Positron Emission Tomography Imaging for In Vivo Measuring of Myelin Content in the Lysolecithin Rat Model of Multiple Sclerosis
Summary
This protocol has the aim of monitoring in vivo myelin changes (demyelination and remyelination) by positron emission tomography (PET) imaging in an animal model of multiple sclerosis.
Abstract
Multiple sclerosis (MS) is a neuroinflammatory disease with expanding axonal and neuronal degeneration and demyelination in the central nervous system, leading to motor dysfunctions, psychical disability, and cognitive impairment during MS progression. Positron emission tomography (PET) is an imaging technique able to quantify in vivo cellular and molecular alterations.
Radiotracers with affinity to intact myelin can be used for in vivo imaging of myelin content changes over time. It is possible to detect either an increase or decrease in myelin content, what means this imaging technique can detect demyelination and remyelination processes of the central nervous system. In this protocol we demonstrate how to use PET imaging to detect myelin changes in the lysolecithin rat model, which is a model of focal demyelination lesion (induced by stereotactic injection) (i.e., a model of multiple sclerosis disease). 11C-PIB PET imaging was performed at baseline, and 1 week and 4 weeks after stereotaxic injection of lysolecithin 1% in the right striatum (4 µL) and corpus callosum (3 µL) of the rat brain, allowing quantification of focal demyelination (injection site after 1 week) and the remyelination process (injection site at 4 weeks).
Myelin PET imaging is an interesting tool for monitoring in vivo changes in myelin content which could be useful for monitoring demyelinating disease progression and therapeutic response.
Introduction
Multiple sclerosis (MS) is a neuroinflammatory disease that affects the central nervous system, characterized by inflammation, demyelination, and axonal loss1. The prognosis of this disease is variable even with advances in treatment, and it is one of the most common causes of neurological deficits in young people1. The diagnosis of MS is based on the criteria of clinical manifestation and visualization of characteristic lesions by magnetic resonance imaging (MRI)2,3.
Positron emission tomography (PET) can be a useful tool for in vivo monitoring of MS progression and therapeutic effects. The Pittsburgh compound B radiotracer (PIB) labeled with carbon-11 (11C-PIB) is widely used to quantify β-amyloid plaques; however, in the last decade, it has been studied to quantify myelin content and show dynamic demyelination and remyelination4,5,6.
Different amyloid PET tracers (11C-PIB, 18F-florbetaben,18F-florbetapir, 18F-flutemetamol) can be used to quantify myelin and provide important information about disease progression and therapeutic response, allowing identification of demyelination and remyelination processes, without the interference of neuroinflammation, which can occur with conventional magnetic resonance images (MRI)7. Amyloid PET imaging showed decreased tracer uptake in active MS patients compared to non-active patients which could be explained by early white matter damage in the active patients8. Lower amyloid tracer uptake was also associated with cognitive decline in a follow-up study, showing this technique to be a valuable tool for studying the pathophysiology of the disease and clinical outcomes9.
The lysolecithin (LPC) rat model is a chemical induced model of multiple sclerosis, where the injected toxin, LPC, induces a high response of macrophages that results in increased inflammation and, consequently, demyelination10,11. The demyelination is rapidly reversed, in approximately 4 weeks, which makes this a good model for evaluating demyelination and remyelination processes in rodents. This model has already been evaluated using PET imaging, with good results and correlation with post-mortem essays12.
Here we present the protocol for myelin PET imaging with 11C-PIB in the lysolecithin rat model, showing this imaging technique to be a useful tool for in vivo measurement of myelin content.
Protocol
All procedures were conducted in accordance with the guidelines of the National Council for the control of Animal Experimentation (CONCEA, Brazil) and were approved by the Ethics Committee for Animal Research of the Medical School of the University of Sao Paulo (CEUA-FMUSP, Brazil – protocol number: 25/15).
NOTE: In this protocol, we show how to induce a lysolecithin rat model of multiple sclerosis and how to acquire and analyze the myelin PET images.
1. Lysolecithin solution preparation
- Weigh lysolecithin (L-α-Lysophosphatidylcholine from egg yolk) on an analytical scale using a conic plastic tube (1.5 mL).
- Add sterile saline to the tube to make 1% solution (for example: weigh 1 mg of lysolecithin and dissolve it with 100 µL of saline) and dissolve the lysolecithin by shaking the tube (shaking from side to side and not turning from top to bottom).
- Prepare the solution just before starting the animal model induction (do not stock the final ready solution).
2. Lysolecithin rat model – Stereotaxic surgery
- Use male Wistar rats weighing between 220 – 270 g. Use gloves and mask during all procedures.
- Induce anesthesia with 5% isoflurane mixed in 100% O2 (1 L/min) using an induction box. Check if the animal is anesthetized by observing absence of movement (only breathing should be observed).
- Place the animal in stereotaxic apparatus on a heating pad. Fix the nose and ears of the animal to the equipment.
NOTE: Details of how to perform stereotaxic surgery can be found in JoVE Science Education Database. Neuroscience. Rodent Stereotaxic Surgery. JoVE, Cambridge, MA, 2021.- Monitor the anesthesia for the whole procedure (including surgery and image acquisition). To adjust the isoflurane concentration, observe the animal breathing rate. A fast breathing rate requires higher concentration and a slow breathing rate requires lower anesthetic concentration.
- Inject the analgesic (ketoprofen – 5 mg/kg) subcutaneously (dilute the medication to 1 mL in saline, this will help to hydrate the animal).
- Put eye cream in the animal's eyes to protect against dehydration.
- Use a 0.5% chlorhexidine solution to clean the incision area.
- Inject 100 µL of lidocaine hydrochloride 2% subcutaneously in the region of incision.
- Shave the skull area.
- Use sterile instruments for this procedure.
- Using a scalpel, make an incision of about 2 cm in the skin over the skull.
- Expose the skull with Bulldog clamps.
- Use a swab to clean the skull area with 1% hydrogen peroxidase.
- Locate and mark the bregma (a stereotaxic rat brain atlas can help to identity the Bregma).
- Position the Hamilton syringe (µL neuros syringes) at the bregma.
- Using the bregma and a stereotaxic atlas as reference, position the Hamilton syringe at the following coordinates: Antero-posterior: -0.30 mm, latero-lateral: -3.0 mm, and ventral until it touches skull bone, and mark the skull and note the coordinates orientation on paper.
- Drill the skull at the marked coordinate. Take care with dura mater (damaging dura mater can cause a lot of bleeding).
- Fill the Hamilton syringe with 7 µL of lysolecithin solution (1% in saline). A greater volume can be placed in the syringe, but only 7 µL will be injected (take the bubbles out of the syringe to measure the volume correctly).
- Position the Hamilton syringe at the previous coordinates to start the drug injection (total of 7 µL into 3 different ventral stereotactic coordinates). Considering the previously noted coordinates, lower the Hamilton syringe to ventral coordinate -5.0 mm.
- Very slowly inject 2 µL of lysolecithin solution (1 µL/10 min). Wait 3 min.
- Take the needle up to the next ventral stereotaxic coordinate (-4.2 mm) and slowly inject 2µL of lysolecithin solution (1 µL/ 10 min). Wait 3 min.
- Inject the third ventral coordinate -3.0 mm (3 µL of lysolecithin solution – 1 µL/ 10 min).
- Wait 5 min and then remove the Hamilton syringe from the brain.
- Suture the skin.
- Remove the animal from the stereotactic apparatus and allow the animal to awaken.
- Return the animal to the home cage, keep the animal alone and under supervision to check for signs of discomfort.
- Inject subcutaneous analgesic (ketoprofen – 5 mg/kg) diluted in saline, at 24 h and 48 h after the surgery.
3. PET acquisition
- Take 7 to 20 MBq of 11C-PIB radioactivity in a syringe (1 mL is the maximum volume allowed for intravenous injection in rats).
- Anesthetize the animal with 5% isoflurane mixed in 100% O2 (1 L/min) using the induction box.
- Inject 11C-PIB (radioactivity defined in item 4.1 above) into the penile vein, or tail vein of the rat (both administration sites are fine, the decision is a personal choice. We only advice not to use a retro-orbital injection since the location is too close to the region of interest (the brain) and can impair image quality.
NOTE: Image acquisition of baseline time point is performed before stereotaxic injection and the other 2 time points at 1 week and 4 weeks after surgery. - Remove the animal from anesthesia to allow the animal to awaken (leave the animal on a warm pad until it is completely awake).
- Return the animal to the home cage.
- Wait 30 min for the next step.
- Anesthetize the rats with 5% isoflurane mixed in 100% O2 (1 L/min) using an induction box.
- Open PET scanner software.
- Select Scan > Pet Ready.
- Complete principal investigator details, Study ID, Series ID, Animal ID, Animal weight (g), and Additional notes. Select Next.
NOTE: Use dot (.) for decimal number in the animal weight. - Edit ROI area for scanning (usually between 3 and 8). This is the area that will be included in the image (areas between the numbers 3 and 8 of the bed cover will appear in the final image).
- Position the anaesthetized rat on a standard rat bed of the PET scanner and turn the anesthesia on (3% isoflurane in 100% O2 is a good start, and then the anesthesia rate should be adjusted as necessary). To adjust the anesthesia, check the monitoring data of the scanner software to verify that the animal is breathing in a constant and slow rhythm.
NOTE: Turn on the vacuum pump coupled to the activated carbon filter to collect isoflurane gas excess (if the pump is available). - Apply eye cream to protect the animal's eyes.
- Push the animal bed inside the PET scanner.
- Complete Activity details, Activity Calibration Time, Isotope (C-11), and Scan duration (20 minutes). Select Start Scan.
NOTE: A Pet Moving Bed message will appear, and the animal bed will move into the equipment and stop at the previously selected ROI position. Time of acquisition will start count down and number of counts per seconds will appear (CPS). - In the scanner software, navigate to the Monitor tab on the left of the screen, check Change Threshold to Respiratory parameters change (BPM).
NOTE: A window will pop up, complete with threshold parameter (500). Select OK. - Navigate to 0% POWER to change temperature parameters to heat the animal during scan. A window will pop up; complete the parameter (80 – 100). Select OK.
NOTE: Choose between 80 and 100% power based on room temperature conditions (the more power, the warmer it will get). - Navigate back to SCAN tab.
- Navigate to configuration tool (gear icon) and complete Injection Time, Remaining Activity, Remaining Activity Calibration Time. Select Save.
NOTE: A window will pop up "Are you sure you want to modify the protocol metadata?"> YES - Navigate back to the Monitor tab (check the animal's respiratory parameters, and if necessary, increase or decrease isoflurane concentration – usually 3% in 100% O2 is enough).
- When PET acquisition is finished, Pet Ready message will appear on the Scan tab, check Arrow Out Icon (left of configuration tool) to move out the animal bed.
- Remove the animal from anesthesia and allow to awaken on a warm pad.
- For reconstructing the image, navigate to Reconstruct tab.
- Check plus icon at bottom left of the screen, and select the study file which will be reconstructed. Select Next.
- Navigate to Energy Resolution tool. A window will pop up. Configure the energy peak (keV) to the equipment parameter (based on monthly quality control). Select Close.
NOTE: Energy peak can change every month when performing monthly equipment calibration. - Keep all other parameters as the default (Isometric voxel size: 400 mm; number of iterations: 30; Energy resolution: 30%; Save last iteration only; uncheck Keep binary data) .
- Check Add.
NOTE: A window will pop up "The reconstruction was added to the queue and will start once the others have finished". Select OK. A file will appear in the reconstruction list on the Reconstruct tab and the status will appear as waiting or % (progress) or finished.
4. Image Analysis
NOTE: Perform image analysis using dedicated image analysis software. In the current protocol the demonstration uses a specific software program, but if it is not available, other options can be used.
- Open PMOD > Fuse it.
- Navigate to the Matching tab at the top of the screen.
- Open the Load Input menu in the right middle of the screen and select Autodetect files, select PET file (DICOM, Interfile or NifTI), add to selected, click with Operations, Reorient to Standard Orientation, click Load and Close.
- Verify if the animal Species is correct at the bottom of the screen (RAT).
- Check Crop box at the bottom right of the screen.
- Adjust the yellow box size in the PET image to take the whole brain.
- Click the Rigid button on the right of the screen. At confirmation window click Yes.
- Click on the brain tool at the right middle of the screen to open Reference Atlas. Select Px Rat (W.Schiffer) – T2.
- Select Match Results from the top right tab (Select processing stage tab).
- Click Data reslicing (4thtab at top right menu).
- Align the PET image with reference template using the rotate tool (white icon at center of PET image). Check alignment for 3 anatomical planes.
- Save the co-registration file (right side menu of the screen).
- Select output format (DICOMor NifTI), directory and file prefix. Click Save.
NOTE: If co-registered output is saved as NifTi the header image information will be lost. - Click VOIs menu at the bottom of the screen.
- Navigate to Template > Atlas at the bottom of the screen (below VOIs window).
- Select Px Rat(W.Schiffer) from the drop-down menu.
NOTE: If you need to analyze only specific VOIs you can select only the brain areas of interest. If you want all brain areas of the brain atlas, no action is needed. - Click Outline at the bottom of the screen.
NOTE: VOIs of brain areas will appear in VOIs window. - Manually draw the VOI in the lesion site and contralateral brain hemisphere area (11C-PIB low uptake area and contralateral brain hemisphere, respectively).
- Click in the area of PET image with 11C-PIB low uptake.
- Select New VOI > OK.
NOTE: A spreadsheet will appear - Navigate to SPHERE icon in the middle part of the screen (to the left of the VOIs window)
NOTE: A spreadsheet will appear. - Choose the VOI name: lesion and select Apply.
NOTE: A sphere will appear in the co-registered image. - Align the sphere in the lesion area and adjust the VOI for all anatomical planes.
- Click Close (at the bottom part of the spreadsheet).
- Select the lesion VOI (from VOIs list).
- Navigate to VOI mirroring operations icon (at the top right of the VOIs window) and select Clone and mirror left/right.
- Navigate to Calculate Selected VOI Statistics at the top of the VOIs list window. Navigate to Select statistics to be calculated icon to choose the output data (to the right side of the VOI statistics icon). Usually for myelin content check Statistics for group of VOIs, Average, SD, Min, Max).
NOTE: A spreadsheet will appear. The default setting Data Unit is kBq/cc. On the left top of the spreadsheet (VOI Statistics) you can check the Data Unit as SUV (Standardized Uptake Value). If you completed the radiotracer administration and image acquisition details correctly in the scanner software, as described previously, the SUV data will be calculated automatically by PMOD software, if not, you can edit the details. - Navigate to Copy using system locale number format.
NOTE: Verify if all statistics are selected to copy as output (Check icon at the right top of the screen). The data that will be copied depends on the Data Unit selected. - Paste the output data in a notepad or spreadsheet.
NOTE: Take care with software settings for dot and comma symbols between numbers. This can be different between language configurations. - Save the file with study name and details.
Representative Results
Figure 1 shows illustrative 11C-PIB PET images with myelin changes over time. In the baseline scan, no differences can be seen in myelin content (i.e., no demyelination is present). In the 1-week time-point image, it is possible to see the focal demyelinated lesion (in the right hemisphere) as indicated by the white arrow. Images are presented in the 3 anatomical planes (coronal, axial, and sagittal) and it is possible to identify the demyelinated lesion in all of them. The 1-week image is the illustration of a well delimited lesion at the injection site, representing the correct model induction and image detection. In the 4 weeks image, no lesion is visible anymore, indicating that remyelination has occurred and myelin content is back to normal (or close to it).
The representative graphs show the quantification of the images of 4 animals in the 3 different time points. The first graph shows the results from the quantification of the lesion (manual VOI) to contralateral side ratio demonstrating more focal myelin changes, where the lysolecithin injection was performed. The second graph shows the same quantification, but in the striatum (injected striatum to contralateral ratio) and in this case the difference is not statistically significant, which can be explained by the small sample size and because the VOI is bigger and the radioactivity concentration is measured not only where the lysolecithin was injected.
Differences between groups were analyzed by the Kruskal Wallis test, followed by Dunn´s test for multiple comparisons and the results are presented as mean ± SD. In the lesion VOI (H = 7.063; P=0.017), in the 1-week image, the tracer uptake ratio (0.90±0.07) was 16% lower than baseline (1.07±0.06), with statistical significance (p=0.024). No significant differences were found in the 4-week image (1.01±0.06).
In the striatum, no statistical differences were found (H =1.412; P=0.5393). The uptake ratios for the images were 1.07±0.07 for baseline, 1.02±0.07 for 1 week, and 1.01±0.08 for 4 weeks.
The third graph (bottom line, left graph) presents the quantification of the contralateral striatum (non-injected side). In this graph it is possible to observe that there was no difference (P=9397) among time points, meaning that the variation in the injected side is due to myelin changes and not due to tracer uptake variation over time.
The final graph, in the bottom right, shows the quantification of the injected site (lesion VOI) in animals where the model was not well induced (probably due to fast lysolecithin injection, wrong stereotaxic manipulation, and/or incorrect solution preparation). In this case, the lower uptake is not seen in the 1 week time point, meaning no demyelination process has occurred, and the low uptake at 4 weeks can be related to a later demyelination process or tissue damage, both situations are related to bad animal model induction. This graph was added to the protocol to exemplify the appearance of the results when the animal induction is not well performed and to emphasize the importance of each step of the protocol, from the beginning to the end. There are no differences in the tracer uptake (H = 2.745, P = 0.267) with uptake ratios of 1.06±0.05, 1.02±0.14, and 0.96±0.10 for baseline, 1 week, and 4 week PET images.
Figure 2 adds more information to the results, where Figure 2A details where the manual VOI was drawn, based on the MRI template reference and Figure 2B shows the luxol fast blue staining (for details about the luxol fast blue staining protocol, see De Paula Faria et al.13) from the injected side and non-injected side at 7 days post stereotaxic injection.
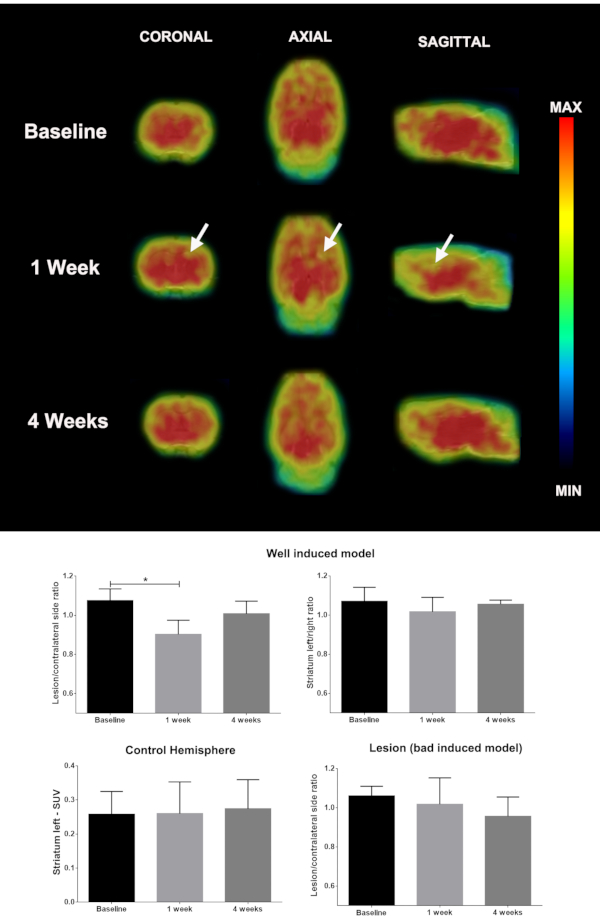
Figure 1: Illustrative 11C-PIB PET images showing images of baseline, 1 week, and 4 weeks after stereotactic injection. The graphs at the bottom of the figure represent the quantification of tracer uptake (n=4) at different time points. The first two graphs represent the uptake ratio in the injected side to contralateral side in the lesion and in the striatum in a well induced model (i.e., rats presenting lesion after lysolecithin injection). The third graph (bottom left) shows the quantification of non-injected striatum (negative control), and the final graph (bottom right) represents the 11C-PIB uptake at the injection site of animals that did not present demyelinated lesion (badly induced model). Results are presented as mean±SD. Please click here to view a larger version of this figure.
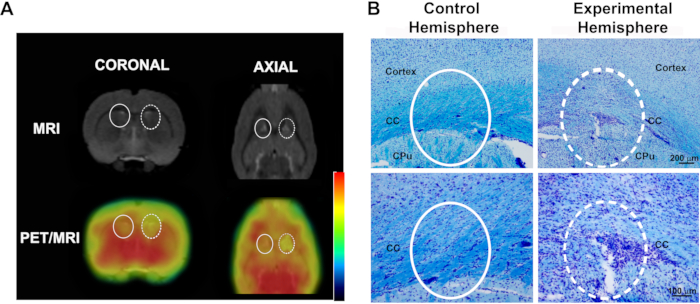
Figure 2: Lesion location details. A) Illustrative VOIs of injected side (dashed line) and non-injected side (white line) drawn manually based on the MRI template (region of corpus callosum and striatum) at 1 week post stereotactic injection. B) Luxol fast blue staining showing demyelination in the injected hemisphere compared to the non-injected side (Top: 40x magnification, bottom: 100x magnification). Please click here to view a larger version of this figure.
Discussion
The biggest advantage of using the lysolecithin model to study multiple sclerosis is the fast timeline for demyelination (about 1 week) and remyelination (about 4 weeks) to occur14. This model can also be induced in mice15, however, induction in rats is more advantageous for in vivo PET imaging due to the larger size of the rat brain compared to mice.
The first step of the induction model is to be extremely cautious. This model was validated for myelin PET imaging by de Paula Faria et al.10 in 2014 and it was shown that the speed of the lysolecithin injection inside the brain is crucial for a well induced model. The injection must be performed very slowly, 1 µL each 10 min, as a way of avoiding tissue damage. The lysolecithin solution should also be prepared on the same day as the stereotactic injection, preferably just before starting the surgery procedure. If the model will be used for the first time in a research group, we recommend that the model should be validated before performing any myelin quantification by PET imaging. The validation needs to include post-mortem tissue analysis by myelin staining, for example: Luxol fast blue histology, as shown in Figure 2, and myelin basic protein (MPB) immunohistochemistry, in the different time points intended to be used in in vivo analysis. In the results section we showed a quantification of radiotracer uptake where lesion induction was not well succeeded and, therefore, the differences were not detected by 11C-PIB PET imaging.
The lesion to be quantified by this technique must be bigger than the PET scanner resolution (about 1 mm in preclinical equipment and about 5 mm in clinical equipment).
Once the model is well induced, the imaging procedure must be well planned, due to the radiotracer labeled with carbon-11, which has a short half-life of 20 minutes. The preclinical imaging laboratory personnel need to prepare all necessary material, fill the anesthesia system, check if everything is working properly, and print the forms to be completed during the experiment. The PET scanner should also be verified prior to the experiment, when all quality controls necessary in the equipment (dependent on each country) must be performed to check the scanner is well functioning. After receiving the tracer for injection, the measurement of activity must also be measured in a calibrated dose calibrator to guarantee the correct injected dose, and the information (activity in the syringe, before and after injection) written on the form, as well as the respective time when the measurement was performed. Establish which watch is going to be used, as the right time is the time on the workstation of the PET scanner, the time that will be considered in the decay correction of the images, therefore, any watches used during the experiment should be synchronized to the scanner workstation time.
During animal image acquisition, temperature and animal breathing should be monitored and the anesthesia adjusted, as necessary. Temperature is location dependent and should be adjusted for the animal well-being. After the image acquisition is finished, it is important to keep the animal on a warm pad to recover before being returned to the cage.
Image processing is crucial for getting reliable results from the experiments using PET imaging. The ideal is that the analyzer is not aware of the animal groups and/or treatment and that he/she already has experience in PET images with the PET tracer used in such a way as to guarantee perfect registration between the PET imaging and MRI template. We used the PMOD software in this protocol, but if this software is not available, alternative image quantification software can be used, although attention must be given to achieving good brain region definition and quantification. For the definition of the lesion location, extra care must be taken to ensure that the injected site is inside the drawn lesion VOI (a knowledge of rat brain anatomy is necessary).
It is important to say that myelin PET imaging can also be performed in other MS animal models, displaying unpredictable lesions, as already shown by our group in the Experimental Autoimmune Encephalomyelitis (EAE) marmoset model5. As already stated, the important parameter to consider in lesion quantification is the PET scanner resolution, which is the limitation for detection of lesions that are too small. PET imaging is a poor resolution imaging technique when compared to other techniques such as MRI, however it is a highly specific modality and, because of this, quantification of the PET images uses an anatomical template, such as the MRI, for helping to draw the region of interest, as shown in the above protocol.
Although the manual drawing of VOIs is operator dependent, it is the best option for the LPC animal model, since the lesion can be variable between animals. To diminish bias in the quantification process, it is important to perform a mirror VOI, as explained in the protocol, which will be in the same region and of the same size as the injected side. It is also important to have the stereotaxic coordinates in mind when drawing the VOI in the MRI template to guarantee that the correct brain region is considered. Using the myelin staining as a guide to identify the demyelinated area can also help in the drawing, as explained in de Paula Faria12.
Divulgations
The authors have nothing to disclose.
Acknowledgements
β-cube equipment (Molecubes NV, Belgium) was supported by the São Paulo Research Foundation, FAPESP – Brazil (#2018/15167-1). LES has a PhD student scholarship from FAPESP – Brazil (#2019/15654-2).
Materials
| Analytical Balance | Marte | AUWZZOD | max: 220 g- min: 1 mg |
| Anestesia vaporizer | Nanitech | 15800 | |
| Beta-cube | Molecubes | ||
| Bulldog clamp | Stoelting | 5212043P | |
| clorexidine | Rioquimica | 0.5%/100 mL | |
| Cotton swabs | johnson e johnson | ||
| Dose calibrator | Capintech | ||
| Drill | Kinzo powertools | 352901 | Model Q0M-DC3C |
| Eppendorf tube | Eppendorf | 30125150 | 1.5 mL |
| Eye lubricant | ADVFARMA | 30049099 | vaseline 15 g (pharmaceutical purity) |
| Fine forceps | Stoelting | 52102-38P | |
| Gloves | Descarpack | 212101 | 6.5 size |
| Heating pad | Softhear | ||
| Injection Syringe | Hamilton | 80314 | 10µ, 32ga, model 701 |
| Insuline syringe | BD | 328328 | 1 mL insulin syringes with needle |
| Isoflurane | Cristália | 410525 | 100 mL , concentration 1 mL/1 mL |
| Ketoprofen or other analgesic | Sanofi | 100 mg/2 mL | |
| lidocaine | Hipolabor | 1.1343.0102.001-5 | 2%/20mL |
| L-α-Lysophosphatidylcholine from egg yolk | Sigma-aldrich | L-4129 | 25 mg – ≥99%, Type I, powder |
| Needle holder | Stoelting | 5212290P | |
| Oxygen | White Martins | 7782-44-7 | Compressed gas |
| PMOD software | PMOD technologies | Version 4.1 | module fuse it |
| Rat anesthesia mask | KOPF | Model 906 | |
| Saline | Farmace | 0543325/ 14-8 | 0.9% sodium chloride for injection, 10 mL |
| Scapel blades | Stoelting | 52173-10 | |
| Scapel handles | Stoelting | 52171P | |
| Scissor | Stoelting | 52136-50P | |
| Semi-analytical Balance | Quimis | BK-3000 | max:3,100 g; min:0.2 g |
| shaver | Mega profissional | AT200 model | |
| Stereotactic Apparatus | KOPF | Nodel 900 | |
| Universal holder with needle support | KOPF | Model 1772-F1 | Hamilton support for 5 and 10 µL |
References
- Oh, J., Vidal-Jordana, A., Montalban, X. Multiple sclerosis: clinical aspects. Current Opinion in Neurology. 31 (6), 752-759 (2018).
- Sand, I. K. Classification, diagnosis, and differential diagnosis of multiple sclerosis. Current Opinion in Neurology. 28 (3), 193-205 (2015).
- Thompson, A. J., et al. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurology. 17 (2), 162-173 (2018).
- Veronese, M., et al. Quantification of C-11 PIB PET for imaging myelin in the human brain: a test-retest reproducibility study in high-resolution research tomography. Journal of Cerebral Blood Flow and Metabolism. 35 (11), 1771-1782 (2015).
- Carvalho, R. H. F., et al. C-11 PIB PET imaging can detect white and grey matter demyelination in a non-human primate model of progressive multiple sclerosis. Multiple Sclerosis and Related Disorders. 35, 108-115 (2019).
- Stankoff, B., et al. Imaging central nervous system myelin by positron emission tomography in multiple sclerosis using [methyl-(1)(1)C]-2-(4′-methylaminophenyl)- 6-hydroxybenzothiazole. Annals of Neurology. 69 (4), 673-680 (2011).
- Faria, D. D. Myelin positron emission tomography (PET) imaging in multiple sclerosis. Neural Regeneration Research. 15 (10), 1842-1843 (2020).
- Pietroboni, A. M., et al. Amyloid PET as a marker of normal-appearing white matter early damage in multiple sclerosis: correlation with CSF -amyloid levels and brain volumes. European Journal of Nuclear Medicine and Molecular Imaging. 46 (2), 280-287 (2019).
- Pytel, V., et al. Amyloid PET findings in multiple sclerosis are associated with cognitive decline at 18 months. Multiple Sclerosis and Related Disorders. 39, (2020).
- Faria, D. d. P., et al. PET imaging of glucose metabolism, neuroinflammation and demyelination in the lysolecithin rat model for multiple sclerosis. Multiple Sclerosis Journal. 20 (11), 1443-1452 (2014).
- Rinaldi, M., et al. Galectin-1 circumvents lysolecithin-induced demyelination through the modulation of microglial polarization/phagocytosis and oligodendroglial differentiation. Neurobiology of Disease. 96, 127-143 (2016).
- Faria, D. d. P., et al. PET imaging of focal demyelination and remyelination in a rat model of multiple sclerosis comparison of [C-11]MeDAS, [C-11]CIC and [C-11]PIB. European Journal of Nuclear Medicine and Molecular Imaging. 41 (5), 995-1003 (2014).
- Faria, D. d. P., et al. PET imaging of focal demyelination and remyelination in a rat model of multiple sclerosis: comparison of [11C]MeDAS, [11C]CIC and [11C]PIB. European Journal of Nuclear Medicine and Molecular Imaging. 41 (5), 995-1003 (2014).
- vander Star, B. J., et al. In Vitro and In Vivo Models of Multiple Sclerosis. CNS & Neurological Disorders-Drug Targets. 11 (5), 570-588 (2012).
- Najm, F. J., et al. Drug-based modulation of endogenous stem cells promotes functional remyelination in vivo. Nature. 522 (7555), 216 (2015).

