Electromagnetic Controlled Closed-Head Model of Mild Traumatic Brain Injury in Mice
Summary
The protocol describes mild traumatic brain injury in a mouse model. In particular, a step-by-step protocol to induce a mild midline closed head injury and the characterization of the animal model is fully explained.
Abstract
Highly reproducible animal models of traumatic brain injury (TBI), with well-defined pathologies, are needed for testing therapeutic interventions and understanding the mechanisms of how a TBI alters brain function. The availability of multiple animal models of TBI is necessary to model the different aspects and severities of TBI seen in people. This manuscript describes the use of a midline closed head injury (CHI) to develop a mouse model of mild TBI. The model is considered mild because it does not produce structural brain lesions based on neuroimaging or gross neuronal loss. However, a single impact creates enough pathology that cognitive impairment is measurable at least 1 month after injury. A step-by-step protocol to induce a CHI in mice using a stereotaxically guided electromagnetic impactor is defined in the paper. The benefits of the mild midline CHI model include the reproducibility of the injury-induced changes with low mortality. The model has been temporally characterized up to 1 year after the injury for neuroimaging, neurochemical, neuropathological, and behavioral changes. The model is complementary to open skull models of controlled cortical impact using the same impactor device. Thus, labs can model both mild diffuse TBI and focal moderate-to-severe TBI with the same impactor.
Introduction
Traumatic brain injury (TBI) is caused by an external force on the brain, often associated with falls, sports injuries, physical violence, or road accidents. In 2014, the Centers for Disease Control and Prevention determined that 2.53 million Americans visited the emergency department to seek medical help for TBI-related accidents1. Since mild TBI (mTBI) represents the majority of TBI cases, over the past several decades, multiple models of mTBI have been adopted, which include weight drop, piston-driven closed head injury and controlled cortical impact, rotational injury, mild fluid percussion injury, and blast injury models2,3. The heterogeneity of the mTBI models is useful to address the different features associated with mTBI seen in people and to help evaluate the cellular and molecular mechanisms associated with brain injury.
Of the commonly used models of closed head injury, one of the first and most widely used models is the weight drop method, where an object is dropped from a specific height onto the animal's head (anesthetized or awake)2,4. In the weight drop method, the injury's severity depends on several parameters, including craniotomy performed or not, head fixed or free, and the distance and weight of the falling object2,4. One disadvantage of this model is the high variability in the severity of the injury and the high mortality rate associated with respiratory depression5,6. A common alternative is to deliver the impact using a pneumatic or electromagnetic device, which can be done directly on the exposed dura (controlled cortical impact: CCI) or closed skull (closed head injury: CHI). One of the strengths of the piston-driven injury is its high reproducibility and low mortality. However, CCI requires craniotomy7,8, and a craniotomy itself induces inflammation9. Instead, in the CHI model, there is no need for craniotomy. As already stated, each model has limitations. One of the limitations of the CHI model described in this paper is that the surgery is performed using a stereotaxic frame, and the head of the animal is immobilized. While the full head immobilization assures reproducibility, it does not account for movement after the impact that could contribute to the injury associated with a mTBI.
This protocol describes a basic method to perform a CHI impact with a commercially available electromagnetic impactor device10 in a mouse. This protocol details the exact parameters involved to achieve a highly reproducible injury. In particular, the investigator has precise control over the parameters (depth of injury, dwell time, and velocity of impact) to precisely define the injury severity. As described, this CHI model produces an injury that results in bilateral pathology, both diffuse and microscopic (i.e., chronic activation of glia, axonal and vascular damage), and behavioral phenotypes11,12,13,14,15. In addition, the described model is considered mild as it does not induce structural brain lesions based on MRI or gross lesions on pathology even 1 year after the injury16,17.
Protocol
The experiments performed were approved by the Institutional Animal Care and Use Committee (IACUC) of the University of Kentucky, and both the ARRIVE and the Guide for the Care and Use of Laboratory Animals guidelines were followed during the study.
1. Surgical setup
NOTE: Mice are housed in groups of 4-5/cage, humidity in the housing room is maintained at 43%-47%, and the temperature is maintained at 22-23 ˚C. Mice are given ad libitum access to food and water and exposed to a 12 h/12 h light/dark cycle (7 a.m./7 p.m.).
- Use a designated surgical area, such as a hood or dedicated surgical procedure room, to perform the animal surgery.
- Ensure that the surgical area includes a heating pad, a stereotaxic frame equipped with an electromagnetic impactor, and an anesthesia mask designed to administer isoflurane gas (see Figure 1A).
- Ensure that the surgeon or personnel involved in the surgery wear a clean lab coat, a face mask, gloves, and a surgical cap.
- Use sterile surgical tools, sterile cotton-tipped applicators, and gauze pads. Use a hot bead sterilizer to sterilize the instruments between mice during the day of surgery.
- Use an anesthesia induction chamber to prepare the mouse for surgery in a pre-op area.
- Use heating pads to maintain the animal's temperature, clean post-op mouse holding cages, and timers to record the righting reflex of the mouse after surgery.
2. Pre-surgery procedure
- Prepare the head support apparatus (see Figure 1B).
- Remove the rolled end ridge from a 1 mL latex pipette bulb (inflatable end) (see Figure 1C).
- Attach the bulb to the tubing using parafilm (see Figure 1C).
- Connect the tubing to a 10 mL syringe using a stopcock. Fill the syringe with water (see Figure 1C).
NOTE: The 1 mL latex pipette bulb will be placed under the mouse's head to displace the impact force away from the ears. Try to remove as much air as possible from the bulb before use so that the bulb is filled with mostly water and not air.
- Impactor setup.
- Select the 5 mm probe tip, screw it to the piston at the bottom center of the actuator (inside the larger cylinder), and gently tighten the probe without applying excessive force. Re-tighten the tip between impacts (see Figure 1B).
- Before turning on the impactor, ensure that the Extend/Retract switch is positioned in the center Off position. Then, connect the cable on the actuator to the jack on the front panel of the impactor control box and the sensor cable to the jack on the front panel. Then, turn on the power switch on the back panel (see Figure 1D).
NOTE: The Extend/Retract toggle switch needs to remain in the center Off position when not in use. - Set up the impact velocity by rotating the large knob on the left side of the control box until an impact velocity of 5.0 ± 0.2 m/s appears on the display (see Figure 1D).
- Set the dwell counter to 100 ms by turning the dials until the dwell reads 0.01 (see Figure 1D).
NOTE: The dwell is the time of contact before automatic retraction occurs. - Place the impactor actuator on an ice pack to prevent the plastic cylinder from expanding, which locks the cylinder in place, preventing the movement of the cylinder and the delivery of future impacts (see Figure 1E).
- Prepare the mouse for surgery.
- Visually inspect the mouse before surgery and eliminate the mouse from the study if one of the following conditions is observed: poor coat condition, lethargy, or poor weight (<20 g) for a 4-month-old mouse.
- Anesthetize the mouse with 4%-5% isoflurane in 100% oxygen using an induction chamber placed on a heating pad for 1-2 min.
- Shave the fur from the operative site using an electric hair clipper.
- Clean the head with sterile alcohol prep pads and apply a topical anesthetic to the shaved scalp at least 15 min before the start of the surgery.
- Return the mouse to a clean holding cage before the surgery. Start the surgery after at least 15 min of topical anesthetic application (induction time).
NOTE: The time for anesthesia could vary depending on the anesthetic used in the procedure.
- Check one more time that the stereotaxic frame, impactor, and digital stereotaxic display (see Figure 1F) are ready to be used.
- Return the mouse to the isoflurane induction chamber with 4%-5% isoflurane in 100% oxygen for approximately 3 min.
- Fix the mouse in the head stage.
3. Surgical procedure
- Secure the mouse into the stereotaxic frame using lightweight acetal resin tapered point ear bars, a bite bar, and a mouse anesthesia mask (see Figure 1G,H). The isoflurane gas is delivered at 2%-3% in room air at 100-200 mL/min. Carefully monitor the mouse's respiration to ensure the depth of anesthesia and adjust the level of gas as needed.
- Apply sterile eye lubricant to the eyes to prevent corneal drying.
- Sterilize the scalp with povidone-iodine swabs and sterile alcohol pads three times.
- Ensure the mouse is deeply anesthetized by verifying the lack of a toe-pinch response.
- Make an approximately 1 cm midline scalp incision between the eyes and neck using a scalpel, exposing the skull (see Figure 1I).
- Allow the skull to dry for 1-2 min.
- Identify bregma (the intersection point of the coronal and sagittal sutures) and lambda (the intersection of the sagittal and lambdoid sutures) (see Figure 1J).
NOTE: A mouse brain atlas could be used for reference. - Place the head support apparatus under the head and inflate the bulb with water until it is pressing against the bottom of the mouse's head but not lifting the head away from the bite bar.
NOTE: This step is essential to reduce possible ear issues from the CHI. Any animal with damage to the ear from the ear bars, resulting in rolling or bleeding, should be eliminated from the study and euthanized. - Move the impactor into place over the animal's head.
- Extend the impactor by placing the Extend/Retract toggle switch (on the impactor control box) on Extend.
NOTE: Be sure to check that the tip is fully extended by pulling down on the tip. - Line up the impactor until it is centered over the bregma (see Figure 1K).
- Reset the digital stereotaxic x and y coordinates in the stereotaxic reader to 0 (on the touch screen control)
- Align the probe over the impact location by moving the probe from the bregma over to the target coordinates: medial-lateral = 0.0 mm, anterior-posterior = −1.6 mm.
- Clip the contact sensor to the animal's ear.
- Slowly lower the probe tip with the extended probe until first contact with the surface is made. Stop at the beep.
- Reset the digital stereotaxic z coordinates in the stereotaxic reader to 0.
- Carefully inspect if the tip is flush with the skull (medial-lateral and anterior-posterior planes).
NOTE: Positioning the probe tip is the most crucial step of this process to prevent skull fractures and ear damage. - Retract the impactor by placing the toggle switch on the control box in the Retract position. The tip withdraws and has no more contact with the animal's head until the time of impact.
- Set the impact depth by adjusting the dorsal-ventral depth to −1.2 mm.
NOTE: The depth of the impact affects the severity of the injury. The depth should be titered for different ages, weights, and strains of mice to the desired injury severity. The depth may need to be adjusted/re-titered over time to maintain a consistent injury severity. The severity can be assessed neuropathologically: microglia and astrocytes (IHC), and behaviorally: the radial arm water maze and the active avoidance test. - Carefully monitor the mouse's respiration to ensure the anesthesia depth and adjust the gas level as needed.
NOTE: Often, the percentage of isoflurane gas should be lowered or shut off for 10-20 s prior to impact. Watch closely for the respiration to accelerate slightly. If respiration is too slow at the time of impact, the animal may die within the first 60 s after the impact from apnea. This can be prevented by adjusting the depth of anesthesia in the seconds before the impact. - Induce the impact by pressing the right toggle switch to impact. The probe tip goes down at the displayed velocity, and then stays down for the set dwell time and retracts.
NOTE: Sham mice receive identical handling to the CHI mice, but the impact is not delivered. - Start the timer immediately after the CHI impact is delivered to record the righting times (time to return from the side position to the prone position) or start the timer when the mouse is removed from the stereotaxic frame for the sham mice. The average righting reflex time is 5-15 min.
NOTE: The righting reflex times may vary based on mouse strain and age. - Evaluate the mice for visible skull fractures, hemorrhages, and apnea. Exclude the mice with a depressed skull fracture or visible hemorrhage from the study.
NOTE: There are graded levels of skull fractures. Animals with decompressed skull fractures, where the bone is observably pressing into the brain tissue, are euthanized (CO2 first, and decapitation used as a secondary method). If the impactor tip is set correctly, these types of skull fractures are exceedingly rare. If a skull fracture does occur, the more common presentation is a small drop of blood on the skull and a slight tactile roughing of the skull, often along the suture connecting the posterior tip of the nasal bone. These mice are noted as possible skull fracture in the records but are not normally excluded from the study. - Remove the animal from the stereotaxic frame.
- Close the scalp by stapling the skin together.
NOTE: Absorbable or non-absorbable sutures could be used to close the scalp as an alternative to staples. - Apply triple antibiotic ointment with a sterile cotton-tipped applicator to the closed incision.
- Return the mouse to a clean holding cage for recovery. Half of the recovery cage is on a heating pad (low setting), providing the ability to move away from the heat when awake and maintaining the animal's temperature while unconscious (see Figure 1L).
NOTE: The mouse is placed on its side in the recovery cage. To prevent suffocation, place the animal in a recovery cage without bedding or on a tissue if bedding is in the cage. - Return the Extend/Retract toggle switch to the Center/Off position.
NOTE: The current will continue running if the switch is left in either the extend or retract position, causing the piston to swell. The impactor will then not be functional until the piston cools down. - Remove the impactor from its holder and gently place it on the ice pack.
NOTE: Keeping the impactor on an ice pack helps reduce the potential swelling of the impactor. - Monitor the animal until the righting reflex occurs and document the time until righting (see Figure 1M).
NOTE: The righting reflex is defined as the moment the mouse returns to a prone position. The cage needs to be left undisturbed; the mouse could right if the cage is touched, moved, or exposed to some noises. - Return the mice to their home cage when they are awake and alert. Usually, within 1 h after injury, animals are fully conscious and ambulating. Also, add some moist food at the bottom of the cage.
4. Post-surgery care
- Monitor the animals for 5 days post-surgery.
- Record their weight and any physical/ behavioral changes like breathing rate (qualitative respiratory function), gait, body and hair coat condition, eating, drinking, defecation, and urination.
- Observe the mouse for any sign of discomfort and the surgical wound for swelling, exudates or red edges, ordehiscence. Contact a veterinarian if the animal shows signs of pain and discomfort (vocalizations, not moving, hypothermia, does not drink or eat).
- Remove the staples 7-10 days post-surgery under anesthesia and on a heating pad.
NOTE: If non-absorbable sutures are used, they must be removed 7-10 days post-surgery under anesthesia.
5. Cleaning
- Clean and sterilize the surgical area and tools.
- Clean the probe tip after each use and at the end of the day with alcohol prep pads.
NOTE: The impactor is calibrated at the factory and is reported to be stable over time and use. No routine calibration is needed. However, the impactor and stereotaxic frame should be routinely inspected. Also, the model endpoint perimeters such as righting reflex time, mortality, and neuropathology should be monitored to evaluate possible experimental drift.
6. Exclusion criteria
- Exclude animals prior to surgery with a poor health condition, like poor weight <20 g for a 4-month-old mouse, lethargy, and poor coat condition.
- Exclude animals with complications during surgery like a depressed skull fracture, a visible hemorrhage related to surgery, or ear bleeding.
- Exclude animals from the study with the following post-surgery symptoms: failure to eat and/or to move normally, unusual vocalizations, weight loss, or failure of the wound to heal normally after surgery.
NOTE: This model could be used as a repetitive model of mild TBI. If the mice receive the second surgery 24 h apart from the first one, the staples or suture could be removed, and the same incision could be used to expose the skull. A new incision needs to be made if a longer time elapses between the surgeries.
Representative Results
This stereotaxic electromagnetic impactor device is versatile. It is used for both an open skull controlled cortical impact (CCI) or a closed head injury (CHI) surgery. Furthermore, the injury severity can be modulated by changing the injury parameters such as impact velocity, dwell time, impact depth, impactor tip, and injury target. Herein is described a CHI surgery using a 5.0 mm steel tip impactor. This injury is considered mild because there are no structural brain lesions. The mortality rate in adult mice is less than 0.9%11,14 and increases slightly to reach ~2.5% in older mice (>8 months old)11. Mortality occurs during the first 2 min because of apnea, which can largely be prevented by carefully monitoring the depth of anesthesia in the seconds before the impact.
The advantage of this CHI model is that the impact produces bilateral diffuse pathology without needing to expose the cortical dural surface (craniotomy). Another feature that makes this an effective TBI model is that less than 1% of mice are excluded from the study due to skull fractures or ear issues following the surgical procedure. Importantly the model produces neuropathological and behavioral impairments with a single impact, which reduces the experimental complexity associated with repetitive mild CHI models15. For instance, a reproducible temporal pattern of microglia and astrocyte morphological changes are identified11 (Figure 2A,B). When validating the model, it is recommended to use the starting ranges of the anterior-posterior coordinates as −1.5 mm ± 0.2 mm and the impact depth as 1.0 ± 0.2 mm. The coordinates may need to be adjusted for the age and strain of the mice, as well as the brand and model of the equipment used. Once the settings have been validated, they should be held constant for an experiment. For validation, the neuropathological characterization of microglia and astrocytes at 3 days post-injury is recommended. Immunohistochemical (IHC) staining was completed following the methods in Bachstetter et al.18. Specifically, 30 μm coronal free-floating sections were stained for glial activation with rabbit anti-GFAP (1:10,000) and for astrocytes using a rabbit anti-IBA1 (1:10,000). An HRP conjugated goat anti-rabbit IgG (1:200) was used to detect both GFAP and IBA-1. Quantification software was used to quantify the staining in each region considered. In addition, at 1-day post-injury, axonal injury markers were found in the neocortex, and changes in mitochondrial metabolism were found by 28 days post-CHI16 (data not shown).
The secondary endpoints for validating the model would be behavioral assays. Reproducible CHI-induced deficits in the radial arm water maze (RAWM)12 and active avoidance13 behaviors were found (Figure 3). The mice were tested in an 8-arm RAWM, a special learning test, as described in Macheda et al.12. Briefly, the mice were tested in a total of 28 trials over a 4 day protocol and had 60 s to locate the platform positioned in the target arm. The total number of trials per day was seven; day 1 and day 2 were considered as training days and day 3 and 4 as testing days. During the training days, the mice were trained to locate the platform, alternating between visible and hidden trials; during the testing days, the platform was hidden during all trials. The experiments were recorded using a camera, and a tracking system was used for behavior analysis (number of errors, total distance, and latency). The mice were tested 2 weeks post-injury. While there was no effect of sex, the CHI mice made more errors to successfully perform the task and reach the platform (Figure 3A). Furthermore, memory impairments have been detected in a 6-arm RAWM test11,14,15,16 as well. Active avoidance, an associative learning-based test, has been used to measure the cognitive deficits associated with this mild model of CHI. The mice were tested using a 5 day protocol and exposed to 50 trials/day13. The mice were trained to avoid a mild foot shock (unconditioned stimulus, US) by associating a conditioned stimulus (CS, light) with it. Over time, the mice learned to avoid the US when the CS was presented. The CHI mice had impaired cognitive function in active avoidance compared to sham mice (Figure 3B). The sham female mice learned significantly faster compared to the males, but the sex did not play a role in CHI mice13. Behavior was recorded using active/passive avoidance software. A reproducible deficit in motor function beyond the first week after the injury has not been detected11.
In this mild TBI model, no gross structural lesions to the brain were found, and a single impact induced bilateral glial activation and changes in microglia morphology. Also, cognitive deficits are associated with this TBI model.
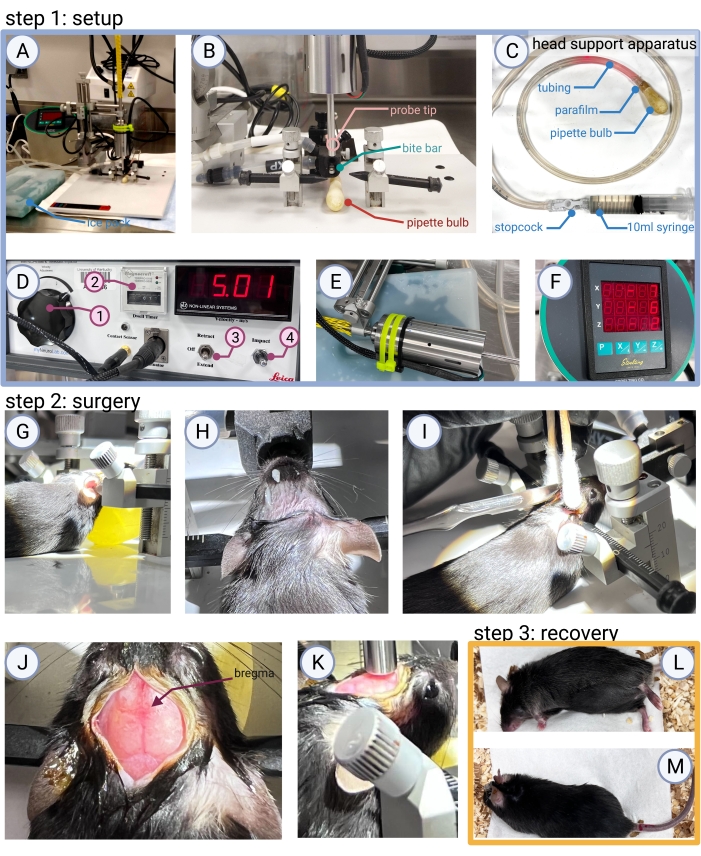
Figure 1: Step 1: Surgical area setup. (A) An example of the surgical area and tools needed to perform CHI surgery (ice pack for the impactor, stereotaxic frame equipped with the impactor, impactor control box, and surgical tools) is shown. (B) A close-up view of the 5 mm steel probe tip, bite bar, and head support apparatus, which illustrates the positioning needed for the midline impact. (C) The head support apparatus is made from a 1 mL latex pipette bulb attached to the tubing by parafilm. A 10 mL syringe is filled with water to inflate the bulb, with a stopcock to keep the bulb inflated once in position. (D) Impactor control box: (1) a large knob to adjust the impact velocity, (2) a dwell counter, (3) an extend/retract toggle switch, (4) a toggle switch that, when pushed down, will deliver the impact. (E) When not in use, the impactor is kept on an ice pack to prevent overheating and possible malfunctioning. (F) A digital stereotaxic display is used for establishing the x (anterior-posterior), y (medial-lateral), and z (dorsal-ventral) coordinates. Step 2: Surgical procedure. (G,H) The anesthetized and shaved mouse is secured into the stereotaxic frame, (I) a midline incision is made to expose the (J) bregma, (K) which is used during surgery to line up the impactor. Step 3: Recovery. (L) The mouse is removed from the stereotaxic frame. After the scalp is closed by stapling or suturing the skin together, it is placed in a clean recovery cage on its side. (M) The mouse is monitored until the mouse rolls over and the righting reflex occurs. Please click here to view a larger version of this figure.
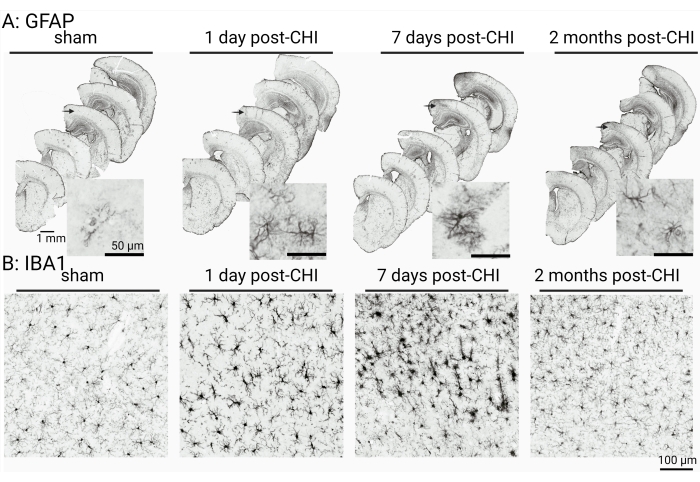
Figure 2: The temporal patterns of astrocyte (GFAP) and microglia (IBA1) morphological changes after a CHI. (A) GFAP staining at low magnification shows the regional increase in staining seen in the cortex of the CHI group. The morphological appearance of the astrocytes is shown in the higher-magnification insets, which were taken from the middle brain sections and from the same regions of the cortex. (B) IBA1-positive staining in the cortex at 1 day, 7 days, and 2 months post-injury shows changes in microglia morphology in the neocortex after the CHI (n = 7-14, 50/50 male/female). The mice (CD-1/129 background) were 8 months old at the time of surgery. This figure has been adapted from 11 and reproduced with permission. Scale bar = 1 mm, 50 µm and 100 µm as indicated in the figure. Please click here to view a larger version of this figure.
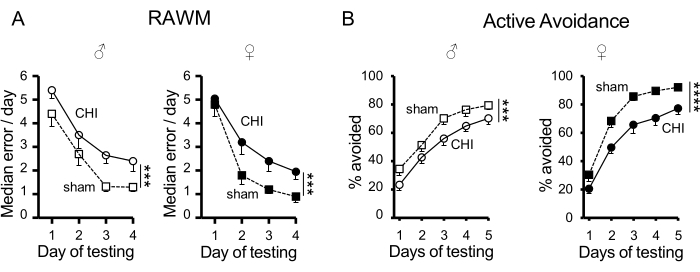
Figure 3: CHI-induced memory deficits in RAWM and active avoidance. (A) At 2 weeks post-injury, both the CHI- and sham-operated mice were able to learn the RAWM task, but the CHI mice made more errors compared to the sham mice (*** p < 0.0005); sham (n = 20/20 male/female); CHI (n = 20/20 male/female). The mice (C57BL/6J) were 3-4 months old at the time of surgery. (B) At 4 weeks post-injury, the CHI and sham-operated mice were able to learn the active avoidance task, but the CHI mice avoided fewer foot-shocks compared to the sham mice (*** p = 0.0005; **** p < 0.0001); sham (n = 10/10 male/female); CHI (n = 9/10 male/female). The mice (C57BL/6J) were 3-5 months old at the time of surgery. Data are shown as mean ± SEM. (A) This figure has been adapted from 12 and reproduced with permission. (B) This figure has been adapted from 13 and reproduced with permission. Please click here to view a larger version of this figure.
Discussion
Several steps are involved in recreating a consistent injury model using the described model. First, it is critical to correctly secure the animal into the stereotaxic frame. The animal’s head should not be able to move laterally, and the skull should be completely flat with bregma and lambda reading the same coordinates. Correctly placing the ear bars is the most difficult aspect of this surgery, and this can only be learned with practice. If the skull is not level, the head should be adjusted before inducing CHI. Failure to adjust the head positioning will cause a skull fracture. To evaluate that the skull is flat, one should look at the gap between the skull and the impact tip from all angles around the tip. Mice with depressed skull fractures should be excluded from experiments, as they have a much stronger inflammatory response and a more severe injury compared to mice that did not suffer skull fractures19. Additionally, mice with skull fractures show more severe TBI outcomes, such as post-traumatic respiratory depression, secondary rebound injury, and eventually death20.
In this study, the animal’s head was secured with ear bars. In particular, only mouse-specific acetal resin ear bars with a tapered point are recommended to be used, not large rat ear bars. It is possible to use non-puncture rubber-tipped ear bars, but these ear bars will compress the skull, altering the biomechanics of the CHI, and are less reproducible. In addition, there is a limitation to using ear bars, as it does not allow for any rotational forces. Nevertheless, the greater reproducibility of the ear bars outweighs the limited number of rotational forces that can be generated if the head is unfixed.
However, fixing the head with ear bars can also cause injury to the ear at impact if the impact forces are all placed at the ears. A head support apparatus placed under the head to displace the forces away from the ears was developed. After testing multiple pillow-like objects, the one that worked the best was the 1 mL latex pipette bulb filled with water. The pipette bulb under the animal’s head can be expanded after the animal is in the stereotaxic frame, allowing it to have a tight fit and provide full support under the head. When placed correctly, there should be no bleeding from the ears or behavioral indications of ear damage (rolling/head tilt) after the injury.
Some versions of the CHI model use a rubber tip probe21,22 or metal helmet23,24 to reduce the occurrence of skull fractures. As long as the 5 mm impactor tip is flush with the skull, there is no need to use any of them. It may be tempting for new users who do not have extensive experience with stereotaxic surgery to induce the injury with the tip not flush with the skull in the medial-lateral plane. If the skull is not level in the medial-lateral plane, it is because the ear bars are not placed correctly. The only fix for this problem is to remove the animal from the impactor and assign the mouse to a sham injury. If the tip is not flush on the anterior-posterior plane, then the height of the bite bar needs to be adjusted and the tip realigned with the bregma. Also, the use of a 5 mm impactor with a flat tip reduces the chance of causing skull fractures19 compared to impactor tips of smaller diameters. Other important factors to consider are the age and weight of the subject, as well as the skull thickness25 and the strains of the mice26.
In people, a mild TBI is not associated with death during the first minutes after the injury. In animals, even a mild injury can cause death. However, in this model, mortality is almost always associated with surgical complications, not the injury alone. The most common reason a mouse would die after the impact is the depth of anesthesia. This could occur if the surgery took longer than expected or if the isoflurane gas was at a higher concentration than needed for that animal. If the animal’s breathing is slow or labored, this could be a sign that the anesthesia depth should be reduced prior to delivering the impact. If the animal’s breath is slow or labored at the time of impact, the animal will likely have apnea and may die.
There are many models of mild TBI. Each has strengths and weaknesses, and this model is no different. As reported, here is described a single hit model of TBI, yet the model has been used to cause a repetitive TBI15. The steps described in this protocol can be repeated to induce a repetitive TBI injury. When evaluating the different TBI models, it is important to consider whether the model has the desired pathology that one is attempting to model. One should also consider how reproducible the model is. It is strongly recommended that the starting point for using this or any TBI model is to independently validate and characterize that the model works as previously reported.
Divulgations
The authors have nothing to disclose.
Acknowledgements
This work was supported in part by the National Institutes of Health under award numbers R01NS120882, RF1NS119165, and R01NS103785 and the Department of Defense award number AZ190017. The content is solely the responsibility of the authors and does not represent the official views of the National Institutes of Health or the Department of Defense.
Materials
| 9 mm Autoclip Applier | Braintree scientific | ACS- APL | Surgery |
| 9 mm Autoclip Remover | Braintree scientific | ACS- RMV | Surgery |
| 9 mm Autoclip, Case of 1,000 clips | Braintree scientific | ACS- CS | Surgery (Staples) |
| Aperio ImageScope software | Leica BioSystems | NA | IHC |
| BladeFLASK Blade Remover | Fisher Scientific | 22-444-275 | Surgery |
| Cotton tip applicator | VWR | 89031-270 | Surgery |
| Digitial mouse stereotaxic frame | Stoelting | 51730D | Surgery |
| Dumont #7 Forceps | Roboz | RS-5047 | Surgery |
| Ear bars | Stoelting | 51649 | Surgery |
| EthoVision XT 11.0 | Noldus Information Technology | NA | RAWM |
| Fiber-Lite | Dolan-Jeffer Industries | UN16103-DG | Surgery |
| Fisherbrand Bulb for Small Pipets | Fisher Scientific | 03-448-21 | Head support apparatus |
| Gemini Avoidance System | San Diego Instruments | NA | Active avoidance |
| Heating Pad | Sunbeam | 732500000U | Surgery prep |
| HRP conjugated goat anti-rabbit IgG | Jackson Immuno Research laboratories | 111-065-144 | IHC |
| Induction chamber | Kent Scientific | VetFlo-0530XS | Surgery prep |
| Isoflurane, USP | Covetrus | NDC: 11695-6777-2 | Surgery |
| Mouse gas anesthesia head holder | Stoelting | 51609M | Surgery |
| Neuropactor Stereotaxic Impactor | Neuroscience Tools | n/a | Surgery: Formally distributed by Lecia as impact one |
| NexGen Mouse 500 | Allentown | n/a | Post-surgery, holding cage |
| Parafilm | Bemis | PM992 | Head support apparatus |
| Peanut – Professional Hair Clipper | Whal | 8655-200 | Surgery prep |
| Povidone-Iodine Solution USP, 10% (w/v), 1% (w/v) available Iodine, for laboratory | Ricca | 3955-16 | Surgery |
| Puralube Vet Oinment,petrolatum ophthalmic ointment, Sterile ocular lubricant | Dechra | 17033-211-38 | Surgery |
| Rabbit anti-GFAP | Dako | Z0334 | IHC |
| Rabbit anti-IBA1 | Wako | 019-19741 | IHC |
| 8-arm Radial Arm Water Maze | MazeEngineers | n/a | RAWM |
| Scale | OHAUS CS series | BAL-101 | Surgery prep |
| Scalpel Handle #7 Solid 6.25" | Roboz | RS-9847 | Surgery |
| Sterile Alcohol Prep Pads (isopropyl alcohol 70% v/v) | Fisher Brand | 22-363-750 | Surgery prep |
| SumnoSuite low-flow anesthesia system | Kent Scientific | SS-01 | Surgery |
| 10 mL syringe Luer-Lok Tip | BD Bard-Parker | 302995 | Head support apparatus |
| Timers | Fisher Scientific | 6KED8 | Surgery |
| Topical anesthetic cream | L.M.X 4 | NDC 0496-0882-15 | Surgery prep |
| Triple antibiotic ointment | Major | NDC 0904-0734-31 | Post-surgery |
| Tubing | MasterFlex | 96410-16 | Head support apparatus |
| Vaporizer Single Channel Anesthesia System | Kent Scientific | VetFlo-1210S | Surgery prep |
References
- Capizzi, A., Woo, J., Verduzco-Gutierrez, M. Traumatic brain injury: An overview of epidemiology, pathophysiology, and medical management. The Medical Clinics of North America. 104 (2), 213-238 (2020).
- Bodnar, C. N., Roberts, K. N., Higgins, E. K., Bachstetter, A. D. A systematic review of closed head injury models of mild traumatic brain injury in mice and rats. Journal of Neurotrauma. 36 (11), 1683-1706 (2019).
- Shultz, S. R., et al. The potential for animal models to provide insight into mild traumatic brain injury: Translational challenges and strategies. Neuroscience and Biobehavioral Reviews. 76, 396-414 (2017).
- Xiong, Y., Mahmood, A., Chopp, M. Animal models of traumatic brain injury). Nature Reviews Neuroscience. 14 (2), 128-142 (2013).
- Albert-Weissenberger, C., Varrallyay, C., Raslan, F., Kleinschnitz, C., Siren, A. L. An experimental protocol for mimicking pathomechanisms of traumatic brain injury in mice. Experimental and Translational Stroke Medicine. 4, 1 (2012).
- Chen, Y., Constantini, S., Trembovler, V., Weinstock, M., Shohami, E. An experimental model of closed head injury in mice: pathophysiology, histopathology, and cognitive deficits. Journal of Neurotrauma. 13 (10), 557-568 (1996).
- Dixon, C. E., Clifton, G. L., Lighthall, J. W., Yaghmai, A. A., Hayes, R. L. A controlled cortical impact model of traumatic brain injury in the rat. Journal of Neuroscience Methods. 39 (3), 253-262 (1991).
- Schwulst, S. J., Islam, M. Murine model of controlled cortical impact for the induction of traumatic brain injury. Journal of Visualized Experiments. (150), e60027 (2019).
- Cole, J. T., et al. Craniotomy: True sham for traumatic brain injury, or a sham of a sham. Journal of Neurotrauma. 28 (3), 359-369 (2011).
- Brody, D. L., et al. Electromagnetic controlled cortical impact device for precise, graded experimental traumatic brain injury. Journal of Neurotrauma. 24 (4), 657-673 (2007).
- Webster, S. J., Van Eldik, L. J., Watterson, D. M., Bachstetter, A. D. Closed head injury in an age-related Alzheimer mouse model leads to an altered neuroinflammatory response and persistent cognitive impairment. The Journal of Neuroscience. 35 (16), 6554-6569 (2015).
- Macheda, T., Roberts, K. N., Morganti, J. M., Braun, D. J., Bachstetter, A. D. Optimization and validation of a modified radial-arm water maze protocol using a murine model of mild closed head traumatic brain injury. PLoS One. 15 (8), 0232862 (2020).
- Macheda, T., Snider, H. C., Watson, J. B., Roberts, K. N., Bachstetter, A. D. An active avoidance behavioral paradigm for use in a mild closed head model of traumatic brain injury in mice. Journal of Neuroscience Methods. 343, 108831 (2020).
- Bachstetter, A. D., et al. Attenuation of traumatic brain injury-induced cognitive impairment in mice by targeting increased cytokine levels with a small molecule experimental therapeutic. Journal of Neuroinflammation. 12, 69 (2015).
- Bachstetter, A. D., et al. The effects of mild closed head injuries on tauopathy and cognitive deficits in rodents: Primary results in wild type and rTg4510 mice, and a systematic review. Experimental Neurology. 326, 113180 (2020).
- Lyons, D. N., et al. A mild traumatic brain injury in mice produces lasting deficits in brain metabolism. Journal of Neurotrauma. 35 (20), 2435-2447 (2018).
- Yanckello, L. M., et al. Inulin supplementation mitigates gut dysbiosis and brain impairment induced by mild traumatic brain injury during chronic phase. Journal of Cellular Immunology. 4 (2), 50-64 (2022).
- Bachstetter, A. D., et al. Early stage drug treatment that normalizes proinflammatory cytokine production attenuates synaptic dysfunction in a mouse model that exhibits age-dependent progression of Alzheimer’s disease-related pathology. The Journal of Neuroscience. 32 (30), 10201-10210 (2012).
- Zvejniece, L., et al. Skull fractures induce neuroinflammation and worsen outcomes after closed head injury in mice. Journal of Neurotrauma. 37 (2), 295-304 (2020).
- Flierl, M. A., et al. Mouse closed head injury model induced by a weight-drop device. Nature Protocols. 4 (9), 1328-1337 (2009).
- Yang, Z., et al. Temporal MRI characterization, neurobiochemical and neurobehavioral changes in a mouse repetitive concussive head injury model. Scientific Reports. 5, 11178 (2015).
- Petraglia, A. L., et al. The spectrum of neurobehavioral sequelae after repetitive mild traumatic brain injury: a novel mouse model of chronic traumatic encephalopathy. Journal of Neurotrauma. 31 (13), 1211-1224 (2014).
- Laskowitz, D. T., et al. COG1410, a novel apolipoprotein E-based peptide, improves functional recovery in a murine model of traumatic brain injury. Journal of Neurotrauma. 24 (7), 1093-1107 (2007).
- Lloyd, E., Somera-Molina, K., Van Eldik, L. J., Watterson, D. M., Wainwright, M. S. Suppression of acute proinflammatory cytokine and chemokine upregulation by post-injury administration of a novel small molecule improves long-term neurologic outcome in a mouse model of traumatic brain injury. Journal of Neuroinflammation. 5, 28 (2008).
- Lillie, E. M., Urban, J. E., Lynch, S. K., Weaver, A. A., Stitzel, J. D. Evaluation of skull cortical thickness changes with age and sex from computed tomography scans. Journal of Bone and Mineral Research. 31 (2), 299-307 (2016).
- Kawakami, M., Yamamura, K. Cranial bone morphometric study among mouse strains. BMC Evolutionary Biology. 8, 73 (2008).

