Screening People on Standing Balance with Romberg Testing and Walking Balance with Tandem Walking
Summary
This article describes procedures for screening people for standing and walking balance impairments using two normed, rapid, low-tech balance tests.
Abstract
The goal of this protocol is to inform readers about the exact procedures to use to perform two screening tests for vestibular disorders: tandem walking (TW) with eyes closed, also known as heel-toe walking, and the Clinical Test of Sensory Integration and Balance (CTSIB), which is also known as the modified Romberg. The study describes the steps for performing each test and each of the three CTSIB subtests so that the reader will be able to replicate the test conditions for use in the clinic, in the clinical laboratory, or in any other situation needing valid and reliable screening for balance skill which might be affected by changes in vestibular system function. The procedures detailed here can be easily administered and take less than 1 min per trial. References to published papers with normative data are provided. The representative results section includes examples of data collected with these screening tests.
Introduction
Screening the vestibular system, the sensory system with receptors in the inner ear that detect head movement, is notoriously difficult. Due to the presence of the vestibulo-spinal tracts, which project from the vestibular nuclei in the rostral medulla down through cervical, thoracic, and lumbosacral levels of the spinal cord, the head velocity signals generated by the vestibular system influence balance during standing and walking1. For that reason, many people with disorders of the vestibular system have impaired balance and are at risk of falling. For example, 25% of American seniors over the age of 65 years fall every year2, and the death rate from falls in the United States in 2016 ranged from 24.2 to 142.7 per 100,000 people, depending on the state3. Therefore, balance testing is often a component of a clinical assessment or screening for a vestibular impairment and is often used in clinical research4. These tests may also be useful for on-site screening of athletes, post-flight astronauts, military personnel, and other individuals who may show some balance problems. Such individuals might need to be screened near an athletic field, at a landing site, in an emergency field hospital, or some other emergency situation, respectively, before being transported a long distance to comprehensive healthcare facilities for detailed testing.
To screen people for balance disorders, two different kinds of balance testing are often used. Standing still and shifting weight, such as when washing dishes at the kitchen sink, involves somewhat different skills than translating the body through space when walking. Both kinds of balance should be examined. Balance testing is often performed with a narrow base of support to make a test challenging for the individual. For example, testing standing balance with feet close together and eyes closed is based on the Romberg sign, i.e., that patients have a good balance with eyes open but lose their balance with eyes closed1. This test has been sharpened over the years several times until the current modified version of the Romberg, or Clinical Test of Sensory Integration and Balance (CTSIB)4, was more useful for clinical screening than previous tests by being simpler, shorter, and having proven good sensitivity. The current version uses unstable, medium-density, compliant foam on the support surface and has been sharpened even further with head movements. These modifications have been used in recent studies showing age-related normative data on children and adults and also in studies showing that the norms are specific to the foam used7,8,9,10.
Tandem walking (TW), also known as heel-toe walking, is performed on the floor, with the subject wearing socks but not wearing shoes and with eyes closed. Recent studies provide age-related normative data on children and adults11,12,13. Reduced performance on TW and CTSIB may be consistent with a disorder of the vestibular system, although balance tests are not direct tests of the vestibular system. When TW and CTSIB are given together to patients who do not have musculoskeletal deformities or significant neurologic problems, the sensitivity of the tests to vestibular disorders is higher than when only TW or CTSIB is given12.
Using the methodology described in this paper, several studies have been performed with healthy participants. For example, a study of 292 healthy controls and 90 patients with vestibular disorders – as indicated on standard, clinical objective tests of the vestibular system using bi-thermal caloric testing, vestibular evoked myogenic potentials, and Dix-Hallpike testing – showed age-related declines among controls on the CTSIB conditions and TW11,12,13.The sensitivity of the individual tests was moderate for TW7 and CTSIB8, but the sensitivity of the combined battery was > 0.9. In a study of CTSIB at the Museum of Science Boston, healthy participants were able to test themselves on CTSIB on compliant foam with the head still condition14. Age-related changes among children and adults were found by that group, too.
These performance-based screening tests cannot be learned from reading about them in the research papers. This paper aims to inform the reader exactly how to perform these tests.
Protocol
The test methodologies described in this study were developed with healthy control subjects and patients with vestibular disorders. Healthy control subjects had no known history of neurologic, otologic, or musculoskeletal disorders. Patients with vestibular disorders had abnormal responses on a battery of objective tests of the vestibular system, including tests of the vestibulo-ocular reflex in darkness, positional tests, and cervical vestibular-evoked myogenic potentials. These studies were approved by the Institutional Review Board for Human Subjects Research at Baylor College of Medicine, Houston, Texas, USA.
NOTE: In a study of 1869, healthy subjects aged 4 to 85 years who were tested at Space Center Houston, a community science education center, subjects were tested with the methodology described in this paper. Participants first removed their shoes but wore socks. Science educators then tested participants on Tandem Walking with eyes closed and on CTSIB on compliant foam with three conditions, each with eyes closed, standing still with the head still, standing still with slow head nodding in pitch (up/down), and standing still with slow head shaking in yaw (right/ left).
1. Patients/research subjects
- Ensure that individuals can stand erect, unsupported, for at least 30 s. They must be able to follow the instructions.
2. Environment and equipment
- Perform the tests in a well-lighted room with a firm surface, e.g., vinyl tile or industrial carpeting. Do not perform these tests on plush carpeting.
- Use a stopwatch, clock with a second hand, or digital timer for CTSIB. No timing device is needed for TW.
- To perform CTSIB, use medium-density, compliant foam which meets the following compliance criterion: PSI = 0.85-0.95. This type of foam is commonly known as temper foam or memory foam. The norms were developed with foam of the following size: 40.64 cm X 45.72 cm X 10 cm. A larger slab of foam may be used if desired, but it is not necessary.
NOTE: More than one manufacturer makes this foam. Using the foam with the correct compliance characteristics is essential. If another type of foam is used, the published norms will not apply.
3. Methodology for CTSIB
- Place the foam near a corner of the room or a wall for safety. Have the individual first practice the test on the floor with eyes open to learn the basic movements involved.
- Instruct the individual being tested to stand erect, not touching anything against the legs or back, with feet together, side by side. Ensure that the individual's arms are crossed at the waist, with each hand holding the contralateral elbow or comfortably crossed at the waist.
- Instruct the individual to look straight ahead. Perform 1-3 test trials for 5-10 s, on the foam, with arms crossed at the waist, feet adjacent, standing erect and looking straight ahead, with nothing touching the legs or back.
- To steady the individual, place a hand on the person's shoulder while the person looks straight ahead.
- To start the test trial say, "Close your eyes". Remove the hand from the person's shoulder, say "Go", and begin timing the trial for up to 30 s. Perform this trial only once. If the individual appeared frightened, distracted by a noise, or did not understand the instructions, perform a second trial and consider the first trial a training trial.
NOTE: The individual will have increased postural sway with eyes closed, which may be a source of concern to the person being tested. Gently advise the individual not to worry about it. - Dependent measure: Measure the time the individual can maintain the erect posture before making an error, up to 30 s, for each CTSIB condition.
NOTE: Errors are opening the eyes, moving the arms, taking a step, or leaning against the wall.
- Perform Trial 1 with the head stationary. If the person has difficulty on Trial 1 the first time, consider that trial a training trial, and give it a second time. Use the score from the second trial.
- Perform Trial 2 with head nodding (up/down) slowly at 0.3 Hz in time to a real metronome or digital metronome application.
- Prior to starting Trial 2, have the individual stand on the floor with eyes open and practice nodding the head in time to the sound until the maximum upper and lower head movements occur in time to the maximum and minimum sounds on the application so that the individual can move at 0.3 Hz.
- To perform Trial 2, instruct the individual to stand on the foam, with feet adjacent and arms crossed, as in Trial 1.
- Start the sound on the metronome or metronome app before the individual closes his/ her eyes. Then instruct the individual to close his/ her eyes while the hand of the investigator is on the person's shoulder to steady him/her.
- To begin Trial 2, instruct the individual to nod his/her head (head moves up/ down) in time to the sound when "Go" is heard.
- Remove the hand from the individual's shoulder, say "Go" and simultaneously start the timer.
- After this trial, allow the individual to rest for a few seconds by stepping off the foam and sitting down if desired.
- Perform Trial 3 with the head shaking (left/right) at 0.3 Hz, in time to the sound. Otherwise, use the same procedure for Trial 2.
4. Methodology for Tandem Walking
- Make sure the room has no obstructions where the individual will walk over a distance of approximately 4.5 m forward and approximately 1 m on either side of the individual. More space can be used but is not required.
- Demonstrate the test for the individual for 3 to 5 steps: Put one foot heel-to-toe in front of the other foot. Repeat for 4 more steps so the individual will know the task.
- Practice trial:
- Instruct the individual to perform a practice trial with eyes open, arms crossed at the waist as for the CTSIB, without wearing shoes but wearing socks for good hygiene.
- Have the individual place one foot directly in front of the other, with no more than 2.4 cm (1 inch) between the front and rear feet. Ensure that the individual performs the practice trial for up to 5 steps. If needed, use more than one practice trial for the individual to understand the motor task.
- Test trial: Have the individual stand with arms crossed, feet at a comfortable distance apart, without wearing shoes but wearing socks for good hygiene. Instruct the individual to close his/her eyes and perform 10 heel-to-toe steps, as described in step 4.3, when the investigator says, "Go."
- Do not time the test.
- Dependent measure: Measure the total number of correct tandem steps performed out of 10 steps, even if the steps are not consecutive. To count incorrect steps, count with the fingers of one hand, the way children use fingers to count. Count the total number of steps aloud, but do not say the number of incorrect steps aloud during the test.
NOTE: Errors are: opening the eyes, moving the arms, stepping out of line, or stepping too far ahead of the rear foot.
5. Scoring for CTSIB and TW
- To score the trials, two sources provide data. Use the norms for children and young adults on CTSIB and TW from the paper with those published data9. Also, CTSIB and TW norms for adults aged 21 to 90 are available in the paper with those published data8.
- Compare the individual's scores to the published data to determine if the scores are normal or abnormal for the individual's age group and, for CTSIB, for each condition.
Representative Results
As with other studies, age-related changes were found on tandem walking and for CTSIB, especially for young children and older adults, although the data for the oldest old may not be reliable due to the small sample size. Figure 1 shows the data for the three conditions of CTSIB. Figure 2 shows the data for eye-closed tandem walking. Young children had reduced scores for both tests compared to children aged 10 and older. Scores declined in the middle- and especially older age. In this particular study, the data for the oldest subjects are unreliable due to small sample sizes.
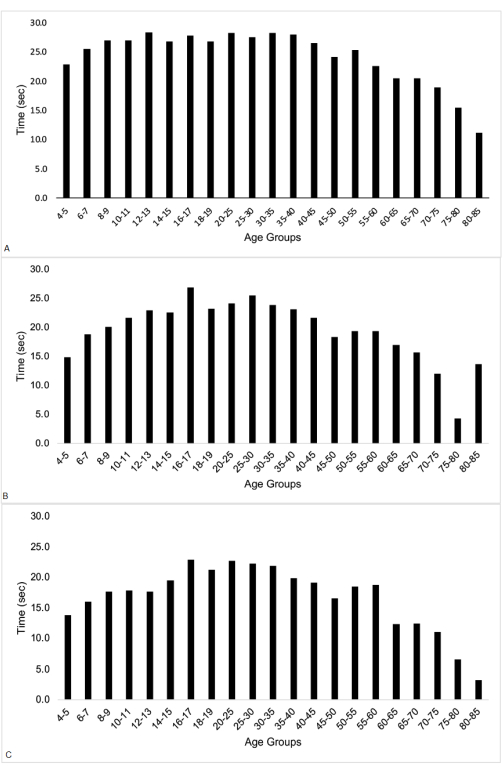
Figure 1: Mean CTSIB data by age groups. The data are the time in seconds. (A) CTSIB head still. (B) CTSIB head yaw. (C) CTSIB head pitch. This figure has been modified from the original paper and used with permission from Friello et al.13. Please click here to view a larger version of this figure.
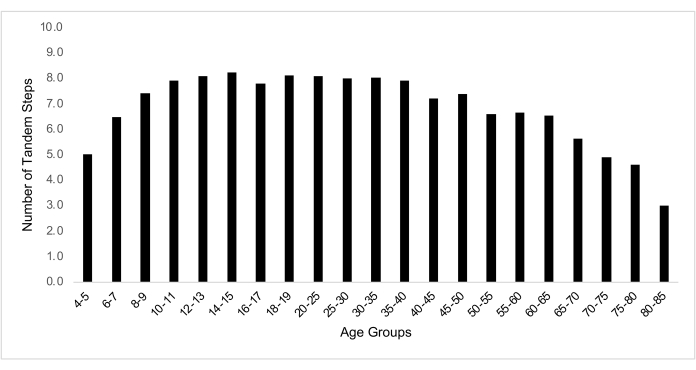
Figure 2: Median TW data by age groups. The data are the number of correct tandem steps. Ranges were from 1 to 10 but varied by age; refer to Friello et al.13 for details. This figure has been modified from the original paper and used with permission from Friello et al.13. Please click here to view a larger version of this figure.
Discussion
These screening tests require minimal or no technology and minimal space. Administration and scoring are quick and easy. Therefore, these screening tests are widely used in healthcare settings by medical providers, occupational therapists, and physical therapists in rehabilitation clinics and epidemiologic screening studies. These tests can be used to screen patients for vestibular disorders and also to screen people with non-vestibular disorders such as presbyastasis. Other balance impairments may also be screened with these tests, but the list of possible disorders is too long to describe here. Clinicians who are trained in the assessment and treatment of various types of vestibular and non-vestibular balance disorders can use these screening tests as part of the clinical toolbox.
The tests have some limitations. These tests can only be used with people who are able to follow the instructions and are able to stand unassisted. Musculoskeletal problems, such as arthritis and joint deformities, amputation of a toe, significant weakness, and incoordination affecting the feet and lower extremities will all affect the test results. Similarly, movement disorders of the nervous system, such as Parkinson's disease, will affect test results. Musculoskeletal and movement disorders may interfere with the ability to stand long enough to perform the test, to have good enough weight-shifting ability, or even the motor control to perform the tests at all. To be consistent with the normative data, shoes should not be worn, but socks should be worn for good hygiene. Obesity affects the outcome5. The type of compliant foam used for CTSIB affects the outcome. If the test administrator prefers to use a different type of foam, then the test administrator should follow the advice of Shumway-Cook and Horak, the originators of CTSIB, and develop norms on healthy individuals before testing with patients15.
These normed balance tests are useful for screening balance in a wide range of ages. They require minimal equipment and minimal time but provide valid and reliable data for use in a variety of settings. The test administrator should use foam with the correct density characteristics, and individuals should perform the tests without shoes but while wearing socks, with eyes closed. Test sensitivity (to patients) and specificity (to healthy controls) will be improved if both tests are used. Test scores will be influenced by the presence of movement disorders, musculoskeletal disorders, or difficulty following instructions. Therefore, interpret the data with care in the presence of such problems.
Divulgazioni
The authors have nothing to disclose.
Acknowledgements
This research work was supported by NIH grant R01 DC009031. Thanks to Sharon L Congdon, Melody A Fregia, and Nathan Silver for technical support.
Materials
| 10 cm thick, medium density, Sunmate foam | Dynamic Systems, Leicester, NC, USA; | sunmatecushions.com | Either this foam or foam by another manufacturer that has the same compliance characteristics as medium density Sunmate foam will be sufficient. Use a slab of foam large enough for an adult man's feet, e.g. 40.65 cm X 45.72 cm or larger |
| Metronome app | Any source | N/A | Either a real, physical metronome or a metronome app that can provide an auditory cue at 0.3 Hz. 0.3 Hz is the equivalent of 18 beats per minute, but using 20 beats per minute is acceptable if your app only goes that low. |
| Stopwatch | Any source | N/A | Any timing device in tenths of seconds will be sufficient |
Riferimenti
- Wilson, V. J., Melvill Jones, G. . Mammalian Vestibular Physiology. , (1979).
- Bergen, G., Stevens, M. R., Burns, E. R. Falls and fall injuries among adults aged ≥65 years-United States, 2014. MMWR Morbidity and Mortality Weekly Report. 65 (37), 993-998 (2016).
- Burns, E., Kakara, R. Deaths from falls among persons aged > 65 years – United States, 2017 – 2016. MMWR Morbidity and Mortality Weekly Report. 67 (18), 509-514 (2018).
- Strupp, M., Brandt, T., Dieterich, M. . Vertigo and Dizziness. , (2023).
- Lanska, D. J. The Romberg sign and early instruments for measuring postural sway. Seminars in Neurology. 22 (4), 409-418 (2002).
- Horak, F. B. Clinical measurement of postural control in adults. Physical Therapy. 67 (12), 1881-1885 (1987).
- Gosselin, G., Fagan, M. Foam pads properties and their effects on posturography in participants of different weight. Chiropractic & Manual Therapies. 23 (1), 2 (2015).
- Lin, C. -. C., et al. Test-retest reliability of postural stability on two different foam pads. Journal of Nature and Science. 1 (2), e43 (2015).
- Cohen, H. S., Sangi-Haghpehkar, H. Differences in responses on the modified clinical test of sensory interaction and balance on medium firm and medium density foam in healthy controls and patients with vestibular disorders. Biomedicine Hub. 5 (1), 1548-1555 (2020).
- Patel, M., Fransson, P. A., Lush, D., Gomez, S. The effect of foam surface properties on postural stability assessment while standing. Gait & Posture. 28 (4), 649-656 (2008).
- Cohen, H. S., et al. Tandem walking as a quick screening test for vestibular disorders. The Laryngoscope. 128 (7), 1687-1691 (2018).
- Cohen, H. S., et al. Screening for vestibular disorders using the modified clinical test of sensory interaction and balance and tandem walking with eyes closed. Otology & Neurotology. 40 (5), 658-665 (2019).
- Friello, P., Silver, N., Sangi-Haghpeykar, H., Cohen, H. S. Screening for balance in children and adults in a community science education setting: normative data, influence of age, sex, and body mass index, and feasibility. PLoS One. 17 (5), e0268030 (2022).
- Bermudez Rey, M. C., Clark, T. K., Merfeld, D. M. Balance screening of vestibular function in subjects aged 4 years and older: a living laboratory. Frontiers in Neurology. 8, 631 (2017).
- Shumway-Cook, A., Horak, F. B. Assessing the influence of sensory interaction on balance. Physical Therapy. 66 (10), 1548-1550 (1986).

