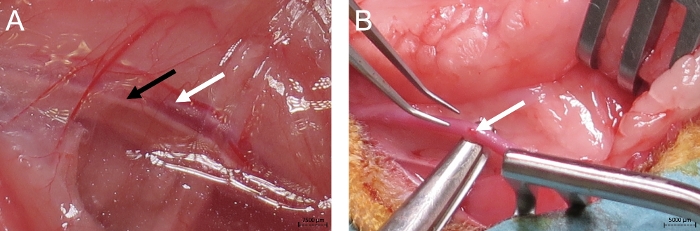
Figure 2: Initial operative step.
Initial operative step, depicting the left carotid artery (white arrow), vagal nerve (black arrow) (A) and the careful separation of the left carotid artery from the vagal nerve distally to avoid laryngeal paresis (B). Please click here to view a larger version of this figure.
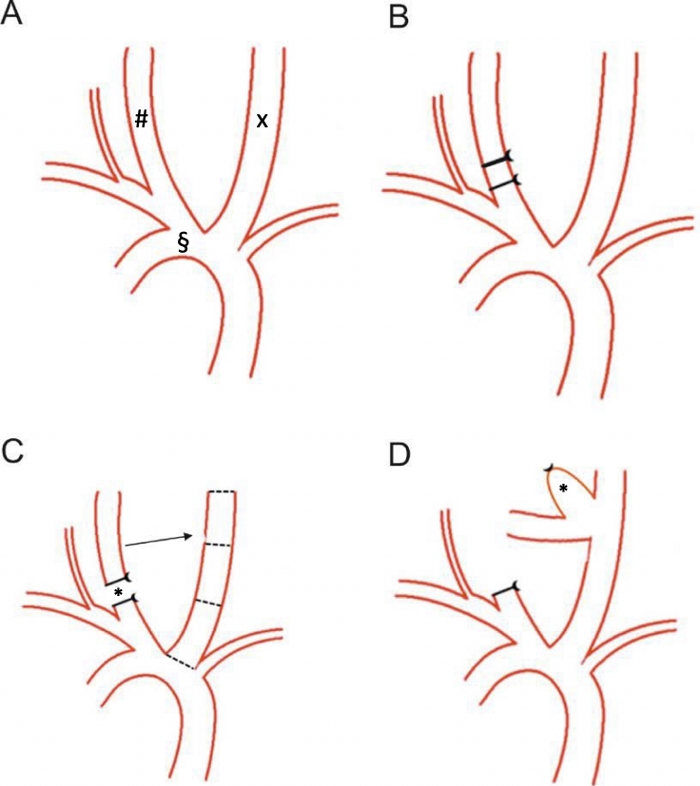
Figure 3: Schematic of the surgical steps.
The aortic arch (§) with both carotid arteries (left carotid artery, x; right carotid artery, #) of a New Zealand White rabbit is shown (A). On the proximal right carotid artery, a 4-0 ligature is performed, and a 6-0 ligature added distally (B). The autologous arterial pouch (*) has already been harvested and the blunt of the right carotid artery is sutured to the distal third of the left carotid artery (C) creating the artificial complex arterial bifurcation (D). Please click here to view a larger version of this figure.
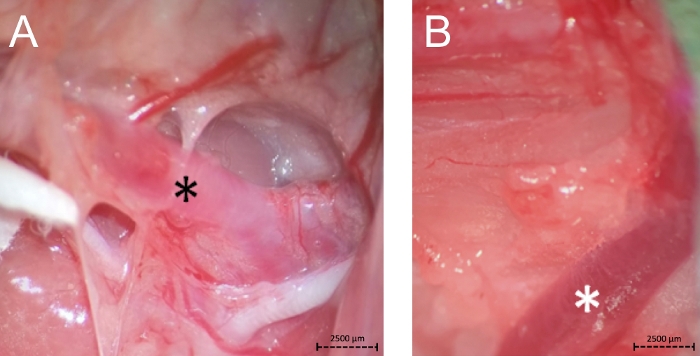
Figure 4: Bifurcation of the left carotid artery as a distal landmark for the left and right side (A, black *) and the internal jugular vein as proximal landmark for preparation of the right side (B, white *). Please click here to view a larger version of this figure.
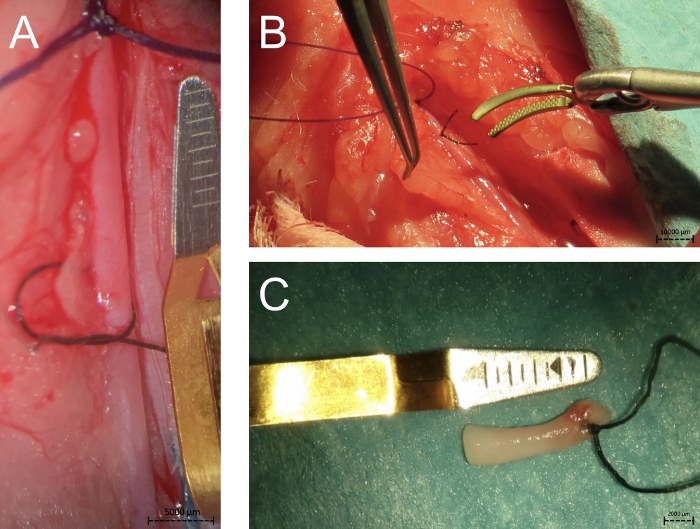
Figure 5: The photographs show the proximal 4-0 and 6-0 ligations of the right carotid artery for creating a new vital arterial pouch (A), the clip placement on the right carotid artery above the two ligatures (B) and the autologous harvested pouch (C). Please click here to view a larger version of this figure.
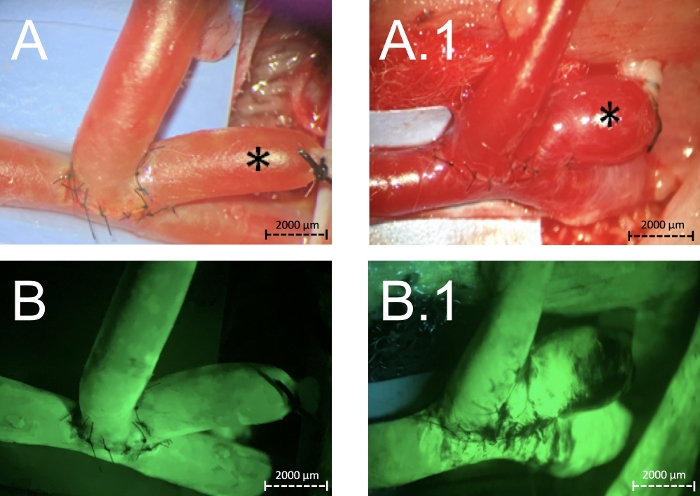
Figure 6: Creation of complex arterial vital (A) and after elastase pretreatment (A.1) bifurcation aneurysms (*).
The same situation after performing a fluorescence angiography showing patency of the parent arteries and of the aneurysms itself (B, B.1). Please click here to view a larger version of this figure.
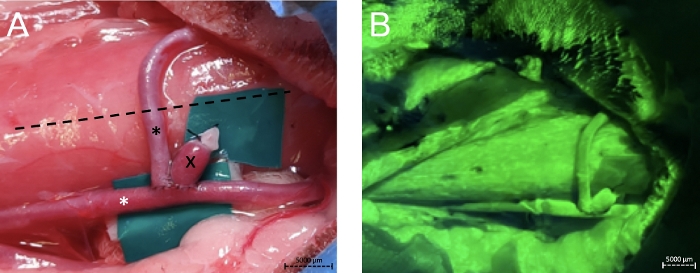
Figure 7: Fluorescence angiography of the vessel complex.
Zoomed out photograph (A) from the operative situs after creation of an elastase pretreated complex bifurcation aneurysm (x). Black * depicts the right common carotid artery, white * the left. The dotted line shows the middle of the neck. The same situation after performing a fluorescence angiography showing patency of the parent arteries and of the aneurysm itself (B). Please click here to view a larger version of this figure.
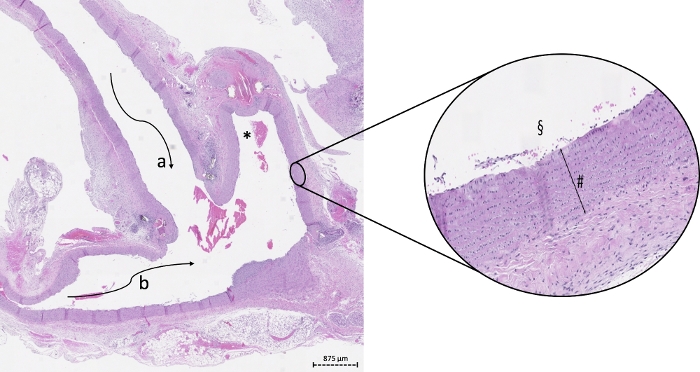
Figure 8: Example of histology on a 2-fold and 20-fold digital zoom of a vital aneurysm in bifurcation constellation.
The vital wall (#) is marked by high cell density. * depicts the lumen of the aneurysm, a the lumen of the right, b the lumen of the left proximal carotid artery, § the magnified luminal side of the aneurysm. Please click here to view a larger version of this figure.
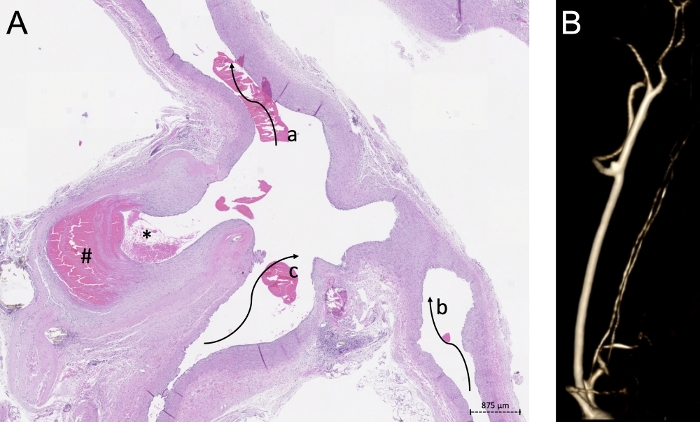
Figure 9: Histological findings correlated with MR-imaging.
(A) Example of 2-fold digital zoom of modified arterial pouch sewn on an arterial bifurcation The partial thrombosed aneurysm dome (#), the lumen of the aneurysm (*), the lumen of the left proximal (b) and distal (a) as well the lumen of the right carotid artery (c) is shown. (B) depicts the CE-3D-MRA morphometric measurements of the aneurysm after 28 days. Please click here to view a larger version of this figure.
| n | Operation Time (min) |
Weight (g) | # of Sutures (n) |
Diameter Parent Artery proximal to the Aneurysm (mm) |
Suture Time (min) |
Diameter Parent Artery distal to the Aneurysm (mm) |
Diameter Aneurysm baseline (mm) |
Volume baseline (mm3) |
Diameter Aneurysm follow-up (mm) |
Volume follow-up (mm3) |
|
| Vital pouches | |||||||||||
| 1 | 187 | 4100 | 24 | 2.5 | 54 | 2.8 | 1 | 1.96 | 1.5 | 5 | |
| 2 | 183 | 4200 | 24 | 3.3 | 53 | 2.9 | 1 | 2.35 | 2.8 | 7.73 | |
| 3 | 163 | 3800 | 26 | 3.4 | 66 | 3 | 1.5 | 4.71 | 3.1 | 28.03 | |
| 4 | 122 | 3600 | 22 | 2.8 | 42 | 2.8 | 2 | 6.28 | 3.2 | 47.37 | |
| 5 | 180 | 3700 | 24 | 3.2 | 45 | 3 | 2 | 10.99 | 2 | 15.82 | |
| 6 | 149 | 3700 | 21 | 2.3 | 47 | 2.2 | 2 | 12.56 | 3.1 | 15.11 | |
| Mean ± SEM | 164.00 ± 10.22 | 3850.00 ± 99.16 | 23.50 ± 0.72 | 2.92 ± 0.19 | 51.17 ± 3.52 | 2.78 ± 0.12 | 1.58 ± 0.201 | 6.48 ± 1.81 | 2.62 ± 0.29 | 19.85 ± 6.40 | |
| Elastase pouches | |||||||||||
| 1 | 158 | 3400 | 26 | 2.9 | 76 | 2.6 | 2 | 9.42 | 2.1 | 12.26 | |
| 2 | 180 | 3400 | 27 | 3.5 | 43 | 2.8 | 2 | 10.99 | 3.3 | 46.16 | |
| 3 | 250 | 3900 | 27 | 3.5 | 70 | 3.2 | 1.4 | 6.59 | 2.2 | 10.1 | |
| 4 | 208 | 4200 | 28 | 3 | 45 | 2.6 | 2 | 9.42 | 2.6 | 24 | |
| 5 | 192 | 3660 | 18 | 2.8 | 53 | 2.8 | 2 | 8.24 | 2.7 | 4.03 | |
| 6 | 217 | 3200 | 24 | 2.7 | 58 | 2.8 | 1.5 | 3.53 | 2.2 | 25.16 | |
| Mean ± SEM | 200.83 ± 13.00 | 3626.67 ± 151.58 | 25.00 ± 1.51 | 3.07 ± 0.14 | 57.50 ± 5.43 | 2.80 ± 0.09 | 1.82 ± 0.12 | 8.03 ± 1.08 | 2.52 ± 0.19 | 20.29 ± 6.16 | |
| p-value | 0.06 | 0.22 | 0.14 | 0.46 | 0.42 | 0.5 | // | 0.46 | // | 0.87 | |
Table 1: Surgical characteristics and CE-3D-MRA morphometric measurements.
Discussion
Our study demonstrates the feasibility of creating a true bifurcation aneurysm model with different wall conditions in rabbits. Overall, 14 female New Zealand White rabbits with a mean weight of 3.7 ± 0.09 kg and mean age of 112 ± 3 days were included in the study. 85.72% of all aneurysms remained patent during a follow-up at 28 days. Two animals died prematurely (12.5% mortality).
Previous studies suggested a variety of extracranial aneurysm models to analyze the management of endovascular aneurysm treatment25,26,27,28. However, none of these have allowed the comparison of different wall conditions. Previous experiments already studied decellularized aneurysms in an aneurysm side-wall rat model29. The model presented in the current study represents a translational refinement, since a true arterial pouch bifurcation model mimicking different wall conditions has not been described in literature, yet. Additionally, intracranial aneurysms in humans occur more frequently at arterial bifurcations30,31. Furthermore, rabbit models were shown to be very close to humans with regards to hemodynamics and comparability of the coagulation system and further on proofed to be cost-effective32,33,34.
Venous pouch models in rabbits (solely, complex bilobular, complex bisaccular or with broad necks) have already been well described.12,13,35,36 Like mentioned, the technique of implanting true arterial pouches or degenerated vessel walls into an artificial bifurcation has not been described, yet.37,38,39 In our study, the mortality rate was 12.5%. Compared to literature with high morbidity and mortality rates up to 50%, we stayed clearly below and thus demonstrated the feasibility of creating complex arterial bifurcation aneurysms in rabbits with low morbidity, mortality and high short term as well as long-term aneurysm patency rates27. An additional important factor that enabled lowering morbidity and mortality rates in this rabbit series was the implementing surgical techniques from former experiences of our laboratory12. Exemplary, the technique of careful preparing a long segment of the left CCA was applied and refined to just dissecting the distal third, especially to avoid iatrogenic lesions on the vagal nerve and superior laryngeal nerves. Also, highly thrombogenic soft tissue was removed meticulously from both CCAs before performing a tensionless anastomosis. Sutures, always starting on the backside for a better visual control, were kept low in number to avoid iatrogenic thrombogenesis. If needed, sealing with autologous fat tissue around the anastomosis was performed to minimize the risk of postoperative bleeding; likewise readapting and suturing the fat-pad directly above the anastomosis provided additional protective effect. A controlled preparation and dissection of the vagal nerve with associated laryngeal fibers as well as a sufficient preparation of the right CCA proximally and distally for creating a tensionless anastomosis, play key roles in reducing mortality and morbidity from respiratory distress or laryngeal palsy12.
Using the anticoagulation regimen with LMH for three days, using ASS (provided as a single shot immediate postoperatively) along with the newly initiated systemic administration of heparin before closing the right CCA led to 85.72% aneurysm and parent-vessel patency. These results are in line with our previous experiences with venous pouch models10,11,12,13,40. In this regard, intraoperative fluorescence angiography also contributed to good long-term patency rates with a reduction in morbidity. In cases of thrombus detection in the aneurysm itself or in the parent artery, reopening of the anastomosis was performed with thrombus evacuation20. No spontaneous aneurysm hemorrhage has been observed. Nevertheless, continuous extraluminal irrigation and vessel protection with wet micro swabs as well as intraluminal irrigation with heparinized 0.9% saline solution additively contributed to counteracting thrombogenic influences. In our opinion, balanced anesthesia and continuous extensive intraoperative and post-operative monitoring positively influenced mortality and morbidity as well. Extending the analgesic care for at least 72 h and guaranteeing an uninterrupted feeding could have contributed to reducing other complications such as gastrointestinal stress ulcers.
Several studies have demonstrated a stronger increase of aneurysm size in deteriorated aneurysms over time7,29. In our series, these findings could not be confirmed. The control group demonstrated a significant aneurysm growth over time. Nevertheless the p-value of the modified group showed a trend towards significant growth pattern compared with the control group (p = 0.054). This insignificant growth rate with equal volumes in the elastase modified group after 28 days could at least be partially explained by the large initial aneurysm volume. Also, the small animal number as well as the follow-up of only 28 days is a potential reason why extensive aneurysm growth was observed in two cases only. Furthermore, there is a learning curve involved for the surgeon14,15,41.
A direct comparison of the control and elastase-modified bifurcation pouches, in terms of endovascular coil treatment, is still missing. For venous pouches, an initial complete and incomplete occlusion rate of 35% and 65% was already reported27. After 3‒6 months follow-up, complete occlusion could just be objectified in 15%27. Regarding the excellent patency rates of this new animal model presented, arterial degenerated pouches can be further evaluated with coil-embolization, stent-treatment or stent-assisted coil-embolization in a prospective setting under physiological and pathophysiological conditions.
The elastase-modified arterial pouches are difficult to be sewn on because the walls of the pouch are very sticky; the pouch itself reacts very thrombogenically and therefore the lumen is not as naturally opened-up as compared to the control group. When suturing the pouch, ensure that no tension is applied on the circumferent vessels because elastase behaves aggressively in impairing angioarchitecture of the parent arteries as mentioned above.
Lastly, this model, if practiced over a certain period of time, provides great value for neurosurgical residents in adapting microsurgical skills by continuously performing highly microsurgical procedures42. After initial training, the techniques can be easily applied and performed in a safe and standardized fashion.
Limitations of this study are the low animal number in terms of a feasibility study as well as the potential thrombogenic properties of the suture material and the modified arterial pouch. Further on, this model depicts an extracranial aneurysm model which cannot be set equivalent to an intracranial setting. Furthermore, this model requires many resources (a veterinarian, a surgical assistant, a nurse and anesthesia machines). An advantage of the approach is the possibility of implanting elastase-modified arterial as well as non-modified pouches in one surgery. So, the 3R principles regarding animal welfare are strictly followed.
In summary, we present a novel, reproducible and standardized protocol to create autologous arterial pouch bifurcation aneurysms mimicking different wall conditions. Given the excellent long-term patency and property of aneurysm growth over time in the non-modified and modified pouch group as well, this model may serve as an important tool for further preclinical evaluation of novel endovascular devices. For sure, these results have to be confirmed in a bigger series.
Divulgaciones
The authors have nothing to disclose.
Acknowledgements
The authors thank Olgica Beslac and Kay Nettelbeck for their excellent support and technical assistance during the peri-operative phase and Alessandra Bergadano, DVM, PhD, for the dedicated supervision of the long-term animal health.
Materials
| 3-0 resorbable suture | Ethicon Inc., USA | VCP428G | |
| 4-0 non-absorbable suture | B. Braun, Germany | G0762563 | |
| 6-0 non-absorbable suture | B. Braun, Germany | C0766070 | |
| 9-0 non-absorbable suture | B. Braun, Germany | G1111140 | |
| Adrenaline | Amino AG | 1445419 | any generic |
| Amiodarone | Helvepharm AG | 5078567 | any generic |
| Anesthesia machine | Dräger | any other | |
| Aspirin | Sanofi-Aventis (Suisse) SA | 622693 | any generic |
| Atropine | Labatec Pharma SA | 6577083 | any generic |
| Bandpass filter blue | Thorlabs | FD1B | any other |
| Bandpass filter green | Thorlabs | FGV9 | any other |
| Bipolar forceps | any other | ||
| Bicycle spotlight | any other | ||
| Biemer vessel clip (2 x) | B. Braun Medical AG, Aesculap, Switzerland | FD560R | temporary |
| Bispectral index (neonatal) | any other | ||
| Blood pressure cuff (neonatal) | any other | ||
| Clamoxyl | GlaxoSmithKline AG | 758808 | any generic |
| Dexmedetomidine | Ever Pharma | 136740-1 | any generic |
| Electrocardiogram electrodes | any other | ||
| Elastase | Sigma Aldrich | 45125 | any generic |
| Ephedrine | Amino AG | 1435734 | any generic |
| Esmolol | OrPha Swiss GmbH | 3284044 | any generic |
| Fentanyl (intravenous use) | Janssen-Cilag AG | 98683 | any generic |
| Fentanyl (transdermal) | Mepha Pharma AG | 4008286 | any generic |
| Fluoresceine | Curatis AG | 5030376 | any generic |
| Fragmin | Pfizer PFE Switzerland GmbH | 1906725 | any generic |
| Glyco | any generic | ||
| Heating pad | any other | ||
| Isotonic sodium chloride solution (0.9%) | Fresenius KABI | 336769 | any generic |
| Ketamine | Pfizer | 342261 | any generic |
| Laboratory shaker | Stuart | SRT6 | any other |
| Lidocaine | Streuli Pharma AG | 747466 | any generic |
| Longuettes | any other | ||
| Metacam | Boehringer Ingelheim | P7626406 | any generic |
| Methadone | Streuli Pharma AG | 1084546 | any generic |
| Microtubes | any other | ||
| Micro needle holder | any other | ||
| Midazolam | Accord Healthcare AG | 7752484 | any generic |
| Needle holder | any other | ||
| O2-Face mask | any other | ||
| Operation microscope | Wild Heerbrugg | any other | |
| Papaverine | Bichsel | any generic | |
| Prilocaine-lidocaine creme | Emla | any generic | |
| Propofol | B. Braun Medical AG, Switzerland | any generic | |
| Pulse oxymeter | any generic | ||
| Rectal temperature probe (neonatal) | any other | ||
| Ropivacaine | Aspen Pharma Schweiz GmbH | 1882249 | any generic |
| Scalpell | Swann-Morton | 210 | any other |
| Small animal shaver | any other | ||
| Smartphone | any other | ||
| Soft tissue forceps | any other | ||
| Soft tissue spreader | any other | ||
| Stainless steel sponge bowls | any other | ||
| Sterile micro swabs | any other | ||
| Stethoscope | any other | ||
| Straight and curved micro-forceps | any other | ||
| Straight and curved micro-scissors | any other | ||
| Straight and curved forceps | any other | ||
| Surgery drape | any other | ||
| Surgical scissors | any other | ||
| Syringes 1 ml, 2ml and 5 ml | any other | ||
| Tris-Buffer | Sigma Aldrich | 93302 | any generic |
| Vascular clip applicator | B. Braun, Germany | FT495T | |
| Vein and arterial catheter 22 G | any generic | ||
| Vitarubin | Streuli Pharma AG | 6847559 | any generic |
| Yasargil titan standard clip (2 x) | B. Braun Medical AG, Aesculap, Switzerland | FT242T | temporary |
Referencias
- Wanderer, S., Mrosek, J., Gessler, F., Seifert, V., Konczalla, J. Vasomodulatory effects of the angiotensin II type 1 receptor antagonist losartan on experimentally induced cerebral vasospasm after subarachnoid haemorrhage. Acta Neurochirurgica (Wien). 160 (2), 277-284 (2018).
- Vatter, H., et al. Effect of delayed cerebral vasospasm on cerebrovascular endothelin A receptor expression and function. Journal of Neurosurgery. 107 (1), 121-127 (2007).
- Andereggen, L., et al. The role of microclot formation in an acute subarachnoid hemorrhage model in the rabbit. Biomed Research International. , 161702 (2014).
- Eriksen, N., et al. Early focal brain injury after subarachnoid hemorrhage correlates with spreading depolarizations. Neurology. 92 (4), 326-341 (2019).
- Thompson, J. W., et al. In vivo cerebral aneurysm models. Neurosurgical Focus. 47 (1), 20 (2019).
- Bouzeghrane, F., Naggara, O., Kallmes, D. F., Berenstein, A., Raymond, J. International Consortium of Neuroendovascular C. In vivo experimental intracranial aneurysm models: a systematic review. American Journal of Neuroradiology. 31 (3), 418-423 (2010).
- Marbacher, S., et al. Loss of mural cells leads to wall degeneration, aneurysm growth, and eventual rupture in a rat aneurysm model. Stroke. 45 (1), 248-254 (2014).
- Marbacher, S., et al. Intraluminal cell transplantation prevents growth and rupture in a model of rupture-prone saccular aneurysms. Stroke. 45 (12), 3684-3690 (2014).
- Marbacher, S., Niemela, M., Hernesniemi, J., Frosen, J. Recurrence of endovascularly and microsurgically treated intracranial aneurysms-review of the putative role of aneurysm wall biology. Neurosurgical Review. 42 (1), 49-58 (2019).
- Marbacher, S., et al. Complex bilobular, bisaccular, and broad-neck microsurgical aneurysm formation in the rabbit bifurcation model for the study of upcoming endovascular techniques. American Journal of Neuroradiology. 32 (4), 772-777 (2011).
- Marbacher, S., et al. Long-term patency of complex bilobular, bisaccular, and broad-neck aneurysms in the rabbit microsurgical venous pouch bifurcation model. Neurological Research. 34 (6), 538-546 (2012).
- Sherif, C., Marbacher, S., Erhardt, S., Fandino, J. Improved microsurgical creation of venous pouch arterial bifurcation aneurysms in rabbits. American Journal of Neuroradiology. 32 (1), 165-169 (2011).
- Sherif, C., et al. Microsurgical venous pouch arterial-bifurcation aneurysms in the rabbit model: technical aspects. Journal of Visualized Experiments. 51, 2718 (2011).
- Brinjikji, W., Ding, Y. H., Kallmes, D. F., Kadirvel, R. From bench to bedside: utility of the rabbit elastase aneurysm model in preclinical studies of intracranial aneurysm treatment. Journal of Neurointerventional Surgery. 8 (5), 521-525 (2016).
- Miskolczi, L., Guterman, L. R., Flaherty, J. D., Hopkins, L. N. Saccular aneurysm induction by elastase digestion of the arterial wall: a new animal model. Neurosurgery. 43 (3), 595-600 (1998).
- Lewis, D. A., et al. Morbidity and mortality associated with creation of elastase-induced saccular aneurysms in a rabbit model. American Journal of Neuroradiology. 30 (1), 91-94 (2009).
- Kilkenny, C., Browne, W., Cuthill, I. C., Emerson, M., Altman, D. G. Group NCRRGW. Animal research: reporting in vivo experiments: the ARRIVE guidelines. Journal of Cerebral Blood Flow and Metabolism. 31 (4), 991-993 (2011).
- Tornqvist, E., Annas, A., Granath, B., Jalkesten, E., Cotgreave, I., Oberg, M. Strategic focus on 3R principles reveals major reductions in the use of animals in pharmaceutical toxicity testing. PLoS One. 9 (7), (2019).
- Irlbeck, T., Zwissler, B., Bauer, A. ASA classification: Transition in the course of time and depiction in the literature]. Der Anaesthesist. 66 (1), 5-10 (2017).
- Grüter, B. E., et al. Fluorescence Video Angiography for Evaluation of Dynamic Perfusion Status in an Aneurysm Preclinical Experimental Setting. Oper Neurosurg (Hagerstown). 17 (4), 432-438 (2019).
- Grüter, B. E., et al. Testing bioresorbable stent feasibility in a rat aneurysm model. Journal of Neurointerventional Surgery. 11 (10), 1050-1054 (2019).
- Strange, F., et al. Fluorescence Angiography for Evaluation of Aneurysm Perfusion and Parent Artery Patency in Rat and Rabbit Aneurysm Models. Journal of Visualized Experiments. (149), e59782 (2019).
- Weaver, L. A., Blaze, C. A., Linder, D. E., Andrutis, K. A., Karas, A. Z. A model for clinical evaluation of perioperative analgesia in rabbits (Oryctolagus cuniculus). Journal of the American Association of Laboratory Animal Science. 49 (6), 845-851 (2010).
- ACLAM Task Force Members. Public statement: guidelines for the assessment and management of pain in rodents and rabbits. Journal of the American Association of Laboratory Animal Science. 46 (2), 97-108 (2007).
- Forrest, M. D., O’Reilly, G. V. Production of experimental aneurysms at a surgically created arterial bifurcation. American Journal of Neuroradiology. 10 (2), 400-402 (1989).
- Kwan, E. S., Heilman, C. B., Roth, P. A. Endovascular packing of carotid bifurcation aneurysm with polyester fiber-coated platinum coils in a rabbit model. American Journal of Neuroradiology. 14 (2), 323-333 (1993).
- Spetzger, U., Reul, J., Weis, J., Bertalanffy, H., Thron, A., Gilsbach, J. M. Microsurgically produced bifurcation aneurysms in a rabbit model for endovascular coil embolization. Journal of Neurosurgery. 85 (3), 488-495 (1996).
- Bavinzski, G., et al. Experimental bifurcation aneurysm: a model for in vivo evaluation of endovascular techniques. Minimal Invasive Neurosurgery. 41 (3), 129-132 (1998).
- Marbacher, S., Marjamaa, J., Abdelhameed, E., Hernesniemi, J., Niemela, M., Frosen, J. The Helsinki rat microsurgical sidewall aneurysm model. Journal of Viusalized Experiments. (92), e51071 (2014).
- Alfano, J. M., et al. Intracranial aneurysms occur more frequently at bifurcation sites that typically experience higher hemodynamic stresses. Neurosurgery. 73 (3), 497-505 (2013).
- Sakamoto, S., et al. Characteristics of aneurysms of the internal carotid artery bifurcation. Acta Neurochirurgica (Wien). 148 (2), 139-143 (2006).
- Dai, D., et al. Histopathologic and immunohistochemical comparison of human, rabbit, and swine aneurysms embolized with platinum coils. American Journal of Neuroradiology. 26 (10), 2560-2568 (2005).
- Shin, Y. S., Niimi, Y., Yoshino, Y., Song, J. K., Silane, M. Berenstein A. Creation of four experimental aneurysms with different hemodynamics in one dog. American Journal of Neuroradiology. 26 (7), 1764-1767 (2005).
- Abruzzo, T., Shengelaia, G. G., Dawson, R. C., Owens, D. S., Cawley, C. M., Gravanis, M. B. Histologic and morphologic comparison of experimental aneurysms with human intracranial aneurysms. American Journal of Neuroradiology. 19 (7), 1309-1314 (1998).
- Spetzger, U., Reul, J., Weis, J., Bertalanffy, H., Gilsbach, J. M. Endovascular coil embolization of microsurgically produced experimental bifurcation aneurysms in rabbits. Surgical Neurology. 49 (5), 491-494 (1998).
- Reul, J., Weis, J., Spetzger, U., Konert, T., Fricke, C., Thron, A. Long-term angiographic and histopathologic findings in experimental aneurysms of the carotid bifurcation embolized with platinum and tungsten coils. American Journal of Neuroradiology. 18 (1), 35-42 (1997).
- Marbacher, S., Strange, F., Frosen, J., Fandino, J. Preclinical extracranial aneurysm models for the study and treatment of brain aneurysms: A systematic review. Journal of Cerebral Blood Flow and Metabolism. , (2020).
- Strange, F., Gruter, B. E., Fandino, J., Marbacher, S. Preclinical Intracranial Aneurysm Models: A Systematic Review. Brain Sciences. 10 (3), 134 (2020).
- Marbacher, S., Wanderer, S., Strange, F., Gruter, B. E., Fandino, J. Saccular Aneurysm Models Featuring Growth and Rupture: A Systematic Review. Brain Sciences. 10 (2), 101 (2020).
- Coluccia, D., et al. A microsurgical bifurcation rabbit model to investigate the effect of high-intensity focused ultrasound on aneurysms: a technical note. Journal of Therapeutic Ultrasound. 2, 21 (2014).
- Hoh, B. L., Rabinov, J. D., Pryor, J. C., Ogilvy, C. S. A modified technique for using elastase to create saccular aneurysms in animals that histologically and hemodynamically resemble aneurysms in human. Acta Neurochirurgica (Wien). 146 (7), 705-711 (2004).
- Morosanu, C. O., Nicolae, L., Moldovan, R., Farcasanu, A. S., Filip, G. A., Florian, I. S. Neurosurgical Cadaveric and In Vivo Large Animal Training Models for Cranial and Spinal Approaches and Techniques – Systematic Review of Current Literature. Neurologia i neurochirurgia polska. 53 (1), 8-17 (2019).

