Protection of H9c2 Myocardial Cells from Oxidative Stress by Crocetin via PINK1/Parkin Pathway-Mediated Mitophagy
Summary
Based on in vitro experiments, this study revealed the mechanism of crocetin in repairing oxidative stress damage of cardiomyocytes by influencing mitophagy, in which the PINK1/Parkin signaling pathway plays an important role.
Abstract
This study aimed to explore the oxidative stress-protective effect of crocetin on H2O2-mediated H9c2 myocardial cells through in vitro experiments, and further explore whether its mechanism is related to the impact of mitophagy. This study also aimed to demonstrate the therapeutic effect of safflower acid on oxidative stress in cardiomyocytes and explore whether its mechanism is related to the effect of mitophagy. Here, an H2O2-based oxidative stress model was constructed and assessed the degree of oxidative stress injury of cardiomyocytes by detecting the levels of lactate dehydrogenase (LDH), creatine kinase (CK), malondialdehyde (MDA), superoxide dismutase (SOD), catalase (CAT), and glutathione peroxidase (GSH Px). Reactive oxygen species (ROS)-detecting fluorescent dye DCFH-DA, JC-1 dye, and TUNEL dye were employed to assess mitochondrial damage and apoptosis. Autophagic flux was measured by transfecting Ad-mCherry-GFP-LC3B adenovirus. Mitophagy-related proteins were then detected via western blotting and immunofluorescence. However, crocetin (0.1-10 µM) could significantly improve cell viability and reduce apoptosis and oxidative stress damage caused by H2O2. In cells with excessive autophagic activation, crocetin could also reduce autophagy flow and the expression of mitophagy-related proteins PINK1 and Parkin, and reverse the transfer of Parkin to mitochondria. Crocetin could reduce H2O2-mediated oxidative stress damage and the apoptosis of H9c2 cells, and its mechanism was closely related to mitophagy.
Introduction
Acute myocardial infarction (AMI) is a life-threatening myocardial necrosis caused by severe and persistent ischemia and hypoxia to coronary arteries1,2. Percutaneous coronary intervention (PCI) is one of the first-line therapeutic strategies for AMI, and usually protects cardiomyocytes from ischemic damage3,4. The distal myocardium will lack blood and oxygen supply if not promptly and effectively treated after AMI, which leads to ischemic necrosis and further cardiovascular complications5,6. Promoting cardiomyocyte recovery and minimizing irreversible myocardial damage after missing the PCI surgical opportunity has been a research hotspot. After AMI, cardiomyocytes are in a state of ischemia and hypoxia, resulting in the inhibition of mitochondrial oxidative phosphorylation, reduction of NAD+ to NADPH, and increased single electron reduction7. As a result, the incomplete reduction reaction of oxygen generates an excess of reactive oxygen species (ROS) and ultimately leads to oxidative stress damage to cardiomyocytes8. An excessive accumulation of ROS triggers lipid peroxidation, further disrupting the structure and function of mitochondrial membranes. The result is a continuous opening of mitochondrial permeability transition pores and a decrease in mitochondrial membrane potential, inducing apoptosis and necrosis.
Angiotensin-converting enzyme (ACE) inhibitors, angiotensin-receptor blockers (ARBs), the inhibitors of β-adrenoceptors, aldosterone antagonists, and other standard drugs in AMI can help enhance heart function after myocardial infarction and prevent the occurrence of malignant events, such as arrhythmias and left ventricular remodeling9. However, postinfarction survival and prognosis are greatly affected by infarct size, and satisfactory results have not been achieved for reducing cardiomyocyte apoptosis10,11. Thus, the development of drugs to promote cardiomyocyte recovery after myocardial infarction has become an urgent issue.
Traditional medicine has been a source of inspiration for modern pharmaceutical research for many years12,13,14,15. Traditional Chinese medicine (TCM) has a long history in the treatment of AMI, and a series of randomized control trials in recent years have confirmed that TCM can indeed improve the prognosis of patients16,17. According to TCM theory, AMI is caused by blood stasis18,19, so drugs for promoting blood circulation are usually used for the treatment of AMI in the acute phase20. Among them, saffron is believed to have a powerful effect on blood activation and stasis, and is often used in the acute treatment of AMI. Crocetin, a major component of saffron, may play a key role in protecting cardiomyocytes21.
In this study, H9c2 myocardial cells were induced by H2O2 to simulate myocardial ischemia/reperfusion, which causes a cardiomyocyte injury of AMI, and crocetin was used as an intervention to investigate its protective effect against oxidative stress-induced myocardial injury. The mechanism of crocetin protecting cardiomyocytes was further explored through mitophagy. More importantly, this article provides a reference for the technical approach to the study of mitophagy and describes the entire experimental procedure in detail.
Protocol
The experiments were performed in the Laboratory of Physiology at the Beijing University of Chinese Medicine, China. All study methods were performed in accordance with the relevant guidelines and regulations of Beijing University.
1. Cell culture
- Add 10% fetal bovine serum and 1% penicillin/streptomycin to Dulbecco's modified Eagle medium (DMEM) basic medium (with 4.5 g/L D-glucose, 4.g.g/L L-glutamine, and 110 mg/L sodium pyruvate; see Table of Materials) to prepare DMEM complete medium.
- Thaw the liquid nitrogen-frozen H9c2 myocardial cells (see Table of Materials) in warm water at 37 °C with a quick and uniform stir until the ice melts.
- Transfer the cells to a centrifuge tube and add four times the volume of the DMEM complete medium. Centrifuge at 358 x g for 5 min at room temperature and discard the supernatant using a pipette.
- Dilute the obtained cell suspension with culture medium, blow gently, and inoculate the cells in a culture flask. Culture in an incubator at 37 °C with 5% CO2.
2. Determination of cell viability
- Dissolve crocetin (see Table of Materials) in dimethyl sulfoxide (DMSO) to concentrations of 0.05 mM, 0.1 mM, 0.5 mM, 1 mM, 5 mM, 10 mM, 50 mM, 100 mM, and 200 mM.
- Dissociate the H9c2 myocardial cells by trypsin, then neutralize the mixture with DMEM complete medium.
- Transfer the cells to a centrifuge tube and centrifuge at 179 x g for 5 min at room temperature. Discard the supernatant and mix the cells in DMEM complete medium by gently blowing.
- Count the cells using a blood cell counting plate22 (see Table of Materials) and dilute them to 5 × 104 cells/mL with DMEM complete medium.
- Divide the cells into nine equal portions. Add DMSO (diluted in a 1:1,000 ratio with DMEM complete medium) to the control group and add different concentrations of crocetin to the remaining groups at a ratio of 1:1,000.
- Seed the cells in 96-well plates at 100 µL per well. Discard the supernatant after incubation for 24 h and wash the cells three times with PBS.
- After adding 100 µL of DMEM basal medium, incubate the cells for 4 h and add 20 µL of MTS (see Table of Materials).
- Incubate the cells for another 2 h, measure the absorbance at a wavelength of 490 nm, and calculate the cell viability.
NOTE: Cell viability = (OD treated – OD blank) / (OD control – OD blank) × 100.
3. Determination of lactate dehydrogenase (LDH), creatine kinase (CK), malondialdehyde (MDA), superoxide dismutase (SOD), glutathione peroxidase (GSH Px), and catalase (CAT)
- Seed the H9c2 cells in a 6-well plate at a density of 1 × 105 cells. Collect the supernatant after the intervention and detect LDH and SOD levels, according to the manufacturer's instructions (see Table of Materials).
- Collect the supernatant and wash it with phosphate-buffered saline (PBS) once. Add the cell lysate to the culture dish and allow it to sit on ice for 20 min. Collect the liquid from the culture dish into a centrifuge tube.
- Detect CK, MDA, GSH-Px, and CAT levels according to the manufacturer's instructions23 (see Table of Materials and Supplementary File 1).
- Detect the total protein concentration of the lysis by the bicinchoninic acid (BCA) method to correct the concentration of CK, MDA, GSH-Px, and CAT24(see Table of Materials).
4. Determination of ROS
- Seed the H9c2 cells in a 48-well plate at a density of 5 × 103 cells. Dilute DCFH-DA (see Table of Materials) at a 1:1,000 ratio with the serum-free medium. Discard the cell supernatant and wash the cell twice with a serum-free medium.
- Add 150 µL of diluted DCFH-DA into each well and incubate at 37 °C for 20 min. Wash the cells three times with a serum-free medium and capture images under a fluorescence microscope (see Table of Materials).
5. Detection of mitochondrial membrane potential
- Detect the mitochondrial membrane potential using a JC-1 mitochondrial membrane potential assay kit25 (see Table of Materials). Discard the culture medium and wash them once with serum-free medium.
- Add JC-1 working solution to each tube and mix them well. Incubate at 37 °C for 20 min and wash the cells twice with JC-1 staining buffer. Add complete medium to each well and capture photographs under a fluorescence microscope.
6. TUNEL staining assay
- Use a TUNEL apoptosis assay kit (see Table of Materials) to determine apoptosis rates26. Discard the supernatant and wash the pellet once with serum-free medium.
- Add cell fixation solution and wash them with PBS once after incubating at room temperature for 30 min.
- Add 0.3% triton-100 to each well and incubate at room temperature for 5 min. Wash the cells with PBS twice. Add TUNEL detection working solution and incubate at 37 °C in the dark for 60 min.
- Add an anti-fluorescence quenching sealing tablet containing 4′,6-diamidino-2-phenylindole (DAPI; see Table of Materials) and capture photographs under a fluorescence microscope.
7. Monitoring autophagic flow by transfection of mCherry GFP-LC3B adenovirus
- Replace half of the medium in each well with fresh medium. Add Ad-mCherry GFP-LC3B adenovirus (multiplicity of infection [MOI] of 2) to the culture medium and add 5 µg/mL polybrene (see Table of Materials) to improve the infection efficiency.
- Replace the fresh medium after 24 h and observe the expression of the fluorescent protein under a confocal microscope.
- Culture the cells with the same conditions as section 1 after confirming successful virus infection and capture images under the confocal microscope27.
NOTE: More than 20% of cells showed green fluorescent protein (GFP) fluorescence, indicating a successful infection.
8. Western blot analysis
- Collect cells for whole protein extraction and lyse them (RIPA, protease inhibitor, and phosphatase inhibitor = 100:1:1; see Table of Materials) on ice for 30 min.
- Add 5x protein loading buffer to the protein sample after protein quantification and boil the samples for 10 min.
- Electrophorese the samples that contain equal amounts of protein with sodium dodecyl-sulfate polyacrylamide gel electrophoresis (SDS-PAGE) gels28. Then, transfer the samples onto polyvinylidene difluoride (PVDF) membranes.
- Block the PVDF membranes for 1 h with 5% skim milk powder and incubate with the primary antibody (PINK1, Parkin; see Table of Materials) at 4 °C overnight and the secondary antibody at room temperature for 1 h.
- Detect the target bands using enhanced chemiluminescence (ECL) solution and the chemiluminescence detection system. Use Image J software to quantify the bands via densitometry28.
9. Detection of Parkin's mitochondrial translocation by immunofluorescence
- Observe the colocalization of Parkin with mitochondria by double immunofluorescence staining. Discard the cell supernatant from each group and wash them three times with PBS.
- Fix the cells for 10 min at room temperature with 4% paraformaldehyde and add 0.1% triton-100 in PBS.
- Block with animal-free block solution (see Table of Materials) for 1 h to prevent non-specific binding between proteins and antibodies and reduce the fluorescence background.
- Incubate with a primary antibody (Parkin and Tom20; see Table of Materials) at 4 °C overnight.
- Add a fluorescent secondary antibody (see Table of Materials) and incubate in the dark for 1 h.
- Add the DAPI-containing anti-fluorescence quenching tablets and capture images under the confocal microscope.
10. Statistical analysis
- Perform statistical analysis using graphing and analysis software (see Table of Materials).
- Compare continuous variables between groups using one-way ANOVA. p < 0.05 was considered statistically significant.
Representative Results
Effects of crocetin on cell viability
Crocetin at 0.1 µM, 0.5 µM, 1 µM, 5 µM, 10 µM, 50 µM, and 100 µM had a significant proliferative effect on cells, while crocetin at concentrations above 200 µM significantly inhibited the proliferation of H9c2 cells (Figure 1A). After 4 h of treatment with 400 µM H2O2, the cell viability was reduced considerably, and crocetin could reverse this change to a certain extent (Figure 1B). Since no significant difference between 10 µM and 100 µM crocetin was observed on the H2O2-induced H9c2 cell viability, 10 µM crocetin was chosen as the high concentration, and 1 µM and 0.1 µM were used as the medium and low dose groups, respectively.
Effects of crocetin on LDH, CK, MDA, SOD, GSH-Px, and CAT in H9c2 cells
After 4 h of treatment with 400 µM H2O2, the levels of LDH, CK, and MDA increased appreciably, while the levels of SOD, GSH-Px, and CAT decreased. Pretreatment of 10 µM crocetin for 24 h can reverse the above changes and shows an obvious dose-dependent effect. As a positive control drug, coenzyme Q10 can only change the levels of CK, MDA, and SOD (Figure 2).
The effect of crocetin on ROS in H9c2 cardiomyocytes
As a blank control, H9c2 cardiomyocytes expressed almost no ROS. At the same time, 400 µM H2O2 for 4 h treatment could enhance the ROS level notably, which can be reversed by 10 µM crocetin to some extent (Figure 3). The fluorescence results showed that green fluorescence was very weak in the normal group. In comparison, 400 µM H2O2 for 4 h treatment could enhance the green fluorescence signal, and this enhancement could be reduced by 10 µM crocetin (Figure 3).
Effects of crocetin on H2O2-induced mitochondrial membrane potential and apoptosis
JC-1 staining showed more red fluorescence and less green fluorescence in the blank control group. After 4 h of treatment of 400 µM H2O2, more green fluorescence and less red fluorescence were observed, and 10 µM crocetin could reverse this change to some extent (Figure 4A). TUNEL staining results showed that apoptosis-related signaling was not detected in the blank control group, while the apoptosis-related signaling was appreciably enhanced after 400 µM H2O2 for 4 h of treatment, which could be reversed by 10 µM crocetin to some extent (Figure 4B).
Effects of crocetin on H2O2-induced excessive autophagy
H9c2 cardiomyocytes in the blank control group showed no obvious autophagy flow. Fluorescence showed the appearance of punctate yellow spots in H9c2 cardiomyocytes pretreated with 400 µM H2O2 for 4 h, indicating an obvious over-activation of autophagy. However, this change was reversed after the 10 µM crocetin pretreatment. In the control group, the Ad-mCherry GFP-LC3B virus could only be observed as a weak diffuse yellow background by fluorescence. However, punctate yellow spots were observed after 400 µM H2O2 for 4 h of treatment, and this change was reversed after the 10 µM crocetin pretreatment (Figure 5).
Detection of crocetin on the expression of mitophagy-related proteins
Western blot results showed that in the control group, the expression levels of PINK1 and Parkin were lower. In 4 h H2O2-stimulated H9c2 cardiomyocytes, the expression levels of PINK1 and Parkin increased, while the 10 µM crocetin pretreatment could reduce the increase of PINK1 and Parkin (Figure 6).
Detection of the effect of crocetin on the translocation of Parkin mitochondria
The immunofluorescence results showed that the red fluorescence signal representing Parkin in the blank control group was very weak; however, after 400 µM H2O2 for 4 h of treatment, the red fluorescence signal was enhanced, and colocalization with the green fluorescence representing Tom20 increased. After the pretreatment of 10 µM crocetin, the red fluorescence signal was weakened, and colocalization with the green fluorescence signal was reduced (Figure 7).
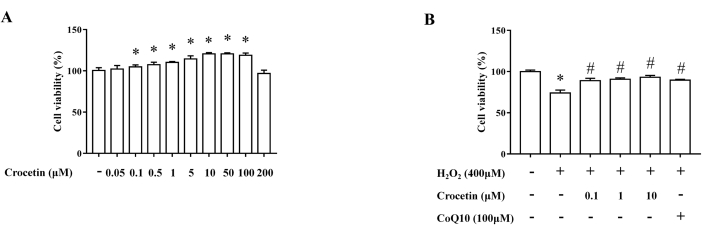
Figure 1: Detection of cell viability by the MTT assay. (A) Effects of crocetin at different concentrations on cell viability (n = 6). (B) Effects of crocetin at different concentrations on cell viability after H202 intervention (n = 6). *p < 0.05 versus control group, #p < 0.05 versus H2O2 treatment group. Please click here to view a larger version of this figure.
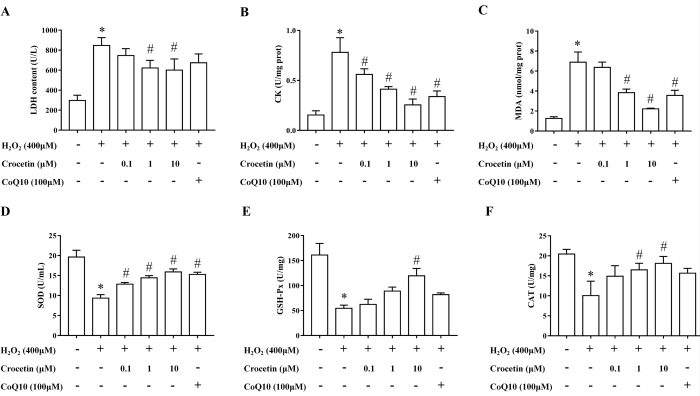
Figure 2: Detection of LDH, CK, MDA, SOD, GSH-Px, and CAT levels. (A) LDH level in cell supernatant (n = 6). (B) CK level in cell lysate (n = 6). (C) MDA level in cell lysate (n = 6). (D) SOD level in cell supernatant (n = 6). (E) GSH-Px level in cell lysate (n = 6). (F) CAT level in cell lysate (n = 6). *p < 0.05 versus blank control group, #p < 0.05 versus H2O2 treatment group. Please click here to view a larger version of this figure.
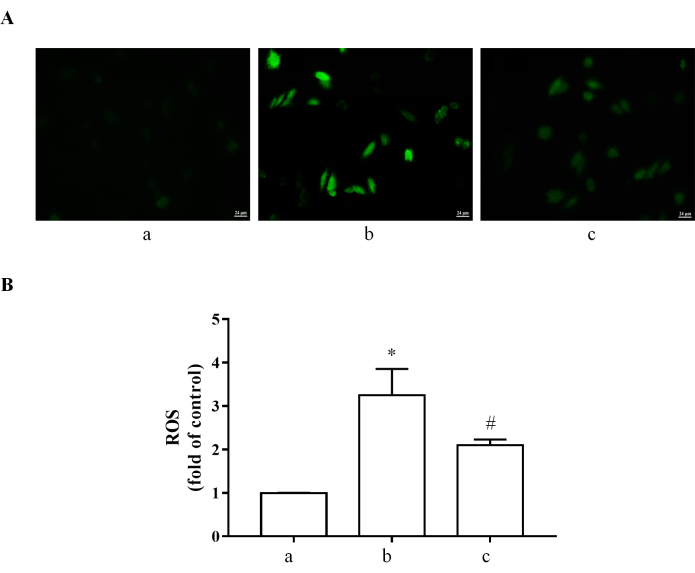
Figure 3: ROS determined by DCFH-DA. (A) DCFH-DA was used to measure ROS levels in H9c2 cardiomyocytes. ROS: green. (B) Quantification data of ROS. (a) H9c2 cardiomyocytes without treatment. (b) H9c2 cardiomyocytes stimulated with 400 µM H2O2 for 4 h. (c) H9c2 cells pretreated with 10 µM crocetin for 24 h and then stimulated with 400 µM H2O2 for 4 h. Scale bar = 24 µm. *p < 0.05 versus blank control group, #p < 0.05 versus H2O2 treatment group. Please click here to view a larger version of this figure.
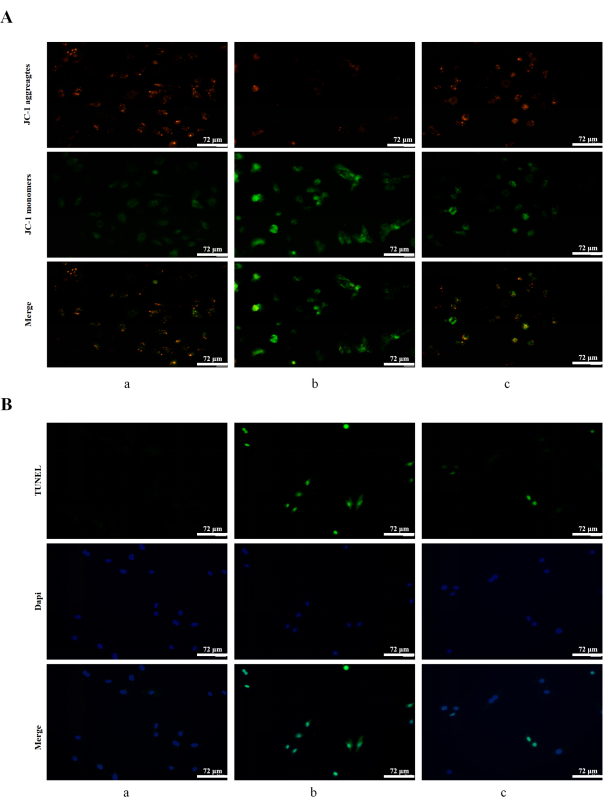
Figure 4: Detection of mitochondrial membrane potential and apoptosis. (A) Mitochondrial membrane potential was determined by JC-1 staining. JC-1 aggregates: red; JC-1 monomers: green. (B) Apoptosis was detected by TUNEL staining in H9c2 cells. TUNEL: green; DAPI: blue. (a) H9c2 cardiomyocytes without treatment. (b) H9c2 cardiomyocytes stimulated with 400 µM H2O2 for 4 h. (c) H9c2 cells pretreated with 10 µM crocetin for 24 h and then stimulated with 400 µM H2O2 for 4 h. Scale bars = 72 µm. Please click here to view a larger version of this figure.
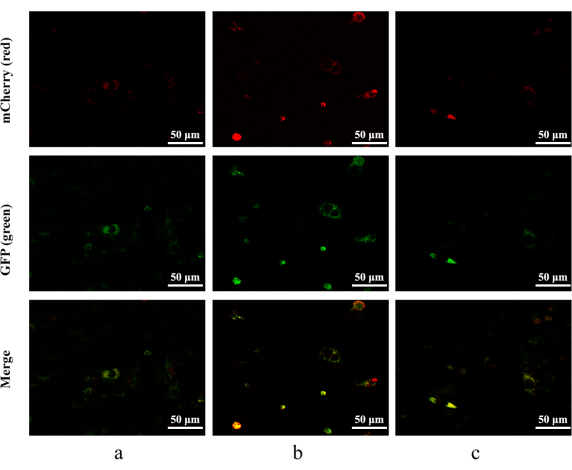
Figure 5: Autophagic flux detected by mCherry-GFP-LC3B adenovirus. mCherry: red; GFP: green. (a) H9c2 cardiomyocytes without treatment. (b) H9c2 cardiomyocytes stimulated with 400 µM H2O2 for 4 h. (c) H9c2 cells pretreated with 10 µM crocetin for 24 h and then stimulated with 400 µM H2O2 for 4 h. Scale bars = 50 µm. Please click here to view a larger version of this figure.
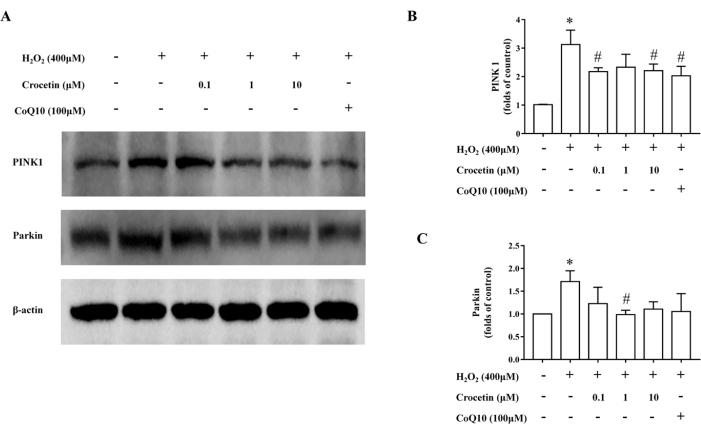
Figure 6: The content of mitophagy-related proteins was detected by western blotting. (A) Representative western blot illustrating PINK1 and Parkin expression. β-actin was adopted as an internal reference. (B) Relative PINK1 expression (n = 3). (C) Relative Parkin expression (n = 3). *p < 0.05 versus control group, #p < 0.05 versus H2O2 treatment group. Please click here to view a larger version of this figure.
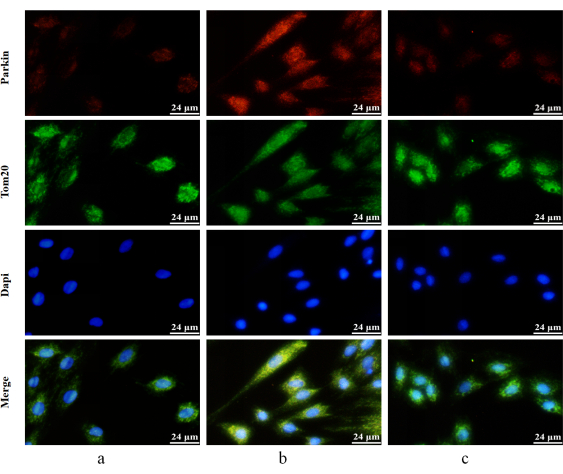
Figure 7: Detection of Parkin's mitochondrial translocation by immunofluorescence double staining. Red fluorescence-labeled Parkin's protein and green fluorescence labeled-Tom20 protein. Parkin: red; Tom20: green; DAPI: blue). (a) H9c2 cardiomyocytes without treatment. (b) H9c2 cardiomyocytes stimulated with 400 µM H2O2 for 4 h. (c) H9c2 cells pretreated with 10 µM crocetin for 24 h and then stimulated with 400 µM H2O2 for 4 h. Scale bars = 24 µm. Please click here to view a larger version of this figure.
Supplementary File 1: The working instructions of LDH, CK, MDA, SOD, GSH-Px, and CAT assays. Please click here to download this File.
Discussion
The exploration of effective ingredients from complex compounds of natural drugs through advanced technology has been a hotspot of TCM research29, and can provide laboratory evidence for future drug development after verification. Safflower is a representative drug in the treatment of "promoting blood circulation and minimizing blood stasis" and is widely used in the treatment of myocardial infarction30,31. Saffron is believed to have similar effects to safflower, and its effect in promoting blood circulation and removing blood stasis is significantly better than safflower31,32. Crocetin is one of the main active components of saffron33, so it was used in the study of this experiment.
H2O2 can cause oxidative stress injury of cardiomyocytes and simulate the myocardial infarction state of cardiomyocytes, which is established as a model of myocardial infarction in vitro34. In this study, a low concentration of crocetin could promote the cell viability of cardiomyocytes, which may be closely related to the activation of mitochondrial energy metabolism. Crocetin can restore the decreased viability of cardiomyocytes induced by H2O2 and has a dose-dependent effect, suggesting that crocetin can improve the oxidative stress damage of cardiomyocytes. Meanwhile, crocetin can effectively reverse myocardial damage and oxidative stress indexes caused by H2O2, further confirming its myocardial protective effect.
The decline in mitochondrial membrane potential is one of the hallmark events in the early stages of apoptosis35. JC-1 dyes aggregate in a potential-dependent manner within the mitochondria. In the normal mitochondrial matrix, JC-1 forms a fluorescent polymer in red. When the mitochondrial membrane potential collapses, JC-1 emits green fluorescence as monomers36. TUNEL detects nuclear DNA strand breaks in the late stages of apoptosis37. Apoptotic cells activate DNA endonuclease enzymes that cut genomic DNA between nucleosomes, and exposed 3'-OH can be detected with green fluorescent probe fluorescein (FITC)-labeled dUTP catalyzed by terminal deoxynucleotidyl transferases37. The results of this study show that the mitochondrial membrane potential decreased and the apoptosis of cardiomyocytes appeared after H2O2 modeling; the changes could be reversed by crocetin to a certain extent, suggesting that crocetin could effectively inhibit the apoptosis of cardiomyocytes caused by oxidative stress.
PINK1/Parkin is a classical pathway that mediates mitophagy38. PINK1 accumulates on the outer mitochondrial membrane after mitochondrial damage and Parkin is recruited to ubiquitinate the extramitochondrial membrane protein, which binds to autophagy-related receptor proteins to form autophagosomes, marking the occurrence of mitophagy39,40,41. The results show that the protein levels of PINK1 and Parkin were increased in cardiomyocytes after H2O2 modeling, suggesting excessive autophagy. After the intervention of crocetin, the protein levels of PINK1 and Parkin in cardiomyocytes treated with H2O2 were reversed to a certain extent, suggesting that it may play a therapeutic role by inhibiting excessive mitochondrial autophagy. In this study, crocetin reduced H2O2-induced oxidative damage and the apoptosis of H9c2 cardiomyocytes, and it is speculated that this effect might be achieved by affecting the PINK1/Parkin pathway to inhibit excessive mitophagy.
This experiment demonstrated the intervention of herbal lyophilized powder on cellular oxidative stress and mitophagy. Using mCherry-GFP-LC3B adenovirus to observe mitochondrial autophagy was a crucial step in the experiment. The key to the success of this step was to increase the infection rate of the cells, and the proviral infection reagent polybrene was added to the medium in advance to increase the infection efficiency greatly. This was achieved by neutralizing the electrostatic repulsion between the cell surface sialic acid and the viral particles, thus facilitating adsorption. It is also worth noting that, as a relatively safe virus, although the adenovirus genome does not integrate into the host cell genome after infection and does not replicate in the cell, it is still potentially biologically dangerous. Therefore, conducting the experiments under strict compliance with regulatory requirements is recommended.
Fluorescent labeling is a common method for detecting mitophagy, but due to its poor specificity, other organelles may be incorrectly labeled and thus interfere with the experimental results41. As technology advances continue, we can expect the development of more precise and reliable fluorescent probes to further explore the mechanism of mitophagy.
Divulgations
The authors have nothing to disclose.
Acknowledgements
This study was supported by the Beijing Natural Science Foundation (No. 7202119) and the National Natural Science Foundation of China (No. 82274380).
Materials
| 0.25% trypsin | Gibco | 2323363 | |
| 1% Penicillin-streptomycin | Sigma | V900929 | |
| 5x protein loading buffer | Beijing Pulilai Gene Technology | B1030-5 | |
| Ad-mCherry GFP-LC3B adenovirus | Beyotime | C3011 | |
| Alexa Fluor 488-conjugated goat anti-rabbit IgG (H+L) | Zhongshan Golden Bridge Biotechnology Co., Ltd. | ZF-0514 | |
| Alexa Fluor 594-conjugated goat anti-mouse IgG (H+L) | Zhongshan Golden Bridge Biotechnology Co., Ltd. | ZF-0513 | |
| Animal-free blocking solution | CST | 15019s | |
| Anti-Parkin antibody | Santa Cruz | sc-32282 | |
| Anti-PINK1 antibody | ABclonal | A11435 | |
| Anti-TOM20 antibody | ABclonal | A19403 | |
| Anti-β-actin antibody | ABclonal | AC026 | |
| BCA protein assay kit | KeyGEN Biotech | KGP902 | |
| Blood cell counting plate | Servicebio | WG607 | |
| CAT assay kits | Nanjing Jiancheng Bioengineering Institute | A007-1-1 | |
| Chemiluminescence detection system | Shanghai Qinxiang Scientific Instrument Factory | ChemiScope 6100 | |
| CK assay kits | Nanjing Jiancheng Bioengineering Institute | A032-1-1 | |
| Coenzyme Q10 (CoQ 10) | Macklin | C6129 | |
| Crocetin | Chengdu Ruifensi Biotechnology Co., Ltd. | RFS-Z01802006012 | |
| DAPI-containing antifluorescence quenching tablets | Zhongshan Golden Bridge Biotechnology Co., Ltd. | ZLI-9557 | |
| DCFH-DA | Beyotime | S0033S | |
| DMSO | Solarbio | D8371 | |
| Dulbecco's modified eagle medium (DMEM) | Gibco | 8122091 | |
| Enhanced Chemiluminescence (ECL) solution | NCM Biotech | P10100 | |
| Fetal bovine serum (FBS) | Corning-Cellgro | 35-081-CV | |
| GraphPad Prism 7.0 | https://www.graphpad.com/ | ||
| GSH-Px assay kits | Nanjing Jiancheng Bioengineering Institute | A005-1-2 | |
| H9c2 myocardial cells | Beijing Dingguochangsheng Biotech Co., Ltd. | CS0062 | |
| Horseradish peroxidase (HRP)-conjugated goat anti-goat IgG (H+L) | Zhongshan Golden Bridge Biotechnology Co., Ltd. | ZB-2305 | |
| Horseradish peroxidase (HRP)-conjugated goat anti-mouse IgG (H+L) | Zhongshan Golden Bridge Biotechnology Co., Ltd. | ZB-2301 | |
| JC-1 mitochondrial membrane potential assay kit | LABLEAD | J22202 | |
| LDH assay kits | Nanjing Jiancheng Bioengineering Institute | A020-2-2 | |
| MDA assay kits | Nanjing Jiancheng Bioengineering Institute | A003-2-2 | |
| Methanol | Aladdin | A2114057 | |
| MTS assay | Promega | G3581 | |
| Perhydrol | G-clone | CS7730 | |
| Phosphatase inhibitor | CWBIO | CW2383 | |
| Polybrene | Beyotime | C0351 | |
| Polyvinylidene difluoride (PVDF) membranes | Millipore | ISEQ00010 | |
| Radioimmunoprecipitation assay (RIPA) lysis buffer | Solarbio | R0010 | |
| SDS-PAGE gels | Shanghai Epizyme Biomedical Technology | PG112 | |
| SDS-PAGE running buffer powder | Servicebio | G2018-1L | |
| SDS-PAGE transfer buffer powder | Servicebio | G2017-1L | |
| SOD assay kits | Nanjing Jiancheng Bioengineering Institute | A001-2-2 | |
| Tris-buffered saline powder | Servicebio | G0001-2L | |
| Triton X-100 | Sigma | SLCC9172 | |
| TUNEL apoptosis assay kit | Beyotime | C1086 | |
| Tween-20 | Solarbio | T8220 |
References
- Anderson, J. L., Morrow, D. A. Acute myocardial infarction. The New England Journal of Medicine. 376 (21), 2053-2064 (2017).
- Samsky, M. D., et al. Cardiogenic shock after acute myocardial infarction: a review. JAMA. 326 (18), 1840-1850 (2021).
- Abbate, A., et al. Survival and cardiac remodeling benefits in patients undergoing late percutaneous coronary intervention of the infarct-related artery: evidence from a meta-analysis of randomized controlled trials. Journal of the American College of Cardiology. 51 (9), 956-964 (2008).
- Santoro, G. M., Carrabba, N., Migliorini, A., Parodi, G., Valenti, R. Acute heart failure in patients with acute myocardial infarction treated with primary percutaneous coronary intervention. European Journal of Heart Failure. 10 (8), 780-785 (2008).
- Dhruva, S. S., et al. Association of use of an intravascular microaxial left ventricular assist device vs intra-aortic balloon pump with in-hospital mortality and major bleeding among patients with acute myocardial infarction complicated by cardiogenic shock. JAMA. 323 (8), 734-745 (2020).
- Wang, Y., et al. Risk factors associated with major cardiovascular events 1 year after acute myocardial infarction. JAMA Network Open. 1 (4), e181079 (2018).
- Jou, M. J., et al. Melatonin protects against common deletion of mitochondrial DNA-augmented mitochondrial oxidative stress and apoptosis. Journal of Pineal Research. 43 (4), 389-403 (2007).
- La Piana, G., Fransvea, E., Marzulli, D., Lofrumento, N. E. Mitochondrial membrane potential supported by exogenous cytochrome c oxidation mimics the early stages of apoptosis. Biochemical and Biophysical Research Communications. 246 (2), 556-561 (1998).
- De Filippo, O., et al. Impact of secondary prevention medical therapies on outcomes of patients suffering from Myocardial Infarction with NonObstructive Coronary Artery disease (MINOCA): A meta-analysis. International Journal of Cardiology. 368, 1-9 (2022).
- Davidson, S. M., et al. Multitarget strategies to reduce myocardial ischemia/reperfusion injury: JACC review topic of the week. Journal of the American College of Cardiology. 73 (1), 89-99 (2019).
- Caricati-Neto, A., Errante, P. R., Menezes-Rodrigues, F. S. Recent advances in pharmacological and non-pharmacological strategies of cardioprotection. International Journal of Molecular Sciences. 20 (16), 4002 (2019).
- Chen, G. Y., et al. Network pharmacology analysis and experimental validation to investigate the mechanism of total flavonoids of rhizoma drynariae in treating rheumatoid arthritis. Drug Design, Development, and Therapy. 16, 1743-1766 (2022).
- Wei, Z., et al. Traditional Chinese medicine has great potential as candidate drugs for lung cancer: A review. Journal of Ethnopharmacology. 300, 115748 (2023).
- Zhi, W., Liu, Y., Wang, X., Zhang, H. Recent advances of traditional Chinese medicine for the prevention and treatment of atherosclerosis. Journal of Ethnopharmacology. 301, 115749 (2023).
- Liu, M., et al. Hypertensive heart disease and myocardial fibrosis: How traditional Chinese medicine can help addressing unmet therapeutical needs. Pharmacological Research. 185, 106515 (2022).
- Zhang, X. X., et al. Traditional Chinese medicine intervenes ventricular remodeling following acute myocardial infarction: evidence from 40 random controlled trials with 3,659 subjects. Frontiers in Pharmacology. 12, 707394 (2021).
- Hao, P., et al. Traditional Chinese medicine for cardiovascular disease: evidence and potential mechanisms. Journal of the American College of Cardiology. 69 (24), 2952-2966 (2017).
- Delgado-Montero, A., et al. Blood stasis imaging predicts cerebral microembolism during acute myocardial infarction. Journal of the American Society of Echocardiography. 33 (3), 389-398 (2020).
- Lu, C. Y., Lu, P. C., Chen, P. C. Utilization trends in traditional Chinese medicine for acute myocardial infarction. Journal of Ethnopharmacology. 241, 112010 (2019).
- Gao, Z. Y., Xu, H., Shi, D. Z., Wen, C., Liu, B. Y. Analysis on outcome of 5284 patients with coronary artery disease: the role of integrative medicine. Journal of Ethnopharmacology. 141 (2), 578-583 (2012).
- Huang, Z., et al. Crocetin ester improves myocardial ischemia via Rho/ROCK/NF-kappaB pathway. International Immunopharmacology. 38, 186-193 (2016).
- Green, M. R., Sambrook, J. Estimation of cell number by hemocytometry counting. Cold Spring Harbor Protocols. 2019 (11), (2019).
- Zeng, Q., et al. Assessing the potential value and mechanism of Kaji-Ichigoside F1 on arsenite-induced skin cell senescence. Oxidative Medicine and Cellular Longevity. 2022, 9574473 (2022).
- Chazotte, B. Labeling mitochondria with JC-1. Cold Spring Harbor Protocols. 2011 (9), (2011).
- Kyrylkova, K., Kyryachenko, S., Leid, M., Kioussi, C. Detection of apoptosis by TUNEL assay. Methods in Molecular Biology. 887, 41-47 (2012).
- Yuan, Y., et al. Palmitate impairs the autophagic flux to induce p62-dependent apoptosis through the upregulation of CYLD in NRCMs. Toxicology. 465, 153032 (2022).
- Kurien, B. T., Scofield, R. H. Western blotting. Methods. 38 (4), 283-293 (2006).
- Chen, G. Y., et al. Total flavonoids of rhizoma drynariae restore the MMP/TIMP balance in models of osteoarthritis by inhibiting the activation of the NF-κB and PI3K/AKT pathways. Evidence-Based Complementary and Alternative. 2021, 6634837 (2021).
- Amin, A., Hamza, A. A., Bajbouj, K., Ashraf, S. S., Daoud, S. Saffron: a potential candidate for a novel anticancer drug against hepatocellular carcinoma. Hepatology. 54 (3), 857-867 (2011).
- Kamalipour, M., Akhondzadeh, S. Cardiovascular effects of saffron: an evidence-based review. The Journal of Tehran Heart Center. 6 (2), 59-61 (2011).
- Mani, V., Lee, S. K., Yeo, Y., Hahn, B. S. A metabolic perspective and opportunities in pharmacologically important safflower. Metabolites. 10 (6), 253 (2020).
- Broadhead, G. K., Chang, A., Grigg, J., McCluskey, P. Efficacy and safety of saffron supplementation: current clinical findings. Critical Reviews in Food Science and Nutrition. 56 (16), 2767-2776 (2016).
- Gao, H., et al. Insight into the protective effect of salidroside against H2O2-induced injury in H9C2 cells. Oxidative Medicine and Cellular Longevity. 2021, 1060271 (2021).
- Chen, G. Y., et al. Prediction of rhizoma drynariae targets in the treatment of osteoarthritis based on network pharmacology and experimental verification. Evidence-Based Complementary and Alternative. 2021, 5233462 (2021).
- Reers, M., et al. Mitochondrial membrane potential monitored by JC-1 dye. Methods in Enzymology. 260, 406-417 (1995).
- Radovits, T., et al. Poly(ADP-ribose) polymerase inhibition improves endothelial dysfunction induced by reactive oxidant hydrogen peroxide in vitro. European Journal of Pharmacology. 564 (1-3), 158-166 (2007).
- Song, M., et al. Interdependence of parkin-mediated mitophagy and mitochondrial fission in adult mouse hearts. Circulation Research. 117 (4), 346-351 (2015).
- Gan, Z. Y., et al. Activation mechanism of PINK1. Nature. 602 (7896), 328-335 (2022).
- Nguyen, T. N., Padman, B. S., Lazarou, M. Deciphering the molecular signals of PINK1/Parkin mitophagy. Trends in Cell Biology. 26 (10), 733-744 (2016).
- Yamada, T., Dawson, T. M., Yanagawa, T., Iijima, M., Sesaki, H. SQSTM1/p62 promotes mitochondrial ubiquitination independently of PINK1 and PRKN/parkin in mitophagy. Autophagy. 15 (11), 2012-2018 (2019).
- Klionsky, D. J., et al. Guidelines for the use and interpretation of assays for monitoring autophagy (4th edition). Autophagy. 17 (1), 1 (2021).

