A Rapid, Simple, and Standardized Homogenization Method to Prepare Antigen/Adjuvant Emulsions for Inducing Experimental Autoimmune Encephalomyelitis
Summary
To induce experimental autoimmune encephalomyelitis, an animal model of multiple sclerosis, mice are immunized with a water-in-oil emulsion containing an autoantigen and complete Freund’s adjuvant. While several protocols exist for the preparation of these emulsions, a rapid, simple, and standardized homogenization protocol for emulsion preparation is presented here.
Abstract
Experimental autoimmune encephalomyelitis (EAE) shares similar immunological and clinical features with multiple sclerosis (MS), and is therefore widely used as a model to identify new drug targets for better patient treatment. MS is characterized by several different disease courses: relapsing-remitting MS (RRMS), primary progressive MS (PPMS), secondary progressive MS (SPMS), and a rare progressive-relapsing form of MS (PRMS). Although animal models do not accurately mimic all of these contrasting human disease phenotypes, there are EAE models that reflect some of the different clinical manifestations of MS. For example, myelin oligodendrocyte glycoprotein (MOG)-induced EAE in C57BL/6J mice mimics human PPMS, while myelin proteolipid protein (PLP)-induced EAE in SJL/J mice resembles RRMS. Other autoantigens, such as myelin basic protein (MBP), and a number of different mouse strains are also used to study EAE. To induce disease in these autoantigen-immunization EAE models, a water-in-oil emulsion is prepared and injected subcutaneously. The majority of EAE models also require an injection of pertussis toxin for the disease to develop. For consistent and reproducible EAE induction, a detailed protocol to prepare the reagents to produce antigen/adjuvant emulsions is necessary. The method described here takes advantage of a standardized method to generate water-in-oil emulsions. It is simple and fast and uses a shaking homogenizer instead of syringes to prepare quality-controlled emulsions.
Introduction
A breakdown of immunological tolerance can result in the generation of autoimmune disorders, such as multiple sclerosis (MS). It is estimated that 2.8 million people are living with MS worldwide1. Although the exact cause of MS is still largely unknown, dysregulation of autoreactive T and B cells, as well as defects in Treg function, play important roles in the pathogenesis of the disease2,3.
Animal models of autoimmune diseases are essential tools to investigate potential therapeutic modalities. The experimental autoimmune encephalomyelitis (EAE) model has been used for almost a century by researchers interested in MS4. In early experiments, the incidence of the disease was relatively low. The introduction of complete Freund's adjuvant (CFA), containing Mycobacterium and pertussis toxin, enabled the consistent induction of EAE in mice4. Most importantly, it is necessary to mix CFA with a central nervous system (CNS)-specific antigen to generate a homogenous water-in-oil emulsion for inducing EAE. The most common currently available EAE models are based on the active immunization of mice with encephalitogenic peptides. The genetic background of the mice plays an important role in disease susceptibility, with myelin oligodendrocyte glycoprotein (MOG35-55) and myelin proteolipid protein (PLP139-151) peptides used to induce EAE in C57BL/6J and SJL mice, respectively5. However, other mouse strains and CNS-derived peptides can also be used.
The quality of the CFA/peptide emulsion is a critical factor that determines disease penetrance in the active immunization EAE model6. A homogeneous water-in-oil emulsion must be prepared by mixing the encephalitogenic peptides dissolved in aqueous buffer with CFA, otherwise animals will not develop the disease. Numerous protocols have been published on the preparation of CFA/peptide emulsions. Examples include the use of a vortex7, sonication8, syringes and a three-way T connector9, or one syringe only5. However, all these methods are difficult to standardize and are often associated with lengthy and complicated protocols.
Compared to all the above methods, the simple method described here for emulsion preparation offers the advantages of having no person-to-person differences and being relatively fast. The emulsion is generated by a homogenizer shaking the reagents with a set speed, time, and temperature, ensuring fast and consistent results. In addition to inducing disease in the EAE model, this method can also be used to study other autoimmune disease models such as collagen-induced arthritis (CIA) and antigen induced arthritis (AIA)6. Therefore, it is anticipated that this method can be used to consistently induce disease in other animal models that depend on water-in-oil emulsions with autoantigens, such as experimental autoimmune neuritis (EAN)10, experimental autoimmune thyroiditis (EAT)11, autoimmune uveitis (EAU)12, and myasthenia gravis (MG)13. This method also induces general immune responses such as delayed-type hypersensitivity (DTH) consistently6, and could therefore be used for delivering cancer and malaria vaccines (see discussion).
Thus, a rapid (total preparation time ~30 min), simple (all reagents can be prepared in advance and stored), and standardized (the emulsion is accomplished using a shaking homogenizer) method has been developed and is presented here. The CFA/antigen emulsions prepared using this protocol consistently induce disease in autoimmune animal models.
Protocol
All animal procedures were performed according to the practices of the Swedish Board of Animal Research and were approved by the Animal Ethics Committee, Lund-Malmö, Sweden (Permit number: M126-16).
NOTE: A schematic flow of the method is described in Figure 1.
1. Material preparation
NOTE: Prepare all the reagents aseptically in a sterile hood, and aliquot and store at the indicated temperature. The reagents can be stored up to 2 years without losing their effect.
- Prepare CFA containing 20 mg/mL Mycobacterium tuberculosis as described below.
- Add 100 mg of freeze-dried M. tuberculosis H37RA (see Table of Materials) and five 3.2 mm steel beads to a 7 mL tube (see Table of Materials). Shake the tube in a homogenizer (see Table of Materials) for 60 s at the highest speed setting (5,000 rpm).
- Add 5 mL of incomplete Freund's adjuvant (IFA) to the tube and shake again for 60 s at the highest speed. Transfer the slurry of homogenized M. tuberculosis in IFA (now named CFA) to a fresh tube with a pipette, leaving the beads behind, and store at 4 °C until use.
- Add ultrapure water to the freeze-dried powder of MOG35-55 peptide (see Table of Materials) to obtain a final peptide concentration of 10 mg/mL. Sterilize the solution by passing it through a 0.2 µm filter. Prepare 60 µL aliquots and store at -20 °C until use.
NOTE: The MOG35-55 peptide used for this experiment is of ImmunoGrade purity (~70%), is TFA-cleaved, dissolves easily in water, and contains a C-terminal amide (-NH2) to increase in vivo stability14. Peptide aliquots were never thawed and re-frozen more than twice, and were stored at -20 °C until use. - Prepare 100 mL of pertussis toxin buffer: Dissolve 2.9 g of NaCl in 80 mL of 1x Ca2+/Mg2+ free PBS and add 100 µL of 10% Triton X-100. Adjust the volume to 100 mL with PBS and sterilize the solution by passing it through a 0.2 µm filter. Prepare 10 mL aliquots and store at 4 °C until use.
2. Preparation of CFA/peptide emulsions
- Calculate the amount of emulsion needed for immunization. In this standard protocol, each mouse receives 50 µg of MOG35-55 peptide and 300 µg of M. tuberculosis dispersed in Freund's adjuvant (CFA). The amount of each reagent (MOG35-55 peptide, PBS, CFA, and IFA) required for preparing the emulsions can be calculated using Supplemental File 1. An additional 20% of all reagents, to compensate for the small loss of emulsion, is included in the calculation.
NOTE: The commercial emulsion kit (see Table of Materials) used in this study comprises a tube, screw cap, and a plunger in a sterilized pouch. Each tube of the emulsion kit holds a maximum of 9.6 mL, making it possible to prepare 8 x 1 mL syringes sufficient for immunizing 40 mice (or 80 mice if using 100 µL of emulsion per animal). - Place the screw capped tube (from the commercial emulsion kit) and reagents to be used on ice.
- Add the emulsion components in the following order in the volumes calculated in step 2.1: PBS, then the peptide, then M. tuberculosis in CFA, and finally IFA.
- Close the tube with the cap firmly by tightening and loosening it several times. Shake the tube vigorously for 5-10 s by hand to pre-mix the reagents.
- Place the tube in the shaking homogenizer and secure it with the rod. Set the speed to the highest setting and the time to 60 s. Once the run is finished, place the tube on ice for 3 min. Repeat the run one or two more times with the same settings.
- Centrifuge the tube at 300 x g for 1 min to remove trapped air and compact the emulsion.
- Remove the cap from the tube, insert the plunger into the tube, and push it down slowly until it reaches the top of the emulsion. Remove the snap off closure at the bottom of the tube by twisting it.
- Remove the plunger from an injection syringe (1 mL; see Table of Materials). Add a needle (preferably 25-27 G) to the injection syringe.
- Attach the back end of the injection syringe to the dedicated lock at the bottom of the tube and lock it with a short twist.
- Transfer the emulsion from the tube to the injection syringe by pushing the plunger gently. Stop when the emulsion reaches the 0.15 mL graduation of the injection syringe.
- Separate the injection syringe from the tube and insert the plunger carefully, taking care that no air enters the syringe. Push the plunger until the emulsion comes out of the needle.
NOTE: At this point, some of the emulsion can be used for quality control (see step 3). - Repeat steps 2.8-2.11 for the rest of the emulsion present in the tube.
NOTE: To minimize the waste of expensive CFA/antigen emulsions, 1 mL syringes should be used. Other syringes that fit the dedicated lock at the bottom of the tube may be used; however, a larger volume of emulsion may need to be prepared. The CFA/MOG35-55 peptide emulsion can be stored at 4 °C for up to 15 weeks without losing its EAE-inducing capacity.
3. Quality control of emulsion
- Drop-test: Add a small drop of the emulsion into a sterile 50 mL conical tube filled with 20 mL of cold water. Close the tube and shake it by hand for a couple of seconds. The appearance of tiny distinct droplets confirms the formation of a water-in-oil emulsion.
- Examine the emulsion using phase contrast microscopy.
- To analyze the size of the water-in-oil particles, add a tiny drop (2-3 µL) of the emulsion to a microscope slide, smear it out with a cover slip, and then push hard in a circular motion to flatten out the emulsion.
- Examine the smeared emulsion under a phase contrast microscope (see Table of Materials) with 400x magnification and focus on a field with a monolayer of the emulsion. Ensure that small uniform grey/white particles are visible (Figure 2A).
- Analyze the emulsion particle size using laser diffraction.
NOTE: Laser diffraction measures particle size distributions using a laser beam. This is the ultimate quality control test for emulsions. A representative result of particle size distributions using the method described here is shown in Figure 2B (for a detailed description, see Topping et al.6). Nevertheless, the drop test and microscope examination are sufficient to validate whether a satisfactory emulsion has been formed.- Set the refractive indices for both red and blue lasers for the dispersant (see Table of Materials) to 1.456 and for the sample to 1.33 on the particle size analyzer (see Table of Materials). Set the absorbance of the refractive index to 0.02.
- Add one drop from the syringe containing the peptide emulsion to the dispersion unit containing light mineral oil. Start the data acquisition instantly after dispersion of the emulsion.
NOTE: A general-purpose model was applied, and spherical particles were assumed, for the estimation of particle size distribution.
4. EAE induction using the MOG 35-55 peptide emulsion in C57BL6/J mice
NOTE: In all experiments, five 8-12-week-old female C57BL6/J mice were used.
- Prior to immunization, anesthetize the mice using 2.5% vaporized isoflurane and confirm using a firm toe pinch.
- Inject each mouse subcutaneously using 1 mL syringes into two different sites, on the right and left sides of the hind flank with 200 µL of emulsion containing 50 µg of MOG35-55 peptide in a 1:1 (v/v) ratio of peptide/CFA.
- At least 1.5 h after the immunization with the emulsion, and then again after 24 h, administer a total of 80 ng of Bordetella pertussis toxin in 200 µL of pertussis toxin buffer to each mouse, through intraperitoneal injections (100 µL on the left and 100 µL on the right site of the belly).
NOTE: Precise localization of intraperitoneal injection with pertussis toxin has been shown to be essential for the activation of T cells in the draining lymph node15. - Optional: Inject MOG35-55 peptide again on day 7 (as used in some protocols16) by repeating step 4.2.
NOTE: Most importantly, make sure that the syringes and needles used for immunization containing MOG/CFA or pertussis toxin are adequately disposed of in biohazard bags/containers. - Evaluate the clinical score daily, using a scale from 0-6 as previously described6.
Representative Results
The rapid, simple, and standardized protocol for the preparation of CFA/MOG emulsions is depicted in Figure 1. This method has recently been described elsewhere6. The CFA/MOG emulsions can also be prepared with other methods, such as the traditional syringe method or by vortexing. These methods were compared here by assessing the quality of the emulsions. All the methods produced water-in-oil emulsions; the homogeneity and quality of these emulsions were assessed by adding a small drop onto a glass-slide followed by observation under a phase-contrast microscope. Emulsions produced by the shaking homogenization method displayed grey/white bean-shaped particles, representing tiny droplets of water-in-oil emulsions. In contrast, the emulsion droplets produced using the syringe method were larger and whiter. In the vortex method, large grey/black particles were observed, corresponding to air-bubbles trapped in the emulsion (Figure 2A).
To test the long-term stability of water-in-oil emulsions, the changes in particle size distribution over time can be measured using a laser diffraction particle size analyzer. Emulsions prepared with the standardized protocol described here did not show any change in particle size over a period of 6 weeks (Figure 2B). Therefore, the possibility that emulsions containing the MOG35-55 peptide can be stored at 4 °C for an extended period of time and still induce disease was tested. Emulsions containing the CFA/MOG35-55 peptide were prepared with this method and used immediately or stored at 4 °C for 3 or 15 weeks (Figure 3A). Mice were injected with 50 µg of MOG35-55 peptide and scored for clinical signs of disease as described in the protocol. Remarkably, the fresh, 3-week-old, and 15-week-old emulsions all induced similar EAE disease in all animals tested throughout the experiment (Figure 3A). Thus, these results revealed that emulsions containing MOG35-55 peptides prepared using the shaking homogenization method can be stored for at least 15 weeks and still induce EAE with disease scores comparable to those achieved with freshly prepared emulsions.
To simplify and speed up the setup of the experiments and to avoid lot-to-lot difference of reagents, all necessary components were prepared, aliquoted, and stored at the appropriate temperature in advance. Then, five experiments were performed over a period of 6 months. C57BL6/J mice were immunized with the MOG/CFA emulsions prepared on the day of immunization, using emulsion kits, and evaluated for clinical symptoms. Mice developed a similar disease pattern in all experiments (Figure 3B), revealing that the homogenization method presented here produced emulsions that induced EAE in a consistent and reproducible manner.
The total preparation time, from retrieving all reagents, adding them and shaking the tube three times, and loading the syringes with the emulsion, ready for immunization, takes no more than 30 min. In addition, only 20% of extra emulsion has to be prepared. This is in stark contrast to other protocols, where the preparation time can be up to 1.5-2 h and 50%-100% of extra emulsion may need to be prepared to ensure sufficient material for immunization16.
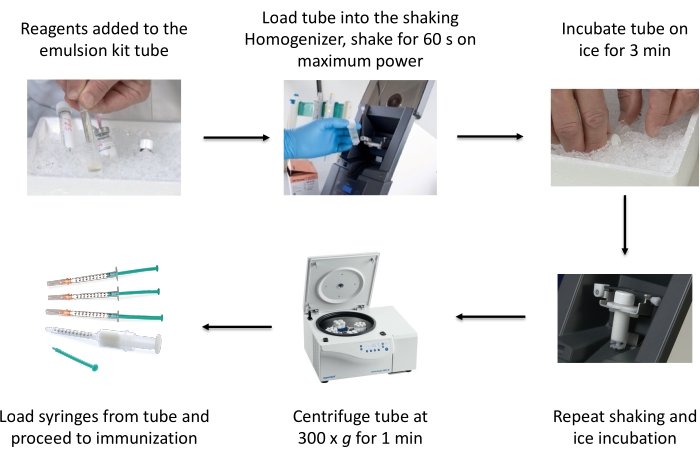
Figure 1: Schematic of the process of emulsion preparation using a commercial emulsion kit. This figure has been reused from Topping et al6 with permission. Please click here to view a larger version of this figure.
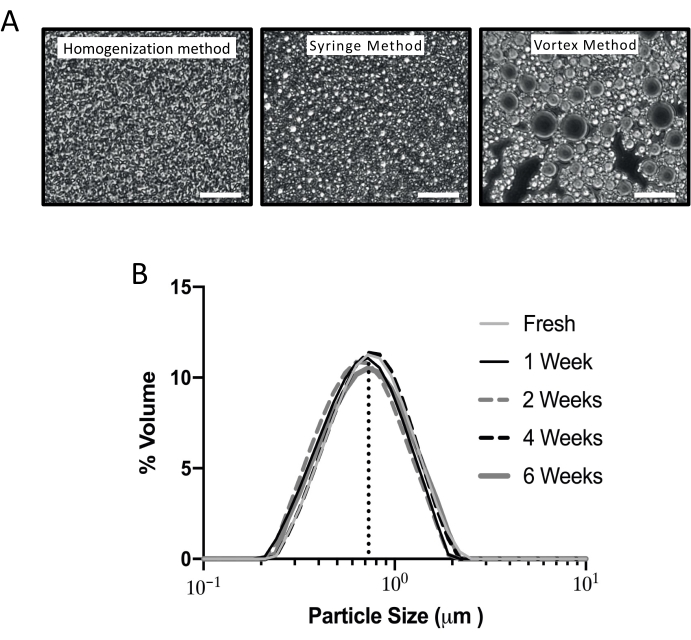
Figure 2: Characterization of emulsions produced using different methods. (A) Representative images from three different preparation methods: standard homogenization method, traditional syringe method, and vortex method. A small amount of emulsion was placed on a glass slide and observed under a phase contrast microscope (400x). Scale bar = 50 µm. A representative preparation is shown of each method from >15 experiments. The average D [4, 3] (the volume weighted mean) was measured with a particle size analyzer to be 0.7 µm for the shaking homogenization method, 1.4 µm for the syringe method, and 5.4 µm for the vortex method. (B) Stability of the emulsion over time was measured using the particle size analyzer. An emulsion of CFA/PBS was prepared with the shaking homogenizer and the emulsion kit, and the particle size determined, using laser diffraction over time. One sample was analyzed immediately and then the emulsions were stored at 4 °C. These samples were analyzed 1, 2, 4, and 6 weeks after preparation. The average D [4, 3] volume weighted mean for all samples was 0.73 µm ± 0.03 µm (SD). This figure has been reused from Topping et al6 with permission. Please click here to view a larger version of this figure.
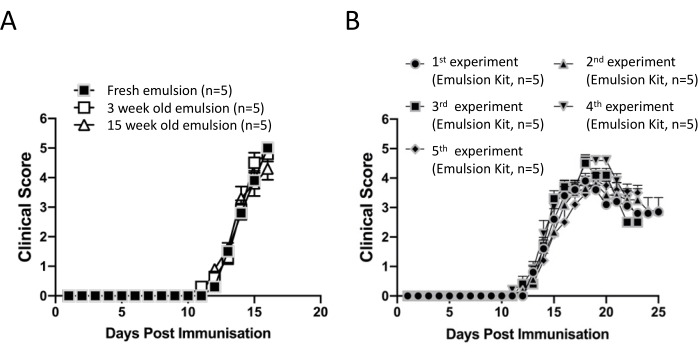
Figure 3: EAE induction in mice immunized with a MOG35-55 peptide/CFA preparation using a commercial emulsion kit. (A) EAE induction of the stored emulsion. Emulsions containing CFA and 50 µg of MOG35-55 peptide/mouse were prepared with the homogenization method and stored at 4 °C for 3 or 15 weeks. The freshly prepared and the stored emulsions were injected on the same day into C57BL/6J mice (n = 5 per group). The mice received 80 ng of pertussis toxin on the same day and 24 h later, and were scored for signs of disease using clinical scores from 0-6. (B) Consistent induction of EAE with the emulsions prepared using the homogenization method. Emulsions containing CFA and 50 µg of MOG35-55 peptide/mouse were prepared at different time points and injected into C57BL/6J mice (n = 5 per group). The mice received 80 ng of pertussis toxin on the same day and 24 h later, and were scored for signs of disease. This figure has been reused from Topping et al6 with permission. Please click here to view a larger version of this figure.
Supplemental File 1: Calculation of the amount of each reagent (MOG35-55 peptide, PBS, CFA, and IFA) for emulsion preparation. Please click here to download this File.
Discussion
Water-in-oil emulsions, such as antigen/Freund's adjuvant, have been used for more than half a century to induce EAE17. There is currently no standardized method to prepare antigen emulsions that is independent of human influence. Manual mixing using syringes is standard for most laboratories, however this method is time consuming, often results in an excessive loss of material, and the quality differs depending on the scientist preparing it.
The method presented in this manuscript uses a standard shaking homogenization machine to prepare the antigen/CFA emulsions. In addition, all reagents used here can be aliquoted and stored for a long period of time, making it convenient and fast to prepare emulsions. The total time for preparing emulsions for up to 80 mice is approximately 30 min. This is in stark contrast to other published methods, which require 1-1.5 h for preparing MOG35-55 emulsions16,18. Other manual methods, such as the one syringe method, are often associated with the introduction of air bubbles within the syringes5. The method presented here has been designed so that the emulsion is pushed into syringes from their back end, which eliminates the introduction of air bubbles and minimizes the loss of material.
To ensure consistent results and minimal waste of emulsion, there are some critical steps in the shaking homogenization method that require specific attention. The tube and reagents should be placed on ice before starting the experiment and after the homogenization step. The PBS and antigen should be added to the tube first, followed by the adjuvant (CFA/IFA), in order to avoid high local concentrations of antigen when mixing with the oil adjuvant. The lid should be tightened firmly by opening and closing it a couple of times to avoid leaks. In addition, the syringe should not be filled with the emulsion completely, only till the 0.15 mL mark on the syringe-barrel to avoid wasting the emulsion. The plunger should be inserted into the syringe very carefully, using both hands. After all the syringes are filled with the emulsion, the syringes can be stored at room temperature if they are to be used the same day; otherwise, they should be stored at 4 °C until use.
Antigen/CFA emulsions prepared by the shaking homogenization method can appear less firm compared to those prepared with the syringe method. An additional shaking step can be added (see step 2.5 in the protocol), which might thicken the emulsion. However, emulsions that pass the "drop test" and phase contrast microscope examination induce EAE regardless of the physical state of the emulsion.
The initial investment required in a shaking homogenization machine is a limitation. However, the preparation steps described here ensure minimal waste of emulsion and the antigen, which is often expensive to purchase or takes a long time to prepare. Therefore, in the long run, this method is cheaper to use since it saves time and reagents. The antigen and buffer used in the shaking homogenization method can affect the quality of the emulsion. The MOG35-55 peptide dissolved in PBS without Ca2+/Mg2+ consistently generated emulsions with small uniform water-in-oil particles (Figure 2A). However, peptide antigens dissolved in PBS with Ca2+/Mg2+, or peptides containing many charged amino acid residues might generate emulsions that are less viscous. Whether such emulsions are less likely to induce disease in animal models has not been tested. Another limitation of this method is that no more than 8 mL of antigen/CFA emulsion can be prepared from one tube. The tubes should not be loaded with more than 9.6 mL in total (4.8 mL of PBS/antigen and 4.8 mL of CFA/IFA), which will be sufficient to load eight 1 mL syringes. Although the tube can hold a greater volume, some air must be present in the tube, otherwise perfect emulsions will not be generated. If more emulsion is needed, it can be prepared using additional tubes.
Compared to existing methods, there is no person-to-person difference when preparing the emulsions with the shaking homogenization method. The most commonly used method to prepare emulsions for EAE experiments utilizes syringes that are pushed back and forth by hand19. The force, time, and temperature cannot be well controlled, and it is therefore difficult to standardize a syringe-based method. Other methods for making water-in-oil emulsions take advantage of ultrasonic water-bath sonicators. Emulsions prepared with a sonication method are able to induce EAE in otherwise resistant BALB/c mice8. The described method could be standardized and therefore useful. However, the problem with ultrasonic water-bath and ultrasonic probe sonicators is that it is difficult to transfer the emulsion in the tubes to syringes used for immunization without introducing air bubbles. The tubes used for the method presented here eliminate this problem.
A vortex method could be regarded to be a standardized method with a set speed, time, and temperature. However, testing this method to prepare an emulsion by vortexing the MOG/CFA preparation for 10 min resulted in no disease induction in C57BL/6J mice (data not shown). Nevertheless, EAE can be induced with an antigen/CFA mixture prepared by vortexing for 45 min18, which would be a much longer procedure compared with the method presented in this manuscript.
Another oil-based adjuvant (see Table of Materials), approved by the FDA to be used on humans, that produces a water-in-oil emulsion has been shown to be a promising adjuvant for cancer and malaria vaccines20,21,22. Therefore, the standardized protocol presented here can be adapted for use in the clinic. Preliminary experiments have revealed that the shaking homogenization method generates emulsions with this FDA-approved oil that are of better quality compared with the manual syringe method (data not shown).
In conclusion, the shaking homogenization method presented here provides a number of benefits, such as the faster generation of quality-controlled emulsions, high reproducibility in a number of autoimmune disease models, and a reduction of expensive reagents needed to prepare antigen/CFA emulsions. Since there is no person-to-person difference generating these water-in-oil emulsions, it offers the possibility to standardize this method needed for reproducible biomedical research and drug discovery in the area of autoimmune diseases and therapeutic vaccine development.
Divulgazioni
The authors have nothing to disclose.
Acknowledgements
The author would like to acknowledge the animal housing units at Lund University, Camilla Björklöv and Agnieszka Czopek, for their support, and Richard Williams, Kennedy Institute of Rheumatology, University of Oxford, UK, for constructive criticism and linguistic support producing this manuscript.
Materials
| 1 mL Injection syringe | B. Braun | 9166017V | |
| 1 mL Injection syringe | Sigma-Aldrich | Z683531 | |
| 7 ml empty tubes with caps | Bertin-Instruments | P000944LYSK0A.0 | 7 mL tube |
| 50 mL sterile centrifuge tube | Fisher Scientific | 10788561 | 50 mL tube |
| Bordetella pertussis toxin | Sigma-Aldrich | P2980 | Store at -20 °C |
| Dispersant, light mineral oil | Sigma-Aldrich | M8410 | Store at RT |
| Emulsion kit | Bertin-Instruments | D34200.10 ea | Containing a tube, cap, and plunger |
| Incomplete Freund's Adjuvant | Sigma-Aldrich | F5506 | Store at +4 °C |
| Mycobacterium tuberculosis, H37RA | Fisher Scientific | DF3114-33-8 | Store at +4 °C |
| Mastersizer 2000 | Malvern Panalytical | N/A | Particle size analyzer |
| Minilys-Personal homogenizer | Bertin-Instruments | P000673-MLYS0-A | Shaking homogenizer |
| MOG 35-55 Peptide | Innovagen | N/A | |
| Montanide ISA 51 VG | Seppic | 36362Z | FDA-approved oil adjuvant |
| Pall Acrodisc Syringe Filters 0.2 μm | Fisher Scientific | 17124381 | Sterlie filter |
| PBS, Ca2+/Mg2+ free | Thermo Fisher Scientific | 14190144 | PBS |
| Phase-Constrast Microscope | Olympus | BX40-B | |
| Steel Beads 3.2 mm | Fisher Scientific | NC0445832 | Autoclave and store at RT |
| Triton X-100 | Sigma-Aldrich | 648463 | Store at RT |
Riferimenti
- Walton, C., et al. Rising prevalence of multiple sclerosis worldwide: Insights from the Atlas of MS, third edition. Multiple Sclerosis. 26 (14), 1816-1821 (2020).
- van Langelaar, J., Rijvers, L., Smolders, J., van Luijn, M. M. B and T cells driving multiple sclerosis: identity, mechanisms and potential triggers. Frontiers in Immunology. 11, 760 (2020).
- Sambucci, M., Gargano, F., Guerrera, G., Battistini, L., Borsellino, G. One, No One, and One Hundred Thousand: T Regulatory Cells’ Multiple Identities in Neuroimmunity. Frontiers in Immunology. 10, 2947 (2019).
- Mix, E., Meyer-Rienecker, H., Hartung, H. P., Zettl, U. K. Animal models of multiple sclerosis–potentials and limitations. Progress in Neurobiology. 92 (3), 386-404 (2010).
- Terry, R. L., Ifergan, I., Miller, S. D. Experimental Autoimmune Encephalomyelitis in Mice. Methods in Molecular Biology. 1304, 145-160 (2016).
- Topping, L. M., et al. Standardization of antigen-emulsion preparations for the induction of autoimmune disease models. Frontiers in Immunology. 13, 892251 (2022).
- Flies, D. B., Chen, L. A simple and rapid vortex method for preparing antigen/adjuvant emulsions for immunization. Journal of Immunological Methods. 276 (1-2), 239-242 (2003).
- Määttä, J. A., Erälinna, J. P., Röyttä, M., Salmi, A. A., Hinkkanen, A. E. Physical state of the neuroantigen in adjuvant emulsions determines encephalitogenic status in the BALB/c mouse. Journal of Immunological Methods. 190 (1), 133-141 (1996).
- Moncada, C., Torres, V., Israel, Y. Simple method for the preparation of antigen emulsions for immunization. Journal of Immunological Methods. 162 (1), 133-140 (1993).
- Waksman, B. H., Adams, R. D. Allergic neuritis: an experimental disease of rabbits induced by the injection of peripheral nervous tissue and adjuvants. The Journal of Experimental Medicine. 102 (2), 213-236 (1955).
- Vladutiu, A. O., Rose, N. R. Autoimmune murine thyroiditis relation to histocompatibility (H-2) type. Science. 174 (4014), 1137-1139 (1971).
- Caspi, R. R. Experimental autoimmune uveoretinitis in the rat and mouse. Current Protocols in Immunology. , (2003).
- Tuzun, E., et al. Guidelines for standard preclinical experiments in the mouse model of myasthenia gravis induced by acetylcholine receptor immunization. Experimental Neurology. 270, 11-17 (2015).
- Brinckerhoff, L. H., et al. Terminal modifications inhibit proteolytic degradation of an immunogenic MART-1(27-35) peptide: implications for peptide vaccines. International Journal of Cancer. 83 (3), 326-334 (1999).
- Kool, M., et al. Alum adjuvant boosts adaptive immunity by inducing uric acid and activating inflammatory dendritic cells. The Journal of Experimental Medicine. 205 (4), 869-882 (2008).
- Hasselmann, J. P. C., Karim, H., Khalaj, A. J., Ghosh, S., Tiwari-Woodruff, S. K. Consistent induction of chronic experimental autoimmune encephalomyelitis in C57BL/6 mice for the longitudinal study of pathology and repair. Journal of Neuroscience Methods. 284, 71-84 (2017).
- Freund, J., Lipton, M. M. Experimental allergic encephalomyelitis after the excision of the injection site of antigen-adjuvant emulsion. The Journal of Immunology. 75 (6), 454-459 (1955).
- Stromnes, I. M., Goverman, J. M. Active induction of experimental allergic encephalomyelitis. Nature Protocols. 1 (4), 1810-1819 (2006).
- Shaw, M. K., Zhao, X. Q., Tse, H. Y. Overcoming unresponsiveness in experimental autoimmune encephalomyelitis (EAE) resistant mouse strains by adoptive transfer and antigenic challenge. Journal of Visualized Experiments. (62), e3778 (2012).
- Arevalo-Herrera, M., et al. Randomized clinical trial to assess the protective efficacy of a Plasmodium vivax CS synthetic vaccine. Nature Communications. 13 (1), 1603 (2022).
- Jiang, C., et al. Potential association factors for developing effective peptide-based cancer vaccines. Frontiers in Immunology. 13, 931612 (2022).
- Neninger Vinageras, E., et al. Phase II randomized controlled trial of an epidermal growth factor vaccine in advanced non-small-cell lung cancer. Journal of Clinical Oncology. 26 (9), 1452-1458 (2008).

