CO2-Lasertonsillotomy Under Local Anesthesia in Adults
Summary
CO2-lasertonsillotomy under local anesthesia is an interesting alternative treatment method for tonsillectomy under general anesthesia for tonsil-related complaints in adults. This report presents a step-by-step protocol detailing the execution of CO2-lasertonsillotomy under local anesthesia.
Abstract
Tonsil-related complaints are very common among the adult population. Tonsillectomy under general anesthesia is currently the most performed surgical treatment in adults for such complaints. Unfortunately, tonsillectomy is an invasive treatment associated with a high complication rate and a long recovery time. Complications and a long recovery time are mostly related to removing the vascular and densely innervated capsule of the tonsils. Recently, CO2-lasertonsillotomy under local anesthesia has been demonstrated to be a viable alternative treatment for tonsil-related disease with a significantly shorter and less painful recovery period. The milder side-effect profile of CO2-lasertonsillotomy is likely related to leaving the tonsil capsule intact. The aim of the current report is to present a concise protocol detailing the execution of CO2-lasertonsillotomy under local anesthesia. This intervention has been performed successfully in our hospital in more than 1,000 patients and has been found to be safe and to be associated with a steep learning curve.
Introduction
Recurrent tonsil disease is a common health problem resulting in frequent visits to outpatient clinics, antimicrobial treatments, and missed work days1. Tonsillectomy2 is currently the most used surgical intervention for tonsil-related complaints in adults. During a tonsillectomy, the patient is brought under general anesthesia and the entire tonsil, including the tonsil capsule, is removed followed by diathermy coagulation of any bleeding sites. This intervention is rather invasive and associated with significant post-operative morbidity and a long, typically painful, recovery period3,4. An alternative to tonsillectomy is tonsillotomy, which is the partial intra-capsular removal of the tonsil tissue.
Both tonsillectomy and tonsillotomy have been performed for millennia 5,6. The first descriptions of subtotal tonsil removal date back to 1 BC6. Since that time many techniques for tonsil removal have been developed including the use of scalpels, microdebriders7, coblators8, electrosurgical scissors9, diode-lasers10, radiofrequency probes11 and CO2-lasers12.
CO2-lasertonsillotomy under local anesthesia (CO2LT) for the treatment of tonsil-related complaints is a fairly novel surgical treatment, which is gaining popularity as an alternative for the classic tonsillectomy. Recent studies have shown a shorter and less painful recovery period, but similar overall patient-satisfaction with CO2LT treatment when compared to conventional tonsillectomy12,13. During a CO2LT the tonsil is locally anesthetized and only the lobules of lymphatic tonsillar tissue are removed. The tonsillar capsule, through which blood vessels, nerves and lymphatic vessels pass, is left intact. Leaving the tonsillar-capsule intact likely leads to a reduced rate of post-operative bleeding, reduced post-operative pain, and a shorter recovery time14.
A potential problem with leaving the tonsillar capsule intact can be the incomplete resolution of the tonsil-related complaints, resulting in the need for a secondary CO2LT in a subset of patients12. Furthermore, to be eligible for CO2LT treatment patients must be able to remain calm during treatment and their gag reflex intensity should not limit treatment possibilities. The gag reflex is a physiological reflex to protect the airway15, which can only be partly blunted by local anesthesia in the mouth and pharynx; a particularly strong gag reflex can compromise the safe performance of a CO2LT. To assess the severity of the reflex the Gagging Severity Index (GSI) can be used15. The GSI is an index ranging from 1 (very mild) to 5 (very severe) [Table 1] and was originally developed in dentistry to classify the intensity of the gagging reflex and its consequences for dental treatments. In any patient with a GSI grade 3 or more the gagging reflex should first be reduced to increase the odds that the CO2LT procedure will be successful. We advise patients to try to fade out their gag-reflex by "brushing" their tongue-base and tonsils each time they brush their teeth. We have found this exercise to be capable of reducing the gag reflex intensity in most patients by 1-2 GSI points.
Protocol
1. Patient Selection
- Consider inclusion of patients with the following tonsil-related diseases: recurrent tonsillitis; dysphagia caused by large tonsils; tonsil stones; obstructive sleep apnea related to tonsils.
- Include only adult patients.
- Check for allergies, specifically to local anesthetics.
- Assess the gag-reflex intensity using the GSI (Table 1). For adequate CO2LT treatment, full visualization of the tonsils is required and patients need to be able to hold their breath for at least 15 s at a time.
- In patients with a GSI > 2 consider the following exercise to decrease the gag-reflex intensity.
- Inform the patient that the gag-reflex can be (partially) faded-out by training.
- Explain to the patient that the exercise will be uncomfortable in the first few days to weeks.
- Advise the patient to use their toothbrush to gently touch / brush their tongue base and tonsils each time they brush their teeth (preferably twice a day). Instruct the patient to increase pressure when performing this procedure each sequential day.
- Exclude the following patients: with Friedman grade IV (kissing) tonsils; with undertreated coagulation disorders; using any form of anticoagulants; with an active tonsil infection / peritonsillar abscess; women who are pregnant; those who are uncooperative during tonsil examination.
2. Informed Consent and Pre-operative Instruction Visit
- Obtain written informed consent including the following.
- Explain the intervention to the patient as follows: "The tonsil(s) will be partially evaporated using a laser beam. Local anesthesia will be used to numb the tissue and therefore you will be fully awake and mentally present during treatment. No pain is expected during treatment and low to moderate pain may occur in the first days after treatment. Treatment will take approximately 10-15 min per tonsil. If no complications occur, admission to the floor after treatment is not necessary and you will be able to leave the hospital in 30 min to an hour after treatment, accompanied by a friend or relative that is able to drive you."
- Explain alternative treatment options (where applicable: expectant management, conventional tonsillectomy or antibiotics).
- Explain possible complications of the CO2LT including: per- and post-operative bleeding, infection, incomplete resolution of tonsil disease; need for a second tonsillotomy or a tonsillectomy, pain, allergic reaction to anesthetic, temporary change of taste, (temporary) damage to surrounding structures.
- Instruct the patient not to eat any heavy meals on the day of treatment.
- Instruct the patient to take 1,000 mg acetaminophen (paracetamol) 30 min before treatment if acetaminophen is not contraindicated in that specific patient (including, but not limited to active liver disease and liver failure).
- Ask patients with a troublesome gag-reflex during examination to reduce the gag-reflex by rubbing their tongue base and tonsils with their toothbrush at least twice a day for 1 min, preferably for at least 2 weeks.
3. Preparation of Patient and Equipment
- Attach the laser pen to the CO2-laser machine.
- Make sure that the correct settings are chosen (Figure 1) such as (i) continuous laser beam, (ii) 15-30 W intensity depending on the size of the tonsil; generally, start at 18 W and increase the power up to 30 W depending on the size of the tonsils and patient's cooperation, (iii) shape-size of 2-4 mm depending on the size of the (remainder of the) tonsil, (iv) shape: round.
- Make sure that the surgeon, the surgical technologist, and the patient are wearing laser safety glasses.
- Make sure that the surgeon and the surgical technologist are wearing appropriate protective surgical masks.
- Confirm that the headlight for the surgeon is working.
- Confirm that a pulse oximeter for patient monitoring is present.
- Confirm that wooden tongue depressors are within reach.
CAUTION: Do not use metal depressors, since they can reflect the laser beam.
4. Time-out Procedure
- Ask the patient for their name and date of birth.
- Ask the patient for the intervention that will take place.
- Ask the patient for the side of treatment.
- Ask the patient for any allergies, specifically for local anesthetics and medications.
- Check with the surgical technologist if all equipment is present.
- Check if the laser-indication light of the operating room is switched on and all windows are covered for laser safety.
5. Patient Instructions Before Surgery
- Ask the patient to inhale deeply, followed by breathing out slowly during treatment.
- Explain to the patient that he/she is in control and can signal at any time, which will lead to a pause of the laser-treatment.
- Instruct the patient to use his/her hand to signal if they wish to pause treatment by tapping the surgeon’s leg.
- Instruct the patient not to swallow any liquids during treatment to prevent aspiration and laryngospasms. Provide a kidney basin to the patient to spit any liquids into when necessary.
- Reassure the patient not to panic if they experience a feeling as if their airway is blocked, as this is due to local anesthesia of the pharynx region. Remind the patient again that the treatment can be paused at any moment.
6. Positioning the Patient and Inspection of the Tonsils
- Place the pulse oximeter on the patient's index finger and confirm that it is functioning correctly.
- Position the patient in an upright position using the chair / table controls.
- Set the height of the chair / table so that the surgeon can stand straight comfortably while performing the laser treatment.
- Ask the patient to make any adjustments to the seating to ensure comfortable and safe positioning.
- Inspect both tonsils and exclude active inflammation.
- Assess the gag-reflex using the GSI and judge the feasibility of the laser treatment. For adequate CO2LT treatment, the surgeon should be able to fully visualize the tonsils and patients need to be able to hold their breath for at least 15 s.
7. Anesthesia of the Tonsil
- Tell the patient that the tonsils will be anesthetized one at a time.
- In case of a significant gag-reflex (GSI grade 2-3) use xylocaine-spray or superficial anesthesia of the tongue-base and pharynx to reduce the gag-reflex.
- Take an ampule with local anesthetic and inject ~0.2 mL slowly into the upper pole, ~0.2 mL into the mid-pole and 0.2 mL into the lower-pole of the tonsil.
NOTE: Optionally, the tonsil-pillars can be infiltrated as well. This is recommended when the tonsils are hidden behind the pillars or to decrease the gag-reflex. - Instruct the patient not to swallow any local anesthetic, but to spit it out.
- Reassure the patient that any feeling of throat tightness is due to the anesthetic; not due to any actual obstruction.
8. Laser-treatment of the Tonsil
- Ask the patient to breathe in deeply and exhale slowly.
- Have the surgical technologist hold the smoke suction close to the opening of the mouth, without blocking the surgeon's view.
- Use two wooden tongue blades to depress the tongue / tongue-base and expose the tonsil.
- During the patient’s exhalation, laser the lymphatic tissue of the lobules in a sweeping motion.
- Stop when the patient taps your (the surgeon's) leg.
- Let the patient catch his/her breath again and repeat steps 8.1–8.4 until complete cryptolysis is accomplished.
- If necessary, inject extra local anesthetic (with or without epinephrine).
9. Tips for Laser Treatment
- In case of peroperative hemorrhage: laser the spot that is bleeding "out of focus". This will lead to burning of the lymphatic tissue with crust formation with a similar effect as coagulation (opposed to evaporation when using the laser 'in focus'). Alternatively, use a (bipolar) coagulation device to stop the bleeding.
- Use the wooden tongue blades to press against the anterior tonsillar pillar to expose the tonsil further.
- Use the wooden tongue blades to press against the upper part of the tonsil pillars to expose the upper lobule of the tonsil.
- Use the wooden tongue blades to scoop up the lower tonsil lobule and expose it for laser treatment (one can leave them scooped up on the tongue blades).
10. Instructions After Treatment
- Give the patient a popsicle for a minimum of 30 min of postoperative observation.
- Instruct the patient not to drink or eat anything else for 2 h until the local anesthetic has worn off to prevent aspiration.
- Instruct the patient not to drink / eat hot (temperature) or spicy drinks/food or food with hard crusts for a week to prevent postoperative bleeding.
- Tell the patient to take pain medication only if necessary.
NOTE: We advise a maximum of 1,000 mg acetaminophen (paracetamol) 4 times a day, if necessary. - Tell the patient to refrain from strenuous physical exercise for a week.
- Advise the patient to go to the nearest emergency department in case a postoperative bleeding occurs. Advise the patient to contact the ENT department in case of a postoperative infection (e.g., fever).
Representative Results
In a previously published prospective study in 107 patients with one year follow-up, postoperative questionnaires were used to assess recovery rate and recurrence of tonsil-related symptoms for CO2LT compared to conventional tonsillectomy12. Forty-six patients underwent conventional tonsillectomy under general anesthesia and 61 patients underwent CO2LT. In total, 72.5% of patients in the CO2LT group were cured from their tonsil-related symptoms. Three patients (7.5%) in the CO2LT group required revision surgery for recurring tonsil complaints. In the tonsillectomy group, 97.2% of patients were cured after initial treatment. The overall satisfaction rate was similar in both treatment groups, but the mean pain intensity scores two weeks post-operatively were 5.4 (out of 10, range 0-9) after tonsillotomy and 7.7 (out of 10, range 2-10) after tonsillectomy leading to longer (9.9 vs. 5.4) use and use of stronger pain medication (NSAIDs / opioids versus acetaminophen) after tonsillectomy. Days to full recovery and number of post-operative bleeding events were both significantly higher in the tonsillectomy group (Figure 2).
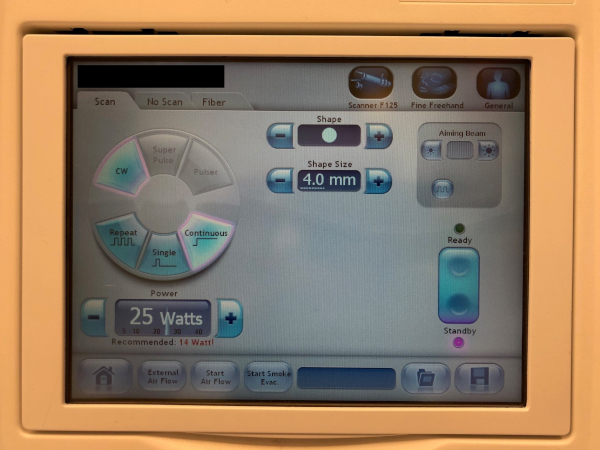
Figure 1: Photo of laser settings. Standard laser settings for CO2LT on the laser system used. Please click here to view a larger version of this figure.
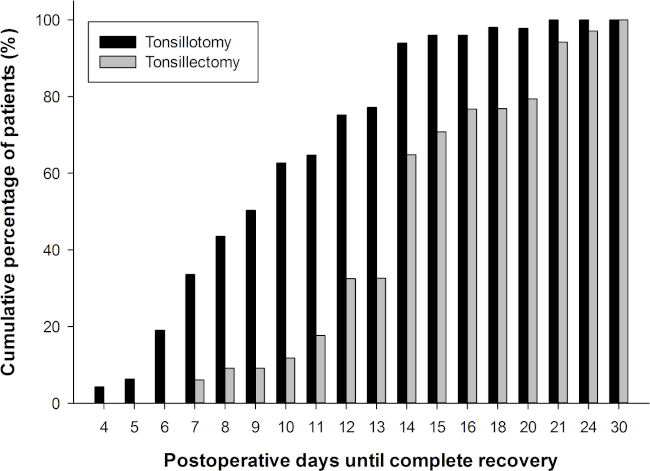
Figure 2: Patient reported recovery after tonsillotomy and tonsillectomy. Cumulative percentage of patients that reported complete recovery postoperatively after tonsillotomy (TO) and tonsillectomy (TE). Data were previously published by Lourijssen et al.12. Please click here to view a larger version of this figure.
| Dickinson and Fiske | Definition and characteristics of grade of reflex |
| Gagging Severity Index grades | |
| Grade I | Very mild, occasional and controlled by the patient. |
| Grade 2 | Moderate, control is required by the patient |
| with reassurance from the dental team. | |
| Grade 3 | Moderate, consistent and limits treatment options. |
| Grade 4 | Severe and treatment is impossible. |
| Grade 5 | Very severe, affecting patient behavior |
| and dental attendance and making treatment impossible. |
Table 1: Gagging Severity Index (GSI) score15.
Discussion
This paper describes the steps to perform a CO2LT. To our knowledge, this is the first article to describe this intervention in such detail. Outpatient CO2LT under local anesthesia is a novel surgical method and therefore the presented procedural details have mostly been developed through hands-on experience of the authors.
As for any surgical intervention, pre-operative patient selection is important. For CO2LT, a relatively calm and cooperative patient without a procedure-restricting gag-reflex is desirable. Therefore, an adequate assessment of limitations due to patient anxiety pertaining to the procedure and gag-reflex are of great importance to reach consistent treatment effects. Furthermore, we advise not to perform CO2LT on patients with grade IV (Friedman grading), or “kissing-tonsils” because of the risks of damaging surrounding tissues with the laser-beam.
In our experience, leaving the tonsil capsule intact and limiting the tissue damage reduces post-operative pain, recovery time and post-operative morbidity compared to tonsillectomy under general anesthesia. This is in agreement with current literature16,17,18,19,20,21,22,23,24,25,26. Despite the potential incomplete resolution of tonsil disease with CO2LT, many patients prefer CO2LT over tonsillectomy when informed of their options. This preference has been consistently reported prospectively (pre-surgery) and retrospectively (at follow-up)12. We therefore believe that CO2LT fills a gap in treatment options for tonsil-related disease, both from the doctors' and the patients' perspective. Current ongoing studies should provide further insight into the value of CO2LT in adults with tonsil diseases13.
There is a wide variety of techniques and devices available to perform a tonsillotomy, each with its own potential pros and cons. Utilized surgical devices besides the CO2-laser include microdebriders, coblators, surgical scissors, radiofrequency ablation probes, interstitial thermal therapy instruments and diode lasers. There is no conclusive evidence favoring any one instrument over another for tonsillotomy in adults27. Microdebriders, coblators and CO2-lasers are among the most frequently used instruments for tonsillotomy28. Reports on effectiveness, pain and postoperative complications vary, but current evidence suggests equal efficacy of tonsillotomy compared to tonsillectomy with less postoperative pain and complications27,28, independent of the method of tonsillotomy.
Even though tonsil-surgery under local anesthesia has been described since decades, it is not performed often in current practice16,29,30,31. Many otolaryngologists are uncomfortable with the idea of tonsil surgery under local anesthesia. This may partly be due to a lack of experience with this specific form of tonsil surgery as well as due to concerns over the airway and bleeding control30.
CO2LT has some clear logistical advantages. First, using only local anesthetics obviates the need for an anesthesia team. Second, the operation can be performed in the outpatient setting and there is no need for an operation room. Third, the surgical instruments used with CO2LT are non-disposable and only the laser pen needs to be sterilized after use. Sterilization of the laser pen is a simple procedure for any central sterile services department. These factors all lead to cost-reduction. On the other hand, the use of a laser requires a specialized intervention room meeting the local laser safety standards.
We currently exclude patients with a history of peritonsillar abscess because of the intrinsic risk in those patients of recurrent peritonsillar abscess (14%)32. The risk of recurrence is zero in patients after tonsillectomy33. In tonsillotomy, residual tissue may lead to a recurrence of an abscess. We also advise to exclude patients on anticoagulants or with bleeding disorders from treatment with CO2LT. Even though our experience is that bleeding sites can easily be managed with the CO2-laser, or if necessary, with bipolar coagulation. The fact that the patient is conscious and not intubated might complicate per-operative treatment of more profound bleeding due to decreased coagulation. If necessary, the patient can be brought under full anesthesia and the bleeding site can be stopped with diathermy or ligation, similar to postoperative bleeding after tonsillectomy. In our >1,000 patient experience, such an event has never occurred. We estimate the need to use bipolar coagulation under local anesthesia to be around 2% of cases.
Furthermore, as of yet we have never had to stop a CO2LT case early due to an uncooperative patient. Incidentally a strong gag-reflex has led to suboptimal laser-treatment of the lower part of the tonsil. In those cases, sending the patient home with our gag-reflex training scheme led to successful treatment of the remaining tonsil tissue during a subsequent CO2LT procedure. It is important to note that these numbers and procedural characteristics are based on personal experience of the authors at a single center and should be evaluated in further studies.
Divulgations
The authors have nothing to disclose.
Acknowledgements
None.
Materials
| Carpule syringe and local anesthetic (eg xylocaïne:adrenaline 1:80.000) | n/a | n/a | n/a |
| CO2 Laser system | Lumenis | AcuPulse DUO CO2 laser | F125 CO2 Laser System |
| Coagulation device | Erbe | Erbe ICC 80 Surgical Generator With Footswitch | n/a |
| Laser safety goggles | Lumenis | Laservision goggles AX0000068 | n/a |
| Operating chair | n/a | n/a | With possibilities for the patient to sit upright (eg opthalmic chair or dental chair) |
| Operating room which meets the local laser-safety standards | n/a | n/a | n/a |
| Suction device | TBH | TBH LN 100 or 2000 | Air suction and filtration device |
| Surgical masks | 3M | 3M 7502 mask with 2138 P3 filters | n/a |
| wooden tongue depressor | n/a | n/a | Do not use metal tongue depressors |
References
- Koskenkorva, T., Koivunen, P., Alho, O. -. P. Predictive Factors for Medical Consultation for Sore Throat in Adults with Recurrent Pharyngotonsillitis. International Journal of Otolaryngology. 2016, 6095689 (2016).
- Cullen, K. A., Hall, M. J., Golosinskiy, A. Ambulatory surgery in the United States, 2006. National Health Statistics Reports. (11), 1-25 (2009).
- Bhattacharyya, N., Kepnes, L. J. Revisits and postoperative hemorrhage after adult tonsillectomy. The Laryngoscope. 124 (7), 1554-1556 (2014).
- Salonen, A., Kokki, H., Nuutinen, J. Recovery After Tonsillectomy in Adults: A Three-Week Follow-up Study. The Laryngoscope. 112 (1), 94-98 (2002).
- Younis, R. T., Lazar, R. H. History and current practice of tonsillectomy. The Laryngoscope. 112 (8), 3-5 (2002).
- Koempel, J. A., Solares, C. A., Koltai, P. J. The evolution of tonsil surgery and rethinking the surgical approach to obstructive sleep-disordered breathing in children. The Journal of Laryngology and Otology. 120 (12), 993-1000 (2006).
- Koltai, P. J., Solares, C. A., Mascha, E. J., Xu, M. Intracapsular partial tonsillectomy for tonsillar hypertrophy in children. The Laryngoscope. 112 (8), 17-19 (2002).
- Arya, A., Donne, A. J., Nigam, A. Double-blind randomized controlled study of coblation tonsillotomy versus coblation tonsillectomy on postoperative pain. Clinical Otolaryngology and Allied Sciences. 28 (6), 503-506 (2003).
- Isaacson, G., Szeremeta, W. Pediatric tonsillectomy with bipolar electrosurgical scissors. American Journal of Otolaryngology. 19 (5), 291-295 (1998).
- D’Eredità, R., Marsh, R. R. Contact diode laser tonsillectomy in children. Otolaryngology–Head and Neck Surgery: Official Journal of American Academy of Otolaryngology-Head and Neck Surgery. 131 (5), 732-735 (2004).
- Hegazy, H. M., Albirmawy, O. A., Kaka, A. H., Behiry, A. S. Pilot comparison between potassium titanyl phosphate laser and bipolar radiofrequency in paediatric tonsillectomy. The Journal of Laryngology and Otology. 122 (4), 369-373 (2008).
- Lourijsen, E. S., Wong Chung, J. E. R. E., Koopman, J. P., Blom, H. M. Post-operative morbidity and 1-year outcomes in CO2-laser tonsillotomy versus dissection tonsillectomy. Acta Oto-Laryngologica. 136 (10), 983-990 (2016).
- Hultcrantz, E., Ericsson, E. Pediatric tonsillotomy with the radiofrequency technique: less morbidity and pain. The Laryngoscope. 114 (5), 871-877 (2004).
- Dickinson, C. M., Fiske, J. A review of gagging problems in dentistry: I. Aetiology and classification. Dental Update. 32 (1), 26-32 (2005).
- Krespi, Y. P., Ling, E. H. Laser-assisted serial tonsillectomy. The Journal of otolaryngology. 23 (5), 325-327 (1994).
- Unkel, C., Lehnerdt, G., Schmitz, K. J., Jahnke, K. Laser-tonsillotomy for treatment of obstructive tonsillar hyperplasia in early childhood: a retrospective review. International Journal of Pediatric Otorhinolaryngology. 69 (12), 1615-1620 (2005).
- Papaspyrou, G., Linxweiler, M., Knöbber, D., Schick, B., Al Kadah, B. Laser CO2 tonsillotomy versus argon plasma coagulation (APC) tonsillotomy: A retrospective study with 10-year follow-up. International Journal of Pediatric Otorhinolaryngology. 92, 56-60 (2017).
- Linder, A., Markström, A., Hultcrantz, E. Using the carbon dioxide laser for tonsillotomy in children. International Journal of Pediatric Otorhinolaryngology. 50 (1), 31-36 (1999).
- Baharudin, A., Shahid, H., Rhendra, M. Z. Laser tonsillotomy in children with tonsillar hyperplasia. The Medical journal of Malaysia. 61 (3), 377-379 (2006).
- Linder, A., Markström, A., Hultcrantz, E. Using the carbon dioxide laser for tonsillotomy in children. International Journal of Pediatric Otorhinolaryngology. 50 (1), 31-36 (1999).
- Magdy, E. A., Elwany, S., El-Daly, A. S., Abdel-Hadi, M., Morshedy, M. A. Coblation tonsillectomy: a prospective, double-blind, randomised, clinical and histopathological comparison with dissection-ligation, monopolar electrocautery and laser tonsillectomies. J Laryngol Otol. , (2008).
- Densert, O., Desai, H., Eliasson, A., Frederiksen, L., Andersson, D., Olaison, J., Widmark, C. Olaison Tonsillotomy in Children with Tonsillar Hypertrophy. Acta Oto-Laryngologica. 121 (7), 854-858 (2001).
- Krespi, Y. P., Kizhner, V. Laser tonsil cryptolysis: In-office 500 cases review. American Journal of Otolaryngology. 34 (5), 420-424 (2013).
- Stelter, K., de la Chaux, R., Patscheider, M., Olzowy, B. Double-blind, randomised, controlled study of post-operative pain in children undergoing radiofrequency tonsillotomy versus laser tonsillotomy. The Journal of Laryngology & Otology. 124 (8), 880-885 (2010).
- Hultcrantz, E., Linder, A., Markström, A. Tonsillectomy or tonsillotomy?–A randomized study comparing postoperative pain and long-term effects. International Journal of Pediatric Otorhinolaryngology. 51 (3), 171-176 (1999).
- Wong Chung, J. E. R. E., van Benthem, P. P. G., Blom, H. M. Tonsillotomy versus tonsillectomy in adults suffering from tonsil-related afflictions: a systematic review. Acta Oto-Laryngologica. 138 (5), 492-501 (2018).
- Windfuhr, J. P., Savva, K., Dahm, J. D., Werner, J. A. Tonsillotomy: facts and fiction. European archives of oto-rhino-laryngology: official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS): affiliated with the German Society for Oto-Rhino-Laryngology – Head and Neck Surgery. 272 (4), 949-969 (2015).
- Schoem, S. R., Watkins, G. L., Kuhn, J. J., Alburger, J. F., Kim, K. Z., Thompson, D. H. Control of Early Postoperative Pain With Bupivacaine in Adult Local Tonsillectomy. Archives of Otolaryngology-Head & Neck Surgery. 119 (3), 292-293 (1993).
- Bredenkamp, J. K., Abemayor, E., Wackym, P. A., Ward, P. H. Tonsillectomy under local anesthesia: A safe and effective alternative. American Journal of Otolaryngology. 11 (1), 18-22 (1990).
- Pekkarinen, H., Kärjä, J. Results of long-term ECG monitoring in patients submitting to tonsillectomy under local anaesthesia. The Journal of Laryngology and Otology. 96 (8), 725-730 (1982).
- Chung, J. H., Lee, Y. C., Shin, S. Y., Eun, Y. G. Risk factors for recurrence of peritonsillar abscess. The Journal of Laryngology and Otology. 128 (12), 1084-1088 (2014).
- Kronenberg, J., Wolf, M., Leventon, G. Peritonsillar abscess: recurrence rate and the indication for tonsillectomy. American Journal of Otolaryngology. 8 (2), 82-84 (1987).

