Development of a Novel Task-oriented Rehabilitation Program using a Bimanual Exoskeleton Robotic Hand
Summary
This study reports the development of a novel robot-assisted task-oriented program for hand rehabilitation. The developmental process consists of experiments using both healthy subjects and subjects who have had a stroke and suffered from subsequent motor control dysfunction.
Abstract
A robot-assisted hand is used for the rehabilitation of patients with impaired upper limb function, particularly for stroke patients with a loss of motor control. However, it is unclear how conventional occupational training strategies can be applied to the use of rehabilitation robots. Novel robotic technologies and occupational therapy concepts are used to develop a protocol that allows patients with impaired upper limb function to grasp objects using their affected hand through a variety of pinching and grasping functions. To conduct this appropriately, we used five types of objects: a peg, a rectangular cube, a cube, a ball, and a cylindrical bar. We also equipped the patients with a robotic hand, the Mirror Hand, an exoskeleton hand that is fitted to the subject’s affected hand and follows the movement of the sensor glove fitted to their unaffected hand (bimanual movement training (BMT)). This study had two stages. Three healthy subjects were first recruited to test the feasibility and acceptability of the training program. Three patients with hand dysfunction caused by stroke were then recruited to confirm the feasibility and acceptability of the training program, which was conducted on 3 consecutive days. On each day, the patient was monitored during 5 min of movement in a passive range of motion, 5 min of robot-assisted bimanual movement, and task-oriented training using the five objects. The results showed that both healthy subjects and subjects who had suffered a stroke in conjunction with the robotic hand could successfully grasp the objects. Both healthy subjects and those who had suffered a stroke performed well with the robot-assisted task-oriented training program in terms of feasibility and acceptability.
Introduction
Most (80%) stroke patients experience a deficit in the hand and have difficulty in independently performing manual tasks that are pertinent to daily living1. However, the complex nature of manual tasks means that it is a significant challenge to design a task-oriented training program for hand rehabilitation2. In recent years, many robotic devices have been developed for hand rehabilitation3,4, but few training protocols assisted by robotic devices allow a patient to interact with real objects. It is unclear exactly how a task-oriented training program for hand function rehabilitation can be applied using robotic devices for patients who experience hand dysfunction due to stroke.
Task-oriented training is used to improve hand function5,6 and is commonly applied in the rehabilitation for upper limb dysfunction due to stroke. It is used to increase neuroplasticity and is highly dependent on individual neurological deficits and functional demands7. However, during task-oriented training, patients experience difficultly in manipulating objects if hand function is impaired. Examples of this include poor grasp or limited pinch functions. Therapists also show difficulty in guiding patients’ finger movements individually, which therefore limits the variation of grasping tasks. Robotic devices are thus necessary to increase the effectiveness of task-oriented training by explicitly guiding hand movement during repetitive training2,8.
Previous studies only used rehabilitation robots for task-oriented training on upper-limb reaching tasks3. It is unclear how robot-assisted rehabilitation can be employed for task-oriented training targeting at hand function. An exoskeleton hand, HWARD, has been used to guide the fingers to grasp and release objects8. However, this device does not allow varied grasping patterns because it lacks the necessary degrees of freedom. Recently, other devices that target moving a patient’s fingers individually have been developed9. However, these devices have not previously been used for neurorehabilitation. The robotic devices mentioned above are all unilateral robots. In contrast, the robotic hand system presented here needs the cooperation of unaffected and affected hands. The robotic hand system is specifically designed for rehabilitation purposes using the master–slave mechanism to achieve symmetric bimanual hand movements. The system consists of an exoskeleton hand (worn on the affected hand), a control box, and a sensory glove (worn on the unaffected hand). Each finger module of the exoskeleton hand is driven by a motor with one degree of freedom and its joints are linked using a mechanical linkage system. Two sizes, S and M, are designed to fit different subjects. The control box provides two therapeutic modes, the passive range of motion (PROM) and mirror-guided motion modes, through which the patient’s affected hand can be manipulated by the exoskeleton hand. In the PROM mode, the control box sends input commands to the exoskeleton while moves the subject’s hand to perform full finger flexion/extension. It contains two modes: single-finger mode (acts in sequence from thumb to little finger) and five fingers mode (five fingers move together). In the mirror-guided motion mode, the master (sensor glove)–slave (exoskeleton hand) mechanism is implemented, in which the movement of each finger is detected by the sensor glove and signals of the joint angles are transmitted to the control box to manipulate the exoskeleton hand.
When equipped the robotic hand system, the subjects were instructed to move their affected hands under the guidance of the exoskeleton hand controlled by unaffected hands which is bimanual movement training (BMT)10. According to previous research, BMT is able to activate similar neural pathways in both hemispheres of the brain and prevent the trans-hemisphere inhibition that hinders the recovery of neuronal function in the lesion hemisphere10. Brunner et al.11 compared BMT to constraint-induced movement therapy (CIMT) in sub-acute stroke patients. They suggested that BMT tends to activate more neural networks in both hemispheres than CIMT, and there was no significant difference in improvement of hand function between the BMT and CIMT approaches. Sleimen-Malkoun et al.12 also suggested that through BMT, stroke patients are able to re-establish both paretic limb control and bimanual control. That is to say, training should comprise bimanual tasks that focus on using the affected arm. Moreover, the coordination of both hands is necessary for activities of daily living (ADL)11,12. Therefore, it is crucial to develop a bimanual robot-assisted task-oriented training program for post-stroke patients and objects that can be grasped or pinched by patients wearing the robotic hand system.
In this study, a variety of grasping objects were designed based on the needs of occupational therapy and the mechanical properties of rehabilitation robots. A task-oriented training protocol was developed using robotic rehabilitation devices for patients with distal upper limb dysfunction due to stroke. The purpose of this study was to investigate the feasibility, and acceptability of the task-oriented training program using an exoskeleton robot and newly designed grasping objects.
Protocol
The training protocol and informed consent document were reviewed and approved by the Institutional Review Board of the Chang Gung Medical Foundation. The details of the study and the procedures were clearly explained to each subject.
1. Recruitment of three healthy adults
- Perform the screening process using the following inclusion criteria: (1) age 20–60 years, (2) already signed informed consent, (3) normal function in upper limbs, (4) Mini-Mental State Examination (MMSE) score ≧24.
- Conduct Trial 1: manipulating objects without wearing the robotic hand system.
- Instruct the subject to sit upright in a chair with a firm back and no armrests. Seat the subject in front of a table. Stand by the subject’s non-dominant side.
- Teach the subject how to manipulate the designed objects for 5 min. Include a palmar prehension to pick up the peg, a lateral prehension to pick up the rectangular cube, a three-point chuck to pick up the cube, a spherical grasp to pick up the ball, and a cylindrical grasp to pick up the cylindrical bar.
NOTE: The objects are shown in Figure 1A. The experimental setup is shown in Figure 1B. The subjects learned the specific grasp patterns for each object. The grasping pattern is shown in Figure 2. - Place two bases bilaterally in front of the subject’s hands. Place each object used in the rehabilitation on top of these bases to assist manipulation. For all the objects, repeat the following sequences 20 times. Ask the subjects to grasp the objects in the starting area of the base, lift, and move them to the midline and release using their non-dominant hands.
- At the same time, measure the success rate for these 20 attempts. Perform this procedure on 3 consecutive days. The success rate is the number of successful manipulations per 20 attempts x 100%. Successful manipulation is defined as when the subjects are able to complete the sequences with specific grasp pattern according to the objects and without dropping them.
- Conduct Trial 2: manipulating objects using robotic hand system (Figure 3).
NOTE: The mechanisms of the robotic hand system are as follows. In the exoskeleton hand, the joints in each finger module are designed in mechanical linking and driven by an individual linear actuator with a constant speed of 10 mm/s. The exoskeleton has different ranges of motion in each finger module (thumb: MCP= 0° to 55°, DIP= 0° to 70°; index and middle fingers: MCP= -10 ° to 55°, PIP=0° to 35°, DIP=0° to 35°; ring and little fingers: MCP= -5 ° to 55°, PIP= 0° to 35°, DIP= 0° to 35°). In the sensor glove, each finger module is installed with a flex sensor which measures the joint angle and sends input signals to the control box through cables.- Sensor glove setup (Figure 1B,b)
- Put the sensor glove on the subject’s dominant hand. Use the Velcro to secure the wrist.
- Exoskeleton setup (Figure 1B,b)
- Use a clean pad to wrap the non-dominant hand. Fasten the Velcro snugly.
- Loosen the thumb mechanism of the exoskeleton hand to allow adjustment of the thumb-opening angle. Place the non-dominant hand in the exoskeleton hand. Fasten the Velcro to the palm through the fastening ring. Fasten the fingers one by one, beginning with the forefinger and finishing with the thumb.
- Then, fasten the Velcro parallel to the wrist through the fastening ring. Adjust the thumb to a comfortable angle and then tighten the thumb mechanism.
- Control box setup (Figure 1A,c)
- Insert the cables for the exoskeleton hand and sensor glove into the sockets in the exoskeleton hand and sensor glove, respectively. After that, insert the cables for the exoskeleton hand and sensor glove into the socket in the control box. Finally, insert the power cable into the control box and connect it to an outlet with the correct voltage.
- Conduct a warm-up session (The PROM mode)
- Switch on the control box and adjust the mode to Five Fingers. This mode allows the exoskeleton hand to move the subject’s fingers passively. Ask the subject to perform a grasp-and-release task guided by the exoskeleton hand for 2.5 min.
- Switch the mode to Single Finger and let the exoskeleton hand move the subject’s fingers individually and passively. Ask the subject to extend and retract individual fingers for 2.5 min, guided by the exoskeleton hand.
- Conduct a robot-assisted bimanual movement session.
- Switch the mode to Mirror. In this mode, the movement of the dominant hand wearing the sensor glove controls the exoskeleton hand’s movements. Any movement that is made by the sensor glove is mimicked and mirrored by the exoskeleton hand. For example, a flexion of the sensor glove’s index finger corresponds to a flexion of the exoskeleton’s index finger.
- Instruct the subject to perform a grasp-and-release task for 2.5 min and make individual finger movements for a further 2.5 min while wearing the sensor glove. This action is mirrored by the exoskeleton hand, which guides the subject’s non-dominant hand in performing the required tasks.
- Sensor glove setup (Figure 1B,b)
- Conduct the task-oriented session.
- Teach the subject how to manipulate the designed objects using the robotic hand system for 5 min. Include a palmar prehension to pick up the peg, a lateral prehension to pick up the rectangular cube, a three-point chuck to pick up the cube, a spherical grasp to pick up the ball, and a cylindrical grasp to pick up the cylindrical bar.
- Place two bases bilaterally in front of the subject’s hands. Place each object used in the rehabilitation on top of these bases to assist manipulation. For all the objects, repeat the following sequences 20 times. Ask the subjects to grasp the object in the starting area of the base, lift, and move them to the midline and release using the robotic hand system.
- At the same time, measure the success rate for these 20 attempts. Perform this procedure on 3 consecutive days. The success rate is the number of successful manipulations per 20 attempts x 100%. Successful manipulation is defined as when the subjects are able to complete the sequences with specific grasp pattern using the robotic hand system and without dropping them.
NOTE: The success rate will be used to assess the feasibility of the bimanual robotic hand system in healthy subjects.
2. Recruit three stroke patients to determine the applicability of the training program
- Perform the screening process using the following inclusion criteria: (1) age 20–60 years; (2) signed informed consent; (3) diagnosed with unilateral stroke ≧ 1 month (4) Modified Ashworth Scale (MAS) score ≦2; (5) Brunnstrom stage ≦2; (6) MMSE score ≧24.
- Conduct Trial 1: manipulating objects when not using robotic hand system (Figure 2).
- Let the subject sit upright in a chair with a firm back and no armrests. Seat the subject in front of a table. Stand by the subject’s affected side. Place a sling under the subject’s elbow and exoskeleton hand to support his/her affected arm.
- Teach the subject how to manipulate the designed objects for 5 min. Include a palmar prehension to pick up the peg, a lateral prehension to pick up the rectangular cube, a three-point chuck to pick up the cube, a spherical grasp to pick up the ball, and a cylindrical grasp to pick up the cylindrical bar.
- Place two bases bilaterally in front of the subject’s hands. Place each object used in the rehabilitation on top of these bases to assist manipulation. Ask the subject to manipulate the five different objects using his/her affected hand 20 times. Support the subject in moving his/her upper arm if needed.
- At the same time, measure the success rate for these 20 attempts. Perform this procedure on 3 consecutive days.
- Conduct Trial 2: manipulating objects using robotic hand system (Figure 3).
- Fit the exoskeleton hand to the subject’s affected hand and the sensor glove to the unaffected hand. Repeat steps 1.3.1–1.3.3. Place a sling under the subject’s elbow and exoskeleton hand to support his/her affected arm.
- Conduct a warm-up session (The PROM mode).
- Switch on the control box and adjust the mode to Five Fingers. Ask the subject to perform a grasp-and-release task guided by the exoskeleton hand for 2.5 min.
- Switch the mode to Single Finger. Ask the subject to extend and retract individual fingers for 2.5 min, guided by the exoskeleton hand.
- Switch the mode to Mirror. Instruct the subject to perform a grasp-and-release task for 2.5 min and make individual finger movements for a further 2.5 min while wearing the sensor glove. This action is mirrored by the exoskeleton hand, which guides the subject’s affected hand in performing the required tasks.
- Conduct a task-oriented session.
- Teach the subject how to manipulate the designed objects using the robotic hand system for 5 min. Include a palmar prehension to pick up the peg, a lateral prehension to pick up the rectangular cube, a three-point chuck to pick up the cube, a spherical grasp to pick up the ball, and a cylindrical grasp to pick up the cylindrical bar.
- Place two bases bilaterally in front of the subject’s hands. Place each object used in the rehabilitation on top of these bases to assist manipulation. For all the objects, repeat the following sequences 20 times. Ask the subjects to grasp the objects in the starting area of the base, lift, and move them to the midline and release using the robotic hand system.
- At the same time, measure the success rate for these 20 attempts. Perform this procedure on 3 consecutive days. The success rate is the number of successful manipulations per 20 attempts x 100%. Successful manipulation is defined as when the subjects are able to complete the sequences with specific grasp pattern using the robotic hand system and without dropping them.
NOTE: The success rate will be used to assess the feasibility of the robotic hand system in stroke patients.
3. Patient evaluation
- To assess acceptability, ask the subjects following questions at the end of each session: (1) was the robotic hand system helpful for you to manipulate the objects? (2) were there any adverse events happened during or after the training program?
Representative Results
A total of six subjects were enrolled in this study, including three healthy subjects and three post-stroke subjects. The demographic data of both groups are shown in Supplementary Table 1. The average age of the healthy group was 28 (range: 24–30), whereas the average age of the patient group was 49 (40–57). The average assessment scores of the patient group were as follows: (1) MMSE=27 (26–29), (2) FMA=11.3 (6–15), (3) MAS=1, (4) Brunnstrom stage=2.
In Step 1, the subjects in the healthy group (n=3) perfectly manipulated all of the objects with and without the robotic hand system (Supplementary Tables 2–6). The average success rates over the 3 days without the robotic hand, as shown in Figure 4, were as follows: peg=100±0% (mean ± S.D.); rectangular cube=100±0%; cube=100±0%; ball=100±0%, and cylindrical bar=100±0%. The average success rates over the 3 days using the robotic hand, as shown in Figure 4, were as follows: peg=100±0%; rectangular cube=100±0%; cube=100±0%; ball=100±0%, and cylindrical bar=100±0%. The results supported the feasibility of the robotic hand system in the healthy group.
In Step 2, all the patients (n=3) exhibited difficulties in manipulating the objects without the robotic hand system (Supplementary Tables 2–6), showing 0±0% success rates for all objects, but their success rates increased significantly when they used the robotic hand system (Figure 4). Specifically, their success rates were as follows: peg=98.89±1.92%, rectangular cube=97.78±3.84%, cube=97.78±2.55%, ball=99.44±0.96%, and cylindrical bar=100±0%. The success rates when using the robotic hand system in the patients were similar to those in the healthy subjects. The results supported the feasibility of the robotic hand system in stroke patients.
In Step 3, all the patients reported that the robotic hand system was helpful to manipulate objects. In addition, all the subjects completed the procedure in 3 consecutive days without reporting any adverse events. The results supported the acceptability of the training program.
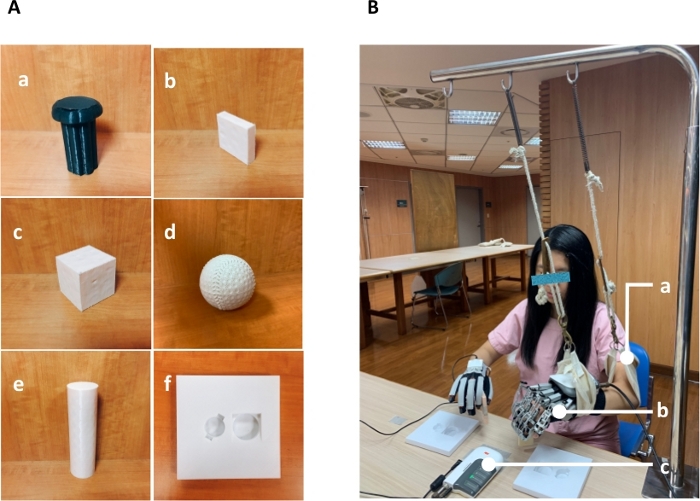
Figure 1: Experimental objects and design.
(A) Designed objects: (a) peg (head: 4.5 cm diameter, body: 3 cm diameter, BRS=3), (b) rectangular cube (1 cm x 4 cm x 4 cm, BRS=4), (c) cube (4 cm3, BRS=4), (d) ball (6 cm diameter, BRS=5), (e) cylindrical bar (4 cm diameter, BRS=5) and (f) base; (B) Experimental setup: (a) Sling, (b) exoskeleton hand, and (c) control box. Please click here to view a larger version of this figure.
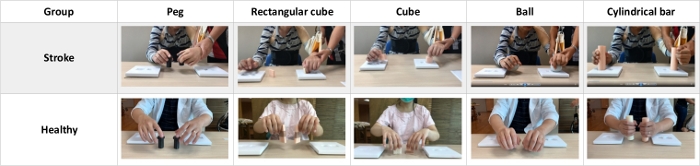
Figure 2: Subjects manipulating objects without using a robotic hand system Please click here to view a larger version of this figure.
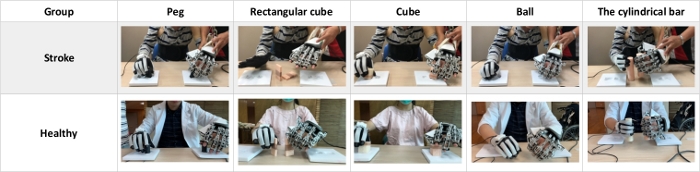
Figure 3: Subjects manipulating objects using a robotic hand system Please click here to view a larger version of this figure.
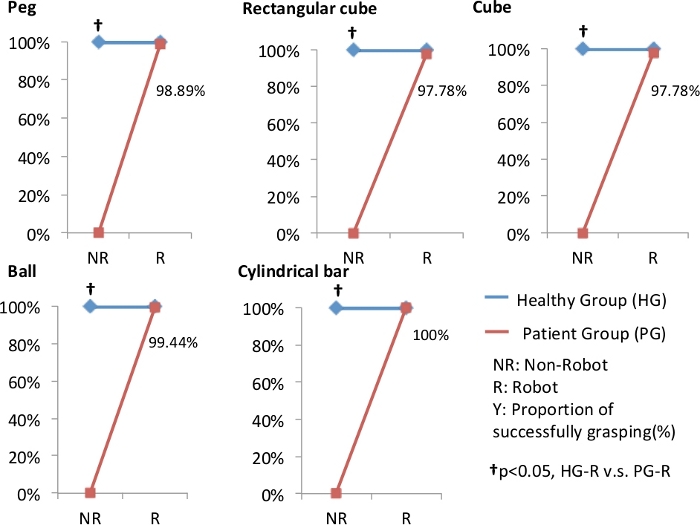
Figure 4: Results of grasping tasks.
The results showed a difference between the healthy and patient groups (Mann-Whitney U test) without using the robot (Non-Robot condition), but the difference was no longer observed with the robot (Robot condition). Please click here to view a larger version of this figure.
Supplemental Table 1. Please click here to download this table.
Supplemental Table 2. Please click here to download this table.
Supplemental Table 3. Please click here to download this table.
Supplemental Table 4. Please click here to download this table.
Supplemental Table 5. Please click here to download this table.
Supplemental Table 6. Please click here to download this table.
Discussion
The results of this study showed the following: (1) both groups could successfully grasp the objects provided with the robotic hand system. They were able to complete this task with a nearly 100% success rate, which verifies the feasibility of the proposed robot-assisted task-oriented training program. (2) There were no reports of injury or adverse events during the study period and all patients reported that the robotic hand system was helpful to manipulate objects. This confirmed the acceptability of the robotic hand system and the training program.
This is the first protocol that uses a bilateral robotic hand system to interact with real objects8,13,14. Everyday activities depending on hand function are complicated15, especially bimanual tasks12, such as putting on pants or wringing a towel. We propose that the training program involving practicing different grasping patterns bimanually will be able to facilitate subjects’ hand function and enhance actual ADL performance. The objects for this study were designed with feasibility, stability, and elasticity in mind. Specifically, the shapes, sizes, and materials of the objects were designed to fit the rigid joint positions of the exoskeleton hand and allow adequate sensory feedback. In addition, each shape was designed to train a different grasp pattern outlined in the “Brunnstrom stage.” It gives therapists a structured system that allows them to grade the difficulty of the task. Moreover, the robotic hand system can be applied to stoke patients who have a severely impaired hand function (i.e., Brunnstrom stage ≤2). They can obtain motor experience and sensory input through the assistance of the exoskeleton robotic hand.
The robotic hand system has several limitations. The movement speed of the exoskeleton hand is fixed and unable to accurately match the movement speed of the sensor glove. This might influence the effects of BMT and limit the variation of training tasks. The small size exoskeleton hand might be too big for some subjects, because it was designed based on a male’s hand. The exoskeleton hand only has one degree of freedom in finger movement and the position of the thumb is fixed, which prohibits three-dimensional movement of the fingers and increases the difficulty of interacting with real-life objects. The weight of the exoskeleton hand is a burden for stroke patients. They showed difficulty reaching out independently with the robotic hand, so a suspension system applied to the arms and forearms is necessary to support the proximal part of the affected upper limbs and assist the hand-training program.
It is important to enhance the symmetry between the sensor glove and exoskeleton hand to achieve truly bimanual-mirrored movements. Extra fixation should be applied to fit smaller hands. A refined version of the exoskeleton hand should be equipped with more adjustable joints to allow the robotic hand to perform multi-dimensional movements and complicated hand training tasks. Furthermore, a portable type of the robotic hand system with the rehabilitation programs remotely planned by therapists may be applied in home-based rehabilitation programs.
There were several limitations in subject inclusion that may affect the generalization of applying the training protocol. This is a pilot study for assessing the feasibility and acceptability of the training program and thus the sample size is very small. The functional characteristics of the stroke patients are quite homogeneous, with MAS = 1, Bunnstrom stage = 2, and FMA score ranging from 6 to 15. These patients have severe motor impairment at their affected hands, so that, following the augmentation using the system, they had a significant improvement in the motor performance as compared with their prior state, a property that may overestimate the effect of our robotic system. In addition, we recruited subjects with lower spasticity for easily guiding the movement of the affected hands by the robotic system, but these devices might not be suitable for patients with strong spasticity. As a feasibility and acceptability study, we did not conduct post-treatment assessments. After this study, we will conduct a randomized controlled trial to characterize the effects of the robotic-assisted task-oriented training program.
This study aimed to develop a novel robot-assisted task-oriented hand rehabilitation program. The protocol created extensively covered the setup and requirements of the procedures while assessing the program’s feasibility and acceptability. The program was concluded to be feasible, acceptable, and safe. The results of the program demonstrated that the training protocol and the objects specifically designed for robot-assisted rehabilitation are suitable for neurorehabilitation for stroke patients. In order to verify these findings, a randomized controlled trial is necessary to determine the therapeutic effect of the training program.
Divulgazioni
The authors have nothing to disclose.
Acknowledgements
This project was supported by Chang Gung Medical Foundation with grant BMRP390021 and the Ministry of Science and Technology with grants MOST 107-2218-E-182A-001 and 108-2218-E-182A-001.
Materials
| Control Box | Rehabotics Medical Technology Corporation | HB01 | The control box includes a power supply, sensor glove signal receiver, motor signal transmitter, and exoskeletal hand motion mode selection unit. |
| Exoskeletal Hand | Rehabotics Medical Technology Corporation | HS01 | It is a wearable device causing the patient's fingers to move and is driven by an external motor and mechanical assembly. |
| Sensor Glove | Rehabotics Medical Technology Corporation | HM01 | Worn on the patient's unaffected side hand. The sensors in the sensor glove will detect flexing and extension of the hand, and this data will be used to control the exoskeletal hand when in bimanual mode. |
Riferimenti
- Hung, C. S., et al. The effects of combination of robot-assisted therapy with task-specific or impairment-oriented training on motor function and quality of life in chronic stroke. PM & R: The Journal of Injury, Function, and Rehabilitation. 8 (8), 721-729 (2016).
- SangWook, L., Landers, K. A., Hyung-Soon, P. Development of a biomimetic hand exotendon device (BiomHED) for restoration of functional hand movement post-stroke. IEEE Transactions on Neural Systems and Rehabilitation Engineering. 22 (4), 886-898 (2014).
- Johnson, M. J., Wisneski, K. J., Anderson, J., Nathan, D., Smith, R. O. Development of ADLER: The Activities of Daily Living Exercise Robot. Proceedings of IEEE/RAS-EMBS International Conference. , (2006).
- Pignolo, L. Robotics in neuro-rehabilitation. Journal of Rehabilitation Medicine. 41 (12), 955-960 (2009).
- Timmermans, A. A., Spooren, A. I., Kingma, H., Seelen, H. A. Influence of task-oriented training content on skilled arm-hand performance in stroke: a systematic review. Neurorehabilitation and Neural Repair. 24 (9), 858-870 (2010).
- Schweighofer, N., Choi, Y., Winstein, C., Gordon, J. Task-oriented rehabilitation robotics. American Journal of Physical Medicine & Rehabilitation. 91, 270-279 (2012).
- Almhdawi, K. A., Mathiowetz, V. G., White, M., delMas, R. C. Efficacy of occupational therapy task-oriented approach in upper extremity post-stroke rehabilitation. Occupational Therapy International. 23 (4), 444-456 (2016).
- Takahashi, C. D., Der-Yeghiaian, L., Le, V. H., Cramer, S. C. A robotic device for hand motor therapy after stroke. Proceedings of 9th International Conference on Rehabilitation Robotics. , (2005).
- Villafañe, J. H., et al. Efficacy of short-term robot-assisted rehabilitation in patients with hand paralysis after stroke: a randomized clinical trial. Hand (NY). 13 (1), 95-102 (2018).
- Cauraugh, J. H., Lodha, N., Naik, S. K., Summers, J. J. Bilateral movement training and stroke motor recovery progress: a structured review and meta-analysis. Human Movement Science. 29 (5), 853-870 (2010).
- Brunner, I. C., Skouen, J. S., Strand, L. I. Is modified constraint-induced movement therapy more effective than bimanual training in improving arm motor function in the subacute phase post stroke? A randomized controlled trial. Clinical Rehabilitation. 26 (12), 1078-1086 (2012).
- Sleimen-Malkoun, R., Temprado, J. J., Thefenne, L., Berton, E. Bimanual training in stroke: how do coupling and symmetry-breaking matter. BMC Neurology. 11, 11 (2011).
- Yue, Z., Zhang, X., Wang, J. Hand rehabilitation robotics on poststroke motor recovery. Behavioural Neurology. 2017, 1-20 (2017).
- Dovat, L., et al. HandCARE: a cable-actuated rehabilitation system to train hand function after stroke. IEEE Transactions on Neural Systems and Rehabilitation Engineering. 16 (6), 582-591 (2008).
- Yoo, C., Park, J. Impact of task-oriented training on hand function and activities of daily living after stroke. Journal of Physical Therapy Science. 27 (8), 2529-2531 (2015).

