Low-Cost, Volume-Controlled Dipstick Urinalysis for Home-Testing
Summary
Dipstick urinalysis is a quick and affordable method of assessing one’s personal state of health. We present a method to perform accurate, low-cost dipstick urinalysis that removes the primary sources of error associated with traditional dip-and-wipe protocols and is simple enough to be performed by lay users at home.
Abstract
Dipstick urinalysis provides quick and affordable estimations of multiple physiological conditions but requires good technique and training to use accurately. Manual performance of dipstick urinalysis relies on good human color vision, proper lighting control, and error-prone, time-sensitive comparisons to chart colors. By automating the key steps in the dipstick urinalysis test, potential sources of error can be eliminated, allowing self-testing at home. We describe the steps necessary to create a customizable device to perform automated urinalysis testing in any environment. The device is cheap to manufacture and simple to assemble. We describe the key steps involved in customizing it for the dipstick of choice and for customizing a mobile phone app to analyze the results. We demonstrate its use to perform urinalysis and discuss the critical measurements and fabrication steps necessary to ensure robust operation. We then compare the proposed method to the dip-and-wipe method, the gold standard technique for dipstick urinalysis.
Introduction
Urine is a non-invasive source of multiple metabolic indicators of disease or health. Urinalysis, the physical and/or chemical analysis of urine, can be performed quickly to detect renal disease, urinary tract disease, liver disease, diabetes mellitus, and general hydration1. Urinalysis dipsticks are affordable, semi-quantitative diagnostic tools that rely on colorimetric changes to indicate approximate physiological levels. Each dipstick can perform a wide variety of assays including testing for pH, osmolality, hemoglobin/myoglobin, hematuria, leukocyte esterase, glucose, proteinuria, nitrite, ketone, and bilirubin2. The principle of dipstick urinalysis relies on the occurrence of a timed reaction through which a color change on the dipstick pad can be compared to a chart to determine analyte concentration3. Given their affordability and ease of use, dipsticks are one of the most common tools for urinalysis in healthcare.
Traditionally, dipstick urinalysis relies on a trained nurse or medical technician to manually insert the dipstick into a cup of urine sample, wipe off excess urine, and compare the color pads to chart colors at specific times. While the dip-and-wipe method is the gold standard for dipstick analysis, its reliance on human visual assessment limits the quantitative information that can be obtained. Moreover, the two manual steps of dipstick urinalysis – the dip-wipe step and colorimetric result comparison – require accurate technique, which limits the possibility of reliable testing in home settings by patients directly. Cross-contamination of the sample pads due to wiping can cause inaccurate color changes. Additionally, inconsistent volumes resulting from the lack of volume control during wiping can result in improper measurement of analyte concentrations. Importantly, the time between dipping the urine (i.e., the start of the assay) and comparison to a chart is critical for accurate analysis of the results and is a huge potential source of human error. The difficulty in manual colorimetric comparison is that many pads must be read at the same time, while some pads are read at different times. Even perfectly timed color comparisons still depend on the visual acuity of the human reader, who may suffer from color blindness or perceive different colors in different lighting environments4. These challenges underscore why clinicians can only rely on dipstick urinalysis performed by trained personnel. However, an automated urinalysis system could address all the aforementioned concerns by eliminating the need for manual dip-wipe steps, incorporating timing controls, and enabling simultaneous color comparisons with calibrated color references. This, in turn, would reduce user error, allowing for possible adoption in home settings.
In the last 20 years, automatic analyzers have been employed to read the results of dipstick urine tests with the same accuracy as or exceeding visual analysis5. Many clinics and doctor offices use such machines to rapidly analyze and print traditional dipstick results. Most urinalysis machines minimize visual inspection errors and ensure consistency in results6. They are easy to use and more efficient than manual inspection but still require the user to perform the dip-wipe method correctly. Hence, these machines have limited ability to be operated by untrained persons such as at-home users; moreover, they are extremely expensive.
Recently, cell phones have emerged as a resourceful tool for various biological colorimetric measurements7,8,9,10, including for urinalysis11,12,13. Given their remote sensing capabilities and high imaging resolution, cell phones have become effective healthcare analytical devices14,15. Indeed, the FDA has cleared several smartphone-based home urine tests16,17,18. Some of the new smartphone-based commercial products incorporate established urinalysis dipsticks, while others feature proprietary colorimetric pads. All such products feature proprietary methods to calibrate for different lighting conditions across different phones types. Still, a problem with these solutions is that the user must manually take a picture at the right time in addition to carrying out a proper manual dip-wipe method (i.e., without cross-contamination). Notably, none of these tests control the volume deposited onto the dipsticks, which we have found can affect the color change19 and interpreted physiological result. The present gaps and costs in the workflows of these devices suggest an additional need to enable a human-free, volume-controlled urine deposition procedure and hands-free dipstick photography.
We describe a protocol for volume-controlled, automated dipstick urinalysis without the need for a manual dip-wipe step. The key to the automated process is a device19 whose underlying principle is based on the SlipChip20 and that transfers liquid between different layers using surface chemistry effects. In brief, the hydrophobic coating on the transfer slide and surrounding plate sleeve force the liquid to move effortlessly through the device and to release onto the dipstick pad once the slide is in its final position, at which point the bottom hydrophobic barrier is replaced with air. Additionally, the coordinated light-blocking box standardizes the lighting conditions, camera angle of view, and the distance for camera focus to ensure accurate and repeatable results that are not influenced by ambient lighting conditions. An accompanying software app automates the capture of images and colorimetric analysis. Following description of the protocol, we provide representative results of the urinalysis test under different conditions. Comparisons with the standard dip-wipe method demonstrate reliability of the proposed method.
Protocol
1. Fabricate and assemble the urinalysis device
- Fabricate the base plate (Figure 1A).
- Use a computer-aided design (CAD) software to draw a rectangular area with dimensions 2.1641 in x 0.0547 in x 6.3828 in (W x H x L) using the polyline tool.
- Measure the test area (rectangular area encompassing the distance between the first and last pad and the width of the pads) on the dipstick.
NOTE: This information is needed to draw the through-holes that hold the dipstick in place and separate the liquid in between the pads (to prevent cross-contamination). - Add through-holes that mimic the size and position of each test pad in the test area.
- Draw two raised side ledges that measure 2.1641 in x 0.6797 in (W x L).
- Draw a stop (0.1172 in by 0.2109 in (W x L)) using the polyline tool to facilitate alignment between the base plate and the slide. The stop should be perpendicular to the ledges and physically stops the slide from moving passed the urine dipstick pads.
- Select the lines for the stop and ledge to make one region using the Region command. Use the Extrude command to raise the region up to a height of 0.0703 in. Repeat this step on the other side of the device.
- Create a notch (0.1895 in by 0.3500 in (W x L)) on both ledges to facilitate alignment with the box. Position it 0.466 in from the bottom edge of the ledge. Use the Region command to create a rectangle and make the extrusion height 0.1250 in.
- Use the Solid Subtract command, select device, press Enter, select the notch region and press Enter. Repeat on the other side of the device.
NOTE: The shape will be removed from the device. - Print the base plate on a 3D printer and sand the top face area between the ledges with sandpaper to roughen the surface.
NOTE: Sanding is important so that the hydrophobic coating can adhere to the base plate securely. - Tape the ledges with adhesive tape (to avoid spraying the ledges) and spray the base plate with a hydrophobic spray. Apply several (4-8) coats of the basecoat to the base plate. Hold the can approximately 8-12 inches away from the base plate when spraying. The device should have a milky white appearance upon drying.
CAUTION: Follow manufacturer instructions for appropriate location and PPE for spraying. - Wait 30 minutes before applying the topcoat several times (6-8x). Allow the base plate to dry for 12 hours before use. Remove the tape from the ledges.
- Fabricate the top plate (Figure 1B).
- Draw a rectangular area to measure 2.05 in x 5.470 in (W x L) in a CAD software using the polyline tool.
- Add a rectangular through-hole (the “viewing through-hole”) slightly larger than the size of the test area of the dipstick (e.g., 0.230 in x 3.147 in (W x L)). Place it 0.921 in from the top, 1.165 in from the left, and 1.165 in from the right edges of the top plate.
- Draw a second through-hole (the “Inlet-hole”) sized 0.075 in x 3.146 in (W x L). Place it 0.236 in from the bottom edge, 1.737 in from the top edge, and 1.162 in from the left and right edges of the top plate.
- Cut the top plate from a piece of clear acrylic with a laser cutter. Wipe off any remaining dust or debris.
- Fabricate the inlet cover (Figure 1B).
- Draw a rectangular area with dimensions 0.247 in x 3.3378 in (W x L) in a CAD software using the polyline tool. Add two circular through-holes with a diameter of 0.127 in approximately 0.073 in from the two edges of the inlet cover, one on either side.
- Cut the inlet cover from a piece of clear acrylic with a laser cutter.
- Fabricate the slide (Figure 1C)
- Draw a rectangular area in CAD software that measures measure 2.771 in x 0.0625 in x 5.000 in (W x H x L) using the polyline tool.
- Add through-holes that match the position of each test pad in the test area. Draw the first 0.105 in square through-hole to overlap with the placement of the first test pad: 1.096 in from the left and right edges of the slide, 0.960 in from the top edge, and 1.681 in from the bottom edge. Add more through-holes as needed (usually 10 total) for the selected dipstick brand of choice. Space each next through-hole by measuring the distance between test pads on the dipstick.
NOTE: The size of the through-holes is important in order to deposit the correct volume of liquid onto the dipstick pad. For our brand of dipstick, we created holes which deposit 15 ul onto each dipstick pad. - Cut the slide from a piece of clear acrylic using a laser cutter. Wipe off any remaining dust or debris.
- Spray the front of the slide with a hydrophobic spray. Apply several coats (6-8x) of basecoat to the slide. Hold the can approximately 8 -12 in away from the slide when spraying.
- Wait 30 minutes before applying the topcoat several times (8-12x). Allow the slide to dry for 12 hours before use.
- Download a QR code from an online QR code generator and print the desired code on paper with sticky adhesive backing. Place the QR code 0.17 in from the right of the first through-hole along the same row as all the through-holes.
NOTE: As long as the QR code is adjacent to the through-holes, accurate placement is not important. - Use clear tape to cover the QR code and secure it to the slide.
- Assemble the inlet and plate sleeve (Figure 1D).
- Fabricate the inlet by using acrylic cement to glue the inlet cover onto the top plate where the inlet-hole is located. Wait 24-48 hours to securely bond the pieces.
- Spray the back of the top plate with a hydrophobic spray once the inlet cover is securely bonded to the top plate. Place the top plate upside down. Apply the first basecoat several times (4-8x).
- Hold the spray 8-12 inches away from the top plate and wait 30 minutes for it to dry. Apply the topcoat several times (6-8x). Allow the top plate to dry for 12 hours before use.
- Assemble the plate sleeve (combined top plate and base plate) by gluing the completed top plate to the ledges of the base plate with acrylic cement. The two pieces are easy to align by visual inspection, as the bottom edge of the top plate will align with that of the base plate. Apply a clamp to the base plate ledges to secure it during drying and wait 24-48 hours before use, as per the manufacturer’s instructions.
- Create the chart sticker.
- Download the color chart for the brand of dipstick from the manufacturer’s website.
- Open the downloaded file in a graphics editor software.
- Open the digital file for the top plate template previously used for the laser cutter (Step 1.2 of this protocol) in a graphics editor software.
- Create the color boxes for the chart sticker by matching color boxes from the manufacturer color chart. Select the first block of color on the manufacturer’s chart with the dropper tool in the graphics editor software and then use the box shape tool to make a box shape in the same color on the top plate template, in the same row where the dipstick pad will be located. Repeat this for each color block corresponding to each pad row.
- Delete the layers associated with the top plate template.
- Print the chart sticker as a vinyl sticker with an online sticker print service. Place the chart sticker onto the plate sleeve and align it with each through-hole.
- Fabricate the box (Figure 1E).
- Draw the two long-sided box pieces (parts “a” and “b”) in the CAD software as rectangles with dimensions of 4.92 in x 6.63 in (W x L). Add a cut-out to part “a” centered on the bottom edge measuring 0.2 in x 6.11 in (W x L).
- Draw the two narrow-sided box pieces (parts “d” and “e”) in the CAD software as rectangles with dimensions measuring 1.805 in x 6.63 in (W x L).
- Draw the box top (part “c”) as a rectangle with dimensions 1.805 in x 6.63 (W x L). Draw the “imaging through-hole” on the top: 0.74 in x 0.910 in (W x L), positioned 3.17 in from the bottom, 2.53 in from the top, 0.65 in from the right edge, and 0.42 in from the left edge.
NOTE: The exact position of the imaging through-hole should be selected on the basis of the cell phones that will be used for the analysis. - Draw each box piece to feature a pattern of interlocking edges that will allow all the box sides to snap together on each edge as described in Figure 1D. To make an interlock edge pattern, alternate an extrusion/intrusion pattern on the long edge with 0.135 in by 1.17 in (W x L) protrusions. Draw two extrusions on each long edge for every side of the box. Use the same extrusion/intrusion pattern for the short edge, but with intrusions measuring 0.135 in by 0.460 in (W x L).
- Cut the five pieces with a laser cutter or print them with a 3D printer.
NOTE: A laser-cut component using acrylic pieces will be cheap to manufacture and can be flattened for easy shipping. Use black acrylic as it is helpful to absorb scattered light during testing. - Add black color construction paper to the box interior to prevent scatter from the flash during image analysis if the box material has a gloss finish.
2. Prepare the test
- Download the UrineTest mobile application from GitHub (https://github.com/Iftak/UrineTestApp).
- Install the app onto a mobile phone.
NOTE: This step only has to be done once for all future uses of a given phone. If needed, enable developer status on the phone to do this. - Launch the UrineTest application in the phone (Figure 2A).
- Read the instructions to change the analyte names and reading timings (Figure 2B) to match those for the dipstick of interest (based on the manufacturer’s specifications) and insert new input via the text holder window on the screen (Figure 2C).
NOTE: The necessary readout time for each dipstick pad will depend on the brand of the dipstick used. - Assemble the various components together and insert the dipstick into the through-holes underneath the plate sleeve (Figure 1F).
- Place the plate sleeve inside the box so that its notch is aligned with the box gap.
- Place the slide inside the plate sleeve so that its through-holes align with the inlet.
- Place the phone on the top of the box with the back-camera lens facing the viewing through-hole to enable imaging. Ensure the camera visibility is not occluded by checking for the image on the phone screen prior to testing. The app will enable the flashlight on the phone automatically.
- Read the instruction for phone alignment (Figure 2D) and align the phone accordingly so that the dipstick coincides with the boundaries of the black rectangular overlay on screen (Figure 2E).
- Click the Start button on the app window to begin the test.
NOTE: This will open the phone camera to read the QR code once in view (Figure 2F).
3. Conduct the test
- Deposit urine into the inlet hole with a disposable polyethylene transfer pipet containing approximately 0.5 mL of urine (Figure 3).
NOTE: The exact amount of liquid is not important, but it should be at least 0.5 mL to ensure that all the through-holes receive sufficient urine. Upon adding the liquid, observe that it moves across inlet and is deposited in each through-hole of the slide. - Initiate the test by pushing the slide into the plate sleeve until it is stopped by the base plate stop.
NOTE: Urine should make contact with dipstick pad when the QR code is in the field of view of the cell phone. After reading the QR code, the application will open a window to analyze the color changes (Figure 2G) and show the results automatically within the same window (Figure 2H). - Discard the urine appropriately and clean the plate sleeve and slide with 10% bleach solution and rinse again with de-ionized water. Allow it to dry before additional use.
Representative Results
Figure 4 demonstrates how the urine is transferred to the dipstick during a urinalysis test. During a typical test, the transfer of urine is not observable because the box occludes the view. Once the sample is deposited in the inlet using a pipette (Step 3.1), it will fill the holes on the slide (Figure 4A). Figure 4B and Figure 4C, respectively, show the progressive movement of the urine across the plate sleeve and after the slide makes contact with the stop. Note that contact of the urine with the dipstick leads to a colorimetric reaction and color change on the dipstick pads.
Figure 5 demonstrates a potential problem that can arise if the surfaces for transferring the urine (i.e., base pate, top plate and slide) are not sufficiently coated with hydrophobic spray. An illustration of a well and poorly coated slide is shown in Figure 5A. If poorly coated, one may observe streaks (shown by white arrows in Figure 5B) during the sliding step that decrease the accuracy of the volume transferred. In addition, one may observe failure of the slide to transfer the urine to the dipstick (Figure 5C), and urine may remain in the through-holes even when the slide is removed from the device. These steps highlight the importance of obtaining good spray coverage (Steps 1.1.8, 1.4.4, 1.5.3, and 1.5.4). If there are concerns about the spray coverage or if you observe these performance errors, it is best to remake the base plate, top plate and slide.
A urinalysis test was performed with a high-quality smartphone: phone 1 (image resolution: 8000-pixels x 6000-pixels). Representative results are shown in Figure 6. We conducted tests with de-ionized water and commercial urine (both standard composition and with high glucose). The color pads on the dipstick change in time in response to the colorimetric reaction of the urine with the analytes in the dipstick. The error bars in Figure 6 represents the standard deviation yielded for three consecutive measurements of each sample recorded by the two smartphones. Figure 6A plots the response for the glucose pad over time for the different test conditions. For the brand of dipstick used, the recommended readout time for the glucose measurement is 30 seconds. As expected, the color of the dipstick does not change over this interval for water, the final value for the standard urine matches with the “normal” urinary glucose threshold level (160-180 mg/dL), and the final value for the “high glucose” condition is elevated above the normal value. Importantly, note that the correct value is not attained until 30 seconds, which illustrates the importance of setting the timing readout interval correctly in Step 2.8. The same experiment was performed with another smartphone having a lower image resolution: phone 2 (image resolution: 3264-pixels x 2448-pixels). Due to the difference in camera resolution, a significant difference from the previous results is observed in the image color and quality while capturing images of the dipstick panel, as shown in Figure 6B. The differences in flashlight specifications also contribute to the differences in image quality. From Figure 6, it can be seen that both phones yield similar trends in the change of color over time, though the actual colors detected are different. The color matching algorithm used by the smartphone application for the urinalysis test yields the same results for the analyte concentrations, despite differences in the physical appearance of the colors of the dipstick pads. The consistency of the results is due to the use of the chart sticker as a reference chart for the analysis. Since both the chart sticker and the dipstick are captured under the same lighting conditions and image quality, the smartphone application evaluates the (R,G,B) components and the color difference of both the reference square and dipstick pad in a similar fashion for both smartphones. These results confirm that the protocol described in this manuscript is independent of the smartphone model, as long as both the reference color chart and the dipstick are imaged under the same environment.
We have previously evaluated the accuracy of the automated urinalysis device by comparing with traditional dip-and-wipe methods using a commercial urine standard19. Table 1 compares the results obtained with the two tests. It can be seen that the accuracy of the system depends on the volume transferred to each dipstick pad. The most accurate results were obtained when the automated urinalysis device was designed to transfer 15 μL of urine; therefore, it is crucial that the device transfer the required urine volume accurately and consistently to the dipstick pads. Representative results to validate the consistency of the device by transferring 15 μL volume of urine samples over seven different trials are shown in Figure 7. The overall standard deviation was found to be below 0.5 μL, which is within 4% range of the target value. The results confirm that the device is able to accurately and consistently transfer microliters of urine to perform the test.
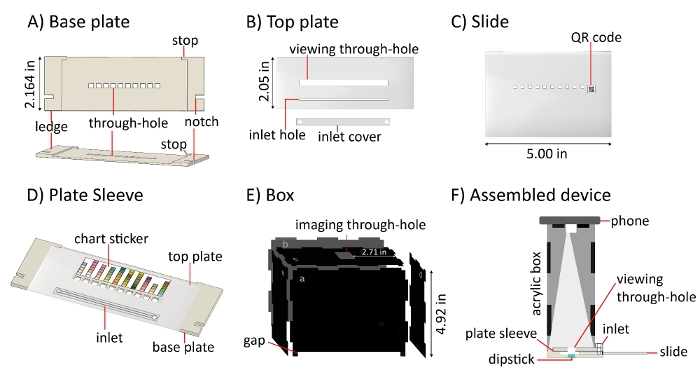
Figure 1: Schematic drawings of device components. A) Base plate. B) Top plate and inlet cover, which are glued together in Step 1.5.1. C) Slide and associated QR code used for timing control. D) Plate sleeve, formed by gluing the top plate to the ledges of the base plate in Step 1.5.4. The chart sticker next to the viewing through-hole enables color analysis. E) Box. F) Assembled device. During use, a mobile phone is placed on the top of the box such that its lens and flashlight are positioned above the imaging through-hole. Please click here to view a larger version of this figure.
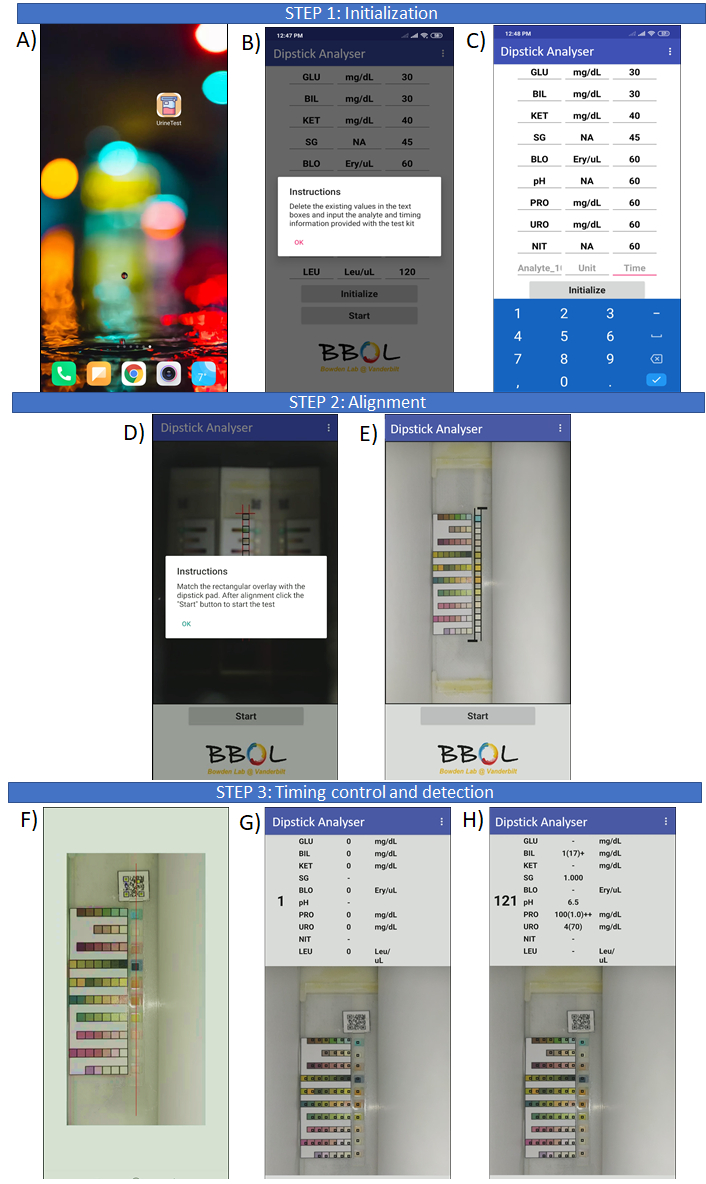
Figure 2: The process of the colorimetric analysis using the app. A) The icon on the phone screen “Urine test” is selected to launch the application. B) A pop-up window informs the user to modify the readout times. C) The user manually enters the analyte name and readout times. D) A pop-up window to inform the user for phone alignment. E) Representative image of a properly aligned dipstick before testing. F) Screenshot after the slide is inserted and the QR code appears to initiate data acquisition. G) The screen one second after starting the test. The black square overlays show the user the exact location from where the app is collecting pixel information. H) The results of the completed dipstick test. Test results with dashes are considered normal for the chosen dipstick. Please click here to view a larger version of this figure.
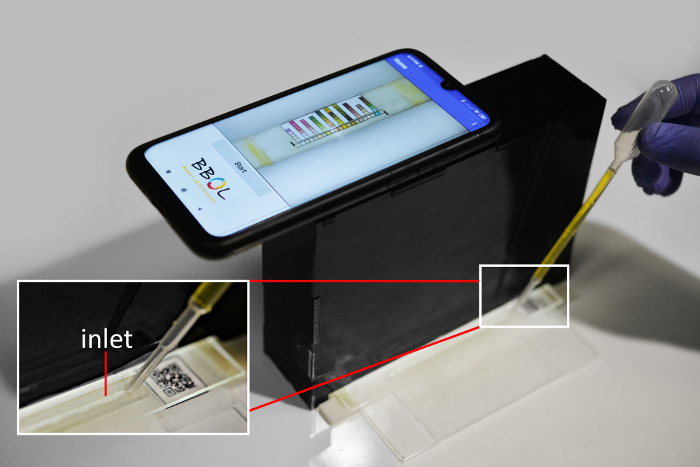
Figure 3: Photograph of the assembled device in action at the start of a urinalysis test. A user begins the test by inserting a pipette with urine into the inlet. Please click here to view a larger version of this figure.
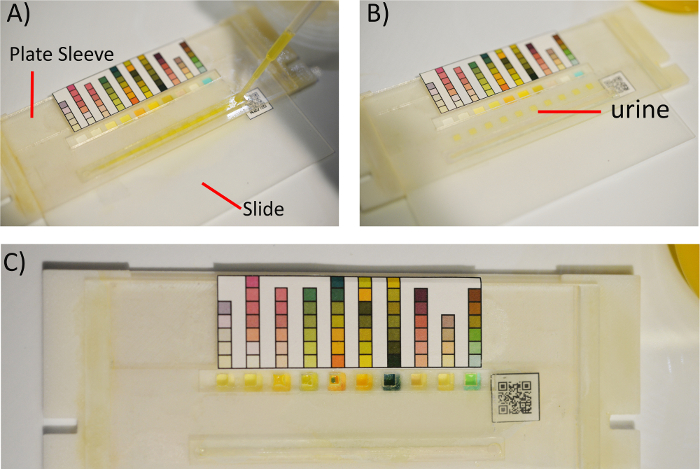
Figure 4: Internal process of liquid deposition onto the dipstick test from start to finish. A) Inserting the slide into the plate sleeve and aligning the slide through-holes with the inlet will allow the transfer pipette to deliver the urine into each through-hole of the slide. B) Slipping the slide through the interior of the hydrophobic coated plate sleeve enables liquid transport. C) When the slide reaches the stop in the baseplate, urine is delivered to the test pads, resulting in colorimetric changes. Please click here to view a larger version of this figure.
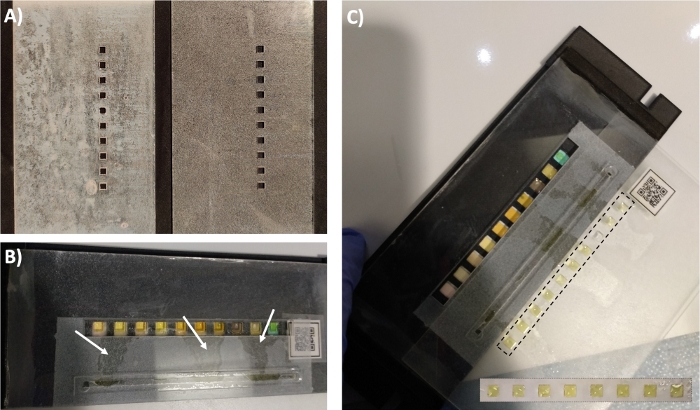
Figure 5: Potential problems associated with insufficient hydrophobicity. A) A slide with and without sufficient coating. B) Insufficiently coated slide shows leaking during the sliding step. C) An insufficiently coated slide does not transfer onto the dipstick pads even after being pulled back out of the device: the liquid remains in the slide through-holes, as seen in the inset on the bottom right. Please click here to view a larger version of this figure.
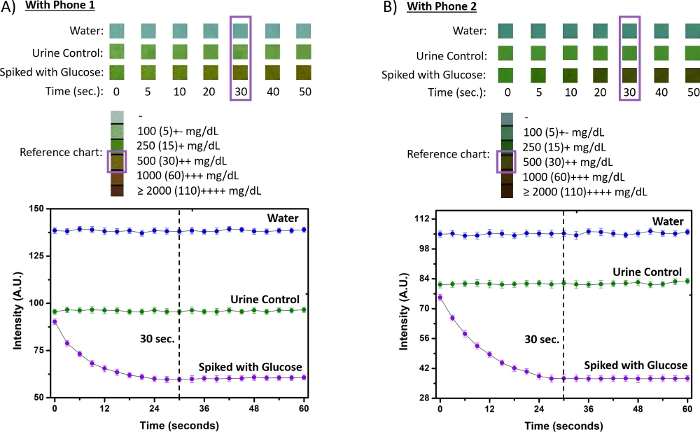
Figure 6: Urinalysis result for the glucose pad with two different smartphones for three types of samples. A) Response characteristics of the glucose pad over time for the different test conditions recorded with a high-camera-resolution camera phone (phone1). B) Response characteristics of the glucose pad over time for the different test conditions recorded with a low-resolution camera phone (phone 2). The readout at 30 seconds corresponds with the desired timing for the manufacturer. Please click here to view a larger version of this figure.
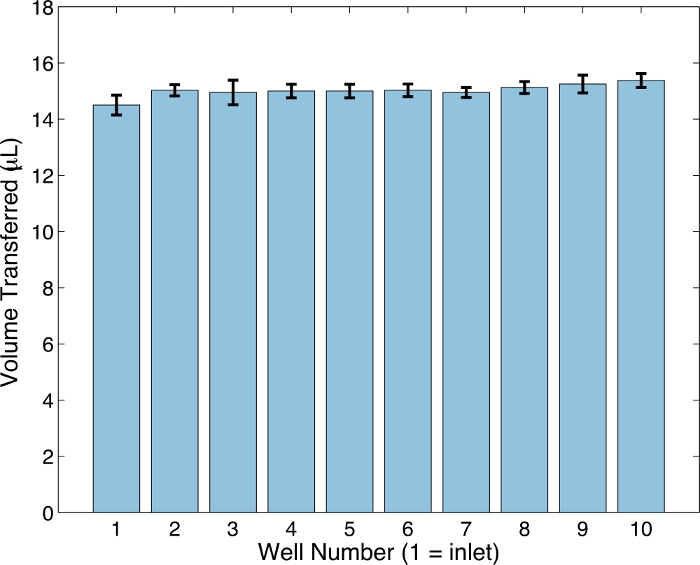
Figure 7: Well number vs average volume transferred. Each well corresponds to a through-hole for a given test pad; the first well is closest to the inlet. This figure has been modified from Smith, et al.19 and reproduced with permission from the Royal Society of Chemistry. Please click here to view a larger version of this figure.
| Analyte | Differences from dip-and-wipe | |||||||||
| LEU | NIT | URO | PRO | pH | BLO | SG | KET | GLU | ||
| Dip-and-wipe | 4 ± 0 | 2 ± 0 | 4 ± 0.53 | 2 ± 0.53 | 4 ± 0 | 5 ± 0 | 3 ± 0.53 | 4 ± 0.49 | 3 ± 0.58 | n/a |
| 5 µL | 3*± 0 | 2 ± 0 | 3* ± 0 | 3* ± 0.49 | 3* ± 0 | 3* ± 0 | 2* ± 0.53 | 4 ± 0.38 | 1* ± 0 | 7 |
| 10 µL | 3* ± 0.38 | 2 ± 0 | 4 ± 0 | 2 ± 0 | 3* ± 0.38 | 4* ± 0 | 1* ± 0.49 | 4 ± 0.49 | 2 ± 0.58 | 5 |
| 15 µL | 4 ± 0 | 2 ± 0 | 4 ± 0.49 | 2 ± 0 | 4 ± 0.38 | 5 ± 0 | 2* ± 0.38 | 4 ± 0.49 | 3 ± 0.49 | 1 |
| 20 µL | 4 ± 0 | 2 ± 0 | 4 ± 0.82 | 2 ± 0.53 | 4 ± 0.53 | 5 ± 0 | 2* ± 0.49 | 4 ± 0.49 | 3 ± 0 | 1 |
Table 1: Median values and standard deviations for analytes using various deposited volumes. The symbol ‡ indicates median values that differ from the median obtained with the dip-and-wipe method, the industry standard. The total number of analyte pads whose medians differ from the dip-and-wipe method are reported in the far right column. Note results are cumulative for all dipsticks used. LEU: leukocytes, NIT: nitrite, URO: urobilinogen, PRO: protein, BLO: blood, SG: specific gravity, KET: ketones, GLU: glucose. This table has been modified from Smith, et al.19 and reproduced with permission from the Royal Society of Chemistry.
Discussion
Traditional dipstick urinalysis is affordable and convenient but requires manual attention to detail to yield accurate results. Manual dipstick urinalysis is subject to variable lighting conditions, individual color perception differences and cross-contamination. Many clinics and hospitals already have instruments to automate urine dipstick analysis, but the instruments are usually bulky, expensive, and still rely on proper performance of the dip-wipe method. Additionally, these instruments require yearly calibration and maintenance for accurate results.
The protocol automates and controls several important steps involved with dipstick urinalysis (e.g., distribution of liquid to the test pads, the timing of the start, control over the lighting and quantitative comparison with the reference standard), which is necessary to obtain reliable results. To this end, critical steps in the protocol relate to the design of the device include steps 1.4.3, 1.1.4, 1.4.7 and 1.1.5, which match the size of the through-holes to the desired volume, ensure proper placement of the stops to align the through-holes with the dipstick, ensure proper placement of the QR code used as the timing indicator and ensure that the test is not influenced by ambient light, respectively. In addition, the transfer of urine through the slide and subsequent deposition onto the dipstick are highly dependent on the surface characteristics of the materials being used. Hence, if non-hydrophobic surfaces are used for the base plate, the top plate and the slide, it is important to apply an adequate amount of hydrophobic spray. It is especially critical to ensure that the inner surfaces of the through-holes of the slide have been sprayed so that the liquid will drop to the dipstick pad after slipping.
The protocol can be easily modified to use with other brands of dipsticks by changing the dimensions and spacing of the through-holes. The volume applied to the dipstick can also be modified by changing the thickness of the acrylic used to fabricate the slide (with commensurate changes in the thickness of the ledges of the base plate) or the size of the through-holes. The accompanying software app allows the user to modify the names and readout timings to align with those for the brand of dipstick used.
The current device combines a 3D-printed base plate and laser-cut top plate to form a plate sleeve. Both of these fabrication methods are affordable, and the material choices can be modified. Excluding the phone and dipstick, the acrylic used in the current device costs approximately $0.85, and material used in the 3D-printed base plate costs around $1.50 per device. Although the base plate we used is 3D-printed from acrylonitrile butadiene styrene (ABS), other polymers that form a hard and rigid surface are also suitable. For example, a version of the device can be made using a plate sleeve completely fabricated from acrylic19. Elastomeric materials such as polydimethylsilioxane (PDMS) are not desirable because their lower rigidity is less compatible with sliding a glass surface to enable the slipping action that is critical to the volume-control design.
One important limitation of the current protocol is that the hydrophobic coating applied to the slide and plate sleeve may peel with frequent use, limiting the stability of the device over time. After 3-4 test runs, the hydrophobic coatings often peel and alter the volume transferred, potentially reducing the accuracy in results. Future method modifications can include the use of more durable hydrophobic coating or materials that are naturally hydrophobic. Additionally, the acrylic bonding may weaken during repeated testing as well. The low cost of the device, however, allows multiple prints to be made and re-glued together as needed. Thus, the slide may be considered as a reusable part.
Another limitation is the inability to saturate the glucose pad with urine due to the hydrophobic nature of the pad. As such, it only partially absorbs liquid with the automated device. We did not find that this reduced the accuracy of the result, but it does require careful execution of Step 2.9 to ensure the camera viewing area captures data from the middle, not the edges of the glucose test pad. Future work may address this issue by incorporating a different brand of dipstick that does not feature hydrophobicity on any dipstick reagent pads on the test.
By controlling the major steps contributing to user error, this method allows for increased accuracy in results performed by non-trained individuals and is suitable for home testing. Unlike other urinalysis apps available7,8,9, the system is modifiable to any brand of dipstick test. The device is reusable and requires no power to use outside of power consumed by the smartphone. In the future, we envision that the protocol could be amenable to patient self-testing. By ensuring the accuracy in dipstick test results, patients may monitor their own urine more frequently without the barriers associated with standard clinical urinalysis practice.
Divulgazioni
The authors have nothing to disclose.
Acknowledgements
This work was funded by the Dorothy J. Wingfield Phillips Chancellor Faculty Fellowship. Emily Kight was funded by NSF GRFP.
Materials
| Black Cast Acrylic Sheet 12" x 24" x 1/8" |
McMaster Carr | 8505K742 | $14.27 |
| Chart sticker | Stickeryou.com | $12.39 | |
| Clear Scratch- and UV-Resistant Cast Acrylic Sheet 12" x 24" x 1/16" |
McMaster Carr | 8560K172 | $9.52 |
| disposable polyethylene transfer pipet | Fischer Brand | 13-711-9AM | lot# 14311021 |
| Fortus ABS-M30 | Stratasys | 345-42207 | lot# : 108078 |
| Githut: https://github.com/Iftak/UrineTestApp | |||
| Innovating Science – Replacement Fluids for Urinalysis Diagnostic Test Kit (IS3008) | Amazon | $49 | |
| Nonwhitening Cement for Acrylic Scigrip 4, 4 oz. Can |
MCM | 7517A1 | $9.22 |
| Rust-Oleum 274232 Repelling treatment base coat-9 oz and top-coat 9-oz , Frosted Clear | Amazon | Color: Frosted Clear | $6.99 |
| Urinalysis Reagent Strips 10 Panel (100 Tests) MISSION BRAND | Medimpex United, Inc | MUI-MS10 | $10.59 |
Riferimenti
- Lei, R., Huo, R., Mohan, C. Expert Review of Molecular Diagnostics Current and emerging trends in point-of-care urinalysis tests. Expert Review of Molecular Diagnostics. 00, 1-16 (2020).
- Kavuru, V., et al. Dipstick analysis of urine chemistry: benefits and limitations of dry chemistry-based assays. Postgraduate Medicine. 5481, (2019).
- Pugia, M. J. Technology Behind Diagnostic Reagent Strips. Laboratory Medicine. 31, 92-96 (2000).
- Dungchai, W., Chailapakul, O., Henry, C. S. Electrochemical detection for paper-based microfluidics. Analytical Chemistry. 81, 5821-5826 (2009).
- Van Delft, S., et al. Prospective, observational study comparing automated and visual point-of-care urinalysis in general practice. BMJ Open. 6, 1-7 (2016).
- . Urisys 1100 Analyzer Available from: https://diagnostics.roche.com/us/en/products/instruments/urisys-1100.html (2020)
- Filippini, D., Lundström, I. Measurement strategy and instrumental performance of a computer screen photo-assisted technique for the evaluation of a multi-parameter colorimetric test strip. Analyst. 131, 111-117 (2006).
- Shen, L., Hagen, J. A., Papautsky, I. Point-of-care colorimetric detection with a smartphone. Lab on a Chip. 12, 4240-4243 (2012).
- Ra, M. Smartphone-Based Point-of-Care Urinalysis under Variable Illumination. IEEE Journal of Translational Engineering in Health and Medicine. 6, 1-11 (2018).
- Yetisen, A. K., Martinez-Hurtado, J. L., Garcia-Melendrez, A., Da Cruz Vasconcellos, F., Lowe, C. R. A smartphone arebeorithm with inter-phone repeatability for the analysis of colorimetric tests. Sensors and Actuators, B: Chemical. 196, 156-160 (2014).
- Wang, S., et al. Integration of cell phone imaging with microchip ELISA to detect ovarian cancer HE4 biomarker in urine at the point-of-care. Lab on a Chip. 11, 3411-3418 (2011).
- Zhang, D., Liu, Q. Biosensors and bioelectronics on smartphone for portable biochemical detection. Biosensors and Bioelectronics. 75, 273-284 (2016).
- Choi, K., et al. Smartphone-based urine reagent strip test in the emergency department. Telemedicine and e-Health. 22, 534-540 (2016).
- Kwon, L., Long, K. D., Wan, Y., Yu, H., Cunningham, B. T. Medical diagnostics with mobile devices: Comparison of intrinsic and extrinsic sensing. Biotechnology Advances. 34, 291-304 (2016).
- Vashist, S., Schneider, E., Luong, J. Commercial Smartphone-Based Devices and Smart Applications for Personalized Healthcare Monitoring and Management. Diagnostics. 4, 104-128 (2014).
- . Inui Available from: https://www.inuihealth.com/inui/home (2020)
- . Healthy.io Available from: https://healthy.io/ (2020)
- . Scanwell Available from: https://www.scanwellhealth.com (2020)
- Smith, G. T., et al. Robust dipstick urinalysis using a low-cost, micro-volume slipping manifold and mobile phone platform. Lab on a Chip. 16, 2069-2078 (2016).
- Du, W., Li, L., Nichols, K. P., Ismagilov, R. F. SlipChip. Lab on a Chip. 9, 2286-2292 (2009).

