Mouse Round Spermatid Injection
Summary
Here, we introduce a method for performing round spermatid injection (ROSI) in mice, a technique with promising clinical applications and utility for investigating the mechanisms underlying embryonic development.
Abstract
Round spermatids, characterized by their haploid genetic content, represent the precursor cells to mature spermatozoa. Through the innovative technique of round spermatid injection (ROSI), oocytes can be successfully fertilized and developed into viable fetuses. In a groundbreaking milestone achieved in 1995, the first mouse fetus was born through ROSI technology. ROSI has since emerged as a pivotal tool for unraveling the intricate mechanisms governing embryonic development and holds significant potential in various applications, including the acceleration of mouse generation and the production of genetically modified mice. In 1996, a milestone was reached when the first human fetus was born through ROSI technology. However, the clinical applications of this method have shown a fluctuating pattern of success and failure. To date, ROSI technology has not found widespread application in clinical practice, primarily due to its low birth efficiency and insufficient validation of fetal safety. This article provides a comprehensive account of the precise methods of performing ROSI in mice, aiming to shed new light on basic research and its potential clinical applications.
Introduction
The final stage of spermatogenesis involves the transformation of a round spermatid into a fully developed spermatozoon, characterized by distinct head, neck, and elongated tail structures1. This transformation encompasses significant changes in cell morphology, such as the condensation of chromatin in the nucleus, replacement of histones by protamine, acrosome formation, mitochondrial sheath development, centriole migration and loss, tail structure formation, and the removal of cellular residues2.
In 1992, the first human fetus was successfully born through intracytoplasmic sperm injection (ICSI) technology3. Since then, researchers have been exploring the potential of utilizing round spermatids, which share the same haploid genetic composition as mature spermatozoa, to fertilize oocytes and sustain viable pregnancies2,4. Subsequently, in 1996, the first human fetus conceived via round spermatid injection (ROSI) technology was delivered5,6. It is worth noting that studies involving ICSI and ROSI in mice lagged behind those in humans due to the susceptibility of the mouse oocyte membrane to damage during the injection process. This issue was successfully resolved with the introduction of the Piezo membrane-breaking device. Consequently, in 1995, the first mouse conceived through ROSI technology was born. Additionally, research on ROSI in various other animals is also underway7,8.
Currently, research on ROSI primarily centers around the following aspects: clinical application, mechanism elucidation, and strategies to enhance developmental efficiency, along with broader applications of ROSI technology. In the context of clinical applications, despite the birth of the first ROSI human fetus through ROSI in 1996, progress has been marked by a series of successes and failures9,10,11,12. To date, ROSI technology has not achieved widespread clinical implementation, largely due to its low efficiency and the need for further validation regarding the safety of fetuses conceived through ROSI technology. Incomplete statistics indicate that globally, fewer than 200 human ROSI-conceived fetuses have been delivered. A turning point in understanding the potential of ROSI technology occurred in 2015 when Tanaka and colleagues reported on the successful birth of 14 fetuses through ROSI technology, instilling renewed confidence in its clinical application and feasibility13,14. ROSI technology holds substantial promise for addressing reproductive biology challenges, particularly in non-obstructive azoospermia patients. In addition to its clinical applications, ROSI serves as a valuable tool for studying the intricate mechanisms of embryonic development15,16,17.
Numerous animal studies have been conducted to investigate the underlying factors contributing to the low efficiency of ROSI in achieving full embryonic development. These factors encompass the choice of assisted oocyte activation (AOA) methods and their timings, abnormalities in genomic stability, and, particularly, abnormalities in epigenetic modifications. It is important to recognize that round spermatids are immature germ cells, differing significantly from mature spermatozoa in various physiological aspects. Mizuki Sakamoto and colleagues indicated that H3K27me3, derived from round spermatids, is associated with chromatin that is less accessible and leads to impaired gene expression in ROSI embryos18. In a related study by Jing Wang and colleagues, reprogramming defects in ROSI embryos at the pronuclear stages were predominantly associated with the misexpression of a cohort of the genes responsible for minor zygotic genome activation19. They also found that introducing a selective euchromatic histone lysine methyltransferase 2 inhibitor, A366, could potentially enhance the overall developmental rate by approximately twofold.
The mouse stands as one of the most valuable model animals for studying embryonic development. This article elaborates on how to perform ROSI on mice. This comprehensive protocol encompasses the selection of suitable mice, detailed ovulation induction procedures, AOA techniques, injection techniques, and the preparation of surrogate mice. Furthermore, we present a comparative analysis of the effects of two injection regimens on birth efficiency: AOA followed by ROSI (A-ROSI; first regimen) and ROSI followed by AOA (ROSI-A; second regimen). We aim to encourage researchers to conduct mouse ROSI experiments with greater precision, offering more robust support for their clinical application and the fundamental research of embryonic development mechanisms.
Protocol
B6D2F1 (C57BL/6 x DBA/2), C57BL/6, and ICR mice used in this experiment were purchased from Beijing Vital River Laboratory Animal Technologies Co. Ltd. (Beijing, China). All animal treatments adhered to the experimental procedures and standards approved by the Experimental Animal Ethics Committee of the First Hospital of Jilin University (approval number: 20200435).
1. Preparation of relevant reagents
- Acquire some reagents commercially and self-prepare the remaining reagents.
- Obtain M2, a buffer system for in vitro processing of round spermatids (RS), spermatozoa, and oocytes from the supplier.
- Prepare the Ca2+-free C.L. Chatot, C.A. Ziomek, and B.D. Bavister (CZB) medium for AOA following the previously published protocol20.
- Obtain the potassium simplex optimized medium supplemented with amino acids (KSOMaa) solution for embryo culture from the supplier.
- Prepare hyaluronidase, with a working concentration of 0.1% (1 g/L), by dissolving 0.1 g of hyaluronidase in 1 mL of embryo water. Take 10 µL of concentrated storage solution and dissolve in 990 mL of M2, which could be stored at 4 °C for 1 week.
- Prepare polyvinylpyrrolidone (PVP), with an average molecular weight of 360,000 and a mass concentration of 12%, by dissolving 1.2 g of PVP in 10 mL of M2. The resulting solution could be stored at 4 °C for 1 week.
- Store the cytochalasin B (CB) stock solution (2 µL), soluble in 18 µL of DMSO at -20 °C. Take 5 µL of the concentrated storage solution and dissolve in 995 mL of M2. The resulting solution could be stored at 4 °C for 1 week.
2. Preparation of oocytes
- Acclimate female B6D2F1 mice, aged 6-8 weeks, to their new environment for at least 1 week. Inject intraperitoneally with 7.5 IU of pregnant mare serum gonadotropin (PMSG) at 5 pm, followed by 7.5 IU of human chorionic gonadotropin (HCG) 48 h later. Ensure no contact with male mice occurs after the injection.
- After 14 h of HCG injection, euthanize the mice using the cervical dislocation method. Open the abdominal cavity and locate the uterus. Identify the ovaries along the uterus and sever the fallopian tubes near the ovaries using scissors. Repeat the same procedure on the other side and place the fallopian tubes in M2, which is preheated at 37 °C in advance.
- Under an upright microscope (10x), locate the enlarged part of the fallopian tube, showing a transparent and swollen appearance. Use a 1 mL syringe to secure the fallopian tube while cutting the enlarged part, collecting oocyte coronal cumulus complexes (OCCCs).
- Place OCCCs into the preheated M2 operating solution containing 0.1% hyaluronidase and remove granulosa cells by gently blowing through an oral pipette.
NOTE: Keep the OCCCs in 0.1% hyaluronidase for a short duration, approximately 2 min, if needed. - After removing the granulosa cells, transfer the oocyte to KSOMaa, rinse 3x, and place in a carbon dioxide incubator for later use (37 °C, 5% CO2).
3. Preparation of round spermatids and spermatozoa
- Collect round spermatids and spermatozoa from the testis and epididymis of male C57BL/6 mice (8-10 weeks), respectively.
- For spermatozoa, euthanize the mice by cervical dislocation. Open the abdominal cavity, locate the epididymis near the testis, and gently excise with scissors.
- Place the epididymis in M2 medium and gently excise using a 1 mL syringe to allow spermatozoa to flow out under an upright microscope (10x).
- Siphon the flowing spermatozoa and M2 suspension into the bottom of a tube containing 0.5 mL of M2, allowing the spermatozoa to flow upstream naturally. Set them aside for later use.
- For round spermatids, remove the testicles from the abdominal cavity and place them in M2. Gently cut the white membrane through using a 1 mL syringe and squeeze the convoluted seminiferous tubules out under an upright microscope (10x).
- Excise the seminiferous tubules carefully using two 1 mL syringes. Extract the suspension and filter with a 400-mesh sieve (38 µm).
- Centrifuge the filtered cells, discard the supernatant, and add 200 µL of Hoechst 33342 for staining, followed by incubation at 37 °C for 10 min.
- Perform fluorescence-activated cell sorting (FACS) to distinguish round spermatids from other cell types. Place the stained cells into a flow cytometry tube and perform a round spermatid screening.
- Different models of flow cytometry machines have different regulatory parameters and can be communicated with technical support during operation. As the first step, adjust the voltage and select the cell population according to forward scatter (FSS) and side scatter (SSC; see Supplementary Table 1).
- For the second step, remove cell adhesions according to FSC and trigger pulse width.
- As the third step, select the target haploid round spermatids. Hoechst 33342 binds to DNA, and cells with different ploidy exhibit different fluorescence intensities. Set the excitation wavelength to 355. Select two detection channels, 460/50 and 670/30, under 355 wavelength laser to sort round spermatids. Subsequently, store the sorted round spermatids in a 4 °C refrigerator for later use.
NOTE: It is also possible to directly select round spermatids based on their morphology under a microscope, but training is required to ensure selection accuracy.
4. Round spermatid injection (ROSI)
- Carry out the ROSI procedure using an inverted microscope with a micromanipulation system.
- In the initial preparation step, make holding and injection needles according to the previously described procedure21. Keep the inner diameter of the injection needle between 6-7 µm, designed for the extraction of round spermatids, and for the holding needle, have an inner diameter of 20 µm for securing the oocyte.
- In the subsequent preparation step, create an injection vessel by placing 10 µL of M2 droplets containing CB to soften oocytes and 10 µL of M2 droplets for storing round spermatids. Use PVP droplets to moisten and cleanse the injection needles.
NOTE: Adding CB here is not a necessary step, but adding CB can greatly improve the survival rate after injection. - Extract round spermatids using an injection needle.
- Rotate the oocyte with a holding needle, positioning the oocyte's polar body at either the 12 o'clock or 6 o'clock position.
- Place the injection needle carefully at the 3 o'clock position on the oocyte, tightly adhering to the zona pellucida. Use a PiezoXpert device to create a hole in the zona pellucida. Adjust the strength from small to large, which is approximately intensity = 5 and speed = 15 here.
- Gently advance the injection needle through the zona pellucida and enter the oocyte horizontally. When it passes the center of the oocyte, apply a piezo (intensity = 1 and speed = 1), resulting in the rupture of the oocyte membrane and the gradual injection of the round spermatid into the oocyte's cytoplasm.
- Withdraw the injection needle and aspirate a small amount of the oocyte's membrane near the opening to seal it. This step is crucial, as failure to seal would result in cytoplasmic leakage and oocyte death.
NOTE: It is worth noting that ROSI required AOA either before or after the injection of round spermatids, which we have discussed in subsequent sections.
5. Intracytoplasmic sperm injection (ICSI)
- Carry out the same steps for ICSI as for ROSI, with the only difference being the diameter of the ICSI injection needle, which measures 9-10 µm.
- Place spermatozoa on a PVP runway to reduce their swimming speed and facilitate sperm extraction.
- Perform separation of the spermatozoa head and tail for ICSI. Aspirate the spermatozoa from the tail and position the spermatozoa's neck precisely at the mouth of the injection needle. Apply a piezo (multiple piezo could be used as needed, intensity = 5 and speed = 15) to separate the head and tail of the spermatozoa.
6. Assisted oocyte activation (AOA)
- According to the protocol, prepare a CZB medium without calcium and magnesium.
- Use strontium chloride hexahydrate (SrCl26H2O), with a molecular weight of 266.62, at a concentration of 10 mM. To prepare it, dissolve 0.26662 g of SrCl26H2O in 1 mL of embryo water. At the time of use, add 10 µL of concentrated storage solution to 990 µL of Ca2+-free CZB medium and use immediately.
- Place the oocytes in the Ca2+-free CZB medium containing SrCl26H2O for activation; each droplet has a volume of 20 µL, and 20 oocytes are placed each time. Incubate for 20 min.
- Simultaneously, establish a group for parthenogenesis activation without injecting round spermatids or spermatozoa. It should be noted that the parthenogenesis activation group is shown without statistical analysis, and the control group is ICSI.
7. Embryo transfer
- House the ligated ICR male and female mice in a ratio of 1:2. The following morning, examine the female mice for the presence of a vaginal plug and select those with a vaginal plug for transplantation.
- Inject the transferred embryos consisting of 2-cell embryos the previous morning and transfer them the next afternoon.
- Make an incision on the back of the female mouse, expose the white fat and ovaries, and locate the enlarged part of the fallopian tube under an upright microscope (10x).
- Use a 1 mL syringe to create an opening in the enlarged part of the fallopian tube and aspirate the embryos through an oral pipette. Gently introduce the embryos in the direction of the uterus. Suture the wound, using 4 x 10 models of curved needles with thread, with a thickness of 5-0 (0.09-0.11 mm). The suture is made in two layers, with one layer for the peritoneum and one layer for the outer skin.
- For surrogate mice, perform cesarean sections based on the experimental schedule. Euthanize the mice by the cervical dislocation method, disinfect with alcohol, and open the abdominal cavity. Gently and quickly cut open the uterus and open the amniotic cavity to show the fetus and placenta. Remove the umbilical cord and cut from the side close to the fetus; the fetus was fed by the same period of breastfeeding mice.
8. Statistical analysis
- Use GraphPad Prism 5 to analyze. Data are expressed in mean ± SD; P < 0.05 indicates a statistical difference, and P < 0.01 indicates a significant statistical difference.
Representative Results
We initiated our investigation by examining AOA's effect on embryos' developmental capability. A schematic illustration of the experimental design is shown in Figure 1A. Before the spermatozoon injection, the oocytes underwent either AOA (A-ICSI) or remained untreated (ICSI). Detailed data on embryonic development is presented in Table 1. The results revealed no significant differences in cleavage, blastocyst, or birth rates between the A-ICSI and ICSI groups (P > 0.05; Figure 1B). These findings indicate that AOA using 10 mM SrCl2 for 20 min did not affect the developmental potential of the embryos.
It was previously reported that there were no discernible differences in the developmental efficiency of ROSI embryos selected either by FACS or by direct visual examination under a microscope22. Our experiments employed FACS technology to identify RS (Figures 2A,B). Under the microscope, mouse round spermatids were approximately 10 µm in diameter and displayed a protrusion-like nucleolus structure in the middle (Figure 2C). We posit that selection through FACS is more accurate than direct visual examination under a microscope. Additionally, the literature supports the direct exploration of RS through morphological differences. ROSI embryos were generated using two distinct methods: the A-ROSI group, where oocytes were subjected to AOA before the round spermatid injection, and the ROSI-A group, where oocytes were subjected to AOA after the round spermatid injection. The schematic diagram of the experimental design is shown in Figure 1C. Notably, no significant differences in the cleavage and blastocyst rates were found among the A-ROSI, ROSI-A, and ICSI groups (P > 0.05; Figure 1D). The blastocyst rates of the A-ROSI, ROSI-A, and ICSI groups were significantly higher than those of the activation group (P < 0.05; Figure 1D). However, the birth rate of the ROSI group was lower than that of the ICSI group, irrespective of whether the oocytes were activated before or after injection (P < 0.05; Figure 1D). Importantly, the birth rate of the A-ROSI group was slightly higher than that of the ROSI-A group (Figure 1D). Further details on embryo development data are presented in Table 1.
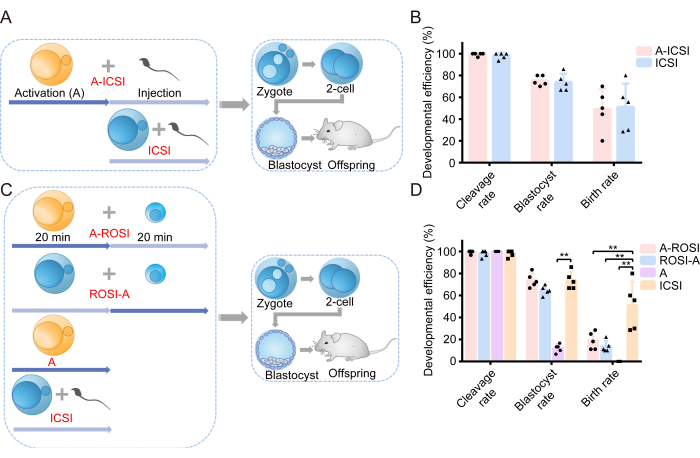
Figure 1: ROSI embryos displayed reduced developmental efficiency compared to ICSI embryos. (A) Schematic illustration of the experimental protocol assessing the effect of activation on ICSI embryonic development. Blue = Oocytes were not activated; Yellow = Oocytes were activated. (B) Developmental efficiency of embryos derived from A-ICSI and ICSI. (C) Schematic illustration of the experimental protocol for generating different types of embryos. (D) Developmental efficiency of embryos derived from A-ROSI, ROSI-A, A, and ICSI. **, P < 0.01. Abbreviations: A= Activation E= Embryonic day; ROSI= Round spermatid injection; ICSI= Intracytoplasmic sperm injection. The error bars show standard deviation. The comparison of rates is conducted using the chi-square test. Please click here to view a larger version of this figure.
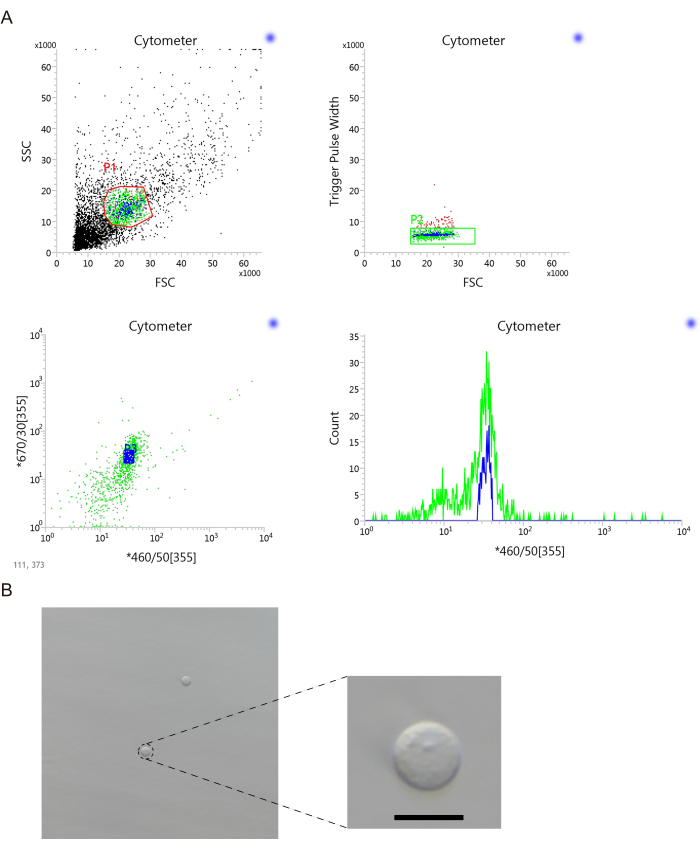
Figure 2: Round spermatids were selected via flow cytometric sorting. (A) A flow cytometric sorting diagram was utilized for the selection of round spermatids. (B) Representative images showcasing the selection of round spermatids. Scale bar: 10 µm. Abbreviations: FSC = Forward scatter; SSC = side scatter; 355 is the excitation wavelength; 460/50 and 670/30 are two detection channels under 355 wavelength laser. Please click here to view a larger version of this figure.
| Groups | Pre-implantation development | Post-implantation development | |||
| Replicates | Cleavage rate (%) | Blastocyst rate (%) | 2-cell embryos transferred/ No. of recipients | Birth rate (%) | |
| A-ICSI | 5 | 99.33 (149/150) | 75.17 (112/149) | 49/5 | 48.98 (24/49) |
| A-ROSI | 5 | 99.33 (149/150) | 73.83 (110/149) | 44/5 | 18.18 (8/44) ** |
| ROSI-A | 5 | 98.00 (147/150) | 64.63 (95/147) | 45/5 | 13.33 (6/45) ** |
| Activation | 5 | 100.00 (150/150) | 12.00 (18/150) ** | 51/5 | 0.00 (0/51) ** |
| ICSI | 5 | 98.00 (147/150) | 73.47 (108/147) | 46/5 | 52.17 (24/46) |
Table 1. The developmental efficiency of embryos derived from different groups.
Supplementary Table 1. The proportion of different cell populations sorted by flow cytometry.P3 part is round spermatids. Please click here to download this File.
Discussion
Assisted oocyte activation
A critical prerequisite for ROSI is AOA since round spermatids alone cannot initiate oocyte activation. Currently, the most established method in mice involves the use of strontium chloride23,24, while the most advanced human application employs electrical activation13,14. The timing of oocyte activation is also of great significance. As reported in the literature, the most optimal activation approach in mice involves initially activating the oocyte and then injecting the round spermatid25. This contrasts with the conventional fertilization process, where sperm initially enters the oocytes, subsequently releasing phospholipase C ζ to activate the oocyte26. Specialized research conducted by Satoshi Kishigami and colleagues emphasizes the differential ability of ROSI to form a male nucleus in pre- or post-activated oocytes. To achieve an efficient offspring production rate, both injection types must be carried out before the oocytes enter the G1 phase25.
The diameter of the injection needle
In the context of ROSI, it is important to note that a larger diameter of the injection needle does not necessarily translate to better outcomes. The injection needle used has a 6-7 µm diameter, slightly smaller than a round spermatid. Therefore, when a round spermatid is aspirated, the cell membrane is subjected to a squeezing effect, potentially leading to the direct exposure of the nucleus. This direct exposure may be conducive to depolymerization and the subsequent formation of the male pronucleus27.
Sealing treatment
Mouse oocytes exhibit less cytoplasmic viscosity compared to other species. Even a small breach in the cell membrane can cause the cytoplasm to flow out easily, resulting in oocyte degeneration28. To mitigate the risk, after injecting the round spermatid into the oocyte cytoplasm and withdrawing the injection needle, it is imperative to aspirate a small portion of the cell membrane near the opening of the oocyte cell membrane to seal the space, akin to the procedure in ICSI21. This sealing process significantly reduces the risk of oocyte degeneration.
Application of ROSI as a model
Beyond clinical applications, ROSI technology has various other applications as a model. It can expedite mouse generation times29, rescue female lethality resulting from a paternally inherited Xist deletion in mice17, generate mice after round spermatid injection into haploid parthenogenetic two-cell blastomeres15, generate transgenic mouse offspring16, and preserve fertility in adolescent children before cancer treatment30,31. Diligent research on mouse ROSI can substantially contribute to advancements in reproductive health research.
Limitations of the article
This article serves as a methodological guide with several limitations, including the absence of a direct comparative selection of RS under a microscope for injection and a perceived lack of innovation.
Divulgaciones
The authors have nothing to disclose.
Acknowledgements
We extend our gratitude to Wenjie Zhao for her invaluable assistance in sorting round spermatids through flow cytometry and to Fang Wang for her expertise in mouse embryo transfer. This work received partial support from the Natural Science Foundation of Jilin Province (No. YDZJ202301ZYTS461). We thank Bullet Edits Limited for the linguistic editing and proofreading of the manuscript.
Materials
| CaCl22H2O | Sigma | C7902 | Preparation of CZB |
| Glucose | Sigma | G6152 | Preparation of CZB |
| HEPES-Na (basic) | Sigma | H3784 | Preparation of CZB |
| Hoechst 33342 | Beyotime | C1025 | FACS |
| human chorionic gonadotropin (HCG) | Ningbo Second Hormone Company | HCG | Ovulation promoting drugs |
| Hyaluronidase | Sigma | H3506 | Removing granulosa cells around the oocyte |
| KCl | Sigma | P5405 | Preparation of CZB |
| KH2PO4 | Sigma | P5655 | Preparation of CZB |
| KSOMaa | Caisson Labs | IVL04-100ML | Potassium simplex optimized medium supplemented with amino acids |
| L-glutamine | Sigma | G8540 | Preparation of CZB |
| M2 | Sigma | M7167-50ML | Operating fluid |
| MgSO47H2O | Sigma | M1880 | Preparation of CZB |
| Na2-EDTA2H2O | Sigma | E5134 | Preparation of CZB |
| NaCl | Sigma | S5886 | Preparation of CZB |
| NaHCO3 | Sigma | S5761 | Preparation of CZB |
| Na-lactate 60% syrup d = 1.32 g/L | Sigma | L7900 | Preparation of CZB |
| Na-pyruvate | Sigma | P4562 | Preparation of CZB |
| Piezo drill tips (ICSI) | Eppendorf | piezoXpert | Piezoelectric membrane rupture |
| pregnant mare serum gonadotropin (PMSG) | Ningbo Second Hormone Company | PMSG | Ovulation promoting drugs |
| PVA | Sigma | P8136 | Preparation of CZB |
Referencias
- Redgrove, K. A., McLaughlin, E. A. The role of the immune response in Chlamydia trachomatis infection of the male genital tract: A double-edged sword. Front Immunol. 5, 534 (2014).
- Yanagimachi, R. Intracytoplasmic injection of spermatozoa and spermatogenic cells: Its biology and applications in humans and animals. Reprod Biomed Online. 10 (2), 247-288 (2005).
- Palermo, G., Joris, H., Devroey, P., Van Steirteghem, A. C. Pregnancies after intracytoplasmic injection of single spermatozoon into an oocyte. Lancet. 340 (8810), 17-18 (1992).
- Kimura, Y., Yanagimachi, R. Mouse oocytes injected with testicular spermatozoa or round spermatids can develop into normal offspring. Development. 121 (8), 2397-2405 (1995).
- Tesarik, J., et al. Spermatid injection into human oocytes. II. Clinical application in the treatment of infertility due to non-obstructive azoospermia. Human Reprod. 11 (4), 780-783 (1996).
- Tesarik, J., Mendoza, C. Spermatid injection into human oocytes. I. Laboratory techniques and special features of zygote development. Human Reprod. 11 (4), 772-779 (1996).
- Hirabayashi, M., et al. Activation regimens for full-term development of rabbit oocytes injected with round spermatids. Mol Reprod Dev. 76 (6), 573-579 (2009).
- Ogonuki, N., et al. Birth of a marmoset following injection of elongated spermatid from a prepubertal male. Mol Reprod Dev. 86 (8), 928-930 (2019).
- Niederberger, C., et al. Forty years of IVF. Fertil Steril. 110 (2), 185 (2018).
- Gross, K. X., Hanson, B. M., Hotaling, J. M. Round spermatid injection. Urol Clin North Am. 47 (2), 175-183 (2020).
- Hanson, B. M., et al. Round spermatid injection into human oocytes: a systematic review and meta-analysis. Asian J Androl. 23 (4), 363-369 (2021).
- Tekayev, M., Vuruskan, A. K. Clinical values and advances in round spermatid injection (ROSI). Reprod Biol. 21 (3), 100530 (2021).
- Tanaka, A., et al. Fourteen babies born after round spermatid injection into human oocytes. Proc Natl Acad Sci U S A. 112 (47), 14629-14634 (2015).
- Tanaka, A., et al. Ninety babies born after round spermatid injection into oocytes: survey of their development from fertilization to 2 years of age. Fertil Steril. 110 (3), 443-451 (2018).
- Yang, H., Shi, L., Chen, C. D., Li, J. Mice generated after round spermatid injection into haploid two-cell blastomeres. Cell Res. 21 (5), 854-858 (2011).
- Moreira, P., et al. Transgenic mouse offspring generated by ROSI. J Reprod Dev. 62 (1), 37-42 (2016).
- Federici, F., et al. Round spermatid injection rescues female lethality of a paternally inherited Xist deletion in mouse. PLoS Genet. 12 (10), e1006358 (2016).
- Sakamoto, M., et al. Paternally inherited H3K27me3 affects chromatin accessibility in mouse embryos produced by round spermatid injection. Development. 149 (18), 200696 (2022).
- Wang, J., et al. Single-cell multiomics sequencing reveals the reprogramming defects in embryos generated by round spermatid injection. Sci Adv. 8, (2022).
- Ward, M. A., Yanagimachi, R. Intracytoplasmic sperm injection in mice. Cold Spring Harb Protoc. 2018 (1), (2018).
- Yoshida, N., Perry, A. C. Piezo-actuated mouse intracytoplasmic sperm injection (ICSI). Nat Protoc. 2 (2), 296-304 (2007).
- Zhu, L., et al. FACS selection of valuable mutant mouse round spermatids and strain rescue via round spermatid injection. Zygote. 23 (3), 336-341 (2013).
- Kong, P., et al. Effects of the histone deacetylase inhibitor ‘Scriptaid’ on the developmental competence of mouse embryos generated through round spermatid injection. Hum Reprod. 32 (1), 76-87 (2017).
- Hosseini, S., Salehi, M. Tricostatin A-treated round spermatid enhances preimplantation embryo developmental competency following round spermatid injection in mice. Zygote. 30 (3), 373-379 (2022).
- Kishigami, S., Wakayama, S., Nguyen, V. T., Wakayama, T. Similar time restriction for intracytoplasmic sperm injection and round spermatid injection into activated oocytes for efficient offspring production. Biol Reprod. 70 (6), 1863-1869 (2004).
- Tao, Y. Oocyte activation during round spermatid injection: state of the art. Reprod Biomed Online. 45 (2), 211-218 (2022).
- Ogura, A., Ogonuki, N., Miki, H., Inoue, K. Microinsemination and nuclear transfer using male germ cells. Int Rev Cytol. 246, 189-229 (2005).
- Kimura, Y., Yanagimachi, R. Intracytoplasmic sperm injection in the mouse. Biol Reprod. 52 (4), 709-720 (1995).
- Ogonuki, N., et al. A high-speed congenic strategy using first-wave male germ cells. PLoS One. 4 (3), e4943 (2009).
- Abdelaal, O., et al. Fertility preservation for pediatric male cancer patients: illustrating contemporary and future options; a case report. Transl Androl Urol. 10 (1), 520-526 (2021).
- Eyni, H., et al. Advanced bioengineering of male germ stem cells to preserve fertility. J Tissue Eng. 12, (2021).

.
