A Rat Dry Eye Model with Lacrimal Gland Dysfunction Induced by Scopolamine
Summary
Here, we establish a rat model of lacrimal gland dysfunction to provide a basis for the study of aqueous-deficient dry eye.
Abstract
Aqueous-deficient dry eye (ADDE) is a type of dry eye disease that can result in the reduction of tear secretion quantity and quality. Prolonged abnormal tear production can lead to a disturbance in the ocular surface environment, including corneal damage and inflammation. In severe cases, ADDE can cause vision loss or even blindness. Currently, dry eye treatment is limited to eye drops or physical therapy, which can only alleviate eye discomfort symptoms and cannot fundamentally cure dry eye syndrome. To restore the function of the lacrimal gland in dry eye, we have created an animal model of lacrimal gland dysfunction in rats induced by scopolamine. Through the comprehensive evaluation of the lacrimal gland, corneas, conjunctivas, and other factors, we aim to provide a full understanding of the pathological changes of ADDE. Compared with the current dry eye mouse model, this ADDE animal model includes a functional evaluation of the lacrimal gland, providing a better platform for studying lacrimal gland dysfunction in ADDE.
Introduction
By 2021, approximately 12% of people are significantly affected by dry eyes1, making it one of the most common chronic eye diseases. Dry eye can be divided into two types: aqueous-deficient dry eye (ADDE) and evaporative dry eye (EDE)2, depending on the different factors that affect the disease. ADDE is further divided into Sjögren's syndrome (SS) and non-SS, but the majority of dry eye patients are non-SS patients in clinical3. Chronic dry eye symptoms seriously affect the visual quality of patients. Currently, the conventional treatment of DED involves the application of artificial tears to lubricate the ocular surface and physical therapy of the eyelids. However, dry eye syndrome may not offer a complete cure in many cases. Therefore, studying the pathogenesis of dry eye disease is crucial for the development of new therapies and drugs. Animal models of dry eye syndrome provide a foundation for further research.
There are many ways to construct animal models of dry eye syndrome4, including changing tear secretion levels by altering hormone levels. For example, removing the testes of rats can reduce androgen secretion, increase tear secretion, and decrease the concentration of free secretory component (SC) and IgA in tears5,6. Another method is to indicate autoimmune reactions in the lacrimal gland by removing the eye surface nerves that control the gland. Additionally, directly reducing tear secretion can be achieved by surgically removing the lacrimal gland7. Changing environmental conditions can also accelerate tear evaporation. For example, culturing animals in low humidity and dry ventilation conditions can establish a model of excessive evaporative dry eye8, which can be combined with other methods to increase the severity of dry eye. The main drugs used to induce dry eye experimental models are atropine and scopolamine9. As parasympathetic inhibitors, both can induce pharmacological blockade of cholinergic (muscarinic) receptors in the lacrimal gland and inhibit tear secretion. Compared with dry eyes caused by atropine muscle injection10, scopolamine has a stronger inhibitory effect on secretion glands, a longer duration of drug action, and weaker effects on cardiac, small intestinal, and bronchial smooth muscles. It is one of the most mature drugs for dry-eye animal models.
Different methods can be used to induce dry eye with scopolamine, such as subcutaneous injection, drug pump, or patch application4,11,12. In order to reduce the frequency of drug administration to experimental animals, many researchers apply transdermal patches to the tails of mice or use drug pumps. However, both of these methods have limitations. For example, the absorption of transdermal patches needs to take into account the individual absorption of mice, which can lead to inconsistent drug dosage. Although drug pumps can accurately control the dosage of each administration, they are not always compatible with the drug being delivered or the concentration being used. They also need to be placed surgically – which is more invasive to the animal, requiring an anesthetic event, and there is potential for post-surgical complications such as dehiscence. Subcutaneous injection, although more cumbersome, can ensure accurate dosage for each administration and maintain consistency in drug administration among different rats. At the same time, it has a lower cost and is suitable for conducting a large number of animal experiments.
This study applies repeated subcutaneous injection of scopolamine to establish a dry eye rat model. We analyze dry eye indicators such as corneal defects, tear secretion levels, and pathological morphology of the cornea, conjunctiva, and lacrimal gland. By combining drug concentration, pathological manifestations, and dry eye symptoms, we further elaborate on the dry eye rat model in detail, providing more accurate experimental data for the study of dry eye treatment and pathological mechanisms. We also describe the modeling process in detail for future researchers.
Protocol
All animal experiments performed following this protocol are performed under the approval of the Institutional Animal Care and Use Committee (IACUC).
1. Animal preparation
- Prepare 12 healthy 6-week-old SPF Wistar female rats weighing 160 g ± 20 g.
- Use a slit lamp and ophthalmoscope to examine the eye conditions of all rats, ensuring that there are no anterior segment or retinal diseases.
- Raise all the rats for 1 week with sufficient food and water sources.
- Randomly divided all rats into normal, scopolamine drug concentration 2.5 mg /mL, scopolamine drug concentration 5 mg/mL, and scopolamine drug concentration 7.5 mg/mL groups, with three animals in each group.
2. Solution preparation
- Prepare scopolamine hydrobromide by dissolving it in 0.9% sodium chloride solution to make a solution with concentrations of 7.5 mg/mL, 5 mg/mL, and 2.5 mg/mL.
- Prepare a 0.9% sodium chloride solution without scopolamine hydrobromide to be used as an injection for the control group of rats.
3. Equipment and material preparation
- Prepare a small animal microscope.
- Prepare materials for the experiment, including 1 mL disposable syringe with needle (26 G); fluorescein sodium ophthalmic strips; Schirmer tear test strip; absolute ethanol; 4% paraformaldehyde; xylene; neutral balsam; hematoxylin, eosin; and periodic acid-Schiff staining kit.
4. Subcutaneous injection
NOTE: This procedure requires assistance from a second person to help secure the rats.
- Hold the rat's body steady and catch and stretch its left (or right) hind legs.
NOTE: An assistant can help in holding the animal. - Clean injection site with alcohol.
- Insert 1 mL disposable syringe with needle (26 G) at the base of skin fold between thumb and finger.
- Aspirate the syringe by pulling back the syringe plunger. Any blood in the syringe indicates improper needle placement; remove and reposition the needle.
- Administer 0.9% sodium chloride solution with or without scopolamine hydrobromide in a steady, fluid motion.
- Inject all rats according to different concentrations, with 0.5 mL injected each time and four times daily (at 9:00, 12:00, 15:00, and 18:00) for a consecutive period of 19 days, alternating between left and right limbs.
NOTE: The groups are named as follows:
Group without scopolamine hydrobromide: 0 group (control)
Group with scopolamine hydrobromide 2.5 mg/mL: 2.5 group
Group with scopolamine hydrobromide 5 mg/mL: 5 group
Group with scopolamine hydrobromide 7.5 mg/mL: 7.5 group - Return the animal to its cage and monitor breathing and behavior for 5-10 min.
5. Tear secretion test (Schirmer tear test, STT)
- Create a modified filter paper strip for rats11. Cut half of the filter paper strip used for humans along the centerline (1 mm × 15 mm), and trim the head of the strip to make it smooth.
NOTE: Before conducting the tear secretion test, manually restrain the rat's body to prevent movement and ensure exposure of the rat's eyes. - Place the filter paper strip on the outer 1/3 of the lower eyelid conjunctival sac of the rat.
- Time the test for 5 min. Control the closure of the rat's eyes throughout the procedure.
- After measuring, use tweezers to clamp the filter paper strip into a microcentrifuge tube and record the tear volume by making a mark on the wall of the tube.
- Measure tear secretion on day 0, day 1, day 3, day 5, day 7, day 11, day 15, and day 19.
6. Corneal fluorescein staining
- Drop 0.5 µL of 0.5% fluorescein sodium solution into the inferior conjunctival sac of each rat.
- Observe the cornea under blue light for 3 min after fluorescein instillation.
- Record the fluorescence staining of each rat's cornea and observe whether there is a corneal defect.
- Perform corneal fluorescein staining on day 0, day 1, day 3, day 5, day 7, day 11, day 15, and day 19.
7. Histological observation of conjunctival tissue
- After completing the model development, anesthetize the rats deeply with an intraperitoneal injection of 0.4 mL/100 g of 10% aqueous chloral hydrate to alleviate the animals' tension. Then, euthanize the rats by cervical dislocation.
- Take the bulbar conjunctiva from the same regions of each rat, with a size of approximately 2 mm x 2 mm.
- Fix the tissues immediately in 4% paraformaldehyde for 24 h and embed in paraffin13.
- Cut 5 µm thickness sections and stain with hematoxylin and eosin (HE)14 and periodic acid-Schiff (PAS) stain (follow manufacturer's instructions).
8. Histological observation of corneal and lacrimal gland tissue
- After completing the model development, euthanize the rat as described in step 7.1.
- Take the cornea on the right side of each rat and fix it immediately in 4% paraformaldehyde solution.
- Cut the cephalic epidermis and subcutaneous tissue along the line connecting the ear and the outer corner of the eye, expand the incision to both sides and further isolate the yellowish extra orbital gland.
- Thoroughly remove the rat's fur and separate the extraorbital gland with 0.9% sodium chloride solution.
- Place the isolated extraorbital glands in 4% paraformaldehyde solution for 24 h and embed in paraffin.
- Cut continuous sections of ~5 µm thickness and stain them with HE for corneal and extraorbital gland tissue specimens.
9. Statistical analysis
- Use appropriate software for statistical analysis of the data.
- Perform one-way analysis of variance (ANOVA) to analyze the data and the least significant difference (LSD) test for comparison between groups. Set the statistical significance level at α = 0.05, with P < 0.05 indicating statistical significance.
NOTE: SPSS 20 software was used for statistical analysis of the experimental data.
- Perform one-way analysis of variance (ANOVA) to analyze the data and the least significant difference (LSD) test for comparison between groups. Set the statistical significance level at α = 0.05, with P < 0.05 indicating statistical significance.
Representative Results
Schirmer I test, SIT I
The tear volume of the rats was measured on days 0, 3, 5, 7, 11, 15, and 19 after the start of the experiment. The experimental results showed that the tear secretion of the scopolamine group (2.5 group, 5 group, 7.5 group), compared with the control group (0 group), was significantly decreased, and the difference was statistically significant (P < 0.01). There was no statistical significance between the 2.5 group, 5 group, and 7.5 group (P > 0.05). There was no significant difference observed between the different groups in terms of the number of days (P > 0.05) (Figure 1, Table 1).
Corneal fluorescein staining
Corneal fluorescein staining was performed on days 0, 3, 5, 7, 11, 15, and 19 of the experiment. The results showed that there was no corneal fluorescein staining in any group, indicating that no obvious corneal epithelial defects were formed during the 20-day experiment with different concentrations of scopolamine drugs (Figure 2).
Pathological analysis of corneal epithelium
After the experiment, corneal tissues from each rat were collected for HE staining to observe the morphology of the corneal epithelium and measure the thickness of the corneal epithelial layer. The corneal epithelium of the control group was composed of 4-6 layers of orderly arranged epithelial cells, among which the basal layer consisted of a single layer of columnar epithelial cells arranged neatly and closely. The corneal epithelium of scopolamine groups 2.5, 5, and 7 were significantly thinner than the control group, with flattened and atrophic cell morphology and disordered cell structure. In group 7.5, there was a loose intercellular connection and vacuolar structure in the basal layer (indicated by the red arrow in Figure 3). Compared with the corneal epithelium of scopolamine groups, the corneal epithelium of the normal control group showed statistical differences in the thickness of the corneal epithelial layer (Figure 4).
Pathological analysis of lacrimal gland
The main gland for tear secretion in rats is the extrorbital lacrimal gland15. When observing lacrimal gland slices, changes in the morphology of the lacrimal gland epithelial cells were observed with the increase of scopolamine concentration, accompanied by inflammation and tissue edema. No such changes were observed in the control group. The pathology results suggest that inflammatory changes of the lacrimal gland, cell edema, and atrophy of the glandular epithelial cells can be used as indicators for functional damage of the lacrimal gland16 (Table 2). These indicators can be used to measure the severity of dry eye in relation to the amount of tear secretion (Figure 5).
Analysis of conjunctival staining results
The structure of the conjunctiva in the control group is complete, mainly composed of the surface layer and the lamina propria. The surface layer is laminated columnar epithelial cells, smooth and complete, with microvilli on the cell surface. Scattered goblet cells were present between the epithelial cells, with large cell volume and mucous granules in the cell cytoplasm. The surface layer of the conjunctival epithelium in the three scopolamine drug groups was significantly thinner, the number of microvilli and goblet cells was reduced, the cell arrangement structure was incomplete, accompanied by edema, and a small amount of inflammatory cells as observed in HE staining (Figure 6).
By staining the conjunctiva with PAS, the average number of goblet cells per 40x microscopic field in three independent samples of each mouse was calculated and expressed as mean ± SD (Figure 7).
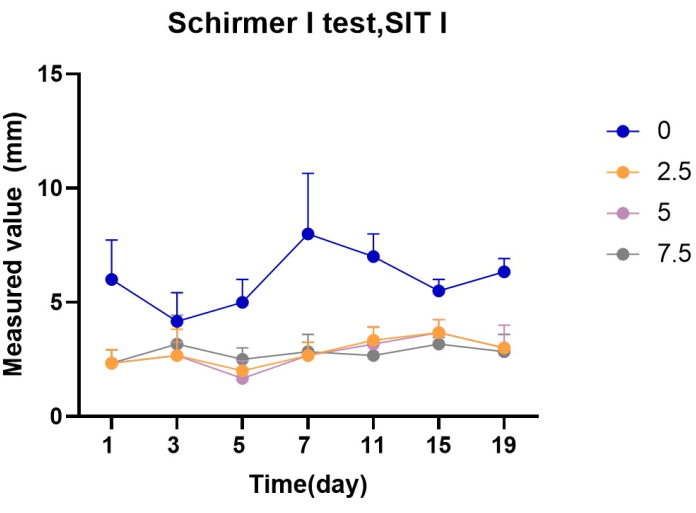
Figure 1: Statistics of Schirmer test value in each group (mm) Please click here to view a larger version of this figure.
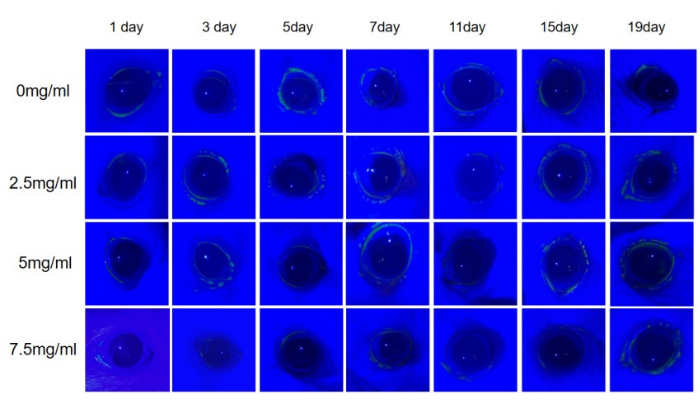
Figure 2: Fluorescein sodium staining of rat cornea. In the 20-day experiment with fluorescein sodium, no positive findings were observed in the corneas of all rats. Please click here to view a larger version of this figure.
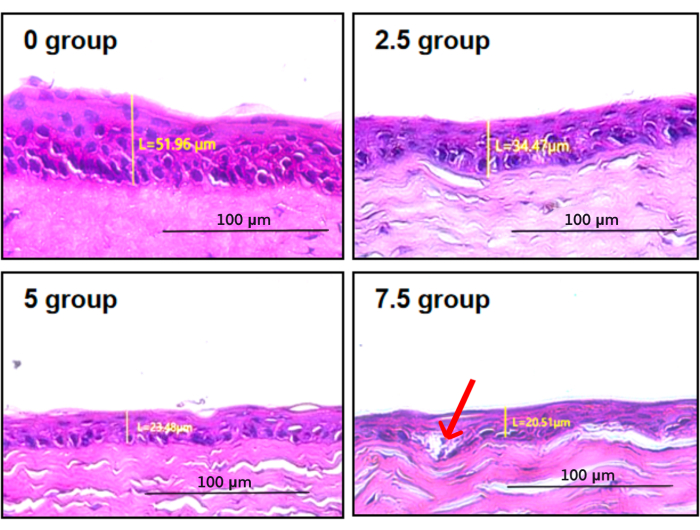
Figure 3: Corneal epithelium staining and thickness measurement. In group 7.5, there was loose intercellular connection and vacuolar structure in the basal layer (indicated by the red arrow) Please click here to view a larger version of this figure.
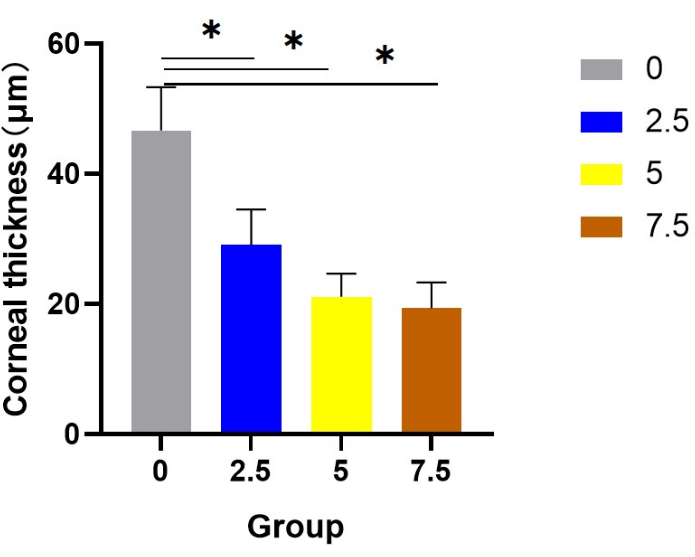
Figure 4: Statistics of corneal epithelial thickness in each group. Compared with the corneal epithelium of scopolamine groups, the corneal epithelium of the normal control group showed statistical differences in the thickness of the corneal epithelial layer. Please click here to view a larger version of this figure.
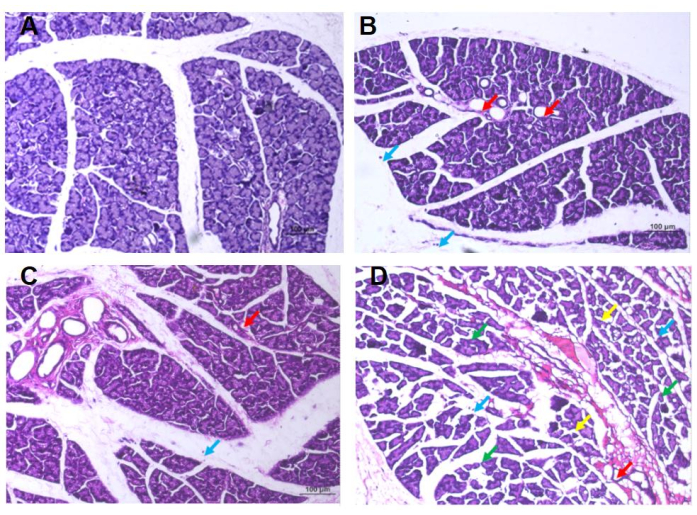
Figure 5: HE staining results of the extrorbital lacrimal gland of rats. (A) Group 0: In the visual field, lacrimal glands showed lobular structure and were composed of ducts and tubular glands, with no obvious abnormalities in the morphology of the ducts, while the tubular glands were composed of cone-shaped glandular cells with abundant mucous substances in the cytoplasm, no obvious edema in connective tissues, no obvious abnormalities in interstitial blood vessels, and no obvious necrosis and inflammatory cell infiltration. (B) Group 2.5: In the visual field, occasional atrophy of the lacrimal gland epithelial cells is observed, with reduced volume, irregularly-shaped dilated glandular cavities, and reduced mucinous substance within the cavity (indicated by the red arrow). There is also occasional infiltration of free lymphocytes in the stroma (indicated by the blue arrow), but no obvious abnormalities in the duct morphology or signs of edema are observed. (C) Group 5: In the visual field, lacrimal epithelial cells were occasionally atrophied and reduced in size, the glandular cavity was enlarged, the mucous substance in the cavity was reduced (red arrow), and free lymphocyte infiltration was occasionally observed in the stroma (blue arrow), and no obvious abnormalities in duct morphology or connective tissue edema between lacrimal gland lobules are observed. (D) Group 7.5: Edema can be seen in the visual field; the spacing between the lacrimal glands is widened, and the arrangement is irregular (green arrow), the epithelial cells of the lacrimal glands are often atrophied, the volume becomes smaller, and the shape is irregular (yellow arrow), occasionally the gland cavity is enlarged, the mucous matter in the cavity is reduced (red arrow), occasionally the free lymphocyte is infiltrated (blue arrow), with no apparent abnormalities in duct morphology. Please click here to view a larger version of this figure.
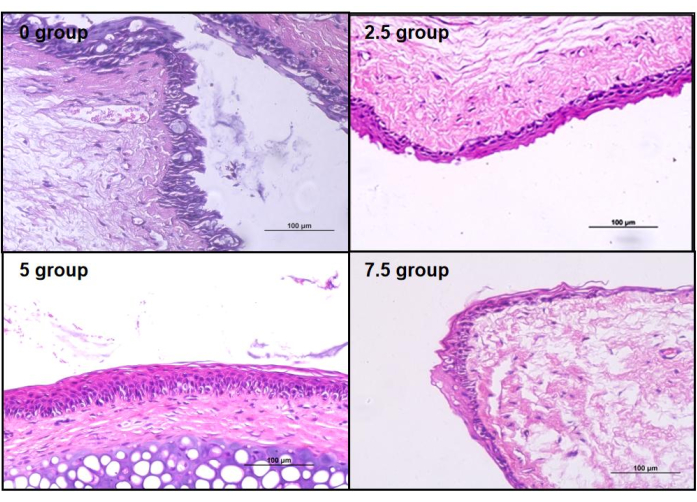
Figure 6: HE staining of rat conjunctiva. Compared to the control group's conjunctival epithelium, all three groups of scopolamine-medicated conjunctival epithelium showed varying degrees of structural damage. Please click here to view a larger version of this figure.
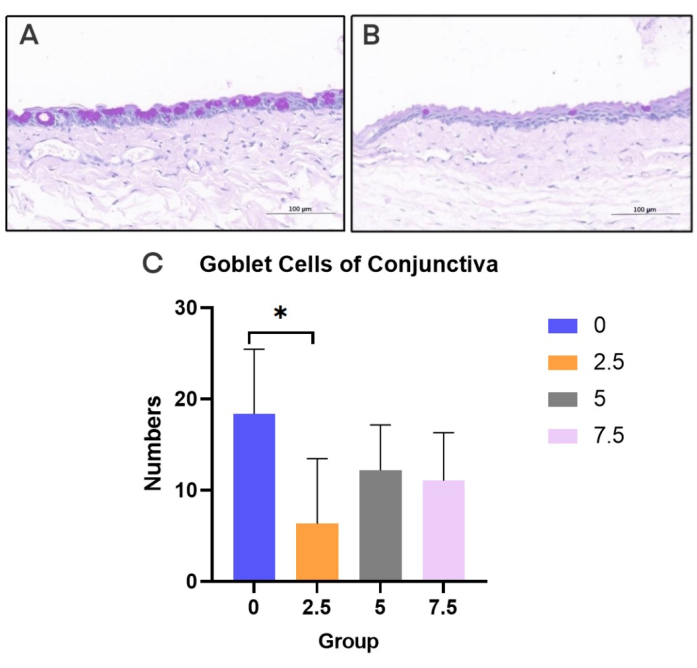
Figure 7: PAS staining of conjunctiva. (A) Normal control rats. (B) scopolamine group rats. (C) Goblet cell density in each group (20x). Black bar = 100 µm. Please click here to view a larger version of this figure.
| Schirmer I test, SIT(Mean value, unit [mm]) | |||||||
| Group | 0 days | 3 days | 5 days | 7 days | 11 days | 15 days | 19 days |
| 0 | 6 | 4.2 | 5 | 8 | 7 | 5.5 | 6.3 |
| 2.5 | 2 | 2.7 | 2 | 2.7 | 3.3 | 3.7 | 3 |
| 5 | 2.3 | 2.7 | 1.7 | 2.3 | 3.2 | 3.7 | 3 |
| 7.5 | 2.3 | 3.2 | 2.5 | 2.8 | 2.7 | 3.2 | 2.8 |
Table 1: Schirmer test of rats in the four groups at different time points (mm). After applying medication, the secretion of tears in rats significantly decreased.
| Number | Necrosis | Inflammation | Edema | Epithelial atrophy |
| 0 Grp-1 | 0 | 0 | 0 | 0 |
| 0 Grp -2 | 0 | 0 | 0 | 0 |
| 0 Grp -3 | 0 | 0 | 0 | 0 |
| 2.5 Grp -1 | 0 | 1 | 0 | 0 |
| 2.5 Grp -2 | 0 | 0 | 0 | 0 |
| 2.5 Grp -3 | 0 | 1 | 0 | 1 |
| 5 Grp -1 | 0 | 1 | 0 | 1 |
| 5 Grp -2 | 0 | 1 | 0 | 1 |
| 5 Grp -3 | 0 | 0 | 0 | 1 |
| 7.5 Grp -1 | 0 | 1 | 2 | 1 |
| 7.5 Grp -2 | 0 | 1 | 0 | 1 |
| 7.5 Grp -3 | 0 | 1 | 2 | 2 |
Table 2: Pathological tissue score of rat lacrimal gland. Scoring criteria: 0: Under normal conditions, considering factors such as animal age, sex, and strain, the tissue is deemed normal;
1: The observed changes have just exceeded the normal range; 2: Lesions can be observed, but they are not yet severe; 3: Lesions are evident and continue to worsen; 4: Lesions are extremely severe and have affected the entire tissue16.
Discussion
Aqueous-deficient dry eye (ADDE) is an important type of dry eye, accounting for about 1/3 of the total dry eye population17, and the main cause of ADDE is lacrimal gland pathological damage and inflammation13. For this type of dry eye, the most common clinical treatment methods are artificial tears to alleviate symptoms or topical application of steroids or cyclosporine18, while there are few treatment options for damage to the lacrimal gland. Therefore, it is very important to explore the impact of lacrimal gland function reconstruction on dry eye and establish an animal model of lacrimal gland dysfunction. We used a method of repeated application of medication to suppress the secretion of the lacrimal gland in rats and created a chronic lacrimal gland dysfunction dry eye animal model.
We chose rats to construct this dry eye model, which has more advantages compared to other animal models19. For example, rabbits have a larger body size and require more doses of medication or more frequent injections to achieve the desired effect. Moreover, rabbits are slightly more expensive, which means more costs for the experiment. Mice are also commonly used in ophthalmic research, but they are generally used to construct Sjögren's syndrome models20. These models focus on comparing organ inflammation and lymphocyte infiltration to explore the immunopathological mechanisms. Mice have small body sizes, complex lacrimal gland anatomy, and low tear secretion, making it difficult to accurately reflect tear production. The rat animal model is a more suitable dry eye model as it allows for convenient drug injections, has relatively simple feeding conditions, is suitable for both clinical and experimental studies, and also has advantages in terms of cost. It is a good animal model for ADDE.
We applied the cholinergic receptor blocker scopolamine to inhibit the cholinergic receptors in the rat's body, reducing the lacrimal gland secretion and altering the pathological structure of lacrimal gland cells, which fundamentally simulates the state of lacrimal glands in dry eye patients. Compared to other methods, this approach better simulates the damaged condition of lacrimal glands in a natural state. Other methods, such as using benzalkonium chloride eye drops21 or altering external conditions such as reducing humidity and increasing ocular surface evaporation4,8, only disrupt the ocular surface environment and do not change the functional state of the lacrimal gland. Therefore, they are not suitable for long-term, chronic dry eye conditions.
In measuring the secretion volume of tears in rats, we improved the Schirmer tear test strips. First, we cut the tear test strip used by humans along the center line. Then, we trimmed the top into a round arc shape and gently folded it back at the top to facilitate easy insertion into the rat's lower conjunctival sac. It should be noted that rats are active, and difficult to measure tears for 5 min. After inserting the Schirmer tear test strip into the rat's lower conjunctival sac, we manually closed the rat's eyes to increase their comfort and avoid struggling during the long measurement of tears, which may affect the measurement results.
While extracting the lacrimal gland, it is necessary first to locate it. The point of lacrimal gland localization is the midpoint between the front of the ear and the inner canthus. Then, cut the skin tissue under the fur, minimizing the entry of fragmented fur and reducing the handling process in the later stage. During the extraction process, it is also important to clean up the fragmented fur in a timely manner. Especially when separating the lacrimal gland, use phosphate-buffered saline (PBS) or saline to repeatedly rinse and avoid mixing with other tissues that may affect the sectioning results.
The advantage of the dry eye animal model developed is that the protocol correlated different drug concentrations with different degrees of lacrimal gland injury. This provides an experimental basis for the study of the treatment of lacrimal gland dysfunction. We have refined some of the operational steps in the modeling process to provide more detailed reference materials for a researcher. In addition, we have added analysis indicators for the dry eye animal model, incorporating morphological indicators of the cornea, conjunctiva, and lacrimal gland, counting conjunctival cells, and scoring the degree of lacrimal gland injury. We evaluated lacrimal gland function from inflammation, edema, and atrophy. We have chosen the most comprehensive, cost-effective, and accurate analysis methods to reflect the degree of dry eye and lacrimal gland dysfunction.
However, our method also has certain limitations. Due to the lengthy process of constructing animal models, experimenters need to inject repeatedly. Although there are currently some methods to replace manual injections, such as drug pumps or transdermal patches, there are still some complications in their use. How to apply better methods to reduce the frequency of medication, avoid the occurrence of complications, and ensure the accuracy of the dosage is our next goal. In conclusion, we have improved a dry eye animal model caused by scopolamine injection, providing an experimental basis for research on lacrimal gland dysfunction in ADDE.
Divulgazioni
The authors have nothing to disclose.
Acknowledgements
This study was supported by Guangdong Provincial High-level Clinical Key Specialties (SZGSP014) and Shenzhen Natural Science Foundation (JCYJ20210324125805012).
Materials
| 0.9% sodium chloride solution | SJZ No.4 Pharmaceutical | H13023201 | |
| 4% paraformaldehyde | Wuhan Servicebio Technology Co., Ltd | G1113 | |
| Absolute ethanol | Sinopharm Chemical Reagent Co., Ltd. | 10009218 | |
| Fluorescein sodium ophthalmic strips | Tianjin Yinuoxinkang Medical Device Tech Co., Ltd | YN-YG-I | |
| Hematoxylin and eosin | Nanjing Jiancheng Bioengineering Institute | D006 | |
| Neutral balsam | Beijing Solarbio Science & Technology Co., Ltd. | G8590 | |
| Paraffin | Beijing Solarbio Science & Technology Co., Ltd. | YA0012 | |
| Periodic Acid-Schiff Staining Kit | Beyotime Biotechnology | C0142S | |
| Schirmer tear test strips | Tianjin Yinuoxinkang Medical Device Tech Co., Ltd | YN-LZ-I | |
| Scopolamine hydrobromide | Shanghai Macklin Biochemical Co., Ltd | S860151 | |
| Small animal microscope | Head Biotechnology Co,. Ltd | ZM191 | |
| Xylene | Sinopharm Chemical Reagent Co., Ltd. | 10023418 |
Riferimenti
- Papas, E. B. The global prevalence of dry eye disease: A Bayesian view. Ophthalmic Physiol Opt. 41 (6), 1254-1266 (2021).
- Sy, A., et al. Expert opinion in the management of aqueous deficient dry eye disease (DED). BMC Ophthalmol. 15 (1), 133 (2015).
- Seo, Y., et al. Activation of HIF-1alpha (hypoxia inducible factor-1alpha) prevents dry eye-induced acinar cell death in the lacrimal gland. Cell Death Dis. 5 (6), 1309 (2014).
- Rahman, M. M., Kim, D. H., Park, C. -. K., Kim, Y. H. Experimental models, induction protocols, and measured parameters in dry eye disease: Focusing on practical implications for experimental research. Int J Mol Sci. 22 (22), 12102 (2021).
- Sullivan, D. A., Bloch, K. J., Allansmith, M. R. Hormonal influence on the secretory immune system of the eye: androgen regulation of secretory component levels in rat tears. J Immunol. 132 (3), 1130-1135 (1984).
- Sullivan, D. A., Allansmith, M. R. Hormonal modulation of tear volume in the rat. Exp Eye Res. 42 (2), 131-139 (1986).
- Maitchouk, D. Y., Beuerman, R. W., Ohta, T., Stern, M., Varnell, R. J. Tear production after unilateral removal of the main lacrimal gland in squirrel monkeys. Arch Ophthalmol. 118 (2), 246-252 (2000).
- Barabino, S., et al. The controlled-environment chamber: a new mouse model of dry eye. Invest Ophthalmol Vis Sci. 46 (8), 2766-2771 (2005).
- Viau, S., et al. Time course of ocular surface and lacrimal gland changes in a new scopolamine-induced dry eye model. Graefes Arch Clin Exp Ophthalmol. 246 (6), 857-867 (2008).
- Altinors, D. D., Bozbeyoglu, S., Karabay, G., Akova, Y. A. Evaluation of ocular surface changes in a rabbit dry eye model using a modified impression cytology technique. Curr Eye Res. 32 (4), 301-307 (2007).
- Daull, P., et al. Efficacy of a new topical cationic emulsion of cyclosporine A on dry eye clinical signs in an experimental mouse model of dry eye. Exp Eye Res. 153, 159-164 (2016).
- Dursun, D., et al. A mouse model of keratoconjunctivitis sicca. Invest Ophthalmol Vis Sci. 43 (3), 632-638 (2002).
- Fischer, A. H., Jacobson, K. A., Rose, J., Zeller, R. Cutting sections of paraffin-embedded tissues. CSH Protoc. 2008, (2008).
- Fischer, A. H., Jacobson, K. A., Rose, J., Zeller, R. Hematoxylin and eosin staining of tissue and cell sections. CSH Protoc. 2008, (2008).
- Shinomiya, K., Ueta, M., Kinoshita, S. A new dry eye mouse model produced by exorbital and intraorbital lacrimal gland excision. Sci Rep. 8 (1), 1483 (2018).
- Ramos, M. F., et al. Nonproliferative and Proliferative Lesions of the Rat and Mouse Special Sense Organs(Ocular [eye and glands], Olfactory and Otic). J Toxicol Pathol. 31, (2018).
- Stapleton, F., et al. TFOS DEWS II Epidemiology report. Ocul Surf. 15 (3), 334-365 (2017).
- Foulks, G. N., et al. Clinical guidelines for management of dry eye associated with Sjogren disease. Ocul Surf. 13 (2), 118-132 (2015).
- Huang, W., Tourmouzis, K., Perry, H., Honkanen, R. A., Rigas, B. Animal models of dry eye disease: Useful, varied and evolving (Review). Exp Ther Med. 22 (6), 1394 (2021).
- Brayer, J. B., Humphreys-Beher, M. G., Peck, A. B. Sjogren’s syndrome: immunological response underlying the disease. Arch Immunol Ther Exp (Warsz. 49 (5), 353-360 (2001).
- Lin, Z., et al. A mouse dry eye model induced by topical administration of benzalkonium chloride). Mol Vis. 17, 257-264 (2011).

