Enrichment and Detection of Clostridium perfringens Toxinotypes in Retail Food Samples
Summary
The objective of this protocol is to detect different Clostridium perfringens toxinotypes in locally purchased foods, particularly epsilon toxin producing strain types B and D, without the use of anaerobic chambers.
Abstract
Clostridium perfringens (C. perfringens) is a prolific toxin producer and causes a wide range of diseases in various hosts. C. perfringens is categorized into five different toxinotypes, A through E, based on the carriage of four major toxin genes. The prevalence and distribution of these various toxinotypes is understudied, especially their pervasiveness in American retail food. Of particular interest to us are the type B and D strains, which produce epsilon toxin, an extremely lethal toxin suggested to be the environmental trigger of multiple sclerosis in humans. To evaluate the presence of different C. perfringens toxinotypes in various food samples, we developed an easy method to selectively culture these bacteria without the use of an anaerobic container system only involving three culturing steps. Food is purchased from local grocery stores and transported to the laboratory under ambient conditions. Samples are minced and inoculated into modified rapid perfringens media (RPM) and incubated overnight at 37 °C in a sealed, airtight conical tube. Overnight cultures are inoculated onto a bottom layer of solid Tryptose Sulfite Cycloserine (TSC) agar, and then overlaid with a top layer of molten TSC agar, creating a "sandwiched", anaerobic environment. Agar plates are incubated overnight at 37 °C and then evaluated for appearance of black, sulfite-reducing colonies. C. perfringens-suspected colonies are removed from the TSC agar using sterile eye droppers, and inoculated into RPM and sub-cultured overnight at 37 °C in an airtight conical tube. DNA is extracted from the RPM subculture, and then analyzed for the presence of C. perfringens toxin genes via polymerase chain reaction (PCR). Depending on the type of food sampled, typically 15–20% of samples test positive for C. perfringens.
Introduction
Clostridium perfringens (C. perfringens) is a Gram positive, anaerobic, spore-forming, rod shaped bacterium that is found ubiquitously in the environment. This species of bacteria carries genes that encode for over 17 toxins and, historically, has been characterized into five toxinotypes (A-E) based on the presence of four different toxin genes: alpha, beta, epsilon, and iota toxin (Table 1)1. Recently, it has been suggested that this typing-scheme needs to be expanded to include types F and G, which harbor the C. perfringens enterotoxin (CPE) and NetB toxin, respectively2. However, more research is needed before this scheming system is formally accepted. While the alpha toxin gene is strictly chromosomally located, the CPE gene can be found both on the chromosome and plasmids. In comparison, the remaining toxins' genes are found on various differently-sized plasmids. We are particularly interested in the prevalence of C. perfringens types B and D as these strains produce epsilon toxin, an extremely potent, pore-forming toxin, which has been suggested to play a role in triggering multiple sclerosis (MS) in humans3,4,5,6,7. How people become infected or colonized by these strains is unknown. One possible explanation is through consumption of contaminated food products. To help answer this question, we sought to determine the prevalence of different C. perfringens toxinotypes in American food samples.
The presence of C. perfringens toxinotypes in American food samples is understudied and often requires use of anaerobic container systems and numerous sub-culturing steps8,9,10,11. Although numerous sub-culturing steps are needed to obtain purified isolates, this method can lead to loss of plasmids over time12,13,14, possibly affecting the detection of plasmid-borne toxin genes including the epsilon toxin gene. We sought to develop an easy method, with fewer sub-culturing steps, to selectively culture C. perfringens without the use of anaerobic chambers, jars, or bags. Briefly, food samples are inoculated into Rapid Perfringens Media (RPM) overnight (ON), then "sandwiched" into TSC agar and incubated ON. Colonies suspected to be C. perfringens are then sub-cultured into RPM and incubated again ON. DNA is extracted and PCR performed to determine genotype (Figure 1). We chose to use RPM as it has been demonstrated to increase the recovery of C. perfringens strains from food samples compared to other more standard media15. In addition, RPM was successfully used to isolate an epsilon toxin producing type B strain from an MS patient4. We use a modified version of RPM instead of the original version to allow easy DNA extraction. While this method allows easy identification of toxin genes within samples, it is possible that an individual sample will contain more than one C. perfringens toxinotype. Because our method does not isolate purified strains using multiple rounds of purification, identification of multiple toxinotypes from one sample is not possible. However, standard purification techniques (typically streaking onto TSC plates or blood agar plates) can be applied at the end of our protocol to achieve purified cultures.
Protocol
NOTE: C. perfringens is considered a biosafety hazard level 2 (BSL2) organism. Although not all food samples will contain C. perfringens, all cultured samples should be treated as such. All proper precautions and personnel protective equipment (PPE) should be worn at all times. Decontaminate all material prior to disposal.
1. Prepare modified RPM4,15
- Combine 30 g/L fluid thioglycolate medium, 60 g/L gelatin, 5 g/L peptone, 5 g/L glucose, 5 g/L potassium phosphate dibasic, 3 g/L yeast extract, 1.5 g/L sodium chloride, 0.5 g/L ferrous sulfate in deionized water until evenly dispersed. We typically make 1 L batches.
- Autoclave at 121 °C for 15 min.
- Allow to cool to approximately 40 °C.
- Once RPM is cool, add D-cycloserine to a final concentration of 440 mg/L.
NOTE: Stock concentrations of D-cycloserine dissolved in sterile water at 50 mg/mL may be stored at -20 °C for future use. - Aseptically transfer 10 mL of RPM to 15 mL conical tubes. RPM can be prepared in batches and stored at 4 °C for up to one month.
- Warm RPM to 37 °C prior to use.
2. Sample collection and RPM incubation
- Transport food to the laboratory under ambient temperatures within 1 h. Food may be transported in original packaging or sterile containers. If not testing immediately, food may be stored at -20 °C until use. Make note of the type of food and the country of origin according to the packaging label, if available, as well as any other relevant information.
- Remove approximately 1.0–2.0 g of food and transfer to sterile Petri dish or equivalent. Finely mince with a sterile razor blade or scalpel.
- Inoculate into 10 mL of phosphate buffered saline (PBS) in a 15 mL conical tube. Mix well.
- To select for vegetative cells, transfer 5 mL of the PBS-food mixture into a 15 mL conical tube containing 10 mL of RPM. Secure the lid tightly.
- To select for spores, heat the remaining 5 mL of PBS-food mixture at 85 °C for 15 min and then transfer to a 15 mL conical tube containing 10 mL of RPM. Secure the lid tightly.
- Vortex and invert the food-RPM cultures to ensure complete mixing.
- Tightly seal the conical tubes and wrap lids with paraffin film or plastic wrap to ensure an anaerobic environment.
- Incubate overnight (ON) at 37 °C.
- The following morning note any turbidity or fermentation in RPM tubes.
3. TSC "sandwich" plating
- Inoculate ON RPM cultures into TSC agar using a “sandwich” technique (Figure 2) described below.
- Prepare TSC agar as per the manufacturer's instructions.
- Prepare the base layer of the TSC plates by transferring 10 mL of molten TSC agar to sterile Petri dishes and allow to solidify. These may be prepared in advanced and stored at 4 °C. Ensure plates are warmed to room temperature prior to use.
- For the top layer of the TSC plate, maintain the remaining molten TSC agar at 40 °C.
NOTE: Although agar's melting point is above 85 °C, molten agar solidifies around 32–45 °C.
- Carefully retrieve the ON RPM cultures and transfer 100 µL to the TSC agar base. Because of fermentation, some cultures may be under pressure. Be sure to wear all appropriate PPE.
- Spread the RPM inoculum using sterilized glass beads or cell spreader.
- Allow RPM to be "absorbed" into TSC agar for 5–10 min at room temperature.
- Carefully transfer 20 mL of molten, 40 °C TSC agar to plate using a serological pipette.
- Replace the Petri dish lid and allow TSC agar to completely solidify at room temperature.
- Invert the Petri dish and incubate at 37 °C ON.
- If serial dilutions are desired, perform dilutions of the ON RPM cultures into fresh, pre-warmed RPM prior to inoculation into TSC agar.
4. Sub-culturing of sulfite-reducing colonies
- The following morning, remove plates from incubator and examine for bacterial growth. Aerobic bacteria may be present on the surface of the agar. Anaerobic bacteria will be found growing embedded within the agar. Sulfite-reducing bacteria will turn surrounding agar black. Possible C. perfringens colonies will be black and embedded in the agar.
- C. perfringens suspected colonies will be positive for sulfite reduction and will appear black, embedded within the agar. Using a sterile, single-use eyedropper, "pluck" the black colonies from the agar and transfer to 10 mL of fresh RPM in a 15 mL conical tube. It is important that the air from the eyedropper be expelled prior to piercing agar.
- If there is a dense amount of aerobic bacterial growth on the surface of the plate, use a sterile cell scraper to remove colonies from selected areas. Multiple C. perfringens suspected colonies can be sampled from the same TSC plate into separate RPM cultures.
- Tightly secure conical tube lids and wrap in paraffin film or plastic wrap. Incubate ON at 37 °C.
5. DNA Extraction
- Remove ON RPM cultures and examine for signs of growth including turbidity and fermentation.
- Gently invert RPM culture to disperse any settled bacteria and carefully open. Transfer 1 mL of the culture to a microcentrifuge tube.
- Centrifuge at top speed (approximately 15,000 x g) for 10 min to pellet bacteria.
- Wash pellet with 1 mL of sterile PBS.
- In some circumstances, undigested gelatin will settle on top of pelleted bacteria. To remove gelatin, "fluff" off gelatin by gently agitating with PBS using a micropipette. This will "fluff-up" the gelatin while leaving the bacterial pellet intact.
- Remove the PBS-gelatin mixture with gentle aspiration. Re-suspend the remaining bacterial pellet with 1 mL of fresh PBS.
- Centrifuge the resuspended bacterial pellet at top speed for 10 min and carefully aspirate the supernatant.
- Immediately perform DNA extraction using a DNA extraction kit and a protocol specifically created for extraction DNA from Gram-positive bacteria (see the Table of Materials).
- Use the extracted DNA immediately or store at -20 °C until PCR analysis.
6. Detection of C. perfringens via PCR genotyping
- To determine if cultures are positive for C. perfringens toxinotypes, examine extracted DNA for different toxin genes via PCR.
NOTE: Because we are most interested in the epsilon toxin producing strains type B and D C. perfringens, we evaluate for the presence of the alpha, beta, and epsilon toxin genes. Primers are listed in Table 2. Primers for 16s ribosomal DNA are used as a DNA extraction control. Additional primers can be used to test for toxinotypes A through G and can be found in published literature2,12,13. - Use previously extracted C. perfringens DNA as a positive control. This control ensures that all components of the PCR reactions are working. We use DNA extracted from C. perfringens type B (ATCC 3626) as our positive control. Grow ATCC 3636 ON in RPM at 37 °C and extract DNA using the same methods described in steps 5.1–5.7. Store extracted DNA at -20 °C until use.
- Set PCR conditions as follows: 94.0 °C for 3 min; 94.0 °C for 30 s; 47.9 °C for 30 s, 72.0 °C for 1 min (Repeat steps 2–4 for 35 cycles); 72.0 °C for 10 min.
- To confirm PCR products, run PCR reactions on a 1.8 g/100 mL agarose gel using standard techniques. Expected PCR product sizes are listed in Table 2. Typical PCR results are displayed in Figure 3.
Representative Results
Using this method, 15–20% of our sampled foods test positive for C. perfringens. While most strains are positive for toxinotype A, we have successfully detected both Type B and D in food samples. In a previously published paper we tested a total of 216 food samples purchased from New York retail stores16 (Table 3). These samples included various meat samples (beef, lamb, pork and lamb), poultry samples (chicken and turkey), and seafood samples (cod, salmon, shellfish, snapper, flounder, squid, tilapia, tuna, and various other fishes). Produce and dairy samples were also tested. Of 216 samples, 34 (16%) were positive for C. perfringens. Of the 34 C. perfringens positive samples, 31 samples (91.2%) contained the alpha toxin, one sample (2.9%) contained the alpha, beta and epsilon toxin, and two samples (5.9%) contained the alpha and epsilon toxin.
Interestingly, we also discovered that C. perfringens was more prevalent as vegetative cells compared to spores. Twenty-five samples were compared for the presence of vegetative C. perfringens cells or spores. Spores were selected for by heat shocking samples at 85 °C for 15 min. Of the 25 samples tested, 16% were positive for vegetative C. perfringens strains versus 4% for spores. This indicates that it may be more cost effective to test for only vegetative cells instead of both.
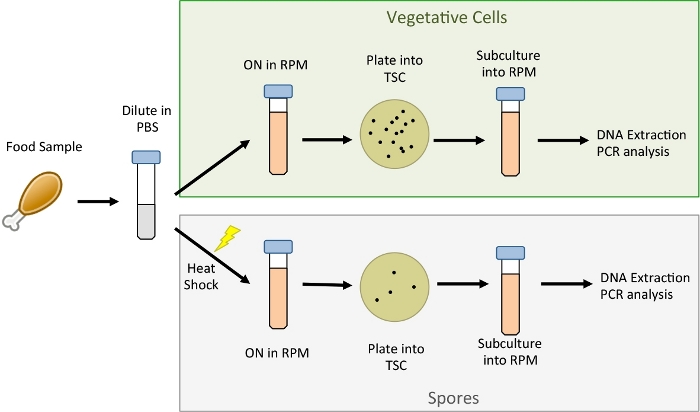
Figure 1: Overview of procedure.
Food samples are minced and diluted into sterile PBS. Half of the PBS-food sample is inoculated into RPM to select for vegetative cells. The remaining PBS-food sample is heat shocked at 85 °C for 15 min to select for spores prior to inoculation in RPM. Cultures are incubated ON at 37 °C then plated into TSC agar. TSC agar is incubated ON at 37 °C and black, sulfite-reducing cultures are sub-cultured into fresh RPM. Sub-cultured RPM cultures are incubated ON at 37 °C and DNA is extracted to perform genotyping via PCR. Please click here to view a larger version of this figure.
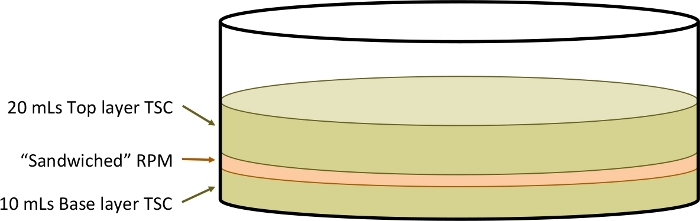
Figure 2: Schematic of TSC agar sandwich technique.
RPM media containing the C. perfringens bacteria are plated between two layers of TSC agar in order to promote an anaerobic environment. Please click here to view a larger version of this figure.
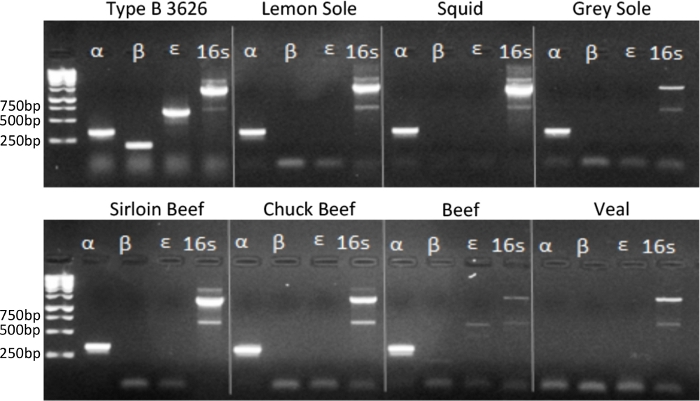
Figure 3: Selected PCR results.
Example images of the genotyping results of C. perfringens from seven different types of food, and a positive control of C. perfringens type B. A molecular weight ladder (first lane of each gel) was used to approximate the size of PCR results in base pairs (bp). Please click here to view a larger version of this figure.
| Toxinotype | Alpha | Beta | Epsilon | Iota | CPE | NetB | |
| Established | A | + | – | – | – | – | – |
| B | + | + | + | – | – | – | |
| C | + | + | – | – | + | – | |
| D | + | – | + | – | + | – | |
| E | + | – | – | + | + | – | |
| Proposed | F | + | – | – | – | + | – |
| G | + | – | – | – | – | + | |
| + present – not present +/- may or may not be present |
|||||||
Table 1: Overview of C. perfringens genotypes. A chart of the combinations of toxins produced by each C. perfringens toxinotype.
| Target | Primer Pairs | Expected PCR Product (bp) |
| alpha | F: GCT AAT GTT ACT GCC GTT GA R: CCT CTG ATA CAT CGT GTA AG |
325 |
| beta | F: GCG AAT ATG CTG AAT CAT CTA R: GCA GGA ACA TTA GTA TAT CTT C |
196 |
| epsilon | F: GCG GTG ATA TCC ATC TAT TC R: CCA CTT ACT TGT CCT ACT AAC |
655 |
| 16s RNA | F: AGA GTT TGA TCC TGG CTC A R: GGT TAC CTT GTT ACG ACT T |
~1300 |
Table 2: Primers and expected PCR products for selected toxin genes. Primers used in the PCR genotyping step.
| Food Type | Type A | Type B | Type C | Type D | C. perf + | |||||||
| alpha toxin positive | alpha, beta, and epsilon toxin positive | alpha and beta toxin positive | alpha and epsilon toxin positive | |||||||||
| n | n | % | n | % | n | % | n | % | n | % | ||
| Meat | beef | 38 | 8 | 21% | 1 | 3% | 0 | 0% | 0 | 0% | 9 | 24% |
| lamb | 10 | 0 | 0% | 0 | 0% | 0 | 0% | 0 | 0% | 0 | 0% | |
| pork | 15 | 2 | 13% | 0 | 0% | 0 | 0% | 0 | 0% | 2 | 13% | |
| mixed | 1 | 1 | 100% | 0 | 0% | 0 | 0% | 0 | 0% | 1 | 100% | |
| subtotal | 64 | 11 | 17% | 1 | 2% | 0 | 0% | 0 | 0% | 12 | 19% | |
| Poultry | chicken | 19 | 5 | 26% | 0 | 0% | 0 | 0% | 0 | 0% | 5 | 26% |
| turkey | 7 | 0 | 0% | 0 | 0% | 0 | 0% | 0 | 0% | 0 | 0% | |
| subtotal | 26 | 5 | 19% | 0 | 0% | 0 | 0% | 0 | 0% | 5 | 19% | |
| Seafood | cod | 4 | 0 | 0% | 0 | 0% | 0 | 0% | 0 | 0% | 0 | 0% |
| mixed | 1 | 0 | 0% | 0 | 0% | 0 | 0% | 0 | 0% | 0 | 0% | |
| salmon | 11 | 2 | 18% | 0 | 0% | 0 | 0% | 0 | 0% | 2 | 18% | |
| shelfish | 32 | 1 | 3% | 0 | 0% | 0 | 0% | 0 | 0% | 1 | 3% | |
| snapper | 4 | 3 | 75% | 0 | 0% | 0 | 0% | 0 | 0% | 3 | 75% | |
| flounder | 12 | 4 | 33% | 0 | 0% | 0 | 0% | 0 | 0% | 4 | 33% | |
| squid | 4 | 1 | 25% | 0 | 0% | 0 | 0% | 0 | 0% | 1 | 25% | |
| tilapia | 21 | 2 | 10% | 0 | 0% | 0 | 0% | 2 | 10% | 4 | 19% | |
| tuna | 3 | 0 | 0% | 0 | 0% | 0 | 0% | 0 | 0% | 0 | 0% | |
| other | 8 | 1 | 13% | 0 | 0% | 0 | 0% | 0 | 0% | 1 | 13% | |
| subtotal | 100 | 14 | 14% | 0 | 0% | 0 | 0% | 2 | 2% | 16 | 16% | |
| Dairy | cow | 3 | 0 | 0% | 0 | 0% | 0 | 0% | 0 | 0% | 0 | 0% |
| goat | 4 | 0 | 0% | 0 | 0% | 0 | 0% | 0 | 0% | 0 | 0% | |
| milk | 3 | 0 | 0% | 0 | 0% | 0 | 0% | 0 | 0% | 0 | 0% | |
| subtotal | 10 | 0 | 0% | 0 | 0% | 0 | 0% | 0 | 0% | 0 | 0% | |
| Produce | vegetable | 12 | 1 | 8% | 0 | 0% | 0 | 0% | 0 | 0% | 1 | 8% |
| fruit | 1 | 0 | 0% | 0 | 0% | 0 | 0% | 0 | 0% | 0 | 0% | |
| herb | 3 | 0 | 0% | 0 | 0% | 0 | 0% | 0 | 0% | 0 | 0% | |
| subtotal | 16 | 1 | 6% | 0 | 0% | 0 | 0% | 0 | 0% | 1 | 6% | |
| Total | 216 | 31 | 14% | 1 | 0.50% | 0 | 0% | 2 | 0.90% | 34 | 16% | |
Table 3: Prevalence of different C. perfringens toxinotypes in 216 food samples. An example of the results obtained when using this method to test retail food for C. perfringens. This table has been modified from the previously published manuscript Regan et al.16.
Discussion
Here we describe a method to identify C. perfringens prevalence in retail food samples with limited subculturing and without use of an anaerobic chamber system. This method uses a combination of techniques to increase identification of C. perfringens from food samples. By using a modified version of RPM media, we allow for the selective growth of C. perfringens. By sandwiching the inoculated RPM in between layers of TSC agar, we are able to identify and isolate anaerobic, sulfite-reducing bacteria characteristic of C. perfringens. To confirm the presence of C. perfringens, sulfite-reducing colonies are sub-cultured into fresh RPM. The modified version or RPM allows us to easily extract DNA from cultures, enabling PCR confirmation of specific toxin genes. Confirmation of C. perfringens contaminated food samples can be achieved within three days.
In early experiments, food samples were simply inoculated into RPM and DNA extracted from ON cultures. This method resulted in detection of C. perfringens in a limited number of samples (data not shown). Although RPM is selective for C. perfringens growth, it is not exclusive for C. perfringens growth. Other, gram-positive, D-cycolserine resistant bacteria can still grow in RPM. We hypothesized that contamination by other bacterial species may have decreased our detection of C. perfringens strains by decreasing the sensitivity of our PCR analysis in our first ON RPM culture. A critical step in increasing the detection of C. perfringens was the inclusion of the TSC agar “sandwich” technique. This allowed us to differentiate and select for anaerobic, sulfite-reducing colonies, characteristic of C. perfringens. A key step in this process is ensuring that the top layer of molten TSC agar is at 40 °C. Although some C. perfringens strains can grow at increased temperatures (46–48 °C)15,16, addition of molten agar at increased temperatures greatly reduces the amount of cultures recovered, mostly likely due to cell death.
There are several potential limitations to this method. As mentioned previously, neither the RPM nor TSC agar selects or differentiates for C. perfringens exclusively, allowing for growth of other bacterial species present in food samples. This may reduce the sensitivity of the assay to select for C. perfringens only. However, this is a common limitation in almost all culturing techniques. Genotyping confirmation of purified isolates is the best method for definitively identifying C. perfringens and other bacterial species. Another limitation of this study is that we do not test the purified isolates. We purposely did this to limit the amount of subculturing, as repeated subculturing is feared to result in plasmid loss. Because we do not isolate to purity, it is possible that multiple C. perfringens toxinotypes may be present in the same sample or subculture. If researchers wish to obtain purified isolates, standard purification methods can be used on the last RPM culture described in this method; this typically requires the use of anaerobic chambers. Although originally used to isolate C. perfringens from food, this method can be used to identify and isolate C. perfringens from a multitude of sources. Specifically, one such application of this method is to test fecal samples from humans (or animals) that are suspected to be infected with C. perfringens and toxinotype the bacteria to better understand the source of infection.
Divulgations
The authors have nothing to disclose.
Acknowledgements
This research did not receive any specific funding from the public, commercial, or not-for profit sectors.
Materials
| D-Cycloserine | Sigma-Aldrich | C6880 | |
| Dextrose | Sigma Life Science | D9434-250G | |
| Disposable Transfer Pipets | any brand | Select one with slim tip like Thermo Scientific Disposable Transfer Pipets 137116M/EMD | |
| DNeasy Blood & Tissue Kits | Qiagen | 69504 | Note: numerous DNA and plasmid extractions kits were evaluated, this kit gave the most desirable results. |
| Dry Incubator | any brand | ||
| Fluid thioglycolate medium | Remel | R453452 | |
| Gelatin from porcine skin | Sigma Life Science | G1890-500G | |
| Individual Primers | Invitrogen | ||
| Iron (II) sulfate heptahydrate | Sigma Life Science | F8633-250 G | |
| Lysozyme from chicken egg white | Sigma-Aldrich | L6876 | Needed for DNA extraction, not provided in kit |
| microcentrifuge tube | any brand | ||
| parafilm or plastic wrap | any brand | ||
| Peptone from casein and other animal proteins | Sigma-Aldrich | 70173-100G | |
| Perfringens Agar Base (TSC + SFP) | Oxoid | CM0587 | Make TSC agar according to instructions |
| Potassium phosphate dibasic | Sigma-Aldrich | P2222-100G | |
| Sodium chloride | Sigma-Aldrich | S-7653 | |
| Sterile Cell Scraper | any brand | ||
| Sterile cell Spreader | any brand | ||
| Sterile petri dishes | any brand | ||
| Supplies and equipment for gel electrophoresis | any brand | ||
| table top centrifuge | any brand | ||
| Taq PCR Master Mix Kit | Qiagen | 201443 | |
| Thermocycler for PCR reaction | any brand | ||
| water bath | any brand | ||
| Yeast extract | Sigma-Aldrich | 70161-100G |
References
- Petit, L., Gibert, M., Popoff, M. R. Clostridium perfringens: toxinotype and genotype. Trends in Microbiology. 7, 104-110 (1999).
- Rood, J. I., et al. Expansion of the Clostridium perfringens toxin-based typing scheme. Anaerobe. , (2018).
- Murrell, T. G., O’Donoghue, P. J., Ellis, T. A review of the sheep-multiple sclerosis connection. Medical Hypotheses. 19, 27-39 (1986).
- Rumah, K. R., Linden, J., Fischetti, V. A., Vartanian, T. Isolation of Clostridium perfringens type B in an individual at first clinical presentation of multiple sclerosis provides clues for environmental triggers of the disease. PLoS One. 8, 76359 (2013).
- Wagley, S., et al. Evidence of Clostridium perfringens epsilon toxin associated with multiple sclerosis. Multiple Sclerosis. , (2018).
- Linden, J. R., et al. Clostridium perfringens Epsilon Toxin Causes Selective Death of Mature Oligodendrocytes and Central Nervous System Demyelination. MBio. 6, 02513 (2015).
- Popoff, M. R. Epsilon toxin: a fascinating pore-forming toxin. FEBS Journal. 278, 4602-4615 (2011).
- Lee, C. A., Labbe, R. Distribution of Enterotoxin- and Epsilon-Positive Clostridium perfringens Spores in U.S. Retail Spices. Journal of Food Protection. 81, 394-399 (2018).
- Wen, Q., McClane, B. A. Detection of enterotoxigenic Clostridium perfringens type A isolates in American retail foods. Applied and Environmental Microbiology. 70, 2685-2691 (2004).
- Cooper, K. K., Bueschel, D. M., Songer, J. G. Presence of Clostridium perfringens in retail chicken livers. Anaerobe. 21, 67-68 (2013).
- Strong, D. H., Canada, J. C., Griffiths, B. B. Incidence of Clostridium perfringens in American foods. Applied and Environmental Microbiology. 11, 42-44 (1963).
- Buogo, C., Capaul, S., Hani, H., Frey, J., Nicolet, J. Diagnosis of Clostridium perfringens type C enteritis in pigs using a DNA amplification technique (PCR). Journal of Veterinary Medicine, Series B. 42, 51-58 (1995).
- Yamagishi, T., Sugitani, K., Tanishima, K., Nakamura, S. Polymerase chain reaction test for differentiation of five toxin types of Clostridium perfringens. Microbiology and Immunology. 41, 295-299 (1997).
- Johansson, A., Engstrom, B. E., Frey, J., Johansson, K. E., Baverud, V. Survival of clostridium perfringens during simulated transport and stability of some plasmid-borne toxin genes under aerobic conditions. Acta Veterinaria Scandinavica. 46, 241-247 (2005).
- Erickson, J. E., Deibel, R. H. New medium for rapid screening and enumeration of Clostridium perfringens in foods. Applied and Environmental Microbiology. 36, 567-571 (1978).
- Regan, S. B., et al. Identification of epsilon toxin-producing Clostridium perfringens strains in American retail food. Anaerobe. 54, 124-127 (2018).

