Transcranial Direct Current Stimulation (tDCS) in Mice
Summary
Transcranial direct current stimulation (tDCS) is a therapeutic technique proposed to treat psychiatric diseases. An animal model is essential for understanding the specific biological alterations evoked by tDCS. This protocol describes a tDCS mouse model that uses a chronically implanted electrode.
Abstract
Transcranial direct current stimulation (tDCS) is a non-invasive neuromodulation technique proposed as an alternative or complementary treatment for several neuropsychiatric diseases. The biological effects of tDCS are not fully understood, which is in part explained due to the difficulty in obtaining human brain tissue. This protocol describes a tDCS mouse model that uses a chronically implanted electrode allowing the study of the long-lasting biological effects of tDCS. In this experimental model, tDCS changes the cortical gene expression and offers a prominent contribution to the understanding of the rationale for its therapeutic use.
Introduction
Transcranial Direct Current Stimulation (tDCS) is a non-invasive, low-cost, therapeutic technique, which focuses on neuronal modulation through the use of low-intensity continuous currents1. There are currently two setups (anodal and cathodal) for tDCS. While the anodal stimulation exerts a current electric field too weak to trigger action potentials, electrophysiology studies have shown that this method produces changes in synaptic plasticity2. For example, evidence shows that tDCS induces long-term potentiation (LTP) effects such as increased peak amplitude of the excitatory postsynaptic potentials3,4 and modulation of cortical excitability5.
Conversely, cathodal stimulation induces inhibition, resulting in membrane hyperpolarization6. A hypothesis for this mechanism is based on the physiological findings where tDCS is described to modulate action potential frequency and duration in the neuronal body3. Notably, this effect does not directly evoke action potentials, though it can shift the depolarization threshold and facilitate or hamper neuronal firing7. These contrasting effects have been previously demonstrated. For example, anodal and cathodal stimulation produced opposing effects in conditioned responses registered via electromyography activity in rabbits8. However, studies have also shown that prolonged anodal stimulation sessions may decrease excitability while increasing cathodal currents may lead to excitability, presenting self-contrasting effects3.
Both anodal and cathodal stimuli aggregate the use of electrode pairs. For example, in anodal stimulation, the "active" or "anode" electrode is placed over the brain region to be modulated whereas the "reference" or "cathode" electrode is situated over a region where the effect of current is assumed to be insignificant9. In the cathodal stimulation, electrode disposition is inverted. The stimulation intensity for effective tDCS depends on the current intensity and electrode dimensions, which affect the electric field differently10. In most published studies, the average current intensity is between 0.10 to 2.0 mA and 0.1 mA to 0.8 mA for human and mice, respectively6,11. Although the electrode size of 35 cm2 is typically used in humans, there is no proper understanding regarding electrode dimensions for rodents and a more thorough investigation is needed6.
tDCS has been proposed in clinical studies with the attempt of offering an alternative or complementary treatment for several neurological and neuropsychiatric disorders11 such as epilepsy12, bipolar disorder13, stroke5, major depression14, Alzheimer's disease15, multiple sclerosis16 and Parkinson's disease17. Despite growing interest in tDCS and its use in clinical trials, detailed cellular and molecular evoked alterations in brain tissue, short and long-lasting effects, as well as behavioral outcomes, are yet to be more deeply investigated18,19. Since a direct human approach to thoroughly study tDCS is not viable, the use of a tDCS animal model may offer valuable insights into the cellular and molecular events underlying the therapeutic mechanisms of tDCS due to the accessibility to the animal's brain tissue.
Available evidence is limited regarding tDCS models in mice. Most of the reported models used different implanting layouts, electrode dimensions, and materials. For example, Winkler et al. (2017) implanted the head electrode (Ag/AgCl, 4 mm in diameter) filled with saline and fixed it to the cranium with acrylic cement and screws20. Different from our approach, their chest electrode was implanted (platinum, 20 x 1.5 mm). Nasehi et al. (2017) used a procedure very similar to ours, although the thoracic electrode was made from a saline-soaked sponge (carbon filled, 9.5 cm2)21. Another study implanted both electrodes into the animal's head, which was achieved by using fixed plates and covering the animal's head with a hydrogel conductor22. Here, we describe a tDCS mouse model that uses a chronically implanted electrode through simple surgical procedures and tDCS setup (Figure 1).
Protocol
Individually-housed male adult (8-12 weeks) C57BL/6 mice were used in this experiment. Animals received proper care before, during and after experimental procedures with food and water ad libitum. All procedures were approved by the animal ethics committee from Federal University of Minas Gerais (protocol number 59/2014).
1. Electrode Placement
- Sedating and fixating the animal onto the stereotaxic apparatus
- Sterilize all the necessary surgical instruments.
Note. Surgical instruments were sterilized for 3 minutes at 440 °C. Cotton swabs were autoclaved at 20 psi (pounds per square inch) at 121 °C for 20 min. - Adjust the thermal platform controller to 37 °C.
- Weigh the animal and calculate the appropriate dose for anesthesia induction. Use a mixture of ketamine and xylazine at a dose of 100 mg/kg ketamine and 8 mg/kg xylazine, given intraperitoneally (needle size, 31 G). The animal should fall asleep within 2 to 3 min.
- Use an electric shaver or razor to shave down the surgical site.
- Place the animal onto the stereotaxic apparatus over the pre-warmed heating plate.
- Hold the animal's head and insert the tip ear bars into each of the animal's ears to fix it to the stereotaxic platform.
- Verify there is no lateral head shifting and little vertical movement after by slowly shifting the animal's head positioning.
- Gently slide the anesthesia mask over the mouse's nose and fix it in place by tightening the screw.
- Set the isoflurane to 1% with 1.0 L/min of O2.
- Apply eye ointment to the animal's eyes to prevent corneal drying during the surgery.
- Sterilize all the necessary surgical instruments.
- Attaching the implant to the animal's head
- Use the cotton swabs to prepare the surgical site with three alternating scrubs of povidone-iodine (or 2% chlorhexidine) and 70% ethanol.
- Use a pair of tweezers to verify anesthesia depth by lightly squeezing the animal's toes and verifying the loss of animal's pedal withdrawal (toe pinch) reflex.
- Make an incision about 3 mm posterior to the animal's ear line and stop at the eye line. The incision site must have approximately 1 cm in length to be large enough to receive the implant.
- Gently scrape the cranium with a bone scraper to improve glue and cement adherence. Do this light handedly with the intention of creating micro scratches.
- Carefully position surgical hooks to the loose skin to maintain an open surgical field and free of obstructions such as skin and fur.
- Use a sterile cotton swab to dry the animal's scalp.
- Use a dissecting microscope to visualize the top of the animal's cranium.
- Attach a needle to the stereotaxic holder and locate the bregma. Position the needle directly above the animal's head slightly touching the bregma.
- Zero out all coordinates on the digital tracer and then raise the needle.
- Fix the tDCS implant on the stereotaxic holder. Position the implant over the animal's head and lower it slowly onto the region of interest using the proper stereotaxic coordinates.
- Use a needle to spread 1 drop (approximately 35 μL) of super glue onto the implant's base.
- Slowly move the holder downwards until it touches the skull. Be sure that the implant base is entirely in contact with the surface.
- Prepare the surgical cement according to the manufacturer's instructions.
- After precise positioning, apply 3 thin, even layer of cement across the cranium and onto the lower portion of the implant. Apply drop per drop using an application brush. Layers must form a hill-shaped structure for further structural support of the implant.
- Leave the implant's screw thread clean of cement to allow a smooth, unobstructed connection.
- Allow each layer to dry for approximately 4 minutes.
- When dry, carefully remove the holder until it is completely detached from the implant. Always use extreme caution when handling the implant, since it may be accidentally extracted from the animal's skull.
- Finishing surgery and post-surgical care
- Hydrate the animal's skin in the incision site with a saline-soaked cotton swab.
- Coat the skin over the base of the tDCS implant.
- Use a pair of tweezers to bring the tissue together and close the incision with a drop of surgical tissue glue per 0.2 cm of tissue.
- Infiltrate 1-2% lidocaine in the incision site and underlying tissues.
- Hydrate the mouse with 500 µL of lactate Ringer's solution subcutaneously.
- Place the mouse into a pre-warmed (37 °C) clean, single-housed cage.
- Put a small dish with wet food pellets in the cage for easy access to food in the following hours.
- Register the animal's post-surgical weight.
- Give the animal ketoprofen (5 mg/kg) subcutaneously after the surgery and on the next 2 days.
- Monitor the recovery of the animal closely for at least 1 week. Assess any sign of distress, such as piloerection, lack of grooming, reduced locomotion, wound scratching and inflammation of the surgical site.
2. tDCS Setup and Stimulation
- tDCS Setup (see Figure 2)
Note. Make sure that the tDCS stimulator is fully charged.- Attach the anode and cathode cables to the tDCS stimulator and make them available near the stimulation site. Attach the pin-type electrode to the stereotaxic holder.
- Set the thermal platform to 37 °C.
- Turn on the oxygen flowmeter on the inhalation anesthesia system to 1 L/min.
- Place the mouse into the anesthesia induction chamber.
- Turn on the isoflurane vaporizer to 3%. Allow the animal to undergo isoflurane effects for 4 min.
- While the animal is in the induction chamber, use a sterile syringe to fill the body electrode with 0.9% saline solution.
- Remove the animal from the induction chamber and position its chest over the body electrode.
- Gently slide the anesthesia mask over the mouse's nose and fix it in place. Lower the isoflurane output to 1.5%.
- Fill the implant and the pin-type electrode with saline and carefully attach them.
- Adjust stimulation time and current intensity.
- Verify the contact quality on the tDCS stimulator.Optimal contact goes from 7 to 10 on a 1 to 10 scale.
- Stimulation
- Start the stimulation.
- Observe the current ramping up for 30 s to the selected value and maintaining itself steady for the established time, then, at the end of the session ramping down again.
- Activate the sham button for control mice.
- Observe the current ramping up for 30 s to the selected value and then down to 1 for the rest of the stimulation period with a final ramp to the selected value at the end with a consecutive ramp down.
- Once the stimulation session is complete, carefully transfer the animal to a pre-warmed (37 °C) cage for 10 min.
Note. Animals start to awaken after 3 min. - Turn the inhalation anesthesia system off.
Representative Results
The surgical protocol presented long-term implant stability for at least one month, with no inflammatory signals at the stimulated site nor any other undesired effect. All the animals survived the surgical procedure and tDCS sessions (n = 8). In this experiment, tDCS implants were positioned over the M1 and M2 cortices (+1.0 mm anterior-posterior and 0.0 mm lateral to bregma). One week later, tDCS (n = 3-4) and sham (n = 3) mice were stimulated for five consecutive days during 10 min at 0.35 mA. Contact quality (CQ) values were registered to assess implant viability and no significant differences were found between the groups during a 5-day stimulation procedure (Figure 3A). By using this animal model, stimulation success can be determined through the evaluation of gene expression levels for brain-derived neurotrophic factor (BDNF) and glial fibrillary acidic protein (GFAP). Both BDNF and GFAP presented significantly higher mRNA levels in the cortex area below the implant when compared to the sham group. The effects of tDCS on gene expression seem to be restricted to specific genes since expression levels of the activity-regulated cytoskeleton-associated protein (ARC), and synapsin 1 (SYN1) genes were not changed (Figure 3B).
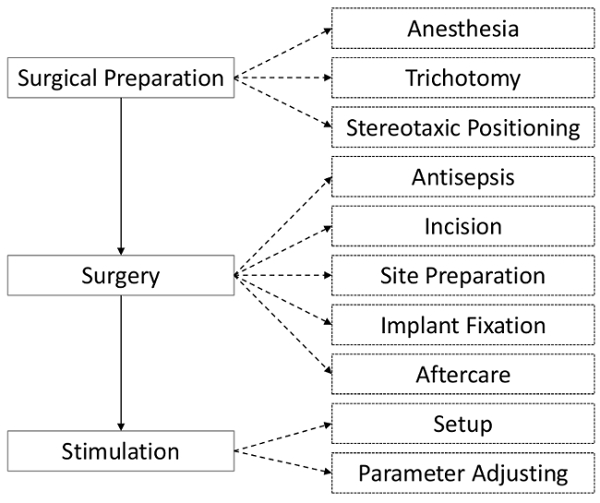
Figure 1. Experimental steps used for implant surgery and stimulation. A schematic flowchart of the steps through tDCS implant placement, tDCS setup, and stimulation procedure. Please click here to view a larger version of this figure.
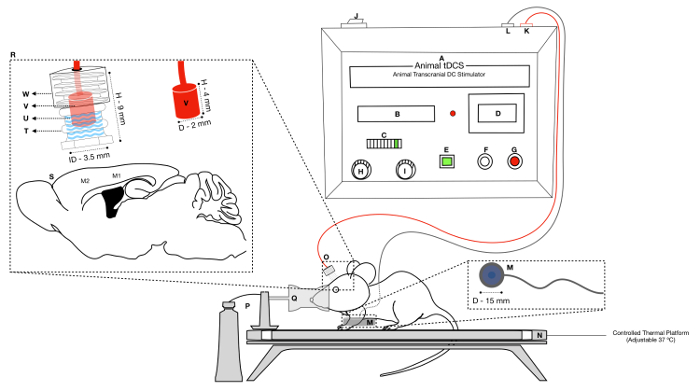
Figure 2. tDCS Setup. The right superior image corresponds to aschematic of the tDCS current stimulator (A), which contains a display for the current intensity and stimulation duration (B), a CQ display (C) scaling from 1 to 10 and a true current display (D). The tDCS stimulator also has buttons to activate sham stimulation (E), to start stimulation (F), and to abort the protocol (G). The two knobs are used for adjusting the current intensity (H) and stimulation duration (I). The on/off switch is located at the rear side (J). Two female insertable entrances are utilized for the electrode cables (K, negative pole) (L, positive pole). The right inferior image showsthe animal setup with the head electrode made of Ag/AgCl (O) and the body electrode made of nickel-plated brass (M) sets and their respective dimensions. An auto adjusted thermal platform (N) maintains the animal's temperature, and isoflurane mixed with 100% oxygen (P) is supplied through the stereotaxic gas mask (Q). The inset (R) shows the positioning of the anode relative to the cortical motor regions M1 and M2 (S). The tDCS headstage is composed of an implantable holder (T) filled with saline (0.9% NaCl) (U) which is closed with a pin-type electrode (V) attached to a plastic cap (W). The respective dimensions are depicted in millimeters (D = diameter, H = height, ID = internal diameter). Please click here to view a larger version of this figure.
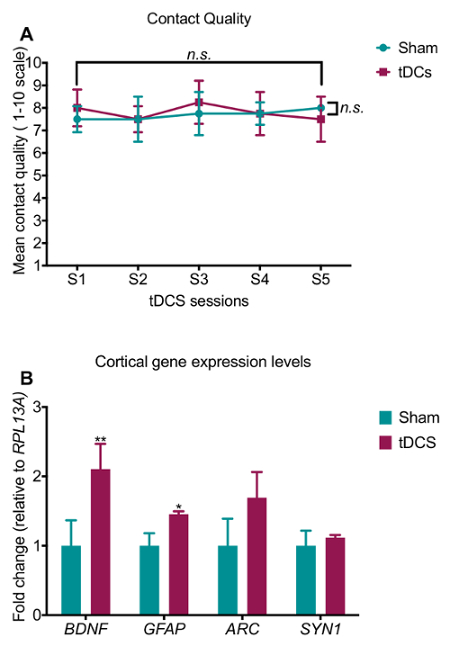
Figure 3. Contact quality and gene expression changes evoked by tDCS. (A) No statistical differences were observed for contact quality (CQ) among the groups. Two-way repeated measures ANOVA, treatment versus day interaction (F4.30 = 0.552, P = 0.698), treatment factor (F4.30 = 0.349, P = 0.810), day factor (F1.30 = 0.157, P = 0.694). (B) Quantitative polymerase chain reaction gene expression data for BDNF (Brain-derived neurotrophic factor), GFAP (glial fibrillary acidic protein), ARC (activity-regulated cytoskeleton-associated protein) and SYN1 (synapsin 1). mRNA levels of both BDNF (p = 0.0081) and GFAP (p = 0.0108) were increased while no change was detected for ARC (p = 0.0760) and SYN1 (p = 0.508), according to D'Agostino-Pearson normality test followed by unpaired parametric Student's t-test. Fold changes were calculated using the 2-ΔΔCQ method relative to RPL13A gene. In all graphs, tDCS group is magenta and sham group is green; n = 3-4/group. Data are expressed as mean and ± S.E.M. error bars. n.s. = nonsignificant, p ≤ 0.05*, p ≤ 0.01**. Please click here to view a larger version of this figure.
Discussion
In recent years, neurostimulation techniques have been entering clinical practice as a promising procedure to treat neuropsychiatric disorders23. To reduce the constraint imposed by the lack of knowledge of the mechanisms of neurostimulation, we presented here a tDCS mouse model carrying an electrode that can target brain regions. Since the electrode is chronically implantable, this animal model enables the investigation of long-lasting biological effects evoked by tDCS (for at least 1 month) in complex stimulation patterns. The described tDCS animal model presents high implant tolerance and little chance of infection if executed correctly. Overall, the surgery steps to place the implant are of quick and straightforward execution (30 min/animal). One additional advantage of this tDCS model is that it is possible to track the electrode contact quality and the actual current stimulation values.
The main drawback of this animal model is the proper implant fixation on the mouse's cranium. During surgery, it is essential to restrict the animal's head in a manner in which no lateral head shifting is possible (the head will only move vertically). This will assure that the animal's scalp is wholly aligned with the implant's base, allowing proper fixation with the dental cement, and higher precision in modulating the intended target area. It is critical to make the incision large enough to receive the implant. A larger cut may be necessary for some tDCS implants. Using two to four surgical hooks made from hypodermic needles will increase the cemented area. However, avoid placing the hooks too close to the animal's eyes to remove any possibility of lesions. Whereas gently scratching the scalp will improve the adhesion of the super-glue and the cement onto the cranium, any residual debris may prevent good implant adherence. Furthermore, when applying the dental cement, prepare the first layer with a higher viscosity, which avoids the cement of running down the animal's skull. Each cement layer must be allowed to dry for at least 4 min because applying cement over wet layers will delay the hardening of the bottom layers and may cause the implant to shift or even fall. From experience, there must be no more than 3 layers of cement around the implant to avoid obstruction of the screw thread. For both the glue and the cement, be sure to maintain their application restricted to the implant's base. Avoid allowing residue to spread within the implant, which will decrease the surface conductivity and lower the tDCS effects.
The implantable electrode used in this procedure was not fabricated in-house but acquired from a medical research company specialized in producing neuromodulation devices. The implants are made out of polypropylene with 9 mm of height and an outer and inner diameter of 5.7 mm and 3.5 mm, respectively. It can hold a total saline volume of 80 µL. The superior portion of the implant is prepared with a screw thread to receive a pin-type electrode holder. The pin-type electrode holder's outer body is also made of polypropylene measuring 4 mm high with a 5.3 mm outer diameter and a 3.75 mm inner diameter. The electrode pin is made from Ag/AgCl, an inert material used due to its non-dissolving properties (Figure 2). Since the implant location is a critical factor for effective tDCS, it is essential to select a proper electrode size according to the region of interest. The implant used in this animal model occupies a surface area of 9.61 cm2, spreading the electrical field over a 1.75 mm radius from the intended brain coordinate resulting in a 36,3967 μA/cm2 current density. Possibly, the tDCS stimulus executed in this protocol was mostly directed to the M1 and M2 cortices.
Usually, the electrode configuration varies according to the intended excitatory or inhibitory stimulation effects (anodal versus cathodal). Although currents will always flow out of the anode in the direction of the cathode, by placing the electrode in inverted terminal positions enables different electrophysiology effects. For example, when ions flow from the cathode in the direction of the anode, the procedure is usually defined as a cathodal stimulation24. In this experiment, we performed anodal stimulation in which the anode was placed over the M1/M2 cortices, and the cathode was placed down on the animal's thorax. Thus, in our tDCS setup, it is expected that stimulation produces excitatory potentials25. The tDCS effect can also be regulated through the changes in current intensity and duration. Most studies in rodents have used currents varying from 0.2 to 1.0 mA. tDCS currents are expected to generate concentrated heat traveling through the electrode. The direct contact of the tDCS electrode to the animal's head must be avoided. The use of conducting mediums stretches the distance between the electrode and the cranium and prevents the harmful effects of local chemical reactions on the biological tissue. It is possible that a high ionic concentration in liquid conduct media may cause gas formation and bubbles resulted from electrolysis23,24. However, this is unlikely to have happened in our tDCS model since isotonic saline solution and low current delivery may decrease the chance of such complications24. Nevertheless, other conducting media can also be used with similar efficiencies, such as gelatinous and cream-like conductors24.
When choosing the tDCS stimulator, it is vital to consider flexible configuration capabilities. For this protocol, we used a stimulator powered by two 9 V alkaline batteries, which render an expected duration of 1 h of stimulation at 0.35 mA. This stimulator possesses a 0.02 to 1 mA current range with a 10 µA resolution, ideal for rodent stimulation. It is critical that the tDCS stimulator is equipped with an actual current indicator and contact quality (CQ) feedback system to verify optimal stimulation conditions. The current indicator assures when the programmed stimulation intensity is being met. In this tDCS model, the most common factor for faulty current is the presence of bubbles in the saline solution. This issue can be indicated by the CQ feedback system, which measures the contact of both electrodes through the conducting medium and the animal's body. The tDCS stimulator used throughout this experiment displays CQ (SMARTscan) values varying from 1 to 10 on a led scale. This scale is based on voltage values that can infer resistance according to Ohm's law. Led 1 indicates little or atypical low resistance, led 2 indicates open circuit and led 3 through 10 indicates poor to optimal quality (Figure 2-item C). The CQ was registered daily for both tDCS and sham groups to verify the electrode viability. It is noteworthy that the average CQ value during stimulation session was higher than 7, meaning that desired currents are being delivered. Overall, no statistical differences were observed for CQ among the groups or day of stimulation (Figure 3A). To further validate our tDCS model, we performed quantitative polymerase chain reactions (qPCR) to investigate whether five tDCS sessions (10 min, 350 μA) change cortical gene expression. We found that mRNA levels of BDNF and GFAP were increased in the M1/M2 cortex of tDCS groups, relative to the Sham mice (Figure 3B). These results are consistent with other studies19,25.
Neurostimulation studies in experimental animals can provide new insights regarding the brain mechanisms with relevance to neuropsychiatric disorders. Depending on the experimental configuration, the tDCS assembly in this animal model can also be combined with an existing optogenetic or electrophysiology headstage to produce a setup for simultaneous recording and stimulation, alongside a multitude of brain sample experiments. These approaches would be challenging to carry out in humans. Therefore, the opportunity of inserting flexible additions to the currently reported animal tDCS offers a prominent contribution for the understanding of the neural subtracts of tDCS and the rationale for its therapeutic use.
Divulgazioni
The authors have nothing to disclose.
Acknowledgements
We thank Mr. Rodrigo de Souza for assistance in maintaining mouse colonies. L.A.V.M is a CAPES postdoctoral fellow. This work was supported by the grant PRONEX (FAPEMIG: APQ-00476-14).
Materials
| BD Ultra-Fine 50U Syringe | BD | 10033430026 | For intraperitonially injection. |
| Shaver (Philips Multigroom) | Philips (Brazil) | QG3340/16 | For surgical site trimming. |
| Surgical Equipment | |||
| Model 940 Small Animal Stereotaxic Instrument with Digital Display Console | KOPF | 940 | For animal surgical restriction and positioning. |
| Model 922 Non-Rupture 60 Degree Tip Ear Bars | KOPF | 922 | For animal surgical restriction and positioning. |
| Cannula Holder | KOPF | 1766-AP | For implant positioning. |
| Precision Stereo Zoom Binocular Microscope (III) on Boom Stand | WPI | PZMIII-BS | For bregma localization and implant positioning. |
| Temperature Control System Model | KOPF | TCAT-2LV | For animal thermal control. |
| Cold Light Source | WPI | WA-12633 | For focal brightness |
| Tabletop Laboratory Animal Anesthesia System with Scavenging | VetEquip | 901820 | For isoflurane delivery and safety. |
| VaporGuard Activated Charcoal Adsorption Filter | VetEquip | 931401 | Delivery system safety measures. |
| Model 923-B Mouse Gas Anesthesia Head Holder | KOPF | 923-B | For animal restriction and O2 and isoflurane delivery. |
| Oxygen regulator, E-cylinder | VetEquip | 901305 | For O2 regulation and delivery. |
| Oxygen hose – green | VetEquip | 931503 | For O2 and isoflurane delivery. |
| Infrared Sterilizer 800 ºC | Marconi | MA1201 | For instrument sterilization. |
| Surgical Instruments | |||
| Fine Scissors – ToughCut | Fine Science Tools | 14058-11 | For incision. |
| Surgical Hooks | INJEX | 1636 | In House Fabricated – Used to clear the surgical site from skin and fur. |
| Standard Tweezers or Forceps | – | – | For skin grasping. |
| Surgical Consumables | |||
| Vetbond | 3M | SC-361931 | For incision closing. |
| Cement and Catalyzer KIT (Duralay) | Reliance | 2OZ | For implant fixation. |
| Sterile Cotton Swabs (Autoclaved) | JnJ | 75U | For surgical site antisepsis. |
| 24 Well Plate (Tissue Culture Plate) | SARSTEDT | 831,836 | For cement preparation. |
| Application Brush | parkell | S286 | For cement mixing and application. |
| Pharmaceutics | |||
| Xylazin (ANASEDAN 2%) | Ceva Pharmaceutical (Brazil) | P10160 | For anesthesia induction. |
| Ketamine (DOPALEN 10%) | Ceva Pharmaceutical (Brazil) | P30101 | For anesthesia induction. |
| Isoflurane (100%) | Cristália (Brazil) | 100ML | For anesthesia maintenance. |
| Lidocaine (XYLESTESIN 5%) | Cristal Pharma | – | For post-surgical care. |
| Ketoprofen (PROFENID 100 mg) | Sanofi Aventis | 20ML | For post-surgical care. |
| Ringer's Lactate Solution | SANOBIOL LAB | ############ | For post-surgical care. |
| TobraDex (Dexamethasone 1 mg/g) | Alcon | 631 | For eye lubrification and protection. |
| Stimulation | |||
| Animal Transcranial Stimulator | Soterix Medical | 2100 | For current generation. |
| Pin-type electrode Holder (Cylindrical Holder Base) | Soterix Medical | 2100 | Electrode support (Implant). |
| Pin-type electrode (Ag/AgCl) | Soterix Medical | 2100 | For current delivery (electrode). |
| Pin-type electrode cap | Soterix Medical | 2100 | For implant protection. |
| Body Electrode (Ag/AgCl Coated) | Soterix Medical | 2100 | For current delivery (electrode). |
| Saline Solution (0.9%) | FarmaX | ############ | Conducting medium for current delivery. |
| Standard Tweezers or Forceps | – | – | For tDCS setup. |
| Real Time Polymerase Chain Reaction | |||
| BioRad CFX96 Real Time System | BioRad | C1000 | For qPCR |
| SsoAdvancedTM Universal SYBR Green Supermix (5 X 1mL) | BioRad | 1725271 | For qPCR |
| Hard Shell PCR Plates PCT COM 50 p/ CFX96 | BioRad | HSP9601 | For qPCR |
| Microseal "B" seal pct c/ 100 | BioRad | MSB1001 | For qPCR |
Riferimenti
- Filmer, H. L., Dux, P. E., Mattingley, J. B. Applications of transcranial direct current stimulation for understanding brain function. Trends in Neurosciences. 37 (12), 742-753 (2014).
- Nitsche, M. A., Paulus, W. Sustained excitability elevations induced by transcranial DC motor cortex stimulation in humans. Neurology. 57 (10), 1899-1901 (2001).
- Kronberg, G., Bridi, M., Abel, T., Bikson, M., Parra, L. C. Direct Current Stimulation Modulates LTP and LTD: Activity Dependence and Dendritic Effects. Brain Stimulation. 10 (1), 51-58 (2017).
- Pelletier, S. J., Cicchetti, F. Cellular and Molecular Mechanisms of Action of Transcranial Direct Current Stimulation: Evidence from In Vitro and In Vivo Models. International Journal of Neuropsychopharmacology. 18 (2), pyu047 (2015).
- Chang, M. C., Kim, D. Y., Park, D. H. Enhancement of cortical excitability and lower limb motor function in patients with stroke by transcranial direct current stimulation. Brain Stimulation. 8 (3), 561-566 (2015).
- Lefaucheur, J. P., et al. Evidence-based guidelines on the therapeutic use of transcranial direct current stimulation (tDCS). Clinical Neurophysiology. 128 (1), 56-92 (2017).
- Monai, H., et al. Calcium imaging reveals glial involvement in transcranial direct current stimulation-induced plasticity in mouse brain. Nature Communications. 7, 11100 (2016).
- Marquez-Ruiz, J., et al. Transcranial direct-current stimulation modulates synaptic mechanisms involved in associative learning in behaving rabbits. Proc. Natl. Acad. Sci. 109, 6710-6715 (2012).
- Jackson, M. P., et al. Animal models of transcranial direct current stimulation: Methods and mechanisms. Clinical Neurophysiology. 127 (11), 3425-3454 (2016).
- Cambiaghi, M., et al. Brain transcranial direct current stimulation modulates motor excitability in mice. The European journal of neuroscience. 31 (4), 704-709 (2010).
- Monte-Silva, K., et al. Induction of late LTP-like plasticity in the human motor cortex by repeated non-invasive brain stimulation. Brain Stimulation. 6 (3), 424-432 (2013).
- San-Juan, D., et al. Transcranial Direct Current Stimulation in Mesial Temporal Lobe Epilepsy and Hippocampal Sclerosis. Brain Stimulation. 10 (1), 28-35 (2017).
- Brunoni, A. R., et al. Transcranial direct current stimulation (tDCS) in unipolar vs. bipolar depressive disorder. Progress in Neuro-Psychopharmacology and Biological Psychiatry. 35 (1), 96-101 (2011).
- Brunoni, A. R., et al. Trial of Electrical Direct-Current Therapy versus Escitalopram for Depression. New England Journal of Medicine. 376 (26), 2523-2533 (2017).
- Boggio, P. S., et al. Prolonged visual memory enhancement after direct current stimulation in Alzheimer’s disease. Brain Stimulation. 5 (3), 223-230 (2012).
- Cosentino, G., et al. Anodal tDCS of the swallowing motor cortex for treatment of dysphagia in multiple sclerosis: a pilot open-label study. Neurological Sciences. , 7-9 (2018).
- Kaski, D., Dominguez, R. O., Allum, J. H., Islam, A. F., Bronstein, A. M. Combining physical training with transcranial direct current stimulation to improve gait in Parkinson’s disease: A pilot randomized controlled study. Clinical Rehabilitation. 28 (11), 1115-1124 (2014).
- Monai, H., et al. Calcium imaging reveals glial involvement in transcranial direct current stimulation-induced plasticity in mouse brain. Nature Communications. 7, 11100 (2016).
- Fritsch, B., et al. Direct current stimulation promotes BDNF-dependent synaptic plasticity: potential implications for motor learning. Neuron. 66 (2), 198-204 (2010).
- Winkler, C., et al. Sensory and Motor Systems Anodal Transcranial Direct Current Stimulation Enhances Survival and Integration of Dopaminergic Cell Transplants in a Rat Parkinson Model. New Research. 4 (5), 17-63 (2017).
- Nasehi, M., Khani-Abyaneh, M., Ebrahimi-Ghiri, M., Zarrindast, M. R. The effect of left frontal transcranial direct-current stimulation on propranolol-induced fear memory acquisition and consolidation deficits. Behavioural Brain Research. 331 (May), 76-83 (2017).
- Souza, A., et al. Neurobiological mechanisms of antiallodynic effect of transcranial direct current stimulation (tDCS) in a mice model of neuropathic pain. Brain Research. 1682 (14-23), (2018).
- Woods, A. J., et al. A technical guide to tDCS, and related non-invasive brain stimulation tools. Clinical Neurophysiology. 127 (2), 1031-1048 (2016).
- Cogan, S. F., et al. Tissue damage thresholds during therapeutic electrical stimulation. Journal of Neural Engineering. 13, 2 (2017).
- Podda, M. V., et al. Anodal transcranial direct current stimulation boosts synaptic plasticity and memory in mice via epigenetic regulation of Bdnf expression. Scientific reports. 6 (October 2015), 22180 (2015).

