Cognitive Function and Upper Limb Rehabilitation Training Post-Stroke Using a Digital Occupational Training System
Summary
The current protocol outlines how the VR-based digital occupational training system enhances the rehabilitation of patients with cognitive impairment and upper limb dysfunction following a stroke.
Abstract
Stroke rehabilitation often requires frequent and intensive therapy to improve functional recovery. Virtual reality (VR) technology has shown the potential to meet these demands by providing engaging and motivating therapy options. The digital occupational training system is a VR application that utilizes cutting-edge technologies, including multi-touch screens, virtual reality, and human-computer interaction, to offer diverse training techniques for advanced cognitive capacity and hand-eye coordination abilities. The objective of this study was to assess the effectiveness of this program in enhancing cognitive function and upper extremity rehabilitation in stroke patients. The training and assessment consist of five cognitive modules covering perception, attention, memory, logical reasoning, and calculation, along with hand-eye coordination training. This research indicates that after eight weeks of training, the digital occupational training system can significantly improve cognitive function, daily living skills, attention, and self-care abilities in stroke patients. This software can be employed as a time-saving and clinically effective rehabilitation aid to complement traditional one-on-one occupational therapy sessions. In summary, the digital occupational training system shows promise and offers potential financial benefits as a tool to support the functional recovery of stroke patients.
Introduction
There is a high incidence, mortality, disability rate, and recurrence associated with stroke, or cerebrovascular accident1. Globally, stroke has surpassed tumors and heart disease to become the second leading cause of death, and it is the primary cause in China2. The incidence and social burden of stroke are expected to increase significantly in the coming years as the population ages. Survivors of stroke may continue to experience sensory, motor, cognitive, and psychological impairments3. The effects of a stroke can include paralysis of one side of the body, including the face, arms, and legs, a condition known as hemiplegia. This is the most common sequel to stroke and significantly impacts people’s quality of life4.
Stroke poses a significant threat to people’s health. Due to brain tissue damage, stroke and hemiplegia can result in hand dysfunction, hindering patients’ activities of daily living (ADLs) and diminishing their quality of life5. Decreased upper limb function, especially of the hands as the distal body part, presents the most significant challenge in upper limb recovery6. Therefore, functional rehabilitation is crucial. Additionally, 20%-80% of stroke patients experience cognitive impairment, leading to deficits in attention, memory, language, and executive abilities7.
Currently, the clinical rehabilitation of upper limb hemiplegia primarily relies on comprehensive upper limb training and various occupational therapies (e.g., mirror box treatment8, suspension9, functional electrical stimulation10, among others). Recently, virtual reality and interactive video games have emerged as alternative rehabilitation methods. These interventions can facilitate high-capacity practice and reduce demands on therapists’ time11. Virtual reality systems have rapidly evolved into new commercial devices that can be utilized to enhance cognitive and upper limb motor function in stroke survivors12. Despite these advancements, there are still unexplored avenues in this field.
Therefore, this study aims to investigate the effects of upper limb rehabilitation training combined with conventional upper limb rehabilitation on cognitive and upper limb motor function in stroke patients during the recovery period of hemiparesis, typically spanning the initial 6-24 weeks after the incident stroke. Additionally, we will examine its impact on daily life abilities. This research seeks to provide valuable evidence for the clinical application of robotic interventions.
Protocol
This study protocol received approval from the ethics committee of the First Affiliated Hospital of Zhejiang University (approval number IIT20210035C-R2), and informed consent was obtained from all participants. An experimental study employing quasi-randomization, single-blinding, and a control group was conducted to assess the feasibility and effectiveness of the program. 24 patients hospitalized in the rehabilitation medicine ward of the First Affiliated Hospital of Zhejiang University were invited to participate in this experiment. Inclusion criteria encompassed stroke patients confirmed by computed tomography (CT) or magnetic resonance imaging (MRI), aged 30-75 years, 6-24 weeks post-stroke, a Montreal Cognitive Rating Scale (MoCA) score <2613, upper limb dysfunction14, unilateral hemiplegia, Brunnstrom stage 3-6 for sitting ability15, and cooperation for assessment and treatment. Exclusion criteria included a history of cognitive disorders, major organ dysfunction, visual or hearing impairment, abnormal mental behavior or antipsychotic drug use, severe spasticity (Ashworth scale 3-4)16, and shoulder subluxation or severe upper limb pain.
1. Study design
- Divide all the patients into the control group and the experimental group (12 in each group) according to the random number table method2.
NOTE: Before the experiment, the following assessments were completed by an experienced occupational therapist for all patients: The Montreal Cognitive Assessment (MoCA)13, Fugl-Meyer Assessment Upper Extremity Scale (FMA-UE)14, and Modified Barthel Index (MBI)17. - Verify and confirm that patients in the experimental group underwent conventional drug therapy, including medications for antihypertensives, antidiabetics, antiplatelets, lipid-regulating agents, etc., as prescribed by their respective physicians.
- Additionally, ensure that they received 30 min of routine occupational therapy training each day, comprising cognitive function training and upper limb function training. Furthermore, confirm that they dedicated 30 min daily to the digital occupational training system for a duration of 8 weeks.
NOTE: The term "conventional drug therapy" refers to standard medications prescribed for post-stroke care, and the specific medications may vary among patients and clinics.
- Additionally, ensure that they received 30 min of routine occupational therapy training each day, comprising cognitive function training and upper limb function training. Furthermore, confirm that they dedicated 30 min daily to the digital occupational training system for a duration of 8 weeks.
- Ensure that patients in the control group receive routine occupational therapy (OT) for 1 h each day, in conjunction with conventional drug therapy.
- Implement routine cognitive function training tailored to the types of patients' cognitive impairment following the steps below:
NOTE: Both control and experimental group of patients receive these trainings.- For Memory dysfunction: Guide patients to engage in activities such as discussing pictures, reciting paragraphs, path memory exercises, and recalling life plots.
- For Attention dysfunction: Instruct patients to participate in eye tracking training, number classification exercises, and similar picture recognition training.
- For Dyscalculia: Request patients to perform simple addition and subtraction exercises involving numbers less than 50, along with activities like shopping and financial simulation training.
- For Visuospatial disturbance: Guide patients through activities such as stacking wood, solving jigsaw puzzles, drawing, and turning objects.
- For Executive dysfunction: Lead patients in activities like origami, hand-making, painting, watering flowers, and others.
- For Thinking and reasoning dysfunction: Guide patients in classifying items, arranging numbers, simulating supermarket shopping, progressing from general reasoning to specific reasoning.
- Instruct patients to engage in conventional upper limb functional exercises, encompassing passive and dominant movements of each joint of the upper limb. This includes activities like roller training, upper limb extraction, throwing and catching the ball, and control training for shoulder, elbow, and wrist movements.
- Additionally, include forearm pronation and supination, finger fine movements, and coordination flexibility training, such as using a pin board and screw screwing.
NOTE: Dressing and stripping training, self-help equipment application, and other exercises to enhance the ability of daily living activities should primarily focus on the affected side, with appropriate incorporation of the healthy side to assist in the training of the affected side. All experimental steps are conducted in the rehabilitation room of the ward. The mentioned training is carried out 5 days a week for a duration of 8 weeks.
- Additionally, include forearm pronation and supination, finger fine movements, and coordination flexibility training, such as using a pin board and screw screwing.
2. Training process of the digital occupational training system
NOTE: Only the experimental group receive these trainings.
- Instruct the patient to stand or sit in front of the device (Figure 1) and adjust the display to an appropriate height and tilt angle, allowing easy access for the patient's hands to touch the screen.
- Create an individualized profile for each patient, including their full name, age, hospitalization identification number, diagnosis, and other relevant medical details.
- Select the appropriate training program based on the patient's cognitive impairment type and the remaining muscle strength of the upper extremities. Set parameters for each program, such as training duration, difficulty level, and left or right side (Figure 2).
- Explain and demonstrate the correct operation method for each program to ensure the patient fully comprehends the purpose of the training.
- Conduct Cognitive function training.
- For patients with Memory dysfunction, follow the training process as mentioned below.
NOTE: If the patient has memory dysfunction, therapists can choose from the following training procedures: "Rapid Matching Training," "Memory Matrix Training," and "Card Memory Training."- Rapid Matching Training: Click pictures on the screen and ask the patient to remember the previous picture. Then ask the patient to click on the Icon button to confirm whether the current picture matches the previous one.
- Memory Matrix Training: Click to make three bright squares flash at different locations on the screen matrix. Then, click to darken all squares and ask the patient to click on the bright squares.
- Card Memory Training: Click to display two pictures on the screen and then flip them over. Instruct the patient to find the target card that matches the one shown on the screen.
- For patients with Attention dysfunction, conduct the following training process.
NOTE: For patients with attention dysfunction, select from the following training procedures: "Reaction Ability Training," "Color Matching Training," "Whack-A-Mole Game," and "Card Memory Training."- Reaction Ability Training: When a cake falls above the cartoon avatar, instruct the patient to quickly click on the catch button to prevent the cake from hitting the head.
- Color Matching Training: When the ball above the track is close to the center of the circle, guide the patient to click on the corresponding color to make the ball bounce, either two or four beats depending on the difficulty.
- Whack-A-Mole Game: Introduce a game where the bad guy crosses the land, or the gopher sticks its head out. Instruct the patient to click and hit the bad guy or the gopher to earn game points.
- Card Memory Training: Display card information, flip the card, and change its position. Ask the patient to find and click on the target card again according to the specified requirements.
- For patients with Numeracy and judgment impairment, conduct the following training process.
NOTE: When the patient has numeracy and judgment impairment, therapists should choose programs such as "Rock-Paper-Scissors," "Arithmetic Reasoning Training," "Sorting and Picking Training," and "Fishing Game."- Rock-Paper-Scissors: Display a left-right hand gesture on the screen and ask the patient to make a quick judgment, clicking to determine whether the left-hand wins, the right-hand wins, or it's a tie.
- Arithmetic Reasoning Training: Instruct the patient to calculate the arithmetic problem on the screen and compare it to the number, selecting the greater than, less than, or equal button. Increase the difficulty of the arithmetic problem with the setting's difficulty level.
- Sorting and Picking Training: Ask the patient to pick and click on the appropriate type and quantity of items from the list according to the requirements in the upper left corner.
- Fishing Game: Following the prompt information, instruct the patient to click on the screen to catch a specific type and number of fish to earn game scores.
- For patients with Visuospatial disturbance, conduct the following training sessions.
NOTE: The following training procedures are suitable for patients with visuospatial disturbance: "Unilateral Neglect Training," "Jigsaw Puzzle Training," "Picture Combination Training."- Unilateral Neglect Training: Click according to the video prompts to control the swimming red fish with the fingers and eat as many fish as possible.
- Jigsaw Puzzle Training: Click and put the broken pieces of the puzzle into the correct position so that they form a complete picture again.
- Picture Combination Training: Select appropriate pictures from various shapes and colors on the left and place them in the correct position on the right to combine and form a specific pattern.
- For patients with Executive dysfunction, conduct the following training sessions.
NOTE: Patients with executive dysfunction can choose the "Virtual Kitchen" program. Patients can gradually complete the production process of "scrambled tomato and egg" virtually under the guidance of the system. Specific steps are as follows:- Prepare food materials: Instruct the patient to virtually (on screen) turn on the faucet, clean the tomatoes, cut the tomatoes into pieces, and place them on the plate. Then, put the eggs into the bowl and stir them.
- Cooking: Instruct the patients to fire up the stove, pour the cooking oil, pour the beaten eggs, and then add the tomatoes.
- Serve the dishes: After completion, guide the patient to turn off the heat and transfer the cooked dish onto the plate.
- For patients with Thinking and reasoning dysfunction, conduct the following.
NOTE: If the patient has naming and conceptual difficulties, choose from "Naming Training," "Card Memory Exercise," and "Object Differentiation Training."- Naming Training: Guide patients to find and click on the correct picture among multiple pictures based on the requirements of text information and sound, or choose and click on the correct name of the item according to the picture information prompts.
- Card Memory Exercise: Among the cards that appear on the screen, ask the patients to find and click the one that is the same as the one in the hand of the cartoon man in the upper right corner.
- Object Differentiation Training: Among several columns of shapes appearing on the screen, ask the patients to identify and click the one that is unique and different from the others.
- For patients with Memory dysfunction, follow the training process as mentioned below.
- Conduct Upper limb functional training.
- Train the patients with Auxiliary exercises or one-handed exercises.
NOTE: If the affected limb is unable to complete the training alone, have the healthy hand hold the affected limb and complete auxiliary training. Once the affected limb regains a certain level of muscle strength, one-handed training can be initiated. The following training procedures are suitable for auxiliary exercises or one-handed exercises: "Drawing Exercise," "Musical Journey," "Walking The Maze."- Drawing Exercise: According to the path prompts appearing on the screen, instruct the patients to draw specific lines or outlines of the pattern. The system will automatically generate a beautiful picture. As the difficulty increases, consider allowing the path to disappear and ask the patient to outline the picture from memory.
- Musical Journey: Have the patient erase gray squares on the screen in sync with the rhythm of the music, transforming them into colorful squares. This provides an intensely pleasurable experience.
- Walking The Maze: Instruct the patient to hold onto the small ball in the maze and guide the ball through the maze to reach the endpoint where the diamond is located.
- Train the patients with Two-handed coordination exercises.
NOTE: If the affected limb has good muscle strength, two-hand coordination training can be initiated. Choose procedures such as "Balance Ball," "Fish Feeding Game," "Archery Practice," and "Reaction Coordination Training."- Balance Ball: Have the patient place their left and right fists on both ends of the balance beam, which has a small blue ball on it. Instruct them to maintain balance and prevent the ball from rolling off either side.
- Fish Feeding Game: Instruct patients to hold down the feed with one hand and click on the small fish swimming on the screen with the other hand to complete the fish feeding task.
- Archery Practice: Guide the patient to place one hand on the bow and the other on the arrow, clicking and controlling the arrow so that it hits the bull's eye perfectly.
- Reaction Coordination Training: Let the right and left hands of the patients hold down the hammer and click to hit the yellow ball alternately, similar to the game of ping-pong, to train the patient's coordination and reaction ability.
NOTE: Upon the completion of training for each procedure, the instrument automatically provides an analysis of the training results, storing them in the patient's exclusive file. The therapist evaluates the patient's training effect by comparing the results each time (Figure 3 and Figure 4).
- Train the patients with Auxiliary exercises or one-handed exercises.
- As the patient's function recovers, ask the therapist to regularly recombine the training program, adjusting the difficulty and duration of the procedure based on the patient's performance.
NOTE: Throughout the training period, the therapist supervises the entire training process of the patient, patiently listens to the patient's needs, assists the patient when encountering difficulties, and offers praise and encouragement upon successful completion of training tasks.
3. Follow up procedures
- Following 8 weeks of treatment, conduct a reassessment of all patients using the MoCA, FMA-UE, and MBI. This reassessment is carried out by the same occupational therapist.
- Statistically analyze the collected data from the pre- and post-training assessments to determine the significance of the outcomes.
NOTE: Appropriate statistical methods were employed, depending on the normality of the data distribution, to assess the impact of the digital occupational training system on the recovery of cognitive and motor functions.
Representative Results
In this study, 24 patients were enrolled presenting with upper limb dysfunction combined with various types of cognitive impairment following a stroke. The observed types of cognitive impairment included Amnesia, Agnosia, Executive Dysfunction, Attentional Impairments, among others. No statistically significant differences were found between the two groups in terms of sex, age, duration of disease, and type of stroke (P > 0.05), as detailed in Table 1. The experimental group, which underwent upper limb rehabilitation using the digital occupational training system, exhibited greater improvements in FMA-UE14, MoCA13, and MBI17 compared to conventional therapy (Table 2).
Following the training period, the experimental group demonstrated a significant improvement in MoCA scores (P < 0.05), while the control group did not show significant differences (P > 0.05). Moreover, the improvement in the experimental group was more pronounced than in the control group (P < 0.05) (Table 2). Regarding FMA upper limb scores, the experimental group showed significant improvement after 8 weeks of training (P < 0.05), with a notable difference in improvement compared to the control group (P < 0.05) (Table 2). Concerning BI scores, both groups exhibited significant improvements compared to before the intervention (P < 0.05), and the improvement in the experimental group was significantly different from that in the control group (P < 0.05) (Table 2). These findings underscore the effectiveness of the digital occupational training system in enhancing patients' cognitive and upper limb abilities, surpassing traditional rehabilitation therapy in cognitive improvements.
Statistical analyses were conducted using a statistical software (see Table of Materials), with the significance level set at a two-tailed P < 0.05. Parametric analysis, assuming data normality and homogeneity of variance, employed the independent samples t-test to compare differences between groups in scale scores.

Figure 1: Digital Occupational Training System. The system's screen is positioned at an ergonomically suitable height and angle for stroke patients in a seated or standing position, promoting interactive engagement for rehabilitation exercises. Please click here to view a larger version of this figure.
Figure 2: Game content and application of cognitive-based upper limb VR scheme. This figure graphically illustrates various tasks within the game, each meticulously designed to target specific cognitive and motor skills. Please click here to view a larger version of this figure.
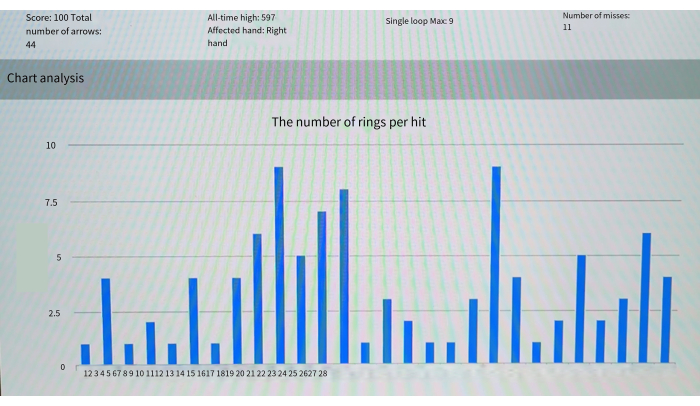
Figure 3: Analysis of archery game training results – the number of rings per target hit. This figure provides a statistical breakdown of participants' performances within the archery game, visualizing the number of rings hit per target across multiple sessions. Please click here to view a larger version of this figure.
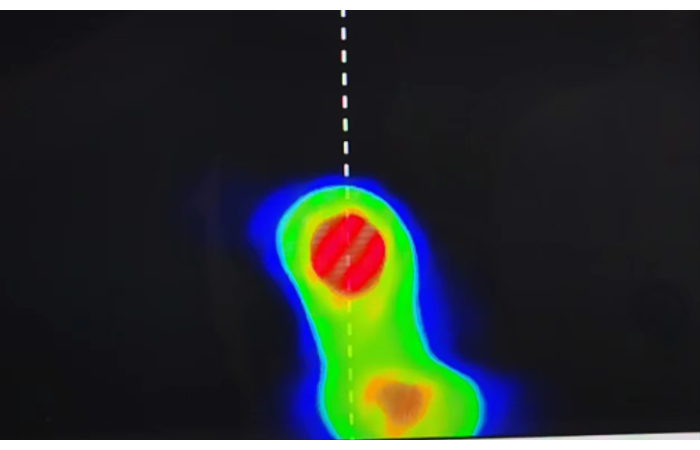
Figure 4: Analysis of archery game training results map of active areas. The color gradients represent areas of high and low activity, providing insight into the accuracy and focal points of participants' attempts, thus serving as a visual tool to assess motor control and coordination throughout the training. Please click here to view a larger version of this figure.
| Group | n | Sex (n) | Age (x±s, y ) | Course of the disease (x±s, d) | Type of stroke (n) | Hemiplegic side (n) | |||||
| Male | Female | Ischemic | Hemorrhagic | Left | Right | ||||||
| Control group (n = 12) | 12 | 6 | 6 | 50.50 ± 5.50 | 37.08 ± 11.48 | 7 | 5 | 7 | 5 | ||
| Experimental group (n = 12) | 12 | 7 | 5 | 50.42 ± 5.52 | 36.0 ± 10.86 | 8 | 4 | 6 | 6 | ||
| P | >0.05 | >0.05 | >0.05 | >0.05 | >0.05 | ||||||
Table 1. Baseline characteristics between the two groups. It presents a comprehensive comparison of baseline characteristics between the control and experimental groups. This includes demographic and clinical data, ensuring comparability between the groups and verifying the randomization process, hence confirming the robustness of the subsequent analysis.
| Group | MoCA | FMA-UE | MBI | |
| Control group (n = 12) | Per-treatment | 18.25 ± 2.42 | 31.83 ± 6.26 | 57.42 ± 7.37 |
| Post-treatment | 19.0 ± 3.16 | 35.58 ± 5.04 | 64.33 ± 6.51 * | |
| Experimental group (n = 12) | Per-treatment | 18.33 ± 2.34 | 32.42 ± 5.84 | 57.33 ± 9.50 |
| Post-treatment | 22.00 ± 2.92 **# | 40.67 ± 6.72**# | 71.42 ± 9.63 **# | |
| *P < 0.05, compared to pre-treatment; #P < 0.05, compared to the control group | ||||
Table 2. Comparison of MoCA, FMA-UE, and MBI scores between two groups before and after training (x ± s). *P < 0.05, compared to pre-treatment. #P < 0.05, compared to the control group. The statistically significant values are highlighted, elucidating the impact of the VR-based training regime on cognitive and motor functions and showcasing the relevant improvements in participants' capabilities post-training.
Discussion
A virtual reality rehabilitation system was implemented to support the recovery of stroke patients, utilizing the latest multi-touch screen technology to enhance training engagement, immersion, interactivity, and conceptualization. This system provides interactive upper limb motor control training that integrates vision, hearing, and touch. It also includes rehabilitation training modules targeting memory, attention, spatial perception, computing, hand-eye coordination, and virtual tasks, offering personalized cognitive training. Moreover, the digital rehabilitation enhances cognitive and upper limb recovery through enriched virtual activities of daily living (ADL) and cognitive training18,19.
The current approach to cognitive function rehabilitation post-stroke typically involves computer-assisted training and occupational therapy, sometimes supplemented by methods like hyperbaric oxygen therapy and transcranial electrical stimulation20. In contrast, the VR-based training system described here offers high-intensity, repetitive, and highly reproducible motor training21. The system intelligently adjusts game difficulty levels based on a patient’s rehabilitation progress, tailoring tasks for high-intensity training. Additionally, virtual reality games are accessible at any time and place, enabling patients to engage in rehabilitation training more frequently and achieve a higher number of repetitions.
Compared to existing VR devices, the digital occupational training system stands out as a more personalized and flexible rehabilitation option, concentrating patients’ efforts and attention for improved outcomes. Active participation by patients is crucial during neuroplasticity, motor learning, and rehabilitation. Combining rehab therapy with patients’ voluntary exercise has been found to promote the recovery of lost motor capabilities22,23. This virtual rehabilitation offers advantages in motivation, safety, and customization, while also allowing for the monitoring and analysis of users’ performance during training. Evaluations using a 7-point Likert-type scale have shown positive results, indicating improved acceptability, expectation effectiveness, satisfactoriness, and stability of the VR system24. Based on feedback from occupational therapists and individuals with cognitive impairment, the results suggest that this training system is both feasible and usable.
The virtual reality device can increase task repetitions (intensity) by enhancing enjoyment to encourage engagement in specific tasks. In comparison to existing VR devices, the digital occupational training system offers a more diverse range of cognitive and activities of daily living (ADL) training games. Low-cost virtual rehabilitation systems can serve as supplements to conventional rehabilitation, requiring reduced direct supervision. The utilization of motion sensors alongside VR systems allows rehabilitation professionals to digitally assess and track patients’ functions25. Rehabilitation based on a digital training system is a promising tool that enables patients to actively participate in rehabilitation plans and achieve better recovery of motor functions.
However, there are lingering questions, such as identifying the primary beneficiaries of virtual reality rehabilitation, assessing the impact of immersive vs. non-immersive experiences, and determining the most effective feedback mechanisms26. Virtual reality can also be integrated into new therapeutic modalities, such as brain-computer interfaces and noninvasive brain stimulation, to enhance neuroplasticity and improve recovery outcomes27. The study faced limitations, including challenges related to gesture recognition, the need for precise motion angle and timing adjustments based on patients’ motor capabilities, and the requirement for careful implementation of threshold limits6. Additionally, the relatively small sample size restricts the generalizability of the findings.
In conclusion, cognitive function training through a digital rehabilitation system significantly improves cognition, upper limb motor function, and ADL capabilities in stroke patients. This approach holds substantial potential for clinical rehabilitation and could be expanded to benefit more stroke rehabilitation centers in the future. Furthermore, the versatility of this method allows its application in various rehabilitation fields, including trauma recovery and the treatment of neurodegenerative diseases.
Divulgations
The authors have nothing to disclose.
Acknowledgements
We thank the patients and healthcare staff of the First Affiliated Hospital of Zhejiang University School of Medicine for their support and cooperation throughout this study.
Materials
| FlexTable digital occupational training system | Guangzhou Zhanghe Intelligent Technology Co., Ltd. | Observation on the rehabilitation effect of digital OT cognitive function training on stroke patients with decreased attention function | FlexTable digital operation training system uses the latest multi-touch screen technology, virtual reality and human-computer interaction technology, integrates a variety of training methods, and provides digital advanced brain function and hand-eye coordination training |
| SPSS 25.0 | IBM | https://www.ibm.com/support/pages/downloading-ibm-spss-statistics-25 |
References
- Feigin, V. L., et al. World stroke organization (wso): Global stroke fact sheet 2022. Int J Stroke. 17 (1), 18-29 (2022).
- Liu, G., Cai, H., Leelayuwat, N. Intervention effect of rehabilitation robotic bed under machine learning combined with intensive motor training on stroke patients with hemiplegia. Front Neurorobot. 16, 865403 (2022).
- Langhorne, P., Bernhardt, J., Kwakkel, G. Stroke rehabilitation. Lancet. 377 (9778), 1693-1702 (2011).
- Feigin, V. L., Lawes, C. M., Bennett, D. A., Barker-Collo, S. L., Parag, V. Worldwide stroke incidence and early case fatality reported in 56 population-based studies: A systematic review. Lancet Neurol. 8 (4), 355-369 (2009).
- Han, Y., Xu, Q., Wu, F. Design of wearable hand rehabilitation glove with bionic fiber-reinforced actuator. IEEE J Transl Eng Health Med. 10, 2100610 (2022).
- Gu, Y., et al. A review of hand function rehabilitation systems based on hand motion recognition devices and artificial intelligence. Brain Sci. 12 (8), 1079 (2022).
- Baltaduonienė, D., Kubilius, R., Berškienė, K., Vitkus, L., Petruševičienė, D. Change of cognitive functions after stroke with rehabilitation systems. Translational Neuroscience. 10 (1), 118-124 (2019).
- Samuelkamaleshkumar, S., et al. Mirror therapy enhances motor performance in the paretic upper limb after stroke: A pilot randomized controlled trial. Arch Phys Med Rehabil. 95 (11), 2000-2005 (2014).
- Xin, T. Effect of suspension-based digit work therapy system training on upper limb motor function in stroke hemiparesis patients. Chinese Journal of Rehabilitation Theory and Practice. 28, 1259-1264 (2022).
- Mccabe, J., Monkiewicz, M., Holcomb, J., Pundik, S., Daly, J. J. Comparison of robotics, functional electrical stimulation, and motor learning methods for treatment of persistent upper extremity dysfunction after stroke: A randomized controlled trial. Arch Phys Med Rehabil. 96 (6), 981-990 (2015).
- Hung, J. W., et al. Comparison of kinect2scratch game-based training and therapist-based training for the improvement of upper extremity functions of patients with chronic stroke: A randomized controlled single-blinded trial. Eur J Phys Rehabil Med. 55 (5), 542-550 (2019).
- Cho, K. H., Song, W. K. Robot-assisted reach training with an active assistant protocol for long-term upper extremity impairment poststroke: A randomized controlled trial. Arch Phys Med Rehabil. 100 (2), 213-219 (2019).
- Lu, J., et al. Montreal cognitive assessment in detecting cognitive impairment in chinese elderly individuals: A population-based study. J Geriatr Psychiatry Neurol. 24 (4), 184-190 (2011).
- Page, S. J., Hade, E., Persch, A. Psychometrics of the wrist stability and hand mobility subscales of the fugl-meyer assessment in moderately impaired stroke. Phys Ther. 95 (1), 103-108 (2015).
- Ottosson, A. Signe brunnstrom’s influence on us physical therapy. Physical Therapy. 101 (8), (2021).
- Urban, P. P., et al. Occurence and clinical predictors of spasticity after ischemic stroke. Stroke. 41 (9), 2016-2020 (2010).
- Duffy, L., Gajree, S., Langhorne, P., Stott, D. J., Quinn, T. J. Reliability (inter-rater agreement) of the barthel index for assessment of stroke survivors: Systematic review and meta-analysis. Stroke. 44 (2), 462-468 (2013).
- Bao, X., et al. Mechanism of kinect-based virtual reality training for motor functional recovery of upper limbs after subacute stroke. Neural Regen Res. 8 (31), 2904-2913 (2013).
- Henderson, A., Korner-Bitensky, N., Levin, M. Virtual reality in stroke rehabilitation: A systematic review of its effectiveness for upper limb motor recovery. Top Stroke Rehabil. 14 (2), 52-61 (2007).
- Faria, A. L., Andrade, A., Soares, L., Sb, I. B. Benefits of virtual reality based cognitive rehabilitation through simulated activities of daily living: A randomized controlled trial with stroke patients. J Neuroeng Rehabil. 13 (1), 96 (2016).
- Chien, W. T., Chong, Y. Y., Tse, M. K., Chien, C. W., Cheng, H. Y. Robot-assisted therapy for upper-limb rehabilitation in subacute stroke patients: A systematic review and meta-analysis. Brain Behav. 10 (8), e01742 (2020).
- Zhang, L., Jia, G., Ma, J., Wang, S., Cheng, L. Short and long-term effects of robot-assisted therapy on upper limb motor function and activity of daily living in patients post-stroke: A meta-analysis of randomized controlled trials. J Neuroeng Rehabil. 19 (1), 76 (2022).
- Lu, C., Hua, The effects of digital cognitive training in occupational therapy on cognition, upper limb movement, and activities of daily living in stroke patients. Modern Medicine. 47, 373-376 (2019).
- Yun, S. J., et al. Cognitive training using fully immersive, enriched environment virtual reality for patients with mild cognitive impairment and mild dementia: Feasibility and usability study. JMIR Serious Games. 8 (4), 18127 (2020).
- Kim, W. S., et al. Clinical application of virtual reality for upper limb motor rehabilitation in stroke: Review of technologies and clinical evidence. J Clin Med. 9 (10), 3369 (2020).
- Høeg, E. R., et al. System immersion in virtual reality-based rehabilitation of motor function in older adults: A systematic review and meta-analysis. Frontiers in Virtual Reality. 2, 39-56 (2021).
- Bevilacqua, R., et al. Non-immersive virtual reality for rehabilitation of the older people: A systematic review into efficacy and effectiveness. Journal of Clinical Medicine. 8 (11), 1882 (2019).

