In Vivo Chronic Two-Photon Imaging of Microglia in the Mouse Hippocampus
Summary
This paper describes a method for chronic in vivo observation of the resting microglia in the mouse hippocampal CA1 using precisely controlled surgery and two-photon microscopy.
Abstract
Microglia, the only immune cells resident in the brain, actively participate in neural circuit maintenance by modifying synapses and neuronal excitability. Recent studies have revealed the differential gene expression and functional heterogeneity of microglia in different brain regions. The unique functions of the hippocampal neural network in learning and memory may be associated with the active roles of microglia in synapse remodeling. However, inflammatory responses induced by surgical procedures have been problematic in the two-photon microscopic analysis of hippocampal microglia. Here, a method is presented that enables the chronic observation of microglia in all layers of the hippocampal CA1 through an imaging window. This method allows the analysis of morphological changes in microglial processes for more than 1 month. Long-term and high-resolution imaging of the resting microglia requires minimally invasive surgical procedures, appropriate objective lens selection, and optimized imaging techniques. The transient inflammatory response of hippocampal microglia may prevent imaging immediately after surgery, but the microglia restore their quiescent morphology within a few weeks. Furthermore, imaging neurons simultaneously with microglia allows us to analyze the interactions of multiple cell types in the hippocampus. This technique may provide essential information about microglial function in the hippocampus.
Introduction
Microglia are the only immune cells and tissue macrophages resident in the brain. In addition to their functions as immune cells, such as rapid response to inflammation, they have been shown to play a variety of physiological roles in the maintenance and remodeling of neural circuits, such as synaptic pruning, regulation of synaptic plasticity, and control of neuronal activity1,2,3,4,5. Physiological interactions between microglia and neurons are of increasing interest in both neural circuit development and disease neurobiology. Analyzing the physiology of microglia in vivo requires methods to observe microglia without tissue damage and inflammatory responses. However, microglia are sensitive to inflammation and dramatically change their shapes and functions in response to tissue damage6,7.
Two-photon in vivo imaging is an ideal tool for capturing the physiological dynamics of microglia8. Initial applications of in vivo two-photon imaging revealed the dynamic movement of microglial processes for environmental surveillance in the adult mouse cortex9,10. The following two-photon imaging studies further extended the in vivo monitoring of microglia for the analysis of functional and structural interactions with neurons5,11,12,13,14. However, the imaging depth of conventional two-photon microscopy has been limited to less than 1 mm from the brain surface15,16. This constraint explains the scarcity of previous studies reporting the behavior of microglia in deep brain regions, such as the hippocampus.
Recent RNA sequencing studies have revealed a considerable regional heterogeneity of microglia, raising the possibility of distinct functional roles17,18,19,20,21. Therefore, it is necessary to record microglial interactions with neurons in various brain regions, but technical difficulties have hampered such studies. In particular, microglial active involvement in synapse remodeling has been reported to be critical in the development of the hippocampal neural network and its memory-related functions22,23. However, effective methods for observing unchallenged hippocampal microglia in vivo have not been available.
This protocol explains the procedures for the chronic in vivo observation of resting microglia in the CA1 of the dorsal hippocampus using precisely controlled surgical techniques. Two-photon imaging of the CA1 area in CX3CR1-GFP mice (CX3CR1+/GFP), which express GFP in microglia24, enabled observation of the ramified microglia in all layers of the CA1 with sufficient resolution. The protocol includes several tips for successful implantation of the observation window and appropriate imaging conditions. In addition, simultaneous visualization of pyramidal neurons and microglia in the CA1 is presented as an application example. The advantages, limitations, and potentials of this technique are also discussed.
Protocol
All animal experiments were approved and carried out following the policies of the Animal Ethics Committee and the Genetic Recombinant Experiment Safety Committee at the University of Tokyo. Both male and female CX3CR1-GFP mice, aged 2-4 months, were used in the experiments. For the safety of the experimenters and the maintenance of sterile conditions, all the procedures were performed with white coats, masks, and sterile gloves. All instruments were sterilized before use.
1. Preparation of instruments and animals
- Assemble a glass-bottom metal tube (Figure 1A).
- Apply a small drop of UV-curing optical adhesive to one end of a custom-made stainless tube (outer diameter 3.0 mm, inner diameter 2.8 mm, height 1.7 mm). Spread the glue on the circular edge of the tube uniformly.
NOTE: A sufficient amount of adhesive should be used to cover the entire edge of the tube. - Place a circular glass coverslip (3.0 mm diameter, 0.15 ± 0.02 mm thickness) to the glue-covered end of the metal tube, and lightly press the coverslip against the tube so that the gap between the tube and the glass is filled with the glue. Next, adjust the position of the glass to fit within the outer edge of the metal tube.
- Irradiate the glass with UV light for a sufficient time to cure the adhesive.
NOTE: Make sure that the glass and the tube are completely attached. If the adhesion is insufficient, the glass may come off after surgery, resulting in unsuccessful imaging or leakage of cerebrospinal fluid (CSF). - Disinfect the assembled glass-bottom metal tube with 70% ethanol and wash with sterile saline to remove debris.
- Apply a small drop of UV-curing optical adhesive to one end of a custom-made stainless tube (outer diameter 3.0 mm, inner diameter 2.8 mm, height 1.7 mm). Spread the glue on the circular edge of the tube uniformly.
- Sterilize all surgical instruments with a dry heat sterilizer.
- Prepare mice for the surgery of window implantation.
NOTE: Mice should be of appropriate age. It is preferable that they are genetically engineered to express fluorescent proteins in the CA1 and the dentate gyrus (DG). These points are further explained in the Discussion section.
2. Anesthesia and head fixation
- Anesthetize a mouse by intraperitoneal injection of ketamine-xylazine (100 mg/kg ketamine and 10 mg/kg xylazine). Administer meloxicam (2 mg/kg) by subcutaneous injection for pre-operative analgesia. Confirm the disappearance of the response to painful stimuli, such as tail pinching to ensure adequate depth of anesthesia. Add a half dose of ketamine-xylazine each time the anesthesia wears off during surgery, typically 1 h after the initial administration and every 30 min thereafter. Use a heating pad under the body to provide thermal support and apply ophthalmic ointment on the eyes to prevent dryness under anesthesia.
NOTE: The choice of anesthesia for surgery is essential. This point is discussed in detail in the Discussion section. - Apply depilatory cream to remove hair from the scalp. Disinfect the scalp several times in a circular motion with povidone-iodine scrub followed by alcohol. Place the mouse on the surgical platform prepared with a sterile waterproof pad and apply sterile drapes to secure the surgical site. Then, cut and remove the scalp circularly with a scalpel so that the parietal and the occipital bones are fully exposed on the operative side.
- Remove the subcutaneous connective tissue by rubbing it with a cotton swab while applying sterile saline to clear the bleeding. Gently scrape the cranial surface with a round-tipped miniature knife to remove the periosteum, which helps to strengthen the adhesion between the cement and the bone (see step 2.6).
- Apply dental etching material to the entire surface, wait for tens of seconds, and rinse with sufficient sterile saline.
- Using waterproof ink, mark the area of the bone to be removed (a circular area with a diameter of 3.0 mm, centered about 2.5 mm posterior and 2.5 mm lateral to the bregma). After marking, dry the skull surface thoroughly.
NOTE: The position of craniotomy depends on the size of the hippocampus and should be optimized for different ages. Useful indicators for the position of craniotomy will be presented below (see step 3.4.5, NOTE). - Attach the rectangular aluminum plate with a thickness of 1.0 mm and with a 5.0 mm diameter hole at the center to the skull using dental resin cement according to the manufacturer's instructions.
- Carefully align the hole at the center of the plate with the circular area marked with a pen (see step 2.5) so that the aluminum plate is parallel to the marked surface of the skull (Figure 1B). Ensure that the cement tightly seals all gaps between the plate and the bone. Wait for about 5 min for the cement to be sufficiently hardened.
- Place the mouse onto the head holding device with angle adjusters via the attached plate.
3. Implantation of the observation window
NOTE: The following surgical procedures should be performed under a stereo microscope.
- Make a circular groove on the skull using a dermal punch with a diameter of 3.0 mm. Align the circular groove and the area marked with a pen in step 2.5. Twist the dermal punch with gentle pressure so that the groove depth gradually increases. Frequently check that the groove depth is constant over the entire circumference.
- When the dermal punch reaches the innermost layer of the cranium, before touching the underlying dura, gently lift the central bone island using a 30 G needle.
NOTE: Slight liquid leakage from the bottom of the groove indicates that the groove is close to the dura. - Remove the dura using a dura picker.
NOTE: Complete removal of the dura within the cranial window is necessary and will require careful resection of the residual dura at the periphery using fine forceps. - Gently aspirate the tissue to expose the alveus of the hippocampus by 23 G or 25 G blunt needles connected to the aspirator.
NOTE: This step is the most critical for successful imaging. Key technical points for the tissue aspiration are described in detail in the Discussion section.- Aspirate the pia and the pial vessels.
- Aspirate the cortical tissue from the surface. Keep the depth of exposed tissue surface homogeneous over the entire cranial window. Gradually deepen the aspiration until fibers of the external capsule are exposed.
- Carefully position the suction tip to the external capsule near the lateral ventricle (LV) located at the rostrolateral end of the cranial window. Remove the surface layer of the external capsule running in the caudomedial to rostrolateral direction, and then the inner layer running in the mediolateral direction.
NOTE: The external capsule near the LV can be easily removed from the underlying structure. - Confirm the removal of the entire external capsule by checking the full exposure of the surface of the alveus and the dorsal hippocampal commissure (DHC).
NOTE: The DHC covers the caudomedial portion of the CA1. The alveus and the DHC can be distinguished from the external capsule by their fiber orientations. Namely, the fibers within the alveus and the DHC run in the rostromedial to caudolateral direction, and can be distinguished from the fibers in the external capsule. The alveus and the DHC are tightly attached to the CA1 and should not be damaged. All fragments of the external capsule should be removed, since any remaining fragments will prevent the direct contact of the glass coverslip to the alveus. - Confirm that the bleeding has stopped thoroughly and fill the hole with sterile saline to the level of the skull surface.
NOTE: The field of view here helps to judge whether the hole is in the appropriate position for the specific age of the mouse. Ideally, the alveus and the underlying CA1 should occupy most of the central area. A part of the DHC is visible in the caudomedial area. The opening of LV is detectable at the rostrolateral edge (Figure 3A).
- Insert the glass-bottom metal tube (see step 1.1) vertically into the hole while aspirating the excess water that overflows from the sides of the tube until the glass bottom lightly presses against the alveus and partially flattens the underlying CA1.
NOTE: This pressure needs to be adjusted appropriately. If it is too strong, the CA1 will be damaged. If it is too weak, the spherical aberration due to the curvature of the CA1 will impair imaging resolution in deep structures. - Using dental resin cement, fix the wall of the inserted tube to the surrounding skull (Figure 1C). Ensure that the entire circumference is tightly sealed and that there is no leakage of air or CSF. Wait for about 5 min for the cement to harden.
NOTE: If the cement is placed when its viscosity is low, it may leak into the brain parenchyma through the gap between the tube and the skull and damage the brain. Therefore, the cement should be applied after polymerization initiation, which increases the viscosity and reduces leakage through the gap. - Wash the entire plate, the skull, and the inside of the tube with sterile saline to remove debris.
4. Two-photon microscopy immediately after surgery for quality check of the surgery
- Set the mouse in the head-holding device under the objective lens of the two-photon microscope and on the motorized XY scanning stage. Use a heating pad for thermal support. Monitor and adjust the depth of anesthesia as described in Step 2.1, as this quality check may take up to 30 mins.
NOTE: The water-immersion objective lens with a working distance (WD) longer than 3 mm and a high numerical aperture (NA) is recommended. A correction collar of the objective lens can improve the resolution by compensating for the refractive index mismatch between the glass and the biomaterials. - Fill the space between the glass and the objective lens with water, taking special care to avoid air bubbles. If necessary, expand the area of the metal plate using a plastic film, which holds more water, to cover the entire front lens of the objective.
- Turn on a femtosecond pulsed laser of 920 nm wavelength for the excitation of the fluorescent probes expressed in the brain and start image acquisition software.
- Adjust the focus to the CA1 with the use of the motorized stage and the motorized focus system. Position the target structure with the guidance of the fluorescence emitted from the brain parenchyma and the reflected light from the edge of the metal tube under continuous illumination by the pulsed laser.
- Measure the depths of the brain parenchyma touching the glass bottom by adjusting the focus with the motorized focus system. Compare the depths at different horizontal locations to judge the alignment of the glass bottom and the imaging plane.
- Adjust the angle of the mouse head by tilting the head holding device until the glass bottom is set to be parallel to the imaging plane.
- Adjust the correction collar of the objective to achieve the highest resolution at the depth of the target structure in the CA1.
- Confirm that the fluorescent cells in the molecular layer (ML) of the DG upper blade at a depth of 500 µm from the glass bottom can be imaged in the entire field of view.
NOTE: This step is important in judging the quality of surgery. If the CA1 is damaged, focal brain edema prevents fluorescence detection at a depth of more than 200 µm from the surface. Only when there is no damage to the CA1, and the curvature of the CA1 layers is properly flattened by the overlying coverslip, the DG signals can be detected immediately after surgery (Figure 2A-D). The Representative Results section provides a simple way to determine the boundary between the CA1 and the DG.
5. Postoperative care
- Aspirate the water inside the tube and cover it with a plastic seal to prevent debris from entering.
- Keep the mouse warm and wait for recovery from the anesthesia.
- Administer meloxicam (2 mg/kg) subcutaneously every 24 h as long as the mouse exhibits pain-related behavior.
- Raise the postoperative mouse in individual housing for several weeks.
6. In vivo chronic two-photon imaging of microglia using CX3CR1-GFP mice
- After induction of anesthesia, wash the inside of the metal tube with sterile saline to remove debris. Ensure that the white alveus of the hippocampus is visible through the glass (Figure 3A) and there are no complications such as postoperative bleeding.
- Set the mouse under the two-photon microscope following steps 4.1 to 4.6.
- Check the quality and intensity of images obtained by two-photon excitation of the hippocampus (Figure 3B). Ensure that the images taken after the reduction of postoperative edema are comparable to or better than those taken on the day of the surgery (Figure 2A, see step 4.5).
NOTE: Image deterioration indicates the presence of tissue damage inside the brain. - Ensure that microglia have already recovered their ramified morphology (Figure 3C).
NOTE: The imaging data of microglia indicates that at least 3-4 weeks are required for microglia to return to their basal state. - Perform in vivo imaging in any layers of the CA1 for the particular purpose of the experiment.
Representative Results
Using this technique, the ramified and quiescent microglia can be chronically observed within all layers of the dorsal CA1, including stratum oriens (SO), stratum pyramidale (SP), stratum radiatum (SR), and stratum lacunosum-moleculare (SLM), especially 3-4 weeks after surgery when the inflammation subsides. If the surgery is performed appropriately, imaging can be performed up to several months after surgery. This section contains three topics useful for the evaluation of intravital imaging. First, sample images immediately following surgery and in the chronic phase are provided as references for appropriate surgical and imaging procedures. Second, the distinct morphology of microglia, their fluorescence intensity, and blood vessel distribution in specific hippocampal layers are described to help readers estimate the imaging depth ranging from the alveus to the DG. Third, an application example is provided that illustrates simultaneous imaging of neurons and microglia.
The representative images of microglia in CX3CR1-GFP mice immediately after surgery are shown in Figure 2. If there is no apparent damage to the CA1 and the curvature of the CA1 layers is properly flattened by the overlying coverslip, two-photon imaging depths of microglia exceed the entire CA1 layers and reach 500 µm from the surgical surface, where the ML or the granule cell layer (GCL) of the DG exist (Figure 2A; see step 4.7 and Figure 4E). Microglia are slightly less ramified, especially in the layer close to the surgical surface in comparison with those in the intact hippocampus. Nevertheless, they exhibit no prominent activation, suggesting proper surgical procedures (Figure 2B). On the other hand, edema in the CA1 induced by tissue damage will limit the imaging depth to 200 µm (Figure 2C). Tissue damage also induces abnormal microglial activation, such as accumulation of bulging processes toward the free tissue surface (Figure 2D; compare to the upper image of Figure 2B). These are signs of inappropriate surgery.
The representative images of microglia in the chronic phase more than 3 weeks after surgery are shown in Figure 3. Microglia can be imaged again beyond the CA1 to the deeper layers of the DG with higher fluorescent intensity and resolution and with more homogenous distribution (see step 6.3, Figure 3B). Imaging quality is better than that immediately after the surgery (Figure 2A). This difference may be explained by reduced edema and inflammation. Microglia in all layers have already restored their ramified morphology (Figure 3C), different from their postoperative appearance (Figure 2B). Time-lapse imaging of microglia in the CA1 reveals the immobile cell bodies and highly motile processes for surveillance (Video 1–2). Their motile behavior is similar to the previous report of microglial process dynamics in the cortex9.
It is straightforward to specify the imaged hippocampal layers based on the distribution and the depth of neuronal cell bodies, using mice expressing fluorescent probes in the hippocampal neurons25,26,27. Without the aid of the positional information about the neuron cell bodies, the signals from fluorescent microglia alone provide some clues to the identification of hippocampal layers (Figure 3B). Microglia in the alveus have elongated cell bodies and processes which tend to extend along the axonal tracts (Figure 4A). Microglia in other layers can be distinguished by their round cell bodies and processes radiating without preferred directions. Microglia in SP are among the densely packed pyramidal neurons and can be distinguished by the lower density of microglial processes. The layers above and below SP are identified as SO and SR, respectively (Figure 4B). It is impossible to distinguish between SR and SLM based on microglial properties alone. The border between the CA1 and the DG is recognized by thick blood vessels running along the boundary (Figure 4C). These vessels can be better recognized by labeling vessels with dyes such as sulforhodamine 101 (SR101; 5 mM, 4 µL/g body weight) injected intraperitoneally (Figure 4D). The fluorescence signal from microglia drops sharply in the DG compared to the overlying CA1, probably due to the difference in the refractive index of these structures. This gap in fluorescence intensity may also help to specify the border between the DG and CA1. As an application example, simultaneous imaging of GFP-positive microglia and tdTomato-labeled pyramidal neurons is shown (Figure 4E). In this experiment, CX3CR1-GFP mice received an injection of adeno-associated virus (AAV) for the expression of tdTomato in the hippocampal pyramidal neurons. Neuronal labeling will help to understand the exact layer structures of the CA1.
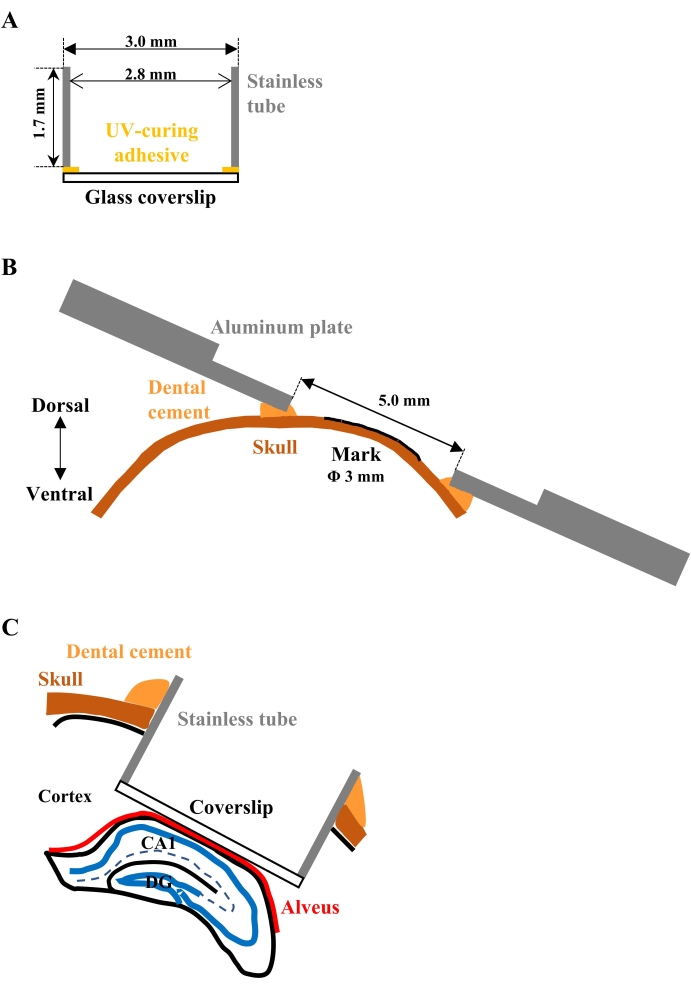
Figure 1: Schematic drawings for the implantation of the observation window. (A) Cross-sectional view of the assembled glass-bottom metal tube. A circular glass coverslip adheres to the one end of the cylindrical stainless tube. (B) Cross-sectional view of the aluminum plate attached to the skull. The plate should be parallel to the marked surface of the skull so as not to interfere with the objective lens, positioned close to the plate for focusing. (C) Cross-sectional view of the implanted tube. The glass bottom should be closely attached to the alveus of the hippocampus to gently press and flatten the surface of the CA1. Please click here to view a larger version of this figure.
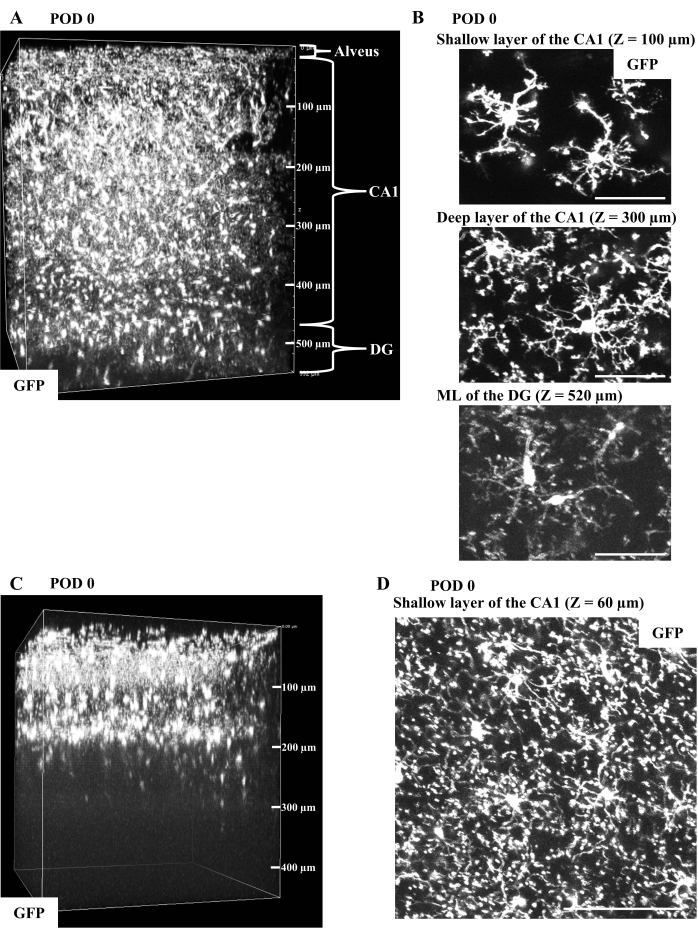
Figure 2: In vivo imaging of microglia in CX3CR1-GFP mice immediately after surgery. (A) Representative 3D reconstruction from the in vivo CA1 imaging of a CX3CR1-GFP mouse on postoperative day (POD) 0 (width: 511 µm, height: 511 µm, depth: 550 µm). The fluorescent microglia in the ML of the DG at a depth of 500 µm from the glass bottom can be imaged through the entire CA1. (B) Typical GFP-filled microglia obtained in (A) are shown as the maximum intensity projections (MIPs) of image stacks with 20 µm thickness at depths of 100, 300, and 520 µm from the glass bottom. Microglial morphology is detectable from the superficial CA1 to the ML of the DG, though with apparent image deterioration in the DG. Microglia especially in the layer close to the surgical surface are less ramified but exhibit no obvious activation. Scale bars, 50 µm. (C) Representative 3D image reconstruction of the surgically damaged CA1. The data was acquired from a CX3CR1-GFP mouse on POD 0 (width: 399 µm, height: 399 µm, depth: 450 µm). Microglial fluorescence is detectable only up to the depth of 200 µm, in contrast with the undamaged CA1 (A) with fluorescent microglia detected at a depth of 500 µm. (D) The typical image of abnormally activated microglia in (C). The MIP of GFP image stacks with 20 µm thickness at a depth of 60 µm shows microglial bulging processes extending toward the surgically exposed tissue surface. The overall microglial morphology is different from the image shown in (B). Scale bar, 100 µm. Please click here to view a larger version of this figure.
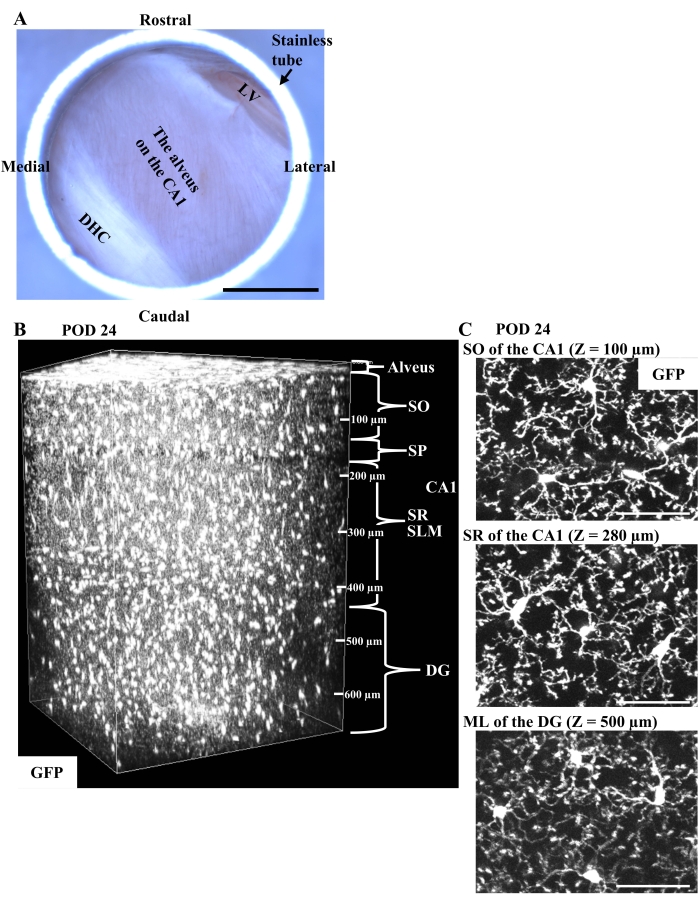
Figure 3: In vivo imaging of microglia in CX3CR1-GFP mice in the chronic phase. (A) The representative appearance of the implanted window on the right dorsal CA1 in the chronic phase. Through the glass bottom, the white fibers of the alveus are clearly observed without postoperative bleeding. The DHC and the LV are partly visible in the caudomedial area and in the rostrolateral edge, respectively. Scale bar, 1 mm. (B) Representative 3D reconstruction from the in vivo chronic CA1 imaging of a CX3CR1-GFP mouse on POD 24 (width: 511 µm, height: 511 µm, depth: 670 µm). Compared to the images immediately after surgery (Figure 2A), microglia show a more homogeneous distribution and can be observed more clearly in the deeper layers of the DG because of the reduction of edema and inflammation. (C) Typical images of microglia from (B) with fully restored ramified morphology are shown as the MIPs of GFP image stacks with 20 µm thickness at depths of 100, 280, and 500 µm from the surgical surface. Scale bars, 50 µm. Please click here to view a larger version of this figure.
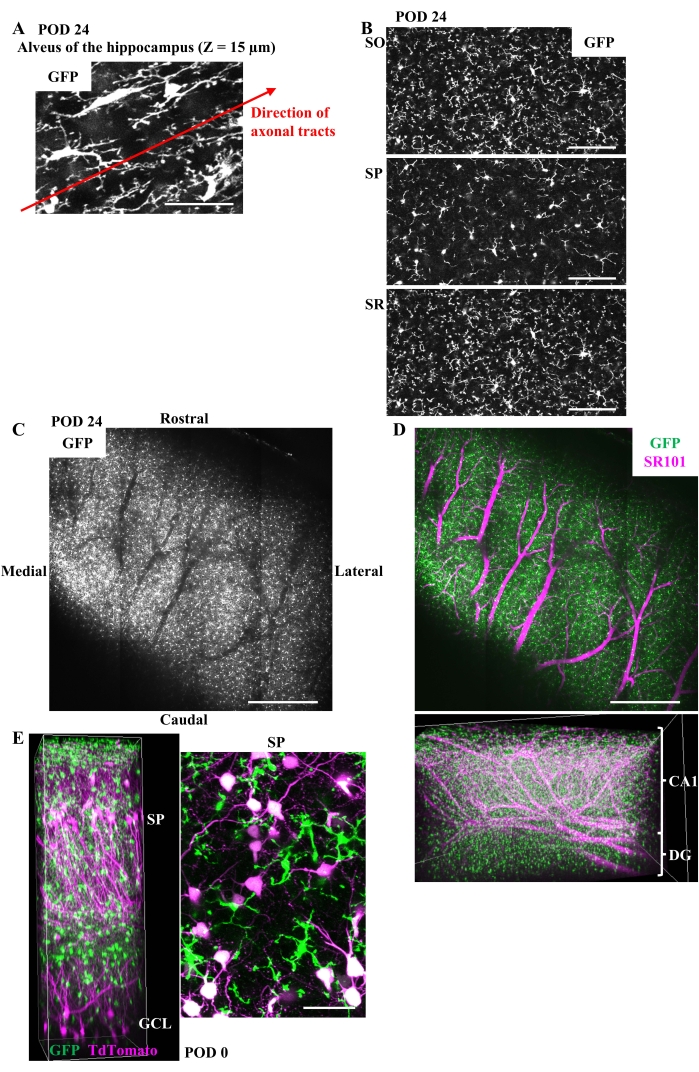
Figure 4: Clues to identifying each layer of the hippocampus during in vivo imaging and an application example of this method. (A) The typical image of microglia in the alveus of CX3CR1-GFP mice in the chronic phase. Microglial cell bodies and processes extending along the axonal tracts are shown in the MIP of GFP image stacks with 10 µm thickness at a depth of 15 µm. Scale bar, 50 µm. (B) Representative images of microglia in SO, SP, and SR in the chronic phase shown as the MIP of GFP image stacks with 5 µm thickness. The local density of microglial processes is lower in SP than in surrounding SO or SR due to the densely packed pyramidal neurons in SP. Scale bars, 100 µm. (C) The thick blood vessels running along the boundary between the CA1 and the DG can be recognized only by the microglial fluorescence. The average intensity projection of tiled GFP image stacks with 90 µm thickness in the chronic phase at a depth of about 500 µm is shown. The void of the GFP signal corresponds to the thick vessels. Scale bar, 500 µm. (D) (Upper) The image of the same field of view as C after intraperitoneal injection of SR101. Scale bar, 500 µm. (Lower) 3D reconstruction of the tiling images after SR101 injection (width: 2.60 mm, height: 1.73 mm, depth: 0.69 mm). The thick vessels running along the border between the CA1 and the DG can be easily recognized by the intravascular SR101 fluorescence. (E) (Left) 3D reconstruction of the CA1 and the DG (width: 255 µm, height: 255 µm, depth: 730 µm) and (right) the MIP of GFP and tdTomato fluorescence in SP made from image stacks with 20 µm thickness. At 1 week before surgery, 1.5 µL of a mixture of AAV1-CAG-FLEX-tdTomato (5.0 x 1012 vg/mL) and AAV1-hSyn-Cre (1.0 x 109 vg/mL) was injected into the hippocampus of a CX3CR1-GFP mouse to label the neurons sparsely. Imaging was performed on POD 0. SP and GCL are easily recognized by the position of neuronal cell bodies. Scale bar, 50 µm. Please click here to view a larger version of this figure.
Video 1: Time-lapse imaging of SO microglia in the chronic phase. The MIP of GFP image stacks with 20 µm thickness in the time-lapse imaging of SO microglia, animated so that 28 min play in 1 sec. Scale bar, 50 µm. Please click here to download this Video.
Video 2: Time-lapse imaging of SR microglia in the chronic phase. The MIP of GFP image stacks with 20 µm thickness in the time-lapse imaging of SR microglia, animated so that 28 min play in 1 sec. Scale bar, 50 µm. Please click here to download this Video.
Discussion
This method contains elaborate surgical procedures, but it can provide high-resolution images over the entire CA1 for an extended period if prepared properly. Experiments with several mice confirmed that the image quality in the chronic postoperative phase is better than that of acute postoperative imaging. The better image quality was maintained for more than 2 months. The most common cause of failure is unintentional damage to the CA1 during surgery, which is identified in the postoperative quality check (see step 4). This can be due to direct injury by aspiration, drying of the brain, excessive pressure by the glass, or toxicity from the dental cement in the final step. Another cause of failure is postoperative bleeding, which can be confirmed through the glass-bottom window within 1 week after surgery (see step 6.1). Read the protocol carefully and take all precautions to avoid such troubles.
Even with the current setup of two-photon microscope with GaAsP detectors in the laboratory, the attempt to image the dorsal CA1 through the cortex results in a significant loss of resolution due to the non-negligible scattering of light. Therefore, to obtain sufficient resolution to observe the movement of microglial processes or the formation of dendritic spines of neurons in the CA1, removing a part of the overlying cortex is inevitable, as in the present method. The only alternative way to reduce the extent of cortical removal while maintaining high image resolution is to embed a relay lens, such as a gradient refractive index (GRIN) lens. In this approach, a GRIN lens has been placed inside a guide tube implanted directly above the CA1 for chronic CA1 imaging28,29. The outer diameter of the guide tube was 1.8 mm, which is smaller than the 3.0 mm of the device in this paper, while producing high resolution (NA; 0.82) comparable to the system here (effective NA; 0.88). However, the approach using a GRIN lens has a narrow field of view for high-resolution observation and a short imaging depth limited by the WD of the GRIN lens. Therefore, imaging all hippocampal layers in a wide field of view with high resolution is a specific advantage of the method in this paper.
A limitation of this procedure is that the partial removal of the cortex and inflammation may have some detrimental effects on the hippocampus. However, because the removed cortex has no direct input to the hippocampus, the entorhinal cortex is not damaged, and the hippocampus itself is not directly injured, the overall evaluation is that the functional impairment of the hippocampus is not significant. Several previous studies have confirmed that hippocampal functions, including learning and memory, are preserved after hippocampal window implantation25,26,27,30,31,32,33,34. Therefore, the imaging approach described here is expected to faithfully report hippocampal functions after a sufficient postoperative period.
Future directions of research subjects based on this imaging technique may include synaptic pruning detected by simultaneous imaging of microglia and neurons5, learning-related microglial interaction with synapses35, microglial motility regulated by the hippocampal neural activity36, and microglial responses to peripheral inflammation or tissue damage7. This method will also help elucidate the progression of neurodegenerative diseases. For example, in Alzheimer's disease (AD), amyloid β and tau proteins accumulate in parallel with neuronal cell deaths and hippocampal atrophy, leading to cognitive dysfunction; microglia have been reported to be involved in this process37,38. In vivo chronic imaging of microglia and neurons using the AD mouse models will enable us to monitor the correlation between microglial functions and neuronal pathology in the hippocampus of the AD mouse models.
This paper focuses on microglial imaging, but the same imaging procedure is applicable to the other neuronal and glial cell types in the CA1. In addition, the protocol is limited to the imaging of anesthetized mice, but the technique can also be extended to monitoring hippocampal microglia in awake mice. The motion artifacts induced by respiration, heartbeats, and body movements, especially in the deep hippocampal layers away from the glass window, may exist in experiments with awake mice. Therefore, an appropriate motion correction system may be required to capture microglial morphology and dynamics.
Discussion related to the Protocol
It is advisable to select mice of appropriate age and genetic modifications for the expression of fluorescent probes with temporal and spatial specificity (see step 1.3). Mice at 1 month of age can be used for experiments, but mice older than 2 months are easier to handle, with their larger body size and resistance to surgical stress. In addition, the external capsule and the alveus of the hippocampus are more difficult to separate in younger mice. Therefore, removing the external capsule in young mice requires surgical skills (see steps 3.4.3-4). Assessment of the surgery and subsequent imaging will be more straightforward with mice expressing fluorescent proteins reproducibly and uniformly in the CA1 and the DG (see step 4.7). Hence, in the initial trials of the surgery, it is advisable to use transgenic mice with sparsely labeled neurons, such as Thy1-YFP or Thy1-GFP mice39, or mice with labeled microglia, such as CX3CR1-GFP mice24.
For successful surgery, the choice of anesthesia is important (see step 2.1). Different types of anesthesia can cause various degrees of intraoperative brain edema, which affect the difficulty of the surgery, the relative position of the implanted metal tube, and the extent of brain compression by the glass window. These factors may also influence the survival of hippocampal neurons after surgery.
In the aspiration process to expose the hippocampus (see step 3.4), the following points should be noted to minimize the damage to the brain and ensure successful imaging. Constantly supply sterile saline onto the tissue surface by positioning an outlet at the side of the cranial window. Prevent the tissue surface from exposure to air during aspiration. The basic principle of tissue aspiration is removing the tissue surface by a liquid flow into the suction tip. Direct contact of the suction tip to the tissue should be avoided. Adjust the negative pressure applied to the suction tube to be minimum. Aspirate the tissue step by step and confirm that bleeding is controlled in each step. When bleeding is prolonged, wait until the bleeding stops spontaneously. Keep aspiration from a short distance from the bleeding spot with a constant flow of sterile saline. Aspirate the tissue to create a cylindrical space with its size fitting to the glass-bottom metal tube (see step 1.1). Choose 23 G needles to aspirate thick pial vessels or large tissue fragments and 25 G needles to suck small tissue debris.
Divulgations
The authors have nothing to disclose.
Acknowledgements
We would like to thank M. Kondo and M. Matsuzaki for lending us the XLPLN25XSVMP objective lens. This work was financially supported from Japan Society for the Promotion of Science (JSPS) by Grant-in-Aid for JSPS Research Fellow (18J21331 to R.K.) and Grants-in-Aid for Scientific Research (20H00481, 20A301, 20H05894, 20H05895 to S.O.), from the Japan Agency for Medical Research and Development (JP19gm1310003 and JP17gm5010003 to S.O.), and from the Japan Science and Technology Agency by Moonshot R&D (JPMJMS2024 to H.M.).
Materials
| 23 G blunt needles | NIPRO | 02-166 | Suction tips for aspiration. |
| 25 G blunt needles | NIPRO | 02-167 | Suction tips for aspiration. |
| 3 mm dermal punches (DermaPunch) | Maruho | 213001610 | Tools for craniotomy. |
| 30 G needles | Dentronics | Disposable needle No. 30 | Tools for craniotomy. |
| A femtosecond pulsed laser | Spectra-Physics | MaiTai Deep See | A Ti:Sapphire laser used at 920 nm wavelength. |
| A two-photon microscope | Nikon | A1R MP+ | Microscope for the CA1 imaging. |
| AAV1-CAG-FLEX-tdTomato | Penn Vector Core | AAV for neuronal labeling. | |
| AAV1-hSyn-Cre | Penn Vector Core | AAV for neuronal labeling. | |
| An objective lens for two-photon imaging | Olympus | XLPLN25XSVMP | 25× objective with a long working distance, a high numerical aperture, and a correction collar |
| Aspirators | Shin-ei Industries | KS-500 | Tools for aspiration. |
| Aluminum plates | Narishige | CP-1 | Plates made of alminum for head fixation. |
| Chemical depilatory cream | YANAGIYA | Cream for hair removal around the surgical site. | |
| Circular glass coverslips | Matsunami Glass | 3φ No.1 | Coverslips bonded to stainless steel tubes. |
| CX3CR1-GFP mice | The Jackson Laboratory | 008451 | Transgenic mice for microglial imaging. |
| Cylindrical stainless steel tubes | MORISHITA | Custom-made | Metal tubes to be implanted. Outer diameter 3.0 mm, inner diameter 2.8 mm, height 1.7 mm. |
| Dental etching material | Sun Medical | 204610461 | Used to etch the skull bones. |
| Dental resin cement (Super-Bond C&B) | Sun Medical | 204610555 | Dental cement. |
| Dura pickers (Micro Points) | Fine Science Tools | 10063-15 | Tools for dura removal. |
| Fine forceps (Dumont #5) | Fine Science Tools | 11252-20 | Surgical tools. |
| Forceps | Bio Research Center | PRI13-3374 | Used to disinfect the surgical site. |
| Head holding device | Narishige | MAG-2 | The head holding device of mice with angle adjusters |
| Heating pad | Bio Research Center | BWT-100A and HB-10 | Tools to provide thermal support for the mouse during surgery. |
| Heating pad | ALA Scientific | HEATINGPAD-1 and Hot-1 | Tools to provide thermal support for the mouse on the head holding device. |
| Ketamine (Ketalar) | Daiichi Sankyo Company | S9-001665 | Anesthesia during surgery. |
| Meloxicam | Tokyo Chemical Industry | M1959 | Analgesia during surgery. |
| Ophthalmic ointment | Sato Pharmaceutical | Used to prevent eye dryness during surgery. | |
| Povidone-iodine scrub solution | Meiji Seika Pharma | 2612701Q1137 | Used to disinfect the surgical site. |
| Round-tipped miniature knives | Surgistar | 4769 | Surgical tools. |
| Scalpel | MURANAKA MEDICAL INSTRUMENTS | 450-098-67 | Disposable surgical tool. |
| Stereo microscopes | Leica Microsystems | S8 APO | Microscopes for surgery. |
| Sterile saline | Otsuka Pharmaceutical Factory | 3311401A2026 | Washing solution during surgery. |
| Sterile waterproof pad | AS ONE | 8-5945-01 | Surgical platform. |
| Sulforhodamine 101 | Sigma-Aldrich | S7635 | A dye for in vivo vessel imaging. |
| Surgical drape | Medline Industries | MP-0606F6T | Perforated drape for surgery. |
| UV light | Toshiba | GL15 | Used to cure the adhesives. |
| UV-curing optical adhesives | Thorlabs | NOA81 | Adhesives for bonding coverslips to stainless steel tubes. |
| Xylazine (Celactal 2%) | Bayer | Anesthesia during surgery. |
References
- Wolf, S. A., Boddeke, H. W. G. M., Kettenmann, H. Microglia in physiology and disease. Annual Review of Physiology. 79, 619-643 (2017).
- Wake, H., Moorhouse, A. J., Miyamoto, A., Nabekura, J. Microglia: actively surveying and shaping neuronal circuit structure and function. Trends in Neurosciences. 36 (4), 209-217 (2012).
- Wu, Y., Dissing-Olesen, L., MacVicar, B. A., Stevens, B. Microglia: dynamic mediators of synapse development and plasticity. Trends in Immunology. 36 (10), 605-613 (2015).
- Nakayama, H., et al. Microglia permit climbing fiber elimination by promoting GABAergic inhibition in the developing cerebellum. Nature Communications. 9 (1), 2830 (2018).
- Iida, T., Tanaka, S., Okabe, S. Spatial impact of microglial distribution on dynamics of dendritic spines. The European Journal of Neuroscience. 49 (11), 1400-1417 (2019).
- Kettenmann, H., Hanisch, U., Noda, M., Verkhratsky, A. Physiology of microglia. Physiological Reviews. 91 (2), 461-553 (2011).
- Kondo, S., Kohsaka, S., Okabe, S. Long-term changes of spine dynamics and microglia after transient peripheral immune response triggered by LPS in vivo. Molecular Brain. 4 (1), 27 (2011).
- Benninger, R. K. P., Piston, D. W. Two-photon excitation microscopy for the study of living cells and tissues. Current Protocols in Cell Biology. 59 (1), 4-11 (2013).
- Nimmerjahn, A., Kirchhoff, F., Helmchen, F. Resting microglial cells are highly dynamic surveillants of brain parenchyma in vivo. Science. 308 (5726), 1314-1318 (2005).
- Davalos, D., et al. ATP mediates rapid microglial response to local brain injury in vivo. Nature Neuroscience. 8 (6), 752-758 (2005).
- Tremblay, M., Lowery, R. L., Majewska, A. K. Microglial interactions with synapses are modulated by visual experience. PLoS Biology. 8 (11), 1000527 (2010).
- Miyamoto, A., et al. Microglia contact induces synapse formation in developing somatosensory cortex. Nature Communications. 7, 12540 (2016).
- Akiyoshi, R., et al. Microglia enhance synapse activity to promote local network synchronization. eNeuro. 5 (5), 0088 (2018).
- Favuzzi, E., et al. GABA-receptive microglia selectively sculpt developing inhibitory circuits. Cell. 184 (15), 4048-4063 (2021).
- Svoboda, K., Yasuda, R. Principles of two-photon excitation microscopy and its applications to neuroscience. Neuron. 50 (6), 823-839 (2006).
- Isshiki, M., Okabe, S. Evaluation of cranial window types for in vivo two-photon imaging of brain microstructures. Microscopy. 63 (1), 53-63 (2014).
- Grabert, K., et al. Microglial brain region-dependent diversity and selective regional sensitivities to aging. Nature Neuroscience. 19 (3), 504-516 (2016).
- De Biase, L. M., et al. Local cues establish and maintain region-specific phenotypes of basal ganglia microglia. Neuron. 95 (2), 341-356 (2017).
- Ayata, P., et al. Epigenetic regulation of brain region-specific microglia clearance activity. Nature Neuroscience. 21 (8), 1049-1060 (2018).
- Böttcher, C., et al. Human microglia regional heterogeneity and phenotypes determined by multiplexed single-cell mass cytometry. Nature Neuroscience. 22 (1), 78-90 (2019).
- Masuda, T., et al. Spatial and temporal heterogeneity of mouse and human microglia at single-cell resolution. Nature. 566 (7744), 388-392 (2019).
- Paolicelli, R. C., et al. Synaptic pruning by microglia is necessary for normal brain development. Science. 333 (6048), 1456-1458 (2011).
- Wang, C., et al. Microglia mediate forgetting via complement-dependent synaptic elimination. Science. 367 (6478), 688-694 (2020).
- Jung, S., et al. Analysis of fractalkine receptor CX3CR1 function by targeted deletion and green fluorescent protein reporter gene insertion. Molecular and Cellular Biology. 20 (11), 4106-4114 (2000).
- Gu, L., et al. Long-term in vivo imaging of dendritic spines in the hippocampus reveals structural plasticity. The Journal of Neuroscience. 34 (42), 13948-13953 (2014).
- Dombeck, D. A., Harvey, C. D., Tian, L., Looger, L. L., Tank, D. W. Functional imaging of hippocampal place cells at cellular resolution during virtual navigation. Nature Neuroscience. 13 (11), 1433-1440 (2010).
- Schmid, L. C., et al. Dysfunction of somatostatin-positive interneurons associated with memory deficits in an Alzheimer’s disease model. Neuron. 92 (1), 114-125 (2016).
- Barretto, R. P., Messerschmidt, B., Schnitzer, M. J. In vivo fluorescence imaging with high-resolution microlenses. Nature Methods. 6 (7), 511-512 (2009).
- Attardo, A., Fitzgerald, J. E., Schnitzer, M. J. Impermanence of dendritic spines in live adult CA1 hippocampus. Nature. 523 (7562), 592-596 (2015).
- Sheffield, M. E. J., Dombeck, D. A. Calcium transient prevalence across the dendritic arbour predicts place field properties. Nature. 517 (7533), 200-204 (2015).
- Attardo, A., et al. Long-term consolidation of ensemble neural plasticity patterns in hippocampal area CA1. Cell Reports. 25 (3), 640-650 (2018).
- Kaifosh, P., Lovett-Barron, M., Turi, G. F., Reardon, T. R., Losonczy, A. Septo-hippocampal GABAergic signaling across multiple modalities in awake mice. Nature Neuroscience. 16 (9), 1182-1184 (2013).
- Lovett-Barron, M., et al. Dendritic inhibition in the hippocampus supports fear learning. Science. 343 (6173), 857-863 (2014).
- Hainmueller, T., Bartos, M. Parallel emergence of stable and dynamic memory engrams in the hippocampus. Nature. 558 (7709), 292-296 (2018).
- Parkhurst, C., et al. Microglia promote learning-dependent synapse formation through brain-derived neurotrophic factor. Cell. 155 (7), 1596-1609 (2013).
- Merlini, M., et al. Microglial Gi-dependent dynamics regulate brain network hyperexcitability. Nature Neuroscience. 24 (1), 19-23 (2021).
- Sarlus, H., Heneka, M. T. Microglia in Alzheimer’s disease. Journal of Clinical Investigation. 127 (9), 3240-3249 (2017).
- Hansen, D. V., Hanson, J. E., Sheng, M. Microglia in Alzheimer’s disease. Journal of Cell Biology. 217 (2), 459-472 (2018).
- Feng, G., et al. Imaging neuronal subsets in transgenic mice expressing multiple spectral variants of GFP. Neuron. 28 (1), 41-51 (2000).

