A Reference Broth Microdilution Method for Dalbavancin In Vitro Susceptibility Testing of Bacteria that Grow Aerobically
Summary
Here, we present a protocol for determination of dalbavancin susceptibility of clinically relevant Gram-positive bacteria using a broth microdilution reference methodology.
Abstract
Antimicrobial susceptibility testing (AST) is performed to assess the in vitro activity of antimicrobial agents against various bacteria. The AST results, which are expressed as minimum inhibitory concentrations (MICs) are used in research for antimicrobial development and monitoring of resistance development and in the clinical setting for antimicrobial therapy guidance. Dalbavancin is a semi-synthetic lipoglycopeptide antimicrobial agent that was approved in May 2014 by the Food and Drug Administration (FDA) for the treatment of acute bacterial skin and skin structure infections caused by Gram-positive organisms. The advantage of dalbavancin over current anti-staphylococcal therapies is its long half-life, which allows for once-weekly dosing. Dalbavancin has activity against Staphylococcus aureus (including both methicillin-susceptible S. aureus [MSSA] and methicillin-resistant S. aureus [MRSA]), coagulase-negative staphylococci, Streptococcus pneumoniae, Streptococcus anginosus group, β-hemolytic streptococci and vancomycin susceptible enterococci. Similar to other recent lipoglycopeptide agents, optimization of CLSI and ISO broth susceptibility test methods includes the use of dimethyl sulfoxide (DMSO) as a solvent when preparing stock solutions and polysorbate 80 (P80) to alleviate adherence of the agent to plastic. Prior to the clinical studies and during the initial development of dalbavancin, susceptibility studies were not performed with the use of P-80 and MIC results tended to be 2-4 fold higher and similarly higher MIC results were obtained with the agar dilution susceptibility method. Dalbavancin was first included in CLSI broth microdilution methodology tables in 2005 and amended in 2006 to clarify use of DMSO and P-80. The broth microdilution (BMD) procedure shown here is specific to dalbavancin and is in accordance with the CLSI and ISO methods, with step-by-step detail and focus on the critical steps added for clarity.
Introduction
Dalbavancin is a semi-synthetic lipoglycopeptide that was approved by the FDA in May 2014 for the treatment of acute bacterial skin and skin structure infections caused by Gram-positive organisms1. The primary goal of detailing this method in a video format is to provide clear guidance to the clinical laboratory and research scientists for testing and reporting of accurate and reproducible dalbavancin susceptibility results.
The determination of an antimicrobial agent MIC by commercial methods is routinely performed in clinical laboratories for assessment of an agent’s in vitro activity against pathogenic bacteria. The method described here is the broth microdilution method as recommended by CLSI and ISO 2,3,4. Since dalbavancin commercial susceptibility methods are not currently available (at the time of this publication) and disk diffusion and agar dilution methods are not currently recommended for dalbavancin, reference broth dilution methods are the current options available 12,14. As this reference method is not a commercial and FDA cleared in vitro diagnostic method, clinical laboratories in the USA that use this procedure for patient testing must abide by regulatory requirements for a laboratory developed test (LDT). It is anticipated that as the dalbavancin use increases, more laboratories will have a need to test this compound. Vancomycin testing as a surrogate for determination of dalbavancin susceptibility of S. aureus has been validated5. However, dalbavancin may be active against vancomycin intermediate S. aureus (VISA) and therefore, clinicians may request dalbavancin MIC results. In addition, MIC results for other bacterial species may be requested.
The FDA susceptible breakpoint for dalbavancin against S. aureus has been established at ≤0.12 µg/ml. FDA assigned only a susceptible category because of the lack of data on resistant isolates. The normal MIC distribution among wild type S. aureus isolates is between 0.03-0.12 µg/ml, with a clear modal MIC of 0.06 µg/ml. A slight variation in MIC results due to method difference, in addition to the inherent BMD variation of ± one dilution, could potentially have a significant impact on the susceptibility rates.6 Similar to other lipoglycopeptide agents, dalbavancin susceptibility testing can be challenging as a result of solubility and the relatively large size of the molecule and its binding properties7,8,9. The reference BMD method described here includes two specific steps that are unique to insoluble agents and/or lipoglycopeptide agents: (1) the use of DMSO for preparation of stock solutions and (2) addition of 0.002% P-80 in the final MIC panel dilutions. The objective of this video publication is to provide clarity to the dalbavancin BMD method and to specifically focus on these key steps, to assure accurate and reproducible MIC results.
Protocol
Note: Refer to CLSI documents M7-A10 and M100-S25 and/or ISO/FDIS 20776-1 for full details of the reference broth microdilution method for antimicrobial susceptibility2, 3, 4. The reference methods allow for options in some of the procedures specific to inoculum preparation and MIC panel production to achieve the same end result. The method detailed here relates to one antimicrobial agent, dalbavancin, and some of the steps represent one of potentially several ways the reference procedure can be done. Appropriate safety precautions (consistent with biosafety level 2) should be utilized10. The MIC panel format used for the purpose of this video publication is shown in Table 1.
1. Store Dalbavancin Powder
- Upon receipt of diagnostic grade dalbavancin powder, store at -20 oC in a desiccated environment in a non-defrosting freezer. Prior to use, the powder should equilibrate to reach RT before opening.
2. Prepare MIC Panel Dilutions
- Prepare a stock solution no higher than 1,600 µg/ml of dalbavancin in neat (pure) DMSO in sterile glass or plastic tubes, and use on the same day of preparation or store at -20 to -60 oC or below for future use in a non-defrosting freezer. Take into consideration the potency of dalbavancin as provided on the documentation received with the powder, when weighing the powder (see Equation 1 for example 800 µg/ml stock preparation).
- Dilute the stock dilution similar to the scheme as is shown in column 1 (“Source Concentration”) in Table 2 with neat DMSO in sterile glass or plastic tubes. Use one pipet for measuring diluent and another pipet for adding the initial dalbavancin stock to the first tube. For each subsequent dalbavancin stock concentration use a new pipet.
- Prepare 100X final MIC panel concentration dilutions (intermediate concentrations) with neat DMSO. As is shown in columns 2-4 of Table 2, combine appropriate volumes of source and DMSO to achieve desired intermediate concentration (volumes to be used will depend on number of MIC panels to be made).
- Prepare 0.004% P80: Prepare a fresh working stock solution of 2% P80 by adding 0.1 ml P80 to 4.9 ml dH2O. Sterilize by passing through a 0.22 micron filter and use solution on the same day of preparation. Prepare 0.004% P80 diluent by making a 1:500 dilution of 2% P80 (e.g., 0.3 ml of 2% P80 to 149.7 ml of CAMHB).
- Further dilute the intermediate concentrations prepared in Step 2.2 1:100 in cation adjusted Mueller Hinton broth (CAMHB) supplemented with 0.004% (v/v) polysorbate-80 (P-80) P-80 and/or LHB (for streptococci) added at double the final concentration because addition of inoculum (step 4.3) will result in a 1:2 dilution. See columns 6 and 7 in Table 2.
3. Prepare MIC Panels
- Dispense 50 µl of each dalbavancin solution prepared in step 2.3 into appropriate wells of the MIC panel and include media only in one well (growth control well). A multi-channel pipet with sterile tips can be used for this step.
- Use panels immediately or seal with plastic film, place in plastic bags and immediately place in a non-defrosting freezer at ≤-20 oC (preferably at ≤-60 oC) until needed. If frozen panels are used, remove seals and place individual panels on lab bench for 15-30 min (until well contents are thawed) before proceeding to panel inoculation.
4. Inoculate MIC Panels, Perform Purity and Setup Colony Count
- Select several well-isolated colonies from an 18-24 hr blood agar or other non-selective agar plate. Touch the top of each colony with a sterile loop or swab and transfer to 1-5 ml CAMHB or saline until turbidity is equivalent to a 0.5 McFarland standard. Assess turbidity by visual comparison to the 0.5 McFarland or with a photometric device.
- Within 15-30 min of preparation, dilute the inoculum 1:100 in CAMHB (100 µl into 10 ml CAMHB). For most bacteria tested against dalbavancin, with the exception of S. pneumoniae, this dilution will provide a final well concentration of 5 x 105 CFU/ml (acceptable range is 2-8 x 105 CFU/ml). For S. pneumoniae, bacterial concentration based on comparison of turbidity to a 0.5 McFarland is typically considerably less, therefore, dilute the inoculum 1:25 (400 µl into 10 ml CAMHB+10% +LHB).
- Within 15 min after inoculum preparation, transfer 50 µl of the final inoculum to each well (with exception of the sterility control well) of the MIC panel prepared in step 3. A multi-channel pipet using sterile tips can be used for this step.
- Perform a purity check by transferring and spreading a 1-10 µl aliquot from the positive growth control well using a sterile loop to a nonselective agar (e.g., trypticase soy agar with 5% sheep blood).
- Setup colony count by removing 10 µl from the growth control well with a single channel pipet and sterile tip and transfer to 10 ml of saline (1:1,000 dilution). Mix and transfer 100 µl with a single channel pipet and sterile tip to a suitable, nonselective agar medium (e.g., trypticase soy agar with 5% sheep blood) and spread over the entire agar surface with a sterile loop, repeating two times in different directions to assure even distribution of the inoculum (1:10 dilution).
5. Incubate MIC Panels, Colony Count and Purity Plates
- Seal each MIC panel or stack of no more than 4 panels in a plastic bag, with plastic tape or with a tight-fitting plastic cover before incubating. Alternatively, place empty MIC panel on the top of stack of no more than 4 MIC panels, place a damp paper towel in a plastic container, place MIC panels in the plastic container and close container securely with lid.
- Incubate MIC panels in an ambient air incubator at 35 °C ± 2 °C for 16-20 hr (staphylococci and enterococci) and 20-24 hr (streptococci) within 30 min of inoculation. Incubate the colony count and purity plates under same conditions except incubate streptococci in a 5% CO2 incubator.
6. Read the MIC and Colony Count Plates; Check Purity Plate
- Read the MIC as the lowest concentration that completely inhibits bacterial growth in the wells as detected by the unaided eye.
- Count colonies on the colony count plate. Multiply each colony by dilution factor (1:10,000) (e.g., 50 colonies is equivalent to 5 x 105 CFU/ml). An acceptable range is 20-80 colonies (2-8 x 105 CFU/ml) and is used as an approximate guideline.
- Check purity plate. If all colonies are similar to the colonies used in step 4.1, then the inoculum can be considered pure. If there are any other colonies present, then there is potential for a contaminant to be present in the MIC panel and the test should be repeated.
7. Check Quality Control Results.
- Refer to Table 3 for expected ranges of CLSI quality control strains. Only report results of test isolates if dalbavancin MIC results for quality control organism(s) are within the expected range.
- If an MIC of ≥0.25 µg/ml is obtained for any clinical S. aureus isolate, repeat the dalbavancin MIC testing and/or send to a reference laboratory for verification.
Representative Results
Standardized MIC methods are necessary in order to monitor resistance development, an important goal of various antimicrobial surveillance programs. Dalbavancin MIC results for isolates collected in Europe and USA in 2011-2013 were <0.25 µg/ml for 99.9% of S.aureus and 100% of streptococci (Table 4).
To assess the importance of using fresh (sealed) DMSO, triplicate testing of dalbavancin BMD MICs for QC strains S. aureus ATCC 29213, and E. faecalis ATCC 29212 and duplicate testing for S. pneumoniae ATCC 49619 was performed using (1) DMSO from sealed ampules, (2) DMSO from a 1 L bottle that was within the expiration date and had been used previously for 2 years and (3) an aliquot of DMSO from the same 1 L bottle (sample 2) that was allowed to sit in an open beaker for 72 hr prior to use. Dalbavancin MIC results using panels made with all three DMSO samples were similar and within the acceptable QC ranges (Table 5).
The loss of dalbavancin activity following exposure of the stock solution to plastic and without the addition of P-80 has been well documented7. In 2 additional studies, the addition of P-80 to the initial and intermediate stock solutions (Table 6) and the use of glass or plastic tubes for the preparation of the initial and intermediate stock solutions (Table 7) did not have an effect on the dalbavancin MIC results. There was also no effect on dalbavancin MIC results when polypropylene and polystyrene plates from three manufacturers were used (Table 7).
The presence of lysed horse blood in the broth media for testing of streptococci has been shown to have a surfactant-like activity, comparable to P-807, 8. The dalbavancin reference method for streptococcus does include both P-80 and lysed horse blood, however, unlike staphylococci and enterococci, dalbavancin MIC results for streptococci are similar (within +/- 1 dilution) with and without the addition of P-80.
As has been previously presented and shown in Figure 1, dalbavancin agar dilution (AD) MICs are typically 2-8 fold higher compared to the current BMD reference12, 13, 14. Unlike BMD, the addition of 0.002% P-80 does not affect dalbavancin AD MIC results12.
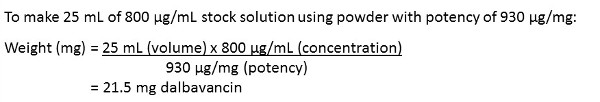
Equation 1: Example of Dalbavancin Stock Solution Preparation. Preparation steps for 25 ml of 800 µg/ml dalbavancin solution.
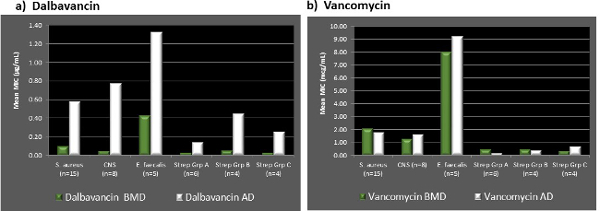
Figure 1. Comparison of Dalbavancin and Vancomycin BMD to AD. Results of study that compared dalbavancin and vancomycin BMD and AD MIC results for select Gram-positive bacterial isolates. Average (A) Dalbavancin and (B) Vancomycin Broth Microdilution and Agar Dilution MIC Results in µg/ml for 15 Staphylococcus aureus, 8 Coagulase Negative Staphylococci (CNS), 5 Enterococcus faecalis and 14 Streptococci (Groups A, B, and C). Please click here to view a larger version of this figure.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
| A | DAL 0.002 | DAL 0.004 | DAL 0.008 | DAL 0.015 | Dal 0.03 | DAL 0.06 | DAL 0.12 | DAL 0.25 | DAL 0.5 | DAL 1 | DAL 2 | Pos Ctrl. |
| B | DAL 0.002 | DAL 0.004 | DAL 0.008 | DAL 0.015 | Dal 0.03 | DAL 0.06 | DAL 0.12 | DAL 0.25 | DAL 0.5 | DAL 1 | DAL 2 | Pos Ctrl. |
| C | DAL 0.002 | DAL 0.004 | DAL 0.008 | DAL 0.015 | Dal 0.03 | DAL 0.06 | DAL 0.12 | DAL 0.25 | DAL 0.5 | DAL 1 | DAL 2 | Pos Ctrl. |
| D | DAL 0.002 | DAL 0.004 | DAL 0.008 | DAL 0.015 | Dal 0.03 | DAL 0.06 | DAL 0.12 | DAL 0.25 | DAL 0.5 | DAL 1 | DAL 2 | Pos Ctrl. |
| E | DAL 0.002 | DAL 0.004 | DAL 0.008 | DAL 0.015 | Dal 0.03 | DAL 0.06 | DAL 0.12 | DAL 0.25 | DAL 0.5 | DAL 1 | DAL 2 | Pos Ctrl. |
| F | DAL 0.002 | DAL 0.004 | DAL 0.008 | DAL 0.015 | Dal 0.03 | DAL 0.06 | DAL 0.12 | DAL 0.25 | DAL 0.5 | DAL 1 | DAL 2 | Pos Ctrl. |
| G | DAL 0.002 | DAL 0.004 | DAL 0.008 | DAL 0.015 | Dal 0.03 | DAL 0.06 | DAL 0.12 | DAL 0.25 | DAL 0.5 | DAL 1 | DAL 2 | Pos Ctrl. |
| H | DAL 0.002 | DAL 0.004 | DAL 0.008 | DAL 0.015 | Dal 0.03 | DAL 0.06 | DAL 0.12 | DAL 0.25 | DAL 0.5 | DAL 1 | DAL 2 | Pos Ctrl. |
| DAL | Dalbavancin | |||||||||||
| Concentrations are stated in µg/ml after 50 µl/well inoculation | ||||||||||||
Table 1. MIC Plate Format. The 96 well plate format showing location of dalbavancin dilutions and positive control wells used as an example in this video publication
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
| Source Conc. (µg/ml) | Volume Source (ml) | Volume DMSO (ml) | Intermediate Conc. in DMSO (µg/ml) | Volume Intermediate Conc. (ml) | Volume CAMHB + 0.004% P80* (ml) | 2X Conc. After 1:100 Dilution in CAMHB (µg/ml) | Final Panel Conc. Post Inoculation (µg/ml) |
| 800 | 1.0 | 1.0 | 400 | 0.02 | 1.98 | 4 | 2 |
| 400 | 0.5 | 0.5 | 200 | 0.02 | 1.98 | 2 | 1 |
| 400 | 0.5 | 1.5 | 100 | 0.02 | 1.98 | 1 | 0.5 |
| 400 | 0.5 | 3.5 | 50 | 0.02 | 1.98 | 0.5 | 0.25 |
| 50 | 0.5 | 0.5 | 25 | 0.02 | 1.98 | 0.25 | 0.125 |
| 50 | 0.5 | 1.5 | 12.5 | 0.02 | 1.98 | 0.125 | 0.06 |
| 50 | 0.5 | 3.5 | 6.25 | 0.02 | 1.98 | 0.06 | 0.03 |
| 6.25 | 0.5 | 0.5 | 3.13 | 0.02 | 1.98 | 0.03 | 0.015 |
| 6.25 | 0.5 | 1.5 | 1.5 | 0.02 | 1.98 | 0.015 | 0.008 |
| 6.25 | 0.5 | 3.5 | 0.8 | 0.02 | 1.98 | 0.008 | 0.004 |
| 0.8 | 0.5 | 0.5 | 0.4 | 0.02 | 1.98 | 0.004 | 0.002 |
| This table has been modified from CLSI M100-S25, Table 8B3 | |||||||
Table 2. Scheme for Preparing Dilutions of Water-Insoluble Antimicrobial Agents to be Used in Broth Dilutions Susceptibility Testing. Volumes of dalbavancin working solutions and diluents for preparation of final MIC dalbavancin solutions of 0.002-2 µg/ml.
| Quality Control Strain | Expected Dalbavancin MIC (µg/ml) |
| S. aureus ATCC 29213 | 0.03-0.12 |
| E. faecalis ATCC 29212 | 0.03-0.12 |
| S. pneumoniae ATCC 49619 | 0.008-0.03 |
Table 3. Expected Dalbavancin MIC Results for Quality Control Strains3, 11. CLSI quality control results for suggested strains to be tested along with clinical isolates in order to verify proper methodology
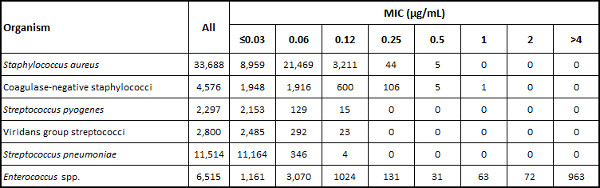
Table 4. Distribution of Dalbavancin MIC Results (Number at each MIC) from USA and European 2011-2013 Surveillance Study15. Dalbavancin MIC results from a published study of recent clinical isolates as an indicator of current dalbavancin in vitro activity.
| Isolate # | Dalbavancin MIC (µg/ml) | ||
| DMSO 1 | DMSO 2 | DMSO 3 | |
| S. aureus ATCC 29213 | 0.12 | 0.06 | 0.06 |
| 0.12 | 0.06 | 0.06 | |
| 0.06 | 0.06 | 0.06 | |
| E. faecalis ATCC 29212 | 0.06 | 0.06 | 0.06 |
| 0.06 | 0.06 | 0.06 | |
| 0.06 | 0.06 | 0.06 | |
| S. pneumoniae ATCC 49619 | 0.015 | 0.015 | 0.015 |
| 0.03 | 0.015 | 0.015 | |
| DMSO 1 = Unopened flame sealed 10 ml ampules | |||
| DMSO 2 = Frequently opened 1L bottle | |||
| DMSO 3 = Frequently opened 1L bottle – sat on bench in uncovered beaker for 72 hr | |||
Table 5. Dalbavancin MIC Results (µg/ml) using DMSO Stock and Intermediate Dilutions Preparation with DMSO from 3 Sources. Results of a dalbavancin MIC study that compared effect of using different DMSO solvents in preparation of the dalbavancin stock and intermediate dilutions.
| Isolate Number | Replicate Number | Dalbavancin MIC (µg/ml) | |
| DALB w/P80 in DMSO | DALB w/o P80 in DMSO | ||
| S. aureus ATCC 29213 | 1 | 0.06 | 0.06 |
| 2 | 0.06 | 0.06 | |
| 3 | 0.06 | 0.06 | |
| 4 | 0.06 | 0.06 | |
| S. aureus clinical DP80-002SA | 1 | 0.03 | 0.03 |
| S. aureus ATCC 700699 | 1 | 0.5 | 0.5 |
| S. pneumoniae ATCC 49619 | 1 | 0.03 | 0.015 |
| 2 | 0.03 | 0.015 | |
| 3 | 0.03 | 0.015 | |
| 4 | 0.03 | 0.015 | |
| S. pyogenes clinical: | |||
| DP80-004PY | 1 | 0.015 | 0.015 |
| DP80-005PY | 1 | 0.03 | 0.03 |
| DP80-006PY | 1 | 0.03 | 0.015 |
| DP80-007PY | 1 | 0.06 | 0.03 |
| DP80-008PY | 1 | 0.03 | 0.015 |
| S. agalactiae clinical: | |||
| DP80-009AG | 1 | 0.06 | 0.12 |
| DP80-010AG | 1 | 0.06 | 0.03 |
| DP80-011AG | 1 | 0.06 | 0.06 |
| DP80-012AG | 1 | 0.06 | 0.06 |
| S. dysgalactiae clinical DP80-013DY | 1 | 0.03 | 0.03 |
| S. pneumoniae clinical: | |||
| DP80-014SP | 1 | 0.06 | 0.06 |
| DP80-015SP | 1 | 0.03 | 0.03 |
| DP80-016SP | 1 | 0.03 | 0.03 |
| DP80-017SP | 1 | 0.06 | 0.06 |
Table 6. Dalbavancin MIC Results using DMSO Stock and Intermediate Dilutions Preparation with and without 0.002% P-80. Results of a dalbavancin MIC study that compared effect of adding 0.002% P-80 to dalbavancin stock and intermediate dilutions.
| Isolate | Replicate Number | Stock Dilution Tubes | Microtiter Plate (Plastic Type) | ||||||
| Poly-propylene, Greiner | Polystyrene | ||||||||
| Glass | Plastic | Plastic 1hr | Plastic 1hr / Intermediate 1hr | Greiner | Corning | Nunc | |||
| S. aureus ATCC 29213 | 1 | 0.06 | 0.03 | 0.03 | 0.03 | 0.06 | 0.03 | 0.06 | 0.03 |
| 2 | 0.03 | 0.03 | 0.03 | 0.03 | 0.03 | 0.03 | 0.03 | 0.06 | |
| 3 | 0.03 | 0.03 | 0.03 | 0.03 | 0.03 | 0.03 | 0.03 | 0.03 | |
| E. faecalis ATCC 29212 | 1 | 0.06 | 0.06 | 0.06 | 0.06 | 0.03 | 0.03 | 0.06 | 0.03 |
| 2 | 0.06 | 0.06 | 0.06 | 0.06 | 0.03 | 0.03 | 0.06 | 0.03 | |
| 3 | 0.06 | 0.06 | 0.06 | 0.06 | 0.03 | 0.03 | 0.06 | 0.03 | |
| S. pneumoniae ATCC 49619 | 1 | 0.015 | 0.015 | 0.015 | 0.015 | 0.008 | 0.008 | 0.008 | 0.008 |
| 2 | 0.015 | 0.015 | 0.015 | 0.015 | 0.008 | 0.015 | 0.008 | 0.008 | |
| Glass = Initial stock made in glass bottle, used immediately to make intermediate concentrations in plastic tubes, used immediately to make broth dilutions. | |||||||||
| Plastic = Initial stock made in plastic centrifuge tube, used immediately to make intermediate concentrations in plastic tubes, used immediately to make broth dilutions. | |||||||||
| Plastic 1 hr = Initial stock made in plastic centrifuge tube, let sit on bench for 1 hr then used to make intermediate concentrations in plastic tubes, used immediately to make concentrations in broth. | |||||||||
| Plastic 1 hr / Intermediate 1 hr = Initial stock made in plastic centrifuge tube, let sit on bench for 1 hr then used to make intermediate concentrations in plastic tubes, let sit on bench for 1 hr then used to make concentrations in broth. | |||||||||
Table 7. Dalbavancin MIC Results using Stock Dilutions Preparation in Plastic and Glass Tubes and MIC Plate Plastic Types. Results of a dalbavancin MIC study that compared effect of using plastic or glass tubes when preparing the stock solutions and also effect of using different sources and types of plastic for microtiter plates.
Discussion
The following method details are presented for additional considerations when preparing for dalbavancin MIC testing. The design of the MIC panel will depend on the number of antimicrobial agents to be tested (i.e., dalbavancin alone or multiple agents) and the species of bacteria to be tested. The dalbavancin concentrations should encompass the interpretive breakpoints for all bacterial species to be tested and the entire range of dilutions expected for at least one QC strain. The antimicrobial dilution series can be organized either in rows or columns depending on the number of antimicrobial agents and/or isolates/plate and method of inoculation. The volume of dalbavancin powder and broth should be calculated to assure that optimal amounts are produced and waste is minimal. For the example used in this publication, volumes are based on preparation of two MIC panels. Cation adjusted Mueller Hinton broth should be prepared and autoclaved according to manufacturer’s instructions and sterility of the media verified. MIC panels can be made and used on same day of preparation or they can be tested with appropriate quality control organisms and the validated panels stored frozen for future use. It is important to use sterile techniques throughout the procedure.
There is no strict criteria for verification of inoculum concentration with colony counts. Colony counts may be checked initially for each species tested and/or periodically to validate the dilution step performed in step 4.2. It is important that the validity of the 0.5 McFarland standard is also checked routinely with E. coli ATCC 25922 using a procedure similar to step 4.5. If results are not equivalent to 1-2 x 108 CFU/ml, a new 0.5 McFarland standard should be obtained. If the colony counts from MIC wells are outside of the acceptable range (2-8 x 105 CFU/ml and MIC results for the clinical isolate(s) vary from the expected normal distribution (eg. 0.03-0.12 ug/ml for S. aureus) and/or MIC results for quality control isolate(s) are outside of expected ranges, validation testing is necessary and method modification may be warranted. It is suggested that a validated 0.5 McFarland standard is used to repeat the colony count(s) and if results are again outside of expected results, the inoculum dilution as performed in step 4.2 should be adjusted accordingly and the MIC repeated. Note that a purity check is necessary even if a colony count is performed because the colony count procedure uses a diluted volume that may not necessarily detect lower concentrations of contaminating organisms.
For a MIC test to be considered valid, acceptable growth must occur in the growth control well. For most bacteria that will be tested against dalbavancin (i.e., staphylococci, streptococci and enterococci, growth will be seen as a button (typically >2 mm) and less frequently, growth may appear as turbidity in the well. Unlike some antimicrobial agents that may exhibit trailing effect as concentrations increase, dalbavancin endpoints are typically well defined. There are various viewing devices intended to facilitate reading microdilution tests, which may be used to read dalbavancin containing plates as long as there is no compromise in the ability to discern growth in the wells.
The critical steps within the protocol are related to the parts of the procedure that are related to the solubility of dalbavancin and addition of P80. It is important that the maximum concentration of dalbavancin used is no greater than 1,600 µg/ml, that DMSO is used as a solvent and that intermediate concentrations are prepared in DMSO prior to making the broth dilutions so that the final concentration of DMSO in the MIC panel wells is no greater than 1%. DMSO is hygroscopic and therefore, the use of older bottles of DMSO was a consideration with regard to dalbavancin solubility. However, while a small BMD study with quality control strains has shown this not to be an important variable (see results section), it is good practice to use new or recently opened bottles of DMSO. It is also important that P80 is added to the broth in the final step of drug dilution preparation and is at a final concentration of 0.002% in the MIC well.
The BMD procedure included here utilizes preparation of MIC panels using 50 µl/well at dalbavancin and P-80 concentrations two times the final concentration and addition of inoculum with 50 µl/well so that final volume/well is 100 µl. This method allows for one MIC panel format to be produced for the testing of both S. aureus and S. pneumoniae because the lysed horse blood can be added to the inoculum. Alternative methods for preparation of MIC panels using 100 µl/well with addition of up to 10 µl/well are described in the CLSI and ISO procedures.
The dalbavancin susceptible breakpoint for S. aureus is ≤0.12 µg/ml (FDA package insert). As is shown in recent surveillance, the majority of isolates are inhibited by dalbavancin at levels of 0.06 µg/ml15. With a susceptible breakpoint close to the modal MIC, any variation in MIC as a result of method differences can affect susceptibility rates. Because the BMD procedure for dalbavancin includes some unique steps (specifically, the use of DMSO in preparation of stock and intermediate drug dilutions and 0.002% P80 in the MIC well, it is imperative that the method is followed exactly. The S. aureus QC organism (ATCC 29213) with a very clear dalbavancin modal MIC of 0.06 µg/ml, has been a good indicator of method variation and should be used routinely to validate the BMD method. If MIC results are with the expected range of 0.03-0.12 µg/ml, but are trending to either the low or high side of this range, further validation of the method is warranted.
The addition of 0.002% P80 is recommended for all relevant Gram-positive organisms (staphylococcci, enterococci, and streptococci.) However, it is noteworthy that it has been shown that lysed horse blood acts similar to P-80 relative to its anti-binding capability and that the addition of P-80 to CAMHB+LHB has no additional effect on dalbavancin streptococci MIC results.
There is currently no disk diffusion method for testing dalbavancin and because of the poor correlation of BMD and AD results, susceptibility testing of dalbavancin using the AD method is not recommended12, 14. The BMD method should be used for the future assessment of dalbavancin susceptibility and as a gold standard for the development of commercial antimicrobial susceptibility tests.
Divulgazioni
The authors have nothing to disclose.
Acknowledgements
Prior work with regard to susceptibility testing of dalbavancin has been valuable in development of a standardized methods and acknowledgement for this work is given to JMI Laboratories, Robert Rennie and Beth Goldstein.
Materials
| Dalbavancin | Metrics, Inc. | Greenville, NC | BI-397 |
| Vancomycin | Sigma-Aldrich | St. Louis, MO | C5793 |
| Cation Adjusted Mueller Hinton Broth | Becton Dickinson | Sparks, MD | 212322 |
| Lysed horse blood | Cleveland Scientific | Bath, OH | |
| Dose-it peristaltic pump | Integra Biosciences | Hudson, NH | |
| Multi-channel pipet (Viaflo II) | Integra | Hudson, NH | 4164 |
| 12 channel pipet (Matrix) | ThermoFisher Scientific | Waltham, MA | |
| Single channelpPipets (Ovation 10 µL – 100 µL) | VistaLab | Brewster, NY | |
| 96 well microplate | Greiner Bio-one | Monroe, NC | 650161 |
| 50 mL flat cap conical bottom centrifuge tubes | ThermoFisher Scientific | Waltham, MA | |
| 16x125mm disposable glass tubes | ThermoFisher Scientific | Waltham, MA | |
| 12x17mm snap cap, polystyrene tubes | ThermoFisher Scientific | Waltham, MA | |
| 16 mL centrifuge tubes | BioExpress | Kaysville, UT | C-3394-2 |
| Reagent reservoirs | Integra Biosciences | Hudson, NH | 4312 |
| Disposable sterilelLoops (1 uL & 10 uL) | Biologix | Lenexa, KA | 65-0001,65-0010 |
| Tryptic soy agar + 5% sheep blood | Becton Dickinson | Sparks, MD | |
| Incubator (ambient) | Sanyo | ||
| Incubator (5% CO2) | Sanyo | ||
| Analytical balance | ThermoFisher Scientific | Waltham, MA | |
| Gloves | Kimberly-Clark | 52817 | |
| Lab coats |
Riferimenti
- Boucher, H. W., et al. Once-weekly dalbavancin versus daily conventional therapy for skin infection. The New England journal of medicine. 370, 2169-2179 (2014).
- . . M07-A10. Methods for Dilution Antimicrobial Tests for Bacteria that Grow Aerobically.: Approved Standard. , (2015).
- . . M100-S25. Performance Standards for Antimicrobial Susceptibility Testing; Twenty-Fifth Informational Supplement. , (2015).
- . Clinical laboratory testing and in vitro diagnostic test systems — Susceptibility testing of infectious agents and evaluation of performance of antimicrobial susceptibility test devices — Part 1: Reference method for testing the in vitro activity of antimicrobial agents against rapidly growing aerobic bacteria involved in infectious diseases. ISO/FDIS. 20776-1, (2006).
- Jones, R. N., Farrell, D. J., Flamm, R. K., Sader, H. S., Dunne, M. W., Mendes, R. E. Surrogate analysis of vancomycin to predict susceptible categorization of dalbavancin. Diagn Microbiol Infect Dis. , (2015).
- Turnidge, J., Paterson, D. L. Setting and revising antibacterial susceptibility breakpoints. Clinical microbiology reviews. 20, 391-408 (2007).
- Rennie, R. P., et al. Factors influencing broth microdilution antimicrobial susceptibility test results for dalbavancin, a new glycopeptide agent. Journal of clinical microbiology. 45, 3151-3154 (2007).
- Arhin, F. F., et al. Effect of polysorbate 80 on oritavancin binding to plastic surfaces: implications for susceptibility testing. Antimicrobial agents and chemotherapy. 52, 1597-1603 (2008).
- Farrell, D. J., Mendes, R. E., Rhomberg, P. R., Jones, R. N. Revised reference broth microdilution method for testing telavancin: effect on MIC results and correlation with other testing methodologies. Antimicrobial agents and chemotherapy. 58, 5547-5551 (2014).
- Ribbon Panel, B. l. u. e. Guidelines for Safe Work Practices in Human and Animal Medical Diagnostic Laboratories. MMWR Supplements. 61 (01), 1-101 (2012).
- Anderegg, T. R., Biedenbach, D. J., Jones, R. N. Initial quality control evaluations for susceptibility testing of Dalbavancin (BI397), an investigational glycopeptide with potent gram-positive activity. Journal of clinical microbiology. 41, 2795-2796 (2003).
- Koeth, L. M., Windau, A. R., Goldstein, B. P. Comparison of Broth Microdilution and Agar Dilution Dalbavancin and Vancomycin MIC Results for 42 Aerobic Gram-positive Bacteria. Poster 132. ASM. , (2012).
- Fritsche, T. R., Rennie, R. P., Goldstein, B. P., Jones, R. N. Comparison of dalbavancin MIC values determined by Etest (AB BIODISK) and reference dilution methods using gram-positive organisms. Journal of clinical microbiology. 44, 2988-2990 (2006).
- Mushtaq, S., Warner, M., Johnson, A. P., Livermore, D. M. Activity of dalbavancin against staphylococci and streptococci, assessed by BSAC and NCCLS agar dilution methods. The Journal of antimicrobial chemotherapy. 54, 617-620 (2004).
- Jones, R. N., Flamm, R. K., Sader, H. S. Surveillance of dalbavancin potency and spectrum in the United States (2012). Diagnostic microbiology and infectious disease. 76, 122-123 (2013).

