Functional Near Infrared Spectroscopy of the Sensory and Motor Brain Regions with Simultaneous Kinematic and EMG Monitoring During Motor Tasks
Summary
Monitoring brain activity during upright motor tasks is of great value when investigating the neural source of movement disorders. Here, we demonstrate a protocol that combines functional near infrared spectroscopy with continuous monitoring of muscle and kinematic activity during 4 types of motor tasks.
Abstract
There are several advantages that functional near-infrared spectroscopy (fNIRS) presents in the study of the neural control of human movement. It is relatively flexible with respect to participant positioning and allows for some head movements during tasks. Additionally, it is inexpensive, light weight, and portable, with very few contraindications to its use. This presents a unique opportunity to study functional brain activity during motor tasks in individuals who are typically developing, as well as those with movement disorders, such as cerebral palsy. An additional consideration when studying movement disorders, however, is the quality of actual movements performed and the potential for additional, unintended movements. Therefore, concurrent monitoring of both blood flow changes in the brain and actual movements of the body during testing is required for appropriate interpretation of fNIRS results. Here, we show a protocol for the combination of fNIRS with muscle and kinematic monitoring during motor tasks. We explore gait, a unilateral multi-joint movement (cycling), and two unilateral single-joint movements (isolated ankle dorsiflexion, and isolated hand squeezing). The techniques presented can be useful in studying both typical and atypical motor control, and can be modified to investigate a broad range of tasks and scientific questions.
Introduction
Neural imaging during functional tasks has become more portable and cost-efficient using non-invasive functional near-infrared spectroscopy (fNIRS) to identify areas of brain activity by measuring blood flow dynamics at the cortex. The portability of fNIRS is especially useful in the study of upright and functional tasks such as gait1, which is not possible with other technologies such as functional magnetic resonance imaging (fMRI). This capability is critical in the fields of neurology and neuroscience, and could provide new insights into mechanisms underlying movement disorders in children and adults with cerebral palsy (CP) and other neurological conditions affecting motor control. Understanding mechanisms improves the ability to design efficacious interventions to target the source of impairments and activity limitations.
Many fNIRS studies of motor tasks to date have been with a healthy population of adults where participants are instructed to perform a certain task and monitoring of task performance is limited to visual inspection. This can be sufficient for those with typical movements and a high level of engagement, but is not acceptable when studying participants with movement disorders or those who have difficulty attending to a task for extended periods of time, including typically developing children. In order to inform the analysis of brain activation in these cases, concurrent monitoring of the motor pattern that is actually completed is required.
Comprehensive reviews of fNIRS systems and usages have been presented in the literature2-5 that guide usage and help to demonstrate the accuracy and sensitivity of these systems, but technical issues in the collection, processing and interpretation of fNIRS data still remain. Color and thickness of hair affect quality of the optical signal, with dark thick hair most likely to block or distort optical transmission3,6. This is especially relevant when studying the sensorimotor areas located on the crown area of the head where hair follicle density is the greatest, and some studies report non-responders6,7. The well established International 10/20 system can be used for placement of the optodes, but particularly in the case of those with atypical brain anatomy, co-registration of optode location to a participant’s anatomical MRI is very useful if not essential to accurately interpret the results.
The use of fNIRS to assess brain activation in childhood-onset brain injury is fairly recent, but gaining traction in the area of unilateral cerebral palsy6,8,9. In consideration of the aforementioned challenges, this protocol combines fNIRS, motion capture, and electromyographic (EMG) monitoring during a number of tasks, including simple single-joint tasks as well as more complex full-body motions. Visual and auditory guidance is used to improve attention and task performance across multiple ages of participants. The goal of the protocol is to identify differences in brain activation patterns in those with unilateral and bilateral childhood-onset brain injury compared to those who are typically developing. We explore a full body movement (gait), a bilateral lower extremity multi-joint movement (cycling), and two unilateral single-joint movements (isolated ankle dorsiflexion, and isolated hand squeezing) to illustrate the variety of applications of the methods. The same or a very similar protocol could be used to study other sensory or movement disorders or other tasks of interest.
Continuous wave near infrared light was emitted and detected at 690 nm and 830 nm over the sensorimotor cortices using the fNIRS system at a rate of 50 Hz, using a custom designed source-detector configuration. EMG data were collected wirelessly at a frequency of 1,000 Hz. Reflective marker 3-D locations were collected by an optical motion capture system at a rate of 100 Hz. Two different computers handled data acquisition, one for the fNIRS and another for the motion capture and EMG. Data were synced using a trigger pulse from a third computer that corresponds to a mouse button press to start the instructional animation for each task. For all tasks except gait, instructional animations were designed to standardize participant performance using visual guidance of the pace of a task (1 Hz), represented by a cartoon animal jumping or kicking, as well as an auditory cue.
Protocol
NOTE: This protocol was approved by the Institutional Review Board of the National Institutes of Health (ClinicalTrials.gov identifier: NCT01829724). All participants are given the opportunity to ask questions and provide informed consent prior to their participation. In consideration of changes to the hemodynamic response caused by recent use of vasodilators and vasoconstrictors, participants are asked to refrain from alcohol and caffeine for 24 hr before the experiment3.These animation videos were custom made in our laboratory, but could be recorded with other sounds or images specific to alternative research questions.
1. Set Up the Room Prior to the Participant’s Arrival.
- Calibrate the motion capture cameras relative to a laboratory’s coordinates according to the motion capture manufacturer’s specific process. Ensure that camera positions will allow recording of all markers on both the body and head of the participant during the tasks that will be tested. The calibration process ensures accuracy of the motion capture system and is standard practice for any motion laboratory. Use a ten camera system, with an approximate volume of 17 m3 where reflective markers could be identified reliably.
- Connect the trigger from the instruction computer to the motion capture and fNIRS computers’ BNC inputs. Ensure that the trigger is connected to a mouse button, and clicking the mouse completes the circuit and sends a pulse simultaneously to the motion capture/EMG data acquisition board and to the fNIRS data acquisition board as auxillary analog inputs.
- Connect this mouse through the USB port to the computer that run instruction animation videos, such that starting the video will cause a voltage change simultaneously on both data acquisition systems.
NOTE: EMG signals are automatically synched and saved by the motion capture software, so additional synching of the EMG system is not needed. - Set up the screen and projector for instructions to be shown to the participant. Remove any unnecessary items that could be distracters. Place the tripod and digital video camera where they will have full view of the participant’s movements.
- Verify that reflective markers are securely attached to the top of each optode in the probe.
- Assemble all necessary documents: consent and assent copies, clinical examination sheets, and experimental note sheets, for example.
2. Basic Measures
- After completing the informed consent process, measure and record participant’s height, weight, age, and head circumference.
- Administer Edinburgh Handedness Inventory10 and other clinical examinations as indicated. Record participant-reported hair and skin types.
- Place reflective markers on the posterior superior iliac spines (PSIS) bilaterally. Have the participant walk at their comfortable pace across the lab 3 – 5 times, and average the speed across trials to estimate their self selected walking pace.
3. Functional Near Infrared Spectroscopy (fNIRS) Setup
NOTE: This can be completed simultaneously with the setup of EMG and motion capture, if there are enough experimenters or research staff to assist, and if the participant is comfortable with several people being close to them at the same time.
- Measure the distance between the nasion (Nz) and the inion (Iz), and between the pre-auricular points on the right (Ar) and left (Al) ears. The intersection of the midpoint of these two measures is Cz, which is marked on the scalp using a washable marker.
- If the participant has long hair, section off small portions of the hair using braids or ponytails in order to expose the scalp where optodes will be placed.
- Place the fNIRS probe onto the participant’s head, taking care to align with Cz, Ar. Then move hair away from under each optode as it is placed it on the scalp. Finally, attach velcro straps to securely hold the optodes in place.
NOTE: In this protocol, use a cap that has one strap that goes behind the head, one that goes across the forehead, and one that goes under the chin. Optodes are anchored to this cap with Velcro on a flexible plastic ring that encircles the ear.- If the participant has short hair (less than approximately 2 inches in length), pull out hair between optodes with a small thin stick or plastic end of a comb.
- Verify that all optode cables are lying flat, and that optodes are approximately perpendicular to the surface of the scalp.
- If necessary, place a thin piece of foam under the group of optode cables to promote perpendicular alignment of the optodes.
- Check with the participant about comfort of the probes, and adjust if needed. Instruct them to tell the experimenters if their comfort decreases at any point during the experiment.
- Turn on sources and check the signals.
- In this system, ensure a signal that has an intensity of at least 80 dB and a heartbeat clearly visible in the deltaOD (change in optical density) signal, at both 690 and 830 nm wavelengths. When channels have signals not meeting these criteria, confirm that hair is not blocking the optode(s) and then adjust detector gains as needed to maximize the signal intensity. Ensure that motion capture cameras are off during this time.
NOTE: Other fNIRS machines may operate at wavelengths different to 690 and 830 nm; in this case, check the wavelengths most appropriate to the machine being used.
- In this system, ensure a signal that has an intensity of at least 80 dB and a heartbeat clearly visible in the deltaOD (change in optical density) signal, at both 690 and 830 nm wavelengths. When channels have signals not meeting these criteria, confirm that hair is not blocking the optode(s) and then adjust detector gains as needed to maximize the signal intensity. Ensure that motion capture cameras are off during this time.
- Add reflective markers to Nz, Iz, Ar, and Al. Ask the participant to hold still and collect approximately 2 sec of motion capture data for these and the fNIRS optode markers. Verify that all markers have been recorded, and collect additional trials as necessary. It may require the participant to change head position to improve line of sight between the cameras and the markers. Use these collected three dimensional locations during analysis for probabilistic registration of a participant’s individual structural MRI if one is available.
- Add a cover with several layers of black felt or other optically absorbent material on top of the fNIRS optodes to protect detectors from interference or saturation from the motion capture cameras. Ensure that the cables and front panel of the fNIRS unit are also well shielded using the same optically absorbent material.
4. Surface Electromyography (EMG) Setup
- Locate the muscle belly of each targeted muscle using anatomical landmarks, palpation during muscle contraction, and electrode placement guides11.
NOTE: The muscles targeted in this protocol include bilateral medial gastrocnemius, tibialis anterior, rectus femoris, vastus lateralis, biceps femoris, extensor carpi radialis, and flexor carpi radialis. - Prepare for EMG electrode placement over the muscle belly by shaving, removing dead skin cells with tape, and then cleaning with an isopropyl alcohol pad, as recommended by SENIAM12 and wait for skin to dry.
- Place EMG electrode oriented to the direction of the muscle fibers.
- Wrap snugly with a self adherent wrap.
- Check muscle signals on the computer while performing manual muscle testing to ensure proper electrode placement, and clear visualization of signal change when the muscle is active.
5. Motion Capture Setup
- Place reflective markers at joint landmarks. These include medial and lateral malleolus, medial and lateral knee joint, anterior superior iliac spine (ASIS), posterior superior iliac spine (PSIS), radial styloid, ulnar syloid, medial humeral epicondyl, and lateral humeral epicondyl.
- Place 3 or more markers, or a rigid body cluster of markers, onto each segment of interest, including the foot, shank, thigh, hand, and forearm.
- Collect approximately 2 sec of motion capture data while the participant is standing still in a standardized position, such as standing with arms at 90° shoulder flexion and 90° elbow flexion. Ensure that all markers are clearly visible to the cameras.
6. Gait Task
- Have the participant transfer to the treadmill. Assist them by supporting the fNIRS optode cables and then secure the cables to the ceiling support after the patient is in position. If patient is at high risk for falls, use a body weight support harness for safety during this task.
- Start the treadmill, slowly building up to the measured self selected walking speed to get the participant comfortable with the set up conditions. Then slow to a stop again.
- Set up the animation file with the auditory feedback that will cue the participant to either rest or move. Review task instructions with the participant, telling them to remain as still and relaxed as possible during “rest” periods and to walk at the treadmill’s set speed during the “task” period, while focusing their attention to the small black circle on the screen for the duration of data acquisition.
- Dim the lights, and begin data acquisition on the motion capture computer and the fNIRS computer. Begin recording on the video camera.
- Using the mouse trigger, click the play button on the animation file associated with this task. Make sure that the trigger was received by both the motion capture and the NIRS systems.
- Switch to an image of a black dot located in the participant’s line of sight, so that they have a focus point for the duration of the trial.
NOTE: The overview schematic for each trial is shown in Figure 2.
- Switch to an image of a black dot located in the participant’s line of sight, so that they have a focus point for the duration of the trial.
- Monitor participant performance and provide feedback about speed, or extraneous voluntary movements as needed.
- At the end of the instructional animation, stop recording on the motion capture, EMG, and fNIRS systems, as well as the video camera. Give the participant an opportunity to rest or shift positions as necessary.
7. Bilateral Lower Extremity Cycling Task
- Have the participant transition to a plinth with movable back and leg support, taking care to support the fNIRS optode cables and to not bump or dislodge the motion capture markers or EMG electrodes. Have a foam seat cushion to improve comfort during the experiment.
- Lift the cycle frame into position and secure it to the plinth with a strap.
- Secure the feet into the pedals and adjust the position of the cycle as necessary to promote a comfortable and natural distance to the pedals. At the furthest point in the cycle, maintain their knee in approximately 10° of flexion.
NOTE: At this point, the participant will be in a semi-recumbent posture, which provides some trunk support and facilitates relaxation during the rest period. - Review task instructions with the participant, telling them to remain as still and relaxed as possible during “rest” periods and to cycle at approximately 60 rpm during the “task” period.
- Repeat steps 6.4 to 6.7. Instead of switching to an image of a dot, project the cartoon animation that will cue the participant to either rest or move through visual and auditory feedback. Maximize the movie window so that the participant is not able to monitor the time that has passed, or is remaining, in the current trial.
8. Hand Squeezing Task
- After removing the feet from the cycle and the cycle itself, place a bed table in front of the participant, making sure that participant’s arms are supported on the table at a comfortable position.
- Instruct participant to squeeze a soft object approximately once per sec (1 Hz) during the “task” period, and remain as relaxed as possible during “rest” periods.
- Repeat step 7.5.
9. Ankle Dorsiflexion Task
- Remove the bed table, and raise the foot rest portion of the plinth up to bring the feet into the participant’s view.
- Remove the participant’s shoe and sock, and replace foot markers in appropriate positions. Support the calf just above their ankle joint with a foam pad to allow ankle joint movement.
- Instruct the participant to dorsiflex their ankle approximately once per sec (1 Hz) during the “task” period, and remain as relaxed as possible during “rest” periods.
- Repeat step 7.5.
10. Conclusion of Protocol
- Remove the cap and inspect skin for areas of pressure or redness.
- Remove all reflective markers and EMG units.
- Thank the participant for their time and invite their input about the subjective experience of the protocol. This can be a formal questionnaire (as used by Garvey and colleagues for transcranial magnetic stimulation13), or an informal discussion to identify common sources of discomfort that could be improved in the future.
Representative Results
This protocol coordinates concurrent acquisition of 3 modalities to capture brain blood flow, electrical muscle activity, and kinematic movement of joints while a participant performs motor tasks (Figure 1).
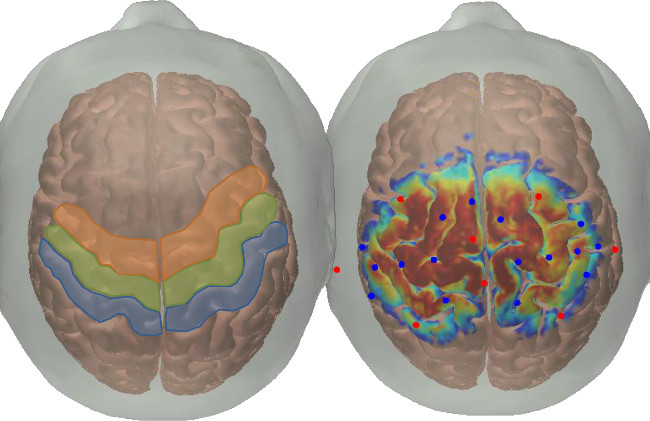
Figure 1. Probe location. The left portion of this figure shows the approximate locations of the sensory areas (in blue, Brodmann areas 1,2,3), the primary motor area (in green, Brodmann area 4), and the premotor area (in orange, Brodmann area 6). The right portion of this figure was generated using AtlasViewerGUI (available for open source download from the MGH Optics Division15) and its associated functions. In brief, this probe design was registered to the surface of the Colin47 Atlas using the spatial arrangement of sources, detectors, and anatomical landmarks (sources are represented by red circles and detectors by blue circles). A Monte Carlo photon migration forward model was run for launching 1 x 108 photons of light through the materials of the skin, skull, and brain, with the sensitivity profiles for all source-detector pairs are projected to the surface of the cortex and all displayed simultaneously in this figure. The color map on the brain’s surface represents the cortical sensitivity of the probe; in other words the number of simulated photons that reach the gyri and sulci located under the sources and detectors (warmer colors indicate more photons than cooler colors, with a range of 2 orders of magnitude on a log 10 scale).
shows an example of source-detector arrangement used in this protocol, and how it is related to underlying neuroanatomical structures on a brain atlas. Figure 2 outlines the block design used in this protocol, as well as screen shots of the instruction videos. Tasks are performed in a block design, with eight 15 sec task blocks interspersed with random length rest periods of 20 – 30 sec. Cartoon animals were specifically chosen to be non human like so as to not engage the mirror neuron system11, and audio cues have been shown to improve task performance in other block design experiments10. The gait task had only an auditory cue, and participants were asked to focus on a small black circle projected onto a screen in front of them.
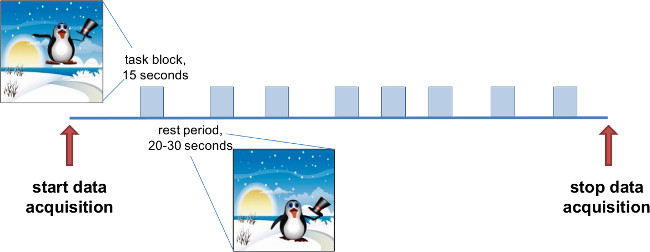
Figure 2. Schematic of each trial. Data collection for each task type lasts approximately 6 min. There are periods of variable rest (ranging between 20 and 30 sec in duration), with 15 sec blocks of activity (gait, cycling, dorsiflexion, or squeezing). Instructional videos were created with visual and auditory cues for the participant to rest or move. The penguin images are taken from one of the instruction videos shown to the patient. He remains on the ground during the rest periods, and jumps in the air 1 time per sec during the task periods. There is also music provided for each condition, a relaxing tune playing during rest and a tune with a strong 60 bpm pace during the task blocks.
Figure 3 is an example of the optical signals recorded during task performance. Data are automatically saved to a file with a *.nirs extension and later transferred from the data acquisition computer for further processing. Figure 4 shows an example of the reconstructed skeletal model, along with joint angle and EMG measures for an ankle dorsiflexion task. The skeletal model and joint angles are created and calculated using Nexus and Visual3D software packages. These data, as well as the EMG have not been processed, and could contain motion artifacts or other noise that could benefit from filtering techniques.
There are a wide array of analysis techniques and software packages available to interpret the data collected. One example is completing fNIRS image reconstruction using an open source software package called HOMer14. An example of the map created is shown in Figure 5 to demonstrate the type of activation information that can be interpreted from the collected optical density signals.
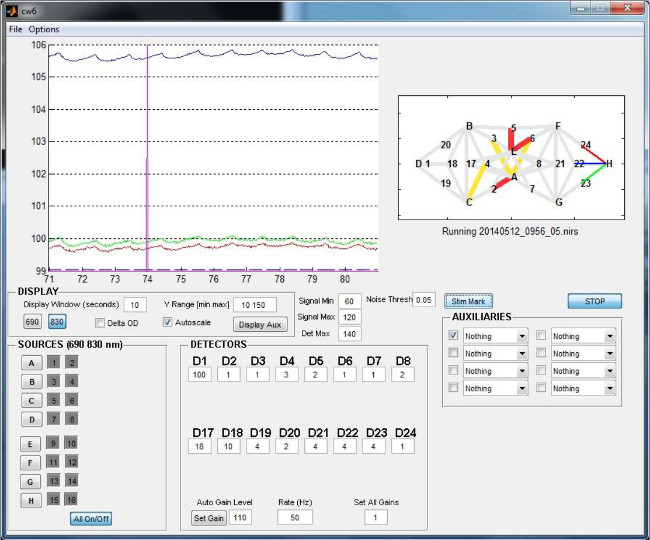
Figure 3. Example of optical density recordings. This screen shot is from the data acquisition software of one type of fNIRS machine. It includes information about the fNIRS probe arrangement (upper right), ability to turn individual laser sources on and off (lower left), and options for modifying the gain of each dectector (bottom middle). In the data visualization window (top left), the vertical pink line represents the start of a block of activity. Colors of the traces correspond to the colors of the channels shown in the probe arrangement on the right. Note that all signals are above 80 dB, and the heart rhythm is clearly visible, even in the light intensity signal.
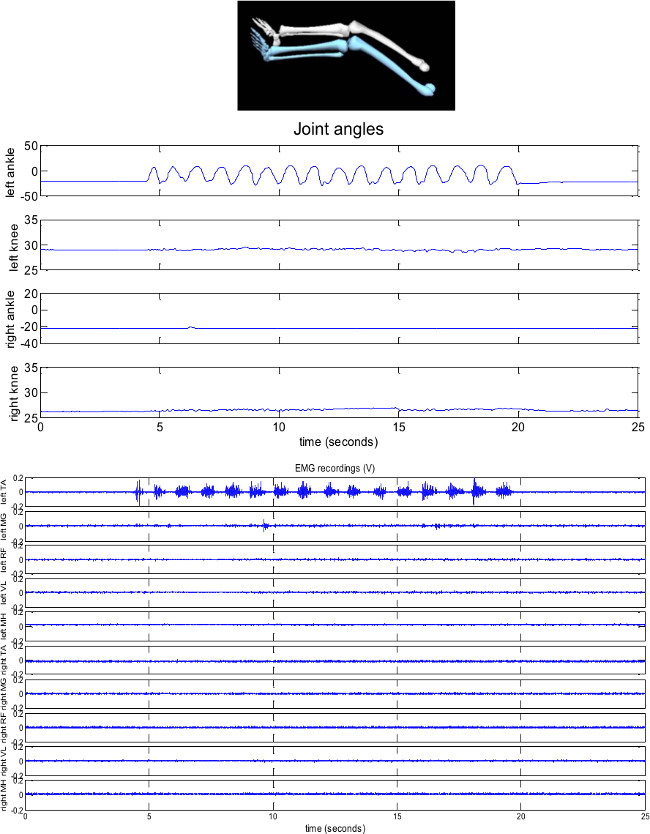
Figure 4. Example skeletal reconstruction, joint angles and EMG for a left dorsiflexion task. The task period during the period represented begins at approximately 4.5 sec, and continues until 19.5 sec. In this typically developing individual (13 years old), there is very limited movement at joints other than the targeted left ankle. In addition, muscles other than the one providing the motion (tibialis anterior) are generally quiescent during the task as well as rest periods. TA = tibialis anterior; MG = medial gastrocnemius; RF = rectus femoris; VL = vastus lateralis; MH = medial hamstrings.
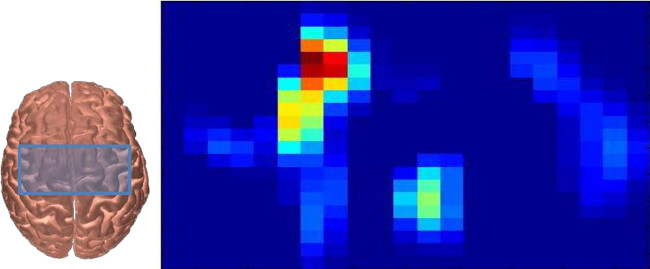
Figure 5. Example of fNIRS activation map during a right handed squeezing task. The blue box on top of the brain outlines the approximate area sampled by this probe design (see also Figure 1). This participant was 13 years old, and had a head circumference of 56 cm). The right portion of the figure shows the average oxygenated hemoglobin (HbO) response during the period 5 – 10 sec following movement onset of one typically developing adolescent squeezing a ball with their right hand. This data in this figure are generated from HOMer14, and then evaluated using a general linear model. The blue colors represent no activation, while the red areas indication regions of increased HbO during the task periods. This is one method of analysis and visualization that researchers use to identify areas of greater changes in oxygenated and/or deoxygenated blood flow.
Discussion
Simultaneous collection of brain activity from targeted areas of the cortex and quantitative data about how a person is moving presents tremendous potential for improving our understanding of the neural control of movement, both in a typically developing population as well as those with movement disorders. There is also broad application in terms of ages and movement tasks that could be completed, as participants are not restricted to a supine position as they would be for a functional MRI. The specific equipment items are not limited to ones suggested in the materials list – there are several motion capture and motion quantification systems, EMG systems, and fNIRS systems available in the market, and they could be used in place of the ones suggested here. In addition, if a chosen motion capture system does not have sufficient volumes of measurement to localize markers on both the body and the head or non-optical technology is used, a 3-D position tracking stylus can be used instead to locate the optodes with respect to anatomical landmarks in a common coordinate system. Finally, if it is possible to additionally collect physiological data such as heart rate and blood pressure, this information would be useful to inform analysis of HbO and HbR time series.
The entire protocol can be completed in approximately 2 hr, with almost half of that time dedicated to setup. For male participants with short hair, the setup time may be less because less time is needed to prepare the hair. It is important for investigators to recruit without bias from all ethnicities and hair types, and to report if there are individuals where useful signals could not be obtained3. Depending on the age and attention span of the person being tested, additional tasks or additional blocks of data collection could be easily added. It is important to note, however, some limitations of fNIRS technology in its current state. Despite careful preparation and care to reduce hair interference, there may be some participants where the melanin content of their hair and skin precludes collection of signals with appropriate intensity. Even among those with adequate intensity, there will be variability in the clarity of the hemodynamic response observed. These issues need to be dealt with during data analysis, with clear reporting of how non-responders were identified and disclosure of the number of participants tested whose data could not be used2-5.
This particular protocol can be adapted in a number of ways for application to specific research questions. The orientation of the sources and detectors has infinite possibilities in terms of locations and arrangements, which provide the flexibility to sample other areas of the cortex, create a denser probe with additional channel overlap in order to facilitate greater resolution, or a more sparse arrangement to cover larger areas of the cortical surface. The overall spatial resolution of fNIRS remains lower compared to fMRI, but this limitation may be outweighed by the ability to use fNIRS in a less confined environment for many research applications, particularly when studying movement tasks. Furthermore, any number of motor, sensory, or imagery tasks could be feasibly incorporated into the presented block design including more complex sequences or other simple single joint movements. In consideration of lower extremity tasks, however, thought must be given to the location of the distal lower extremity representation on the motor homunculus as it may not be possible to get that deep with a surface based approach such as fNIRS. In addition, there are studies that also use an event-related paradigm16,17, which could easily be integrated by altering the animations and instructions to participants. These paradigms require a larger number of movement blocks, but they can be completed with less rest in between so the total data acquisition time may not differ significantly from the presented block paradigms.
Kinematic and EMG data can be used in a number of ways. Qualitatively, it provides a useful confirmation that the participant was completing a task as instructed. Particularly in cases where movements are not as expected, due to decreased attention or the presence of a movement disorder, these signals can be very valuable as quantitative methods of removing blocks of data, or as regressors in a general linear model (GLM) analysis of the data, as shown by Hervey et al.18. Determining coordinates of fNIRS optodes and anatomical landmarks is necessary for co-registration to a participant’s individual structural MRI. Co-registration of optode locations represents an important step in increasing the reliability and neuro-anatomical relevance of fNIRS findings, especially in populations with brain injuries. Finally, one could consider adding tracking of cable motion as an additional step to account for movement artifacts within the recorded data.
Childhood-onset brain injuries such as cerebral palsy are known to cause a number of peripheral symptoms such as spasticity, muscle weakness, and reduced selective motor control19. Passive electrophysiological or brain imaging techniques such as transcranial magnetic stimulation20,21 and diffusion tensor imaging22,23 have shown alterations in cortical organization. fMRI has been useful in detecting differences in activation in small isolated movements24-26, but monitoring task performance can be a challenge in the MRI environment, and even small motion of the head can cause large artifacts. In this population in particular, complementary or concurrent use of neuroimaging modalities such as fNIRS or electroencephalography (EEG) presents an opportunity to gain a greater understanding about the underlying source of movement problems, and an additional tool for monitoring progress related to motor interventions.
Divulgazioni
The authors have nothing to disclose.
Acknowledgements
This project was funded by the Intramural Research Program at the National Institutes of Health Clinical Center. We acknowledge the helpful discussions with Dr. Thomas Bulea, PhD and Laurie Ohlrich, PT in refining the procedures presented in this protocol. Muyinat W. Osoba and Andrew Gravunder, MS assisted with the animations.
Materials
| Name of Reagent/ Equipment | Company | Catalog Number | Comments/Description |
| CW6 | TechEn | http://nirsoptix.com/ | fNIRS machine with variable number of sources and detectors, depending on the number of modules included |
| MX system with ten T40-series cameras | Vicon Motion Systems Ltd., Oxford, UK | http://www.vicon.com/System/TSeries | Motion capture cameras |
| reflective 4 mm markers | Vicon Motion Systems Ltd., Oxford, UK | n/a | Markers used by the motion capture cameras to locate fNIRS optodes, Ar, Al, Nz, and hand coordinates. |
| reflective 9.5 mm markers | Vicon Motion Systems Ltd., Oxford, UK | n/a | Markers used by the motion capture cameras to locate arm and leg coordinates. Clusters are used for the limb segments, and markers with offsets are uses for PSIS and Iz to improve reliability in data capture. |
| Trigno Wireless EMG system | Delsys, Inc. Natick, MA | http://www.delsys.com/products/wireless-emg/ | Electromyography |
| Bertec split-belt instrumented treadmill | Bertec Corporation, Columbus, OH | http://bertec.com/products/instrumented-treadmills.html | Treadmill |
| ZeroG body-weight support system | Aretech, LLC, Ashburn, VA | http://www.aretechllc.com/overview.html | Track and passive trolley used to support cables, harness can be used for patient safety during gait trials |
| 3DS Max 2013 | Autodesk, Inc., San Francisco, CA | http://www.autodesk.com/ | 3-D animation software used to animate animals for instructional videos |
| Windows Movie Maker | Microsoft Corporation, Redmond, WA | http://windows.microsoft.com/en-us/windows-live/movie-maker | software used to combine animation footage with music |
| Audacity | open source | http://audacity.sourceforge.net/ | Software used to alter musical beat to appropriate cadence |
Riferimenti
- Suzuki, M., et al. Prefrontal and premotor cortices are involved in adapting walking and running speed on the treadmill: an optical imaging study. Neuroimage. 23 (3), 1020-1026 (2004).
- Leff, D. R., et al. Assessment of the cerebral cortex during motor task behaviours in adults: a systematic review of functional near infrared spectroscopy (fNIRS) studies. Neuroimage. 54 (4), 2922-2936 (2011).
- Orihuela-Espina, F., Leff, D. R., James, D. R., Darzi, A. W., Yang, G. Z. Quality control and assurance in functional near infrared spectroscopy (fNIRS) experimentation. Phys Med Biol. 55 (13), 3701-3724 (2010).
- Pellicer, A., Bravo Mdel, C. Near-infrared spectroscopy: a methodology-focused review. Semin Fetal Neonatal Med. 16 (1), 42-49 (2011).
- Wolf, M., Ferrari, M., Quaresima, V. Progress of near-infrared spectroscopy and topography for brain and muscle clinical applications. J Biomed Opt. 12 (6), 062104 (2007).
- Tian, F., et al. Quantification of functional near infrared spectroscopy to assess cortical reorganization in children with cerebral palsy. Opt Express. 18 (25), 25973-25986 (2010).
- Koenraadt, K. L., Duysens, J., Smeenk, M., Keijsers, N. L. Multi-channel NIRS of the primary motor cortex to discriminate hand from foot activity. J Neural Eng. 9 (4), 046010 (2012).
- Khan, B., et al. Identification of abnormal motor cortex activation patterns in children with cerebral palsy by functional near-infrared spectroscopy. J Biomed Opt. 15 (3), 036008 (2010).
- Tian, F., Alexandrakis, G., Liu, H. Optimization of probe geometry for diffuse optical brain imaging based on measurement density and distribution. Appl Opt. 48 (13), 2496-2504 (2009).
- Oldfield, R. C. The assessment and analysis of handedness: the Edinburgh inventory. Neuropsychologia. 9 (1), 97-113 (1971).
- Delagi, E. F., Perotto, A. Anatomic guide for the electromyographer–the limbs. , (1980).
- Hermens, H. J., Freriks, B., Disselhorst-Klug, C., Rau, G. Development of recommendations for SEMG sensors and sensor placement procedures. J Electromyogr Kinesiol. 10 (5), 361-374 (2000).
- Garvey, M. A., Kaczynski, K. J., Becker, D. A., Bartko, J. J. Subjective reactions of children to single-pulse transcranial magnetic stimulation. J Child Neurol. 16 (12), 891-894 (2001).
- Huppert, T. J., Diamond, S. G., Franceschini, M. A., Boas, D. A. HomER: a review of time-series analysis methods for near-infrared spectroscopy of the brain. Appl Opt. 48 (10), 280-298 (2009).
- Boas, D. A. . HOMER2. , (2012).
- Jasdzewski, G., et al. Differences in the hemodynamic response to event-related motor and visual paradigms as measured by near-infrared spectroscopy. Neuroimage. 20 (1), 479-488 (2003).
- Plichta, M. M., et al. Event-related functional near-infrared spectroscopy (fNIRS): are the measurements reliable. Neuroimage. 31 (1), 116-124 (2006).
- Hervey, N., et al. Photonic Therapeutics and Diagnostics IX. SPIE. , (2013).
- Sanger, T. D., Delgado, M. R., Gaebler-Spira, D., Hallett, M., Mink, J. W. Classification and definition of disorders causing hypertonia in childhood. Pediatrics. 111 (1), 89-97 (2003).
- Eyre, J. A., et al. Is hemiplegic cerebral palsy equivalent to amblyopia of the corticospinal system. Ann Neurol. 62 (5), 493-503 (2007).
- Maegaki, Y., et al. Central motor reorganization in cerebral palsy patients with bilateral cerebral lesions. Pediatr Res. 45 (4 pt 1), 559-567 (1999).
- Hoon, A. H., et al. Sensory and motor deficits in children with cerebral palsy born preterm correlate with diffusion tensor imaging abnormalities in thalamocortical pathways. Dev Med Child Neurol. 51 (9), 697-704 (2009).
- Yoshida, S., et al. Quantitative diffusion tensor tractography of the motor and sensory tract in children with cerebral palsy. Dev Med Child Neurol. 52 (10), 935-940 (2010).
- Lotze, M., Sauseng, P., Staudt, M. Functional relevance of ipsilateral motor activation in congenital hemiparesis as tested by fMRI-navigated TMS. Exp Neurol. 217 (2), 440-443 (2009).
- Phillips, J. P., et al. Ankle dorsiflexion fMRI in children with cerebral palsy undergoing intensive body-weight-supported treadmill training: a pilot study. Dev Med Child Neurol. 49 (1), 39-44 (2007).
- Wilke, M., et al. Somatosensory system in two types of motor reorganization in congenital hemiparesis: topography and function. Hum Brain Mapp. 30 (3), 776-788 (2009).

