Synthesis of Decellularized Cartilage Extracellular Matrix Hydrogels
Summary
This paper introduces a new method for the synthesis of decellularized cartilage extracellular matrix (DC-ECM) hydrogels. DC-ECM hydrogels have excellent biocompatibility and provide a superior microenvironment for cell growth. Therefore, they can be ideal cell scaffolds and biological delivery systems.
Abstract
Decellularized cartilage extracellular matrix (DC-ECM) hydrogels are promising biomaterials for tissue engineering and regenerative medicine due to their biocompatibility and ability to mimic natural tissue properties. This protocol aims to produce DC-ECM hydrogels that closely mimic the native ECM of cartilage tissue. The protocol involves a combination of physical and chemical disruption and enzymatic digestion to remove the cellular material while preserving the structure and composition of the ECM. The DC-ECM is cross-linked using a chemical agent to form a stable and biologically active hydrogel. The DC-ECM hydrogel has excellent biological activity, spatial structure, and biological induction function, as well as low immunogenicity. These characteristics are beneficial in promoting cell adhesion, proliferation, differentiation, and migration and for creating a superior microenvironment for cell growth. This protocol provides a valuable resource for researchers and clinicians in the field of tissue engineering. Biomimetic hydrogels can potentially enhance the development of effective tissue engineering strategies for cartilage repair and regeneration.
Introduction
Cartilage tissue engineering is a rapidly developing field that seeks to regenerate damaged or diseased cartilage tissue1. One key challenge in this field is the development of biomimetic scaffolds that can support the growth and differentiation of chondrocytes, the cells responsible for producing cartilage2. The ECM of cartilage tissue plays a critical role in regulating the behavior of chondrocytes. DC-ECM is an effective scaffold for tissue engineering applications3.
A number of techniques have been developed to produce DC-ECM from cartilage tissue, including chemical, enzymatic, and physical methods. However, these methods often result in the generation of ECM hydrogels that are insufficiently biomimetic, which limits their potential for use in tissue engineering applications4,5. Thus, there is a need for a more effective method for producing DC-ECM hydrogels.
The development of this technique is important because it can advance the field of tissue engineering by providing a new approach for creating biomimetic scaffolds that can support tissue regeneration and repair. Furthermore, this technique could be easily adapted to produce ECM hydrogels from other tissues, thereby expanding its potential applications.
In the broader body of literature, there has been growing interest in using DC-ECM as a scaffold for tissue engineering applications6. Numerous studies have demonstrated the effectiveness of DC-ECM hydrogels in promoting cell growth and differentiation in various tissues, including cartilage7,8. Therefore, the development of a protocol for producing DC-ECM hydrogels that closely mimic the natural ECM of cartilage tissue is a significant contribution to the field.
The protocol presented in this paper addresses this need by providing a novel method for producing DC-ECM hydrogels that closely mimic the natural ECM of cartilage tissue. The protocol involves decellularizing cartilage tissue, isolating the resulting ECM, and creating a hydrogel by cross-linking the ECM with a biocompatible polymer. The resulting hydrogel has shown promising results in supporting the growth and differentiation of chondrocytes.
Protocol
This study was approved by the Ethics Committee of Tongde Hospital of Zhejiang Province.
1. Preparation of the DC-ECM hydrogel
NOTE: In this study, the cartilage was obtained from the knee joints of 12 month old Bama miniature pigs, avoiding the collection of bone tissue.
- Take the collected cartilage, and block and chop it into 1-2 mm3 pieces with a scalpel.
- Place 20 g of the minced cartilage in a 50 mL centrifuge tube, and add 20 mL of hypotonic Tris-HCl buffer (10 mM Tris-HCl, pH 8.0) to submerge the tissue completely. Place the centrifuge tube in a −80 °C freezer for 3 h and then in a 37 °C oven for 3 h. Repeat the freezing and heating step six times. In this step, the hypotonic Tris-HCl buffer does not need replacement.
- Shake the centrifuge tube for 30 s using a vortex mixer at a speed of 1,000 rpm. Place a stainless-steel sieve (pore size: ~250 µm) on a new 50 mL centrifuge tube.
- Slowly decant the decellularized cartilage into the stainless-steel sieve, wash the tissue three times with sterile PBS, and collect the cartilage.
- Add 10 mL of trypsin solution (0.25% trypsin in PBS), and place the tube on a shaker at 37 °C for 24 h. During this period, replace the trypsin every 4 h. Filter the suspension using the stainless-steel sieve, and preserve the tissue. The trypsin can be treated overnight during one of the digestion processes, and this will not affect the final digestion.
- Wash the trypsinized tissue with hypertonic buffer (1.5 M NaCl, 50 mM Tris-HCl, pH 7.6).
- Add 10 mL of nuclease solution (50 U/mL deoxyribonuclease and 1 U/mL ribonuclease in 10 mM Tris-HCl, pH 7.5), and place the tube on a shaker at 37 °C for 4 h.
- Remove the nuclease solution, wash the cartilage three times with sterile PBS, and add hypotonic Tris-HCl solution. Place the centrifuge tube on a shaker, and rinse for 20 h at room temperature (RT).
- Remove the hypotonic Tris-HCl solution, wash the cartilage three times with sterile PBS, and add 1% Triton X-100 solution to submerge the tissue for 24 h.
- Remove the Triton X-100 solution, and thoroughly rinse the decellularized cartilage with distilled water for 3 days, changing the distilled water every 12 h.
- Soak the cartilage in peracetic acid solution (0.1% PAA in 4% ethanol) for 4 h. Remove the peracetic acid solution, and wash the cartilage three times with sterile distilled water.
- Place the stainless-steel sieve (pore size: ~250 µm) on a 50 mL centrifuge tube. Slowly decant the decellularized cartilage into the stainless-steel sieve, and collect the cartilage. Test the degree of decellularization and the matrix retention of the cartilage by estimating the DNA, collagen, and glycosaminoglycan (GAG) content.
- Put the decellularized cartilage into a grinding bowl, add liquid nitrogen, and grind the decellularized cartilage to form a powder. Take 2 g of the decellularized cartilage powder, add 80 mL of 0.5 M acetic acid and 20 mg of pepsin, and digest for 24 h. Centrifuge at 400 x g for 10 min; discard the sediment, and collect the supernatant solution (DC-ECM solution).
- Decant 1 mL of DC-ECM solution per well into 6-well plates. Place the 6-well plates in a lyophilizer. Freeze the DC-ECM solution. Once the temperature in the freeze-dryer drops to −40 °C, turn on the vacuum pump, and maintain the vacuum degree at 10 Pa for 22 h.
- Take out the freeze-dried DC-ECM solution, place it in centrifuge tubes, and store at −20 °C. The minimum storage period of freeze-dried DC-ECM solution exceeds half a year.
- Add 1 mL of sterile distilled water to dissolve 20 mg of freeze-dried DC-ECM solution in the centrifuge tube. Shake for 1 min using a vortex mixer at a speed of 1,000 rpm at RT. Add 1 mg of vitamin B2 (0.1% w/v) to the DC-ECM solution, incubate at 37 °C for 60 min, and irradiate with UV light (370 nm, 3.5 mW/cm2) for 3 min to form a hydrogel (DC-ECM hydrogel).
2. Detection of decellularized cartilage
- DNA content detection of decellularized cartilage
NOTE: Extract the DNA using the DNEasy Blood & Tissue Kit.- First, take 20 mg of DC-ECM cartilage in a centrifuge tube. Add 180 µL of Buffer GTL and 20 µL of Proteinase K by vortex oscillation, and incubate the cartilage at 56 °C for 4 h until it is completely dissolved.
- Shake the centrifuge tube for 15 s using a vortex mixer at a speed of 1,000 rpm at RT. Next, add 200 µL of Buffer GL and anhydrous ethanol, and thoroughly mix by vortex vibration. Centrifuge the samples for 1 min at a speed of 6,000 x g at 4 °C.
- Add 500 µL of Buffer GW1 to the adsorption column, and centrifuge the samples for 1 min at a speed of 12,000 x g at 4 °C. Add 500 µL of Buffer GW2 to the adsorption column, and centrifuge at 20,000 x g at 4 °C for 1 min. Finally, add 50 µL of sterilized water to the adsorption column, and centrifuge for 1 min at a speed of 6,000 x g at 4 °C to collect the DNA solution. Determine the DNA content using a spectrophotometer.
- Collagen content detection in the decellularized cartilage
- To detect the collagen content in the decellularized cartilage, use hydroxyproline as a collagen amino acid marker. Acidify 5 mg of decellularized cartilage with 5 mL of 6 M hydrochloric acid at 100 °C for 20 min, and then neutralize it with 5 mL of a 6 M sodium hydroxide solution.
- Calculate the content of hydroxyproline by measuring the absorbance of the sample at 570 nm with a spectrophotometer. Obtain a concentration-absorption linear regression using the standard hydroxyproline sample.
- GAG content detection in the decellularized cartilage
NOTE: The GAG content in the DC-ECM cartilage was detected using a tissue GAG colorimetric quantitative detection kit. All the reagents below are available in the kit.- Take 200 mg of DC-ECM cartilage powder, and add 500 µL of Reagent A by vortex oscillation. Incubate the sample at 4 °C for 16 h, and then centrifuge at 14,000 x g for 10 min.
- Take 50 mL of sample solution, and add 50 µL of high-salt solution (Reagent B) and 50 µL of acid solution(Reagent C) by vortex oscillation. Incubate the sample for 10 min.
- Add 750 µL of dye solution (Reagent D) by vortex oscillation, and incubate the sample for 30 min in dark conditions. Centrifuge the sample at 14,000 x g for 10 min, and then discard the supernatant.
- Add 1 µL of cleaning solution (Reagent E), and mix well. Centrifuge the sample at 14,000 x g for 10 min, and discard the supernatant.
- Add 1 µL of dissociation solution (Reagent F) to the sample, and mix well. Incubate the sample for 30 min under dark conditions. Finally, determine the GAG content using a spectrophotometer at 600 nm.
- Scanning electron microscope (SEM) and transmission electron microscope (TEM) analysis of the decellularized cartilage
- Compare the decellularized cartilage and normal cartilage tissue. Place the sample in a 2.5% glutaraldehyde solution, incubate at 4 °C overnight and then wash with PBS three times.
- Fix the sample in 1% OsO4 for 1 h, and then wash three times with PBS.
- Dehydrate the sample by sequential immersion in 50%, 70%, 90%, and 100% ethanol, as well as 100% acetone for 15 min each.Place the sample in a mixed solution of hexamethyldisilazane and ethanol (1:1) for 15 min, followed by immersion in pure hexamethyldisilazane for 15 min.
- Place the sample in an HCP-2 dryer, and then dry using liquid nitrogen. Then, coat the fully dried specimen with a thin layer of gold-palladium using sputter coating, and image using SEM. The sputter coating was performed at a power of 120 W for 5 min. The experiment was carried out under the following conditions: a working voltage of 15 kV, and a vacuum degree lower than 5 x 10−5 Pa.
- For the TEM analysis, place the sample in a mixture of anhydrous acetone and resin (1:1) for 1 h, followed by a mixture of anhydrous acetone and resin (1:3) for 3 h. Then, place the sample in resin overnight.
- Place the sample in embedding medium-filled capsules, and heat at 70 °C for 9 h.
- After embedding, cut the specimen into 70 nm thin slices using an ultrafine microtome, and place on a copper mesh.
- Pipet 20 µL of uranyl acetate staining solution onto the copper mesh, and stain for 15 min at RT. Remove the staining solution by gently washing the mesh twice with distilled water.
- Then, pipet 20 µL of lead citrate staining solution onto the copper mesh, and stain for 15 min at RT. Wash the mesh three times with distilled water.
- Place the copper mesh onto a clean Petri dish lined with filter paper. After air-drying, photograph the sections using TEM. The probe was applied with a downward force of 500 nN, scanned at a rate of 1 Hz, and had an elastic constant (k-value) of 40 Nm-1. The radius of the probe tip was measured to be 8 nm.
Representative Results
To prepare a better DC-ECM cartilage hydrogel, we studied and reviewed the previous literature and compared the various decellularization protocols in terms of the decellularization ratio, immunogenicity, and mechanical functionality9.
On this basis, we prepared the DC-ECM cartilage hydrogel and explored the effect of a radially oriented extractive matrix/mesenchymal stem cell exosome bio-ink in treating osteochondral defects. The results showed that the DC-ECM cartilage hydrogel had low immunogenicity and could enhance cell migration and promote cartilage repair10.
In recent years, we have optimized the preparation of the DC-ECM cartilage. We prepared the decellularized cartilage using the above experimental steps. The results showed that the DNA content was eliminated in the decellularized cartilage compared with that in native cartilage (p < 0.001, Figure 1A). The hydroxyproline test indicated that the collagen content was similar between the native and decellularized cartilages (p = 0.48, Figure 1B). The DMMB assay showed that glycosaminoglycan was well-retained in the decellularized cartilage compared with the native cartilage (p = 0.68, Figure 1C). Furthermore, SEM and TEM were used to observe the ultrastructure of the DC-ECM (Figure 1D).
To prepare a DC-ECM hydrogel, the freeze-dried DC-ECM solution was solubilized for a final concentration of 2 wt%. Further, the DC-ECM solution was mixed with VB2, followed by UVA (370 nm)-induced cross-linking (Figure 2A). We placed the DC-ECM solution and DC-ECM hydrogel into microcentrifuge tubes (Figure 2B). When the tubes were inverted, the hydrogel in the tubes did not flow to the bottom, which was a sign of gelation. The gelation time for the DC-ECM solution based on collagen self-assembly at 37 °C without a cross-linking agent was approximately 15 min (Figure 2C). The viscosity and dynamic modulus of the DC-ECM solution and hydrogel were tested. We found that the solution viscosity of the DC-ECM hydrogel was higher than that of the DC-ECM solution, and higher shear rates were associated with lower solution viscosity (Figure 2D). In addition, the storage modulus of both the DC-ECM solution and hydrogel was much higher than the loss modulus, indicating that they both had properties of a gel rather than a liquid (Figure 2E). Notably, after cross-linking and freeze-drying, the pore sizes of the DC-ECM solution and DC-ECM hydrogel, measured with SEM, decreased from 137.672 µm to 37.936 µm (p < 0.00195, Figure 2F,G).
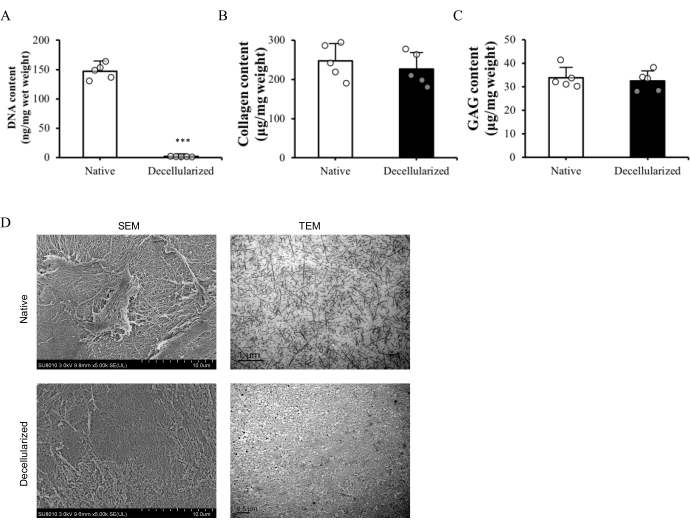
Figure 1: Preparation and characterization of the decellularized cartilage. The decellularized cartilage was compared with the native cartilage. (A–C) Quantification of the DNA, collagen, and glycosaminoglycan (GAG) content. n = 5, ***p < 0.001 (Student's t-test). All the experiments were performed at least three times. (D) Microscopic structures of the native cartilage and decellularized cartilage photographed with SEM and TEM. Please click here to view a larger version of this figure.
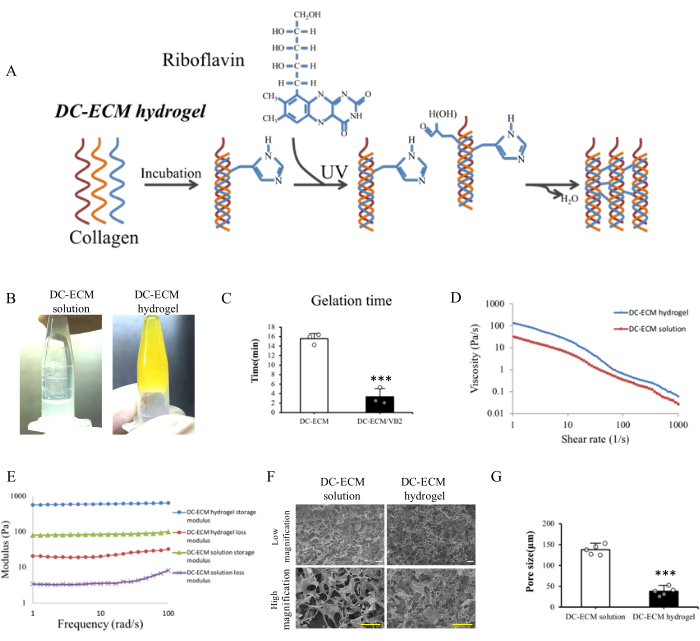
Figure 2: Preparation and characterization of the DC-ECM hydrogel. Under ultraviolet light, the DC-ECM solution and VB2 cross-linked and formed a DC-ECM hydrogel. (A) Molecule structures and synthesis of the DC-ECM hydrogel. The appearance, characterization, and mechanical properties were compared between the DC-ECM solution and DC-ECM hydrogel. (B) The images of the DC-ECM solution and DC-ECM hydrogel in microcentrifuge tubes. (C) The gelation time of the DC-ECM hydrogel and DC-ECM/VB2 hydrogel. n = 3, ***p < 0.001 (Student's t-test). (D) The viscosity and (E) dynamic modulus of the DC-ECM solution and DC-ECM hydrogel. (F) Microscopic structures of the DC-ECM solution and hydrogel (low and high magnification). Scale bars = 100 µm. (G) Pore sizes of the DC-ECM solution and hydrogel. n = 5, ***p < 0.001 (Student's t-test). All the experiments were performed at least three times. Please click here to view a larger version of this figure.
Discussion
This protocol provides a systematic approach for the preparation of decellularized cartilage extracellular matrix hydrogels that closely mimic the native ECM of cartilage tissue. The protocol involves a combination of physical, chemical, and enzymatic disruption to remove cellular material while preserving the structure and composition of the ECM. The protocol’s critical steps include adjusting the decellularization time and methods and ensuring complete decellularization.
Compared to other existing methods for tissue engineering and regenerative medicine, this protocol offers several advantages. DC-ECM hydrogels have excellent biological activity, spatial structure, and biological induction function, as well as low immunogenicity, and these characteristics are beneficial in promoting cell adhesion, proliferation, differentiation, and migration11. DC-ECM hydrogels can also be used for drug delivery and cartilage defect treatment12.
One modification that can be made to this protocol is the use of different cross-linking agents to enhance the mechanical properties of the hydrogel. For example, nano-metal materials can be used to improve the mechanical properties of the hydrogel13. In addition, the concentration of riboflavin and the exposure times to UV light can be optimized to control the compressive and tensile strengths of the hydrogel.
Despite its many advantages, this technique has some limitations that should be considered. One limitation is that the decellularization process may cause some damage to the ECM, leading to changes in its mechanical properties14. Another limitation is that the decellularization process may not completely remove all antigenic material, leading to a potential immune response15. Furthermore, it is important to note that the protocol described in this paper is specific to cartilage tissue, and other types of tissue may require adjustments to the decellularization method.
In terms of future applications, this protocol can be further optimized to develop DC-ECM hydrogels with different compressive and tensile strengths. Additionally, this technique can be applied to other tissues to develop biomimetic hydrogels for tissue engineering and regenerative medicine applications. Overall, the protocol presented in this paper provides a valuable resource for researchers and clinicians in the field of tissue engineering and has the potential to enhance the development of effective tissue engineering strategies for cartilage repair and regeneration.
Divulgations
The authors have nothing to disclose.
Acknowledgements
This work was sponsored by the Medicine and Health Technology Plan of Zhejiang Province (2019KY050), the Traditional Chinese Medicine Science and Technology Plan of Zhejiang Province (2019ZA026), the Key Research and Development Plan in Zhejiang Province (Grant No.2020C03043), the Traditional Chinese Medicine Science and Technology Plan of Zhejiang Province (2021ZQ021), and the Zhejiang Provincial Natural Science Foundation of China (LQ22H060007).
Materials
| 1 M Tris-HCl, pH7.6 | Beyotime | ST776-100 mL | |
| 1 M Tris-HCl, pH8.0 | Beyotime | ST780-500 mL | |
| -80 °C Freezer | Eppendorf | F440340034 | |
| Deoxyribonuclease | Aladdin | D128600-80KU | |
| DNEasy Blood &Tissue Kit | Qiagen | No. 69506 | |
| GAG colorimetric quantitative detection kit | Shanghai Haling | HL19236.2 | |
| HCP-2 dryer | Hitachi | N/A | |
| Nanodrop8000 | Thermo Fisher | N/A | Spectrophotometer |
| PBS (10x) | Gibco | 70011044 | |
| Ribonuclease | Aladdin | R341325-100 mg | |
| Sigma500 | ZIESS | N/A | Scanning electron microscope |
| Spectra S | Thermo Fisher | N/A | Transmission electron microscope |
| Stainless steel sieve | SHXB-Z-1 | Shanghai Xinbu | |
| Triton X-100 | Beyotime | P0096-500 mL | |
| Trypsin | Gibco | 15050065 | |
| Ultraviolet lamp | Omnicure 2000 | N/A | |
| Vitamin B2 | Gibco | R4500-5G | |
| Vortex mixer | Shanghai Qiasen | 78HW-1 |
References
- Vega, S. L., Kwon, M. Y., Burdick, J. A. Recent advances in hydrogels for cartilage tissue engineering. European Cells & Materials. 33, 59-75 (2017).
- Yang, J., Zhang, Y. S., Yue, K., Khademhosseini, A. Cell-laden hydrogels for osteochondral and cartilage tissue engineering. Acta Biomaterialia. 57, 1-25 (2017).
- Bejleri, D., Davis, M. E. Decellularized extracellular matrix materials for cardiac repair and regeneration. Advanced Healthcare Materials. 8 (5), e1801217 (2019).
- Brown, M., Li, J., Moraes, C., Tabrizian, M., Li-Jessen, N. Y. K. Decellularized extracellular matrix: New promising and challenging biomaterials for regenerative medicine. Biomaterials. 289, 121786 (2022).
- Barbulescu, G. I., et al. Decellularized extracellular matrix scaffolds for cardiovascular tissue engineering: Current techniques and challenges. International Journal of Molecular Sciences. 23 (21), 13040 (2022).
- Zhang, W., Du, A., Liu, S., Lv, M., Chen, S. Research progress in decellularized extracellular matrix-derived hydrogels. Regenerative Therapy. 18, 88-96 (2021).
- Zhu, W., et al. Cell-derived decellularized extracellular matrix scaffolds for articular cartilage repair. International Journal of Artificial Organs. 44 (4), 269-281 (2021).
- Li, T., Javed, R., Ao, Q. Xenogeneic decellularized extracellular matrix-based biomaterials for peripheral nerve repair and regeneration. Current Neuropharmacology. 19 (12), 2152-2163 (2021).
- Xia, C., et al. Decellularized cartilage as a prospective scaffold for cartilage repair. Materials Science & Engineering C-Materials for Biological Applications. 101, 588-595 (2019).
- Chen, P., et al. Desktop-stereolithography 3D printing of a radially oriented extracellular matrix/mesenchymal stem cell exosome bioink for osteochondral defect regeneration. Theranostics. 9 (9), 2439-2459 (2019).
- Saldin, L. T., Cramer, M. C., Velankar, S. S., White, L. J., Badylak, S. F. Extracellular matrix hydrogels from decellularized tissues: Structure and function. Acta Biomaterialia. 49, 1-15 (2017).
- Yuan, X., et al. Stem cell delivery in tissue-specific hydrogel enabled meniscal repair in an orthotopic rat model. Biomaterials. 132, 59-71 (2017).
- Zheng, L., et al. Intensified stiffness and photodynamic provocation in a collagen-based composite hydrogel drive chondrogenesis. Advanced Science. 6 (16), 1900099 (2019).
- Young, J. L., Holle, A. W., Spatz, J. P.Nanoscale and mechanical properties of the physiological cell-ECM microenvironment. Experimental Cell Research. 343 (1), 3-6 (2016).
- Abdolghafoorian, H., et al. Effect of heart valve decellularization on xenograft rejection. Experimental and Clinical Transplantation. 15 (3), 329-336 (2017).

