Optogenetic Manipulation of Neural Circuits During Monitoring Sleep/wakefulness States in Mice
Summary
Here, we describe methods of optogenetic manipulation of particular types of neurons during monitoring of sleep/wakefulness states in mice, presenting our recent work on the bed nucleus of the stria terminalis as an example.
Abstract
In recent years, optogenetics has been widely used in many fields of neuroscientific research. In many cases, an opsin, such as channel rhodopsin 2 (ChR2), is expressed by a virus vector in a particular type of neuronal cells in various Cre-driver mice. Activation of these opsins is triggered by application of light pulses which are delivered by laser or LED through optic cables, and the effect of activation is observed with very high time resolution. Experimenters are able to acutely stimulate neurons while monitoring behavior or another physiological outcome in mice. Optogenetics can enable useful strategies to evaluate function of neuronal circuits in the regulation of sleep/wakefulness states in mice. Here we describe a technique for examining the effect of optogenetic manipulation of neurons with a specific chemical identity during electroencephalogram (EEG) and electromyogram (EMG) monitoring to evaluate the sleep stage of mice. As an example, we describe manipulation of GABAergic neurons in the bed nucleus of the stria terminalis (BNST). Acute optogenetic excitation of these neurons triggers a rapid transition to wakefulness when applied during NREM sleep. Optogenetic manipulation along with EEG/EMG recording can be applied to decipher the neuronal circuits that regulate sleep/wakefulness states.
Introduction
Sleep is essential for optimal cognitive function.Recent findings also suggest that disturbances in sleep are associated with a wide range of diseases1,2,3. Although the functions of sleep are as yet largely unresolved, substantial progress has been made recently in understanding the neural circuits and mechanisms that control sleep/wakefulness states4. In mammals, there are three states of vigilance: wakefulness, non-rapid eye movement (NREM) sleep, and rapid eye movement (REM) sleep. Wakefulness is characterized by fast EEG oscillations (5-12 Hz) of low amplitude with purposeful and sustained motor activity. NREM sleep is defined by slow oscillations (1-4 Hz) of high amplitude (delta waves), with lack of consciousness and purposeful motor activity. REM sleep is characterized by relatively fast oscillations (6-12 Hz) of low amplitude and almost complete bilateral muscle atonia5.
Borbely proposed a theory of sleep-wakefulness regulation known as the two process model6,7. A homeostatic process, also referred to as process S, represents sleep pressure that accumulates during wakefulness and dissipates during sleep. Another process, referred to as process C, is a circadian process, which explains why vigilance levels fluctuate in the 24 h cycle. In addition to these two processes, allostatic factors are also important for regulation of sleep/wakefulness8,9. Allostatic factors include nutritional states and emotion. Fear and anxiety are usually accompanied by an increase in arousal along with autonomic and neuroendocrine responses10,11,12. The limbic system is believed to play a role in regulation of fear and anxiety, and mechanisms underlying autonomic and neuroendocrine responses have been studied extensively, but the pathway by which the limbic system influences sleep/wakefulness states has not yet been revealed. A large number of recent studies using opto- and pharmacogenetics have suggested that neurons and neuronal circuits that regulate sleep/wakefulness states are distributed throughout the brain, including the cortices, basal forebrain, thalamus, hypothalamus, and brain stem. In particular, recent advances in optogenetics have allowed us to stimulate or inhibit specific neural circuits in vivo with high spatial and temporal resolutions. This technique will allow progress in our understanding of the neural substrates of sleep and wakefulness, and how sleep/wakefulness states are regulated by circadian processes, sleep pressure, and allostatic factors, including emotion. This paper aims to introduce how to use optogenetic manipulation combined with sleep/wake recording, which could have the potential to update our understanding of the connectomes and mechanisms in the brain that play a role in the regulation of NREM sleep, REM sleep, and wakefulness. Understanding of this mechanism by which the limbic system regulates sleep/wakefulness states is of paramount importance to health, because insomnia is usually associated with anxiety or fear of being unable to sleep (somniphobia).
The BNST is thought to play an essential role in anxiety and fear. GAD 67-expressing GABAergic neurons are a major population of the BNST12,13. We examined the effect of optogenetic manipulation of these neurons (GABABNST) on sleep/wakefulness states. One of the greatest advances in neuroscience in recent years has been methods that enable manipulation of neurons with particular chemical identities in vivo, with high spatial and temporal resolutions. Optogenetics is highly useful for demonstrating causal links between neural activity and specific behavioral responses14. We describe optogenetics as a method to examine the functional connectivity of defined neural circuits in the regulation of sleep/wakefulness states. By utilizing this technique, great progress has been achieved in understanding the neuronal circuits that regulate sleep/wakefulness states15,16,17,18,19. In many cases, opsins are specifically introduced in neurons with particular chemical identities in selective brain regions by a combination of Cre-driver mice and Cre-inducible AAV-mediated gene transfer. Further, focal expression of photo-sensitive opsins such as channelrhodopsin 2 (ChR2)20 or archaerhodopsin (ArchT)21 combined with a Cre-loxP or Flp-FRT system allows us to manipulate a selective neuronal population and specific neural pathway22.
We describe here experiments on GABAergic neurons in the BNST as an example. To express opsins in a designated neuronal population, appropriate Cre driver mice and Cre-dependent virus vectors are most frequently used. Transgenic or knock-in lines in which opsins are expressed in particular neuronal populations are also useful. In the following experiments, we used GAD67-Cre knock-in mice23 in which only GABAergic neurons express Cre recombinase with a C57BL/6J genetic background, and an AAV vector which contains ChR2 (hChR2 H134R) fused with EYFP or EYFP as a control with a "FLEx (Flip-excision) switch"24. The procedure specifically describes optogenetic excitation of GABAergic neurons in the BNST during monitoring of sleep/wakefulness states25.
Protocol
All experiments here were approved by the Animal Experiment and Use Committee of the University of Tsukuba, complying with NIH guidelines.
1. Animal Surgery, Virus Injection, Electrode for EEG/EMG, and Optical Fiber Implantation
CAUTION: Appropriate protection and handling techniques should be selected based on the biosafety level of the virus to be used. AAV should be used in an isolated P1A graded room for injection, and the tube carrying AAV must be sterilized with an autoclave after all the volume is used up. The surgical site and all implanted material should be clean and sterile during use.
NOTE: See Figure 1.
- Disinfect the surgical equipment with the autoclave.
- Anesthetize mice with isoflurane using an anesthetic vaporizer. Observe until the mouse has reached the desired depth of anesthesia, determined by loss of response to pinching the tail with forceps. Apply ophthalmic ointment to the eyes to prevent them drying.
- Disinfect the surgical field with iodine solution or 70% EtOH (3x) and dry sufficiently. Allow the virus to thaw on ice as the surgery is being performed. Cover the surgical area with absorbent lab bench paper.
- Fix the mouse's head in the stereotactic apparatus with ear bars and a nose pinch. After confirming the head is held stably, make a midsagittal incision in the scalp to ensure the positions of the bregma and lambda are located at the same level on a horizontal line.
- To avoid a positioning gap, appropriately adjust the levels of the nose pinch and ear bars up and down. The bregma and lambda refer to the intersection between the sutura saggitalis and sutura coronalis or sutura lambdoidal, respectively (Figure 2).
- Use Serafin clamps to hold the skin to maintain access to the cranium. After exposure of the skull, disinfect the surface of the skull with iodine or 5% H2O2, to enable the cranial sutures including the bregma and lambda to be visualized more clearly.
- Prepare AAV vector injection:
- Wash the inside of a 10 mL syringe (see Table of Materials) sequentially with 70% EtOH, 100% EtOH, and sterilized water, 5 times each. Secure the syringe in the clamp of a microinjection pump arm and make sure all solution in the syringe is discharged.
- Carefully aspirate 2 µL of mineral oil without air bubbles, then aspirate the designated volume of the virus solution. After aspiration, manipulate the plunger button and confirm that virus solution emerges at the tip of the needle.
NOTE: The injection volume of the virus solution was determined in pilot experiments using the same mouse strain and same virus product. The relation between the volume of virus solution and extent of the infection area should be estimated in advance.
- Inject AAV vector:
- Adjust the tip of the microinjection needle on the bregma and note the coordinates as the original point. Move the tip to the designated injection site (for the BNST: anteroposterior + 0.2 mm, mediolateral ± 1.0 mm, dorsoventral – 4.2 mm) and place the tip of the needle onto the position. Put a mark on the skull and drill holes of approximately 2 mm in diameter using a dental drill with a 0.7 mm carbide cutter. Be careful not to damage the dura or brain tissue.
- After removing blood from around the holes with a cotton swab, slowly move the needle into the position of the BNST. Slowly inject the designated amount of virus solution (0.07 µl/min) with a mechanical microinjector. After completing the injection, leave the needle for 5 min to allow the solution to sufficiently infiltrate the BNST tissue. Carefully take out the needle.
- For bilateral injection, repeat steps 1.8.1-1.8.2 on the other side. Throughout the procedure, keep the skull moist with applications of sterile saline.
NOTE: We used custom EEG/EMG implants (W: 5 mm, D: 7 mm, H: 1 mm) with four EEG electrodes (4 mm), two EMG electrodes (2 mm; cut the 4 mm electrode to 2 mm with nippers) and 6 electrodes (4.5 mm) (Figure 2A).
- Solder two stainless steel wires (see Table of Materials) from which 1 mm of the insulation is stripped off both ends to the EMG electrodes. Adjust the center of the electrodes to the bregma and mark the position of each EEG electrode (anteroposterior ± 1.5 mm, mediolateral ± 1.0 mm), and determine the position of the implant (Figure 2B).
- Implant optical fibers:
- Attach an optic fiber ferrule to the manipulator and rotate the manipulator arm so that it has an angle of ±30° against a horizontal line (this process is only needed to avoid interference between electrodes and optic fibers, such as in the case of BNST stimulation). Put the fiber tip on the bregma and record the coordinates.
- Move the tip to the targeted insertion line and mark the position on the skull. Also put additional marks near the insertion site for the anchor screws. Drill the skull on each site with a dental drill to insert the optic fiber and fix the screw. Fix the screw on the skull. Be careful not to break the dura or damage any tissue by screw.
- Insert the optic fiber gently until reaching above the BNST with a manipulator. The ferrule should rest on the remaining cranium (Figure 1B).
- Apply photocurable dental cement (see Table of Materials) to cover the fiber and the screw. The reaction time to solidify the glue should be specified by the manufacturer's manual (Our material needs exposure to light for at least 10 s with specific wave length photo-generator. It is unnecessary to dry the glue after this).
- In this step, make sure that no materials (screw or glue) occupy the mounting space for the electrodes. In addition, avoid making any interruption in the cement for the ferrule connecting to the optic fiber and cable. Repeat steps 1.10.1-1.10.4 on the opposite side for bilateral stimulation.
- Drill holes for EEG/EMG electrodes. Insert the tips of the electrodes into the holes. Hold the implant and apply cyanoacrylate adhesive to the space between the skull and the electrodes. Insert again with attention not to interfere with any materials.
- Cover the circumference of the electrodes and optic fibers with cyanoacrylate adhesive followed by application of cyanoacrylate accelerant on the adhesive. This step avoids causing any interruption at the ferrule-to-optic cable and electrode-to-lead wire connecting zone (Figure 1C).
NOTE: Cyanoacrylate adhesive and its accelerant are harmful to the mouse eye. Pay attention not to cause spillage of these chemical substances. Also, be careful not to strongly touch the electrodes and the fibers in order to avoid unexpected deviation immediately after adhesive solidification. - Expose the mouse neck muscles and insert the wires for the EMG electrode under the muscle. Adjust the length of EMG electrode so that it locates just under the nuchal muscles. Light connection between tip of electrode and muscle fascia is enough to catch the EMG signal.
- Apply cyanoacrylate adhesive to fill the implants and solidify the adhesive with acceleration liquid. Then, put the mouse on a heat pad for recovery until the postural reflex appears. Adjust heat pad temperature to animal resting body temperature (36.0 °C in ZT 0-12 in case of C57BL6 mice; do not exceed 38.0 °C).
NOTE: An antibiotic is not required for sterile surgery. - Follow your local institutional guidelines for post-operative analgesia. Keep the mice in a home cage for a recovery period of at least 7 days.
2. EEG/EMG Monitoring with Photo-excitation of Targeted Neurons in Specific Sleep States
CAUTION: This protocol includes use of class 3B laser equipment or LED devices. Experimenters should be aware of safety information. Protective eye goggles are required.
- Before connecting the laser cable to the optic fiber, adjust laser intensity with a scaler. Tether the tip of the laser cable to an unused optic fiber with a ferrule and confirm that there is no space at the junction between the fiber and the cable.
- Turn on the main switch of the laser and wait 20 min for it to warm up.
- Emit the laser to the intensity checker and adjust laser intensity to 10 mW/mm2. Change the laser mode to transistor logic and confirm that light pulses are emitted from the fiber controlled by the pattern regulator which is set at 10 ms for duration, 40 ms for rest, 20 times for cycle, and 20 times repeat (that is, 20 Hz of 10 ms light pulses for 20 s).
- After the recovery period, move the mice to the experimental chamber for recording EEG/EMG. House mice at a constant 23 °C with a 12 h light/dark cycle with food and water available ad libitum.
- Connect the implanted electrode and cable adaptor which is tethered to a slip ring to avoid entanglement. It is recommended to cover the junction with light-impermeable material such as aluminum foil to prevent laser leakage. If a bilateral experiment is required, use a slip ring with a bifurcate attachment for the cables.
- In this protocol, we assess latency to wakefulness from NREM sleep or REM sleep, so the recording time should be limited in optimized zeitgeber time (ZT0 is defined as the time when the light is on). This protocol was conducted between ZT4 – ZT10. Let the mice stay freely in the experimental chamber for at least 1 h as acclimatization.
- During the experimental period, monitor EEG and EMG signals in the same monitor and evaluate the mouse's state as wakefulness, NREM sleep or REM sleep. Use the gain control for each wave to make it easier to distinguish each state.
- For measurement of NREM sleep to wakefulness latency, observe stable NREM sleep for 40 s or stable REM sleep for 30 s, then turn on the switch of the pattern generator for photostimulation (this protocol generates 20 Hz of 10 ms light pulses for 20 s). Confirm laser emission to the implanted optic fibers.
- Record EEG/EMG signals until the sleeping state changes to wakefulness. If two or more experimental trials are needed, limit optogenetic manipulation to once a day because photostimulation is an artificial intervention which might affect sleep/wakefulness architecture.
- After the experiment, deeply anesthetize and perfuse with sterile saline and paraformaldehyde (PFA) for sampling the whole brain for immunohistochemical analysis26.
3. Analysis of Latency Time from NREM Sleep to Wakefulness
- After recording EEG/EMG signals, transfer the signal data to a computer for scoring sleep/wakefulness states. This protocol describes the method for EEG analysis with recording software (see Table of Materials).
- Start the sleep sign application and click the File tab and select Open to choose the recorded data (.kcd file). Click the Sleep tab to select Epoch time for adjusting the time window for each epoch (we use 1 epoch/4 sec).
- Manually score sleep/wakefulness states based on EEG/EMG signals, according to the following criteria: wakefulness, high EMG and low EEG voltage with high frequency; NREM, low EMG tone and high EEG voltage with high δ (0.5-4 Hz) frequency; and REM, EMG indicates muscle atonia and low EEG voltage with high θ (6-9 Hz) frequency. A state that does not consecutively continue for 16 s (i.e. 4 epochs) is not defined as a state change because it is not a stable state.
- Click and hold the left mouse button on the first epoch and drag the cursor until the specific trend of more than 16 s (4 epochs) is ended. Then, release the left mouse button and choose the appropriate state (wakefulness or NREM sleep or REM sleep) in the pop-up window. Repeat this procedure to score all EEG/EMG signals recorded in the file.
- Find the exact time of stimulation in the epoch where the EEG shows NREM or REM sleep, and the epoch showing state transition following the stimulation point. Count the number of epochs between the periods just after stimulation and just before state transition.
- Then multiply counted number of epochs by 4 s (A). In the epoch of stimulation, take a screen shot and measure the width between the stimulation point and the end of the epoch. Then, divide the measured length by the entire epoch length and multiply by 4 s (B). Similarly, calculate the duration of NREM sleep in the epoch of state change, which means the time between the start of the epoch and the state change point (C).
- Sum A, B and C to obtain the latency from NREM sleep to wakefulness. The same procedure is used for analysis of state transition from REM sleep to wakefulness.
Representative Results
The present study showed the effect of optogenetic excitation of GABABNST neurons on sleep state transition. ChR2-EYFP was focally expressed in GABA neurons in the BNST. An in situ hybridization histochemical study showed that ChR2-EYFP was colocalized in neurons expressing GAD 67 mRNA signals, indicating that these are GABAergic neurons. Immunohistochemical slice samples confirmed the position of the optic fiber, whose tip was just above the BNST25.
Figure 3A shows representative EEG/EMG traces before and after photostimulation during NREM sleep. High voltage and slow frequency EEG with no EMG signals represent NREM sleep. Photostimulation (10 ms pulses at 20 Hz for 20 sec) was applied following stable NREM sleep. Stimulation triggers acute transition to wakefulness (low voltage and high frequency EEG with active EMG signals) about 2 s after stimulation in ChR2-expressing mice. Control mice (EYFP) did not show transition after stimulation (latency of waking from NREM: EYFP, 295.39 ± 106.61 sec, n = 6; ChR2: 2.71 ± 0.59 sec, n = 6; t10 = 2.35, p < 0.05; Figure 3B, upper). These data suggest that excitation of GABABNST neurons during NREM sleep triggers rapid induction of wakefulness. On the other hand, photostimulation during REM sleep had no effect (EYFP: 36.45 ± 13.08 sec, n = 6; ChR2: 37.29 ± 15.19 sec, n = 6; t10 = 0.04, p = 0.484; Figure 3B, bottom) so a transition effect only emerged in NREM sleep.
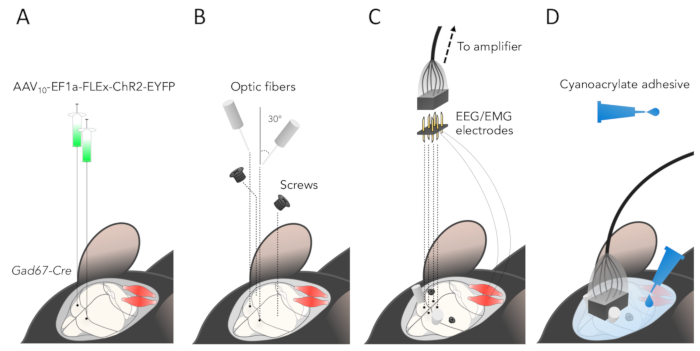
Figure 1: Procedure to inject AAV, implant optic fibers and EEG/EMG implants. (A) Experimental procedure of virus injection. EYFP-fused ChR2 or EYFP (for control) gene incorporated in AAV vector whose transcription is activated by Cre recombinase was bilaterally injected into the BNST. (B) Optic fibers were inserted toward the BNST at a 30° angle to the horizontal to prevent collision with the electrode. Two screws were inserted around it. (C) EEG/EMG recording device was implanted after secured placement of the optic fibers. (D) At the end of the operation, the entire surgical area should be covered with cyanoacrylate adhesive and strongly fixed. Make sure not to apply any agent to the region connecting the electrode and ferrules. Please click here to view a larger version of this figure.
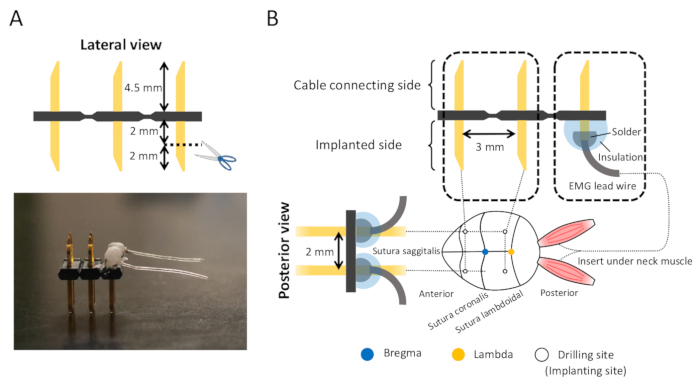
Figure 2: Custom EEG/EMG electrode and electrode pins insertion sites. (A) Top: Out of 6 electrode pins, the external two pins are cut down to 2 mm. Bottom: EEG/EMG electrodes. (B) These electrodes and EMG conduction wires are then soldered. The connecting zone should be isolated with any insulation like cyanoacrylate adhesive. Insertion sites of electrodes are relative to the bregma (anteroposterior ± 1.5mm, mediolateral ± 1.0 mm). EMG wires are inserted under the neck muscle with removal of insulation protecting the wire at the insertion site (1 mm). Please click here to view a larger version of this figure.
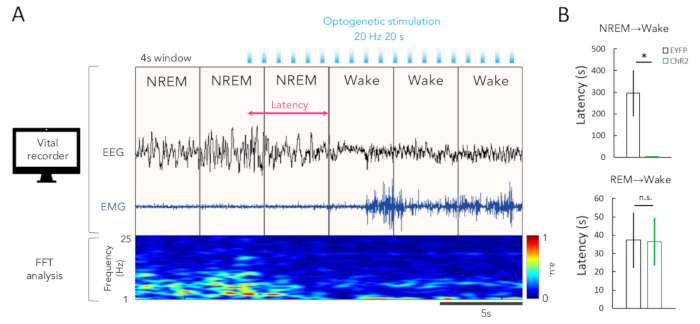
Figure 3: Effect of GABABNST stimulation on state transition in NREM sleep and REM sleep. (A) Representative EEG and EMG wave and EEG power spectrum. Photostimulation (10 ms pulses at 20 Hz for 20 sec) was applied to ChR2-expressing GABABNST neurons following 40 s NREM sleep. Wakefulness was rapidly induced after a 2 s. The EEG showed low voltage and high frequency with EMG bursting. The EEG power spectrogram also showed transition from low to high frequency. (B) Optogenetic excitation of GABABNST neurons showed rapid transition from NREM sleep to wakefulness (upper), but this effect was not seen in the case of applying the same manipulation in REM sleep (bottom). *p < 0.05, Welch's t-test. Please click here to view a larger version of this figure.
Discussion
We here presented a method to evaluate the effect of optogenetic stimulation of neurons with particular chemical identities on state transitions of sleep/wakefulness and gave an example of manipulation of GABABNST neurons. Our data showed that optogenetic excitation of GABABNST neurons results in immediate transition from NREM sleep to wakefulness.
Various experimental designs are available because of the development of numerous types of optogenetic tools. It is possible to activate or inhibit neuronal activity of particular neurons using different kinds of opsins, such as ChR2, SSFO, halorhodopsin, ArchT, and iChloC27. ChR2 can activate neurons a few milliseconds after photo-stimulation and this can be used to evoke action potentials in a phase-lock manner by a pulse generator to examine the acute impact in specific sleep stages. A stably activating opsin such as stable step function opsin (SSFO), which induces depolarization of neurons for 15 to 30 min after stimulation, might also be useful for some kinds of experiments designed to observe a semi-chronic effect28. Depolarized cells with SSFO might become more sensitive to various physiological neuronal input and be deactivated by applying long wavelength light. Furthermore, we can activate axons by implantation of optic fibers at the site of an axonal projection. Fiber stimulation could provide information on the function of a particular axonal projection pathway.
EEG/EMG recording during optogenetic manipulation is a less invasive method to determine the direct consequences of selective excitation/inhibition of neural circuits on sleep/wakefulness states in mice. With this method, many neuronal populations and neural circuits have been shown to be involved in the regulation of sleep/wakefulness states. Towards further development of this technique, it is possible to implant multiple fibers to manipulate multiple pathways simultaneously, or this could be also used in combination with fiber photometory or miniscopes to monitor neuronal activities.
In conclusion, it is anticipated that optogenetics will accelerate progress in unlocking the mystery of sleep regulation by the brain and the development of innovative therapies for refractory insomnia and other sleep disorders.
Divulgazioni
The authors have nothing to disclose.
Acknowledgements
This study was supported by the Merck Investigator Studies Program (#54843), a KAKENHI Grant-in-Aid for Scientific Research on Innovative Areas, "WillDynamics" (16H06401) (T.S.), and a KAKENHI Grant-in-Aid for Exploratory Research on Innovative Areas (T.S.) (18H02595).
Materials
| 1×1 Fiber-optic Rotary Joints | Doric | FRJ 1×1 FC-FC | for optogenetics |
| 6-pin header | KEL corporation | DSP02-006-431G | |
| 6-pin socket | Hirose | 21602X3GSE | |
| A/D converter | Nippon koden | N/A | Analog to digital converter |
| AAV10-EF1a-DIO-ChR2-EYFP | 3.70×1013(genomic copies/ml) | ||
| AAV10-EF1a-DIO-EYFP | 5.82×1013(genomic copies/ml) | ||
| Ampicillin | Fuji film | 014-23302 | |
| Amplifier | Nippon koden | N/A | for EEG/EMG recording |
| Anesthetic vaporizer | Muromachi | MK-AT-210D | |
| Automatic injecter | KD scientific | 780311 | |
| Carbide cutter | Minitor | B1055 | φ0.7 mm. Reffered as dental drill, used with high speed rotary micromotor |
| Cyanoacrylate adhesion (Aron alpha A) and acceleration | Konishi | #30533 | |
| Dental curing light | 3M | Elipar S10 | |
| Epoxy adhesive | Konishi | #04888 | insulation around the solder of 6-pin and shielded cable |
| Fiber optic patch cord (branching) | Doric | BFP(#)_50/125/900-0.22 | |
| Gad67-Cre mice | provided by Dr. Kenji Sakimura | Cre recombinase gene is knocked-in in the Gad67 allele | |
| Hamilton syringe | Hamilton | 65461-01 | |
| High speed rotary micromotor kit | FOREDOM | K.1070 | Used with carbide cutter |
| Interconnecting sleeve | Thorlab | ADAF1 | φ2.5 mm Ceramic |
| Isoflurane | Pfizer | 871119 | |
| Laser | Rapp OptoElectronic | N/A | 473nm wave length |
| Laser intesity checker | COHERENT | 1098293 | |
| Laser stimulator | Bio research center | STO2 | reffered as pulse generator in text |
| Optic fiber with ferrule | Thorlab | FP200URT-CANNULA-SP-JP | |
| pAAV2-rh10 | provided by PennVector Core | ||
| pAAV-EF1a-DIO-EYFP-WPRE-HGHpA | Addgene | plasimid # 20296 | |
| pAAV-EF1a-DIO-hChR2(H134R)-EYFP-WPRE-HGHpA | provided by Dr. Karl Deisseroth | ||
| Patch cord | Doric | D202-9089-0.4 | 0.4m length, laser conductor between laser and rotary joint |
| pHelper | Stratagene | ||
| Photocurable dental cement | 3M | 56846 | |
| Serafin clamp | Stoelting | 52120-43P | |
| Shielded cable | mogami | W2780 | Soldering to 6-pin socket for EEG/EMG recording |
| Sleep recording chamber | N/A | N/A | Custum-made (21cm× 29cm × 19cm) with water tank holder |
| Sleep sign software | KISSEI COMTEC | N/A | for EEG/EMG analysis |
| Slip ring | neuroscience,inc | N/A | for EEG/EMG analysis |
| Stainless screw | Yamazaki | N/A | φ1.0 x 2.0 |
| Stainless wire | Cooner wire | AS633 | 0.0130 inch diameter |
| Stereotaxic frame with digital console | Koph | N/A | Model 940 |
| Syringe needle | Hamilton | 7803-05 | |
| Vital recorder software | KISSEI COMTEC | N/A | for EEG/EMG recording |
Riferimenti
- Spoormaker, V. I., Montgomery, P. Disturbed sleep in post-traumatic stress disorder: Secondary symptom or core feature?. Sleep Medicine Reviews. 12 (3), 169-184 (2008).
- Dworak, M., Wiater, A., Alfer, D., Stephan, E., Hollmann, W., Struder, H. K. Increased slow wave sleep and reduced stage 2 sleep in children depending on exercise intensity. Sleep Medicine. 9 (3), 266-272 (2008).
- Mellman, T. A. Sleep and anxiety disorders. Psychiatric Clinics of North America. 29 (4), 1047-1058 (2006).
- Scammell, T. E., Arrigoni, E., Lipton, J. O. Neural circuitry of wakefulness and sleep. Neuron. 93 (4), 747-765 (2017).
- Chemelli, R. M., et al. Narcolepsy in orexin knockout mice: Molecular genetics of sleep regulation. Cell. 98 (4), 437-451 (1999).
- Borbély, A. A., Daan, S., Wirz-Justice, A., Deboer, T. The two-process model of sleep regulation: A reappraisal. Journal of Sleep Research. 25 (2), 131-143 (2016).
- Daan, S., Beersma, D. G., Borbely, A. A. Timing of human sleep: recovery process gated by a circadian pacemaker. American Journal of Physiology-Regulatory, Integrative and Comparative Physiology. 246 (2), R161-R183 (1984).
- Saper, C. B., Cano, G., Scammell, T. E. Homeostatic, circadian, and emotional regulation of sleep. Journal of Comparative Neurology. 493 (1), 92-98 (2005).
- Saper, C. B., Fuller, P. M., Pedersen, N. P., Lu, J., Scammell, T. E. Sleep state switching. Neuron. 68 (6), 1023-1042 (2010).
- LeDoux, J. E. Emotion circuits in the brain. Annual Review of Neuroscience. 23, 155-184 (2000).
- Tovote, P., Fadok, J. P., Lüthi, A. Neuronal circuits for fear and anxiety. Nature Reviews Neuroscience. 16 (6), 317-331 (2015).
- Lebow, M. A., Chen, A. Overshadowed by the amygdala: the bed nucleus of the stria terminalis emerges as key to psychiatric disorders. Molecular Psychiatry. 21 (4), 450-463 (2016).
- Wu, S., et al. Tangential migration and proliferation of intermediate progenitors of GABAergic neurons in the mouse telencephalon. Development. 138 (12), 2499-2509 (2011).
- Tye, K. M., Deisseroth, K. Optogenetic investigation of neural circuits underlying brain disease in animal models. Nature Reviews Neuroscience. 13 (4), 251-266 (2012).
- de Lecea, L., Carter, M. E., Adamantidis, A. Shining light on wakefulness and arousal. Biological Psychiatry. 71 (12), 1046-1052 (2012).
- Carter, M. E., Brill, J., Bonnavion, P., Huguenard, J. R., Huerta, R., de Lecea, L. Mechanism for hypocretin-mediated sleep-to-wake transitions. Proceedings of the National Academy of Sciences of the United States of America. 109 (39), E2635-E2644 (2012).
- Weber, F., Dan, Y. Circuit-based interrogation of sleep control. Nature Publishing Group. 538, 51-59 (2016).
- Weber, F., Chung, S., Beier, K. T., Xu, M., Luo, L., Dan, Y. Control of REM sleep by ventral medulla GABAergic neurons. Nature. 526, 435-438 (2015).
- Oishi, Y., et al. Slow-wave sleep is controlled by a subset of nucleus accumbens core neurons in mice. Nature Communications. 8 (1), 1-12 (2017).
- Boyden, E. S., Zhang, F., Bamberg, E., Nagel, G., Deisseroth, K. Millisecond-timescale, genetically targeted optical control of neural activity. Nature Neuroscience. 8 (9), 1263-1268 (2005).
- Han, X., et al. A high-light sensitivity optical neural silencer: development and application to optogenetic control of non-human primate cortex. Frontiers in Systems Neuroscience. 5, 1-8 (2011).
- Kim, C. K., Adhikari, A., Deisseroth, K. Integration of optogenetics with complementary methodologies in systems neuroscience. Nature Reviews Neuroscience. 18 (4), 222-235 (2017).
- Saito, Y. C., et al. GABAergic neurons in the preoptic area send direct inhibitory projections to orexin neurons. Frontiers in Neural Circuits. 7 (December), 1-3 (2013).
- Atasoy, D., Aponte, Y., Su, H. H., Sternson, S. M. A FLEX switch targets Channelrhodopsin-2 to multiple cell types for imaging and long-range circuit mapping. Journal of Neuroscience. 28 (28), 7025-7030 (2008).
- Kodani, S., Soya, S., Sakurai, T. Excitation of GABAergic neurons in the bed nucleus of the stria terminalis triggers immediate transition from non-rapid eye movement sleep to wakefulness in mice. Journal of Neuroscience. 37, 7174-7176 (2017).
- Lin, F., Pichard, J. . Handbook of practical immunohistochemistry: frequently asked questions. , (2011).
- Wiegert, J. S., Mahn, M., Prigge, M., Printz, Y., Yizhar, O. Silencing neurons: tools, applications, and experimental constraints. Neuron. 95 (3), 504-529 (2017).
- Yizhar, O., Fenno, L. E., Prigge, M., Schneider, F., Davidson, T. J., O’Shea, D. J., Sohal, V. S., Goshen, I., Finkelstein, J., Paz, J. T., Stehfest, K., Fudim, R., Ramakrishnan, C., Huguenard, J. R., Hegemann, P., Deisseroth, K. Neocortical excitation/inhibition balance in information processing and social dysfunction. Nature. 40 (6), 1301-1315 (2012).

