Technical Considerations and Approach to Redo Foregut Surgery
Summary
Redo foregut surgery is associated with increased patient morbidity and presents a technical challenge for the surgeon. We describe our approach and considerations when performing a redo hiatal hernia repair to provide a guide for other surgeons and improve patient outcomes.
Abstract
Foregut surgical techniques have advanced significantly over the years and have become increasingly popular. However, new challenges and technical considerations have arisen when dealing with reoperation for complications or surgical failure. This study focuses on the technical considerations and approach when dealing with reoperative foregut surgery, particularly redo hiatal hernia repair. We describe our approach starting from the preoperative workup to the procedural steps of the surgery. The present study describes the main steps for robotic reoperative hiatal hernia repair in a patient who had previously undergone laparoscopic hiatal hernia repair with Nissen fundoplication but did not present a recurrence of reflux and dysphagia symptoms. The patient is positioned supine with arms out and a footboard for steep Trendelenburg. We place six trocars, including an assistant port and a liver retractor port, to facilitate visualization and retraction. After docking the robot, we use a combination of electrocautery and sharp dissection to free the hernia sac and reduce the hiatal hernia. The previous fundoplication is then taken down carefully and the esophagus is mobilized through a transhiatal approach with a combination of blunt and sharp dissection until at least 3 cm of intra-abdominal esophageal length is achieved, after which a leak test is performed. We then perform a crural repair to reapproximate the hiatus with two posterior stitches and one anterior stitch. Lastly, a redo Nissen fundoplication is performed over a bougie, and endoscopy is used to confirm a loose stack-of-coin appearance. By emphasizing the crucial steps of redo hiatal hernia repair, including preoperative evaluation, our goal is to provide an approach for the foregut surgeon to maximize patient outcomes.
Introduction
Over the past century, improvements in the understanding and diagnosis of foregut disorders have led to the evolution of better procedures and surgical approaches. This innovation brings new challenges related to complications and reoperation for the foregut surgeon. Surgical reinterventions are particularly challenging from a technical perspective due to multiple factors, including dense adhesions, scarring, obliteration of tissue planes, and altered anatomy1,2,3,4,5. These redo foregut surgeries have increased morbidity in patients with higher incidences of esophageal perforation, delayed gastric emptying, and vagal nerve injury1,6,7,8. Mesh repairs at the hiatus complicate reintervention further, having higher rates of major resection requiring complex reconstruction9,10. The advent of advanced endoscopic therapies creates ever-evolving challenges for foregut surgeons when dealing with their associated complications or failures11,12,13. Furthermore, redo foregut operations are associated with worsening success rates and patient satisfaction with successive reoperations compared with primary intervention14,15,16,17. This highlights the importance of patient selection and accurate diagnosis prior to redo surgery for optimal outcomes.
While traditionally performed using an open approach, laparoscopic approaches to redo foregut surgery are safe and efficacious14,18. However, due to the greater difficulty associated with altered anatomy and adhesions, conversion to open surgery is still a possibility. With the emergence of robot-assisted surgery in urology and gynecologic surgery19,20, the superior visualization and dexterity compared to laparoscopy would appear to likely have some benefit in redo foregut surgery as well. Indeed, emerging research has shown safety and improved outcomes, including less conversions to open surgery and decreased hospital stays compared with the laparoscopic approach for redo foregut surgery21,22,23.
Although it is ultimately up to the foregut surgeon to determine the safest procedure, this article aims to demonstrate the approach and technical considerations for redo foregut surgery to provide a "framework" when confronted with this challenge. While a robotic-assisted approach is described, the principles described could be similarly applied to laparoscopy.
Protocol
The protocol and methods described here were approved and followed the ethical guidelines of the Institutional Review Board (IRB) of the University of Minnesota. Described here is a reoperative hiatal hernia repair and takedown of a previous Nissen fundoplication in a 73-year-old woman. The patient presented to the clinic with a history of laparoscopic hiatal hernia repair and a fundoplication 5 years ago at an outside hospital for epigastric pain and fullness after meals. She also complained of significant reflux and dysphagia with solid food intake. Her symptoms had temporarily resolved after the first surgery but had now recurred. Of note, her body mass index (BMI) at the time of consultation was 40. No previous preoperative workup could be obtained prior to the consultation. The patient provided written informed consent before redo foregut surgery.
1. Patient preparation and operative set-up
- Preoperative workup and testing
- Discuss the possibility of reoperation and proceed with a thorough workup as mentioned:
- Perform an esophagram. The esophagram of this patient showed moderate to severe esophageal dysmotility (Figure 1).
- Perform endoscopy. For this patient, upper endoscopy showed no stenosis or strictures but demonstrated a portion of the stomach herniating upward through the diaphragm on a retroflexed view, which confirmed a hiatal hernia.
- Perform computed tomography of the abdomen. This test also confirmed a herniated wrap (Figure 2).
- Perform wireless esophageal pH testing. This showed a DeMeester score24,25 of 38.4 with borderline symptom association probability for acid reflux.
- Perform high-resolution manometry. In this patient, it showed a nonspecific motility disorder.
- Discuss the possibility of reoperation and proceed with a thorough workup as mentioned:
- Preoperative planning
- Ensure initial recommendations include weight loss and hence referral to a bariatric surgeon if needed.
NOTE: The patient did well with the weight loss program and could bring down her weight to a BMI of 32. At this point, she continued to have symptoms, and her case was discussed at the multidisciplinary esophageal conference for operative planning. The consensus was that the manometric findings were likely due to reflux and hernia and that a reoperative hernia repair with a loose fundoplication would be appropriate.
- Ensure initial recommendations include weight loss and hence referral to a bariatric surgeon if needed.
- Anesthesia
- Perform anesthesia following institutional guidelines. Intubate the patient with a single lumen endotracheal tube with rapid sequence intubation because of the risk of aspiration from reflux and a hiatal hernia. She had an arterial line for hemodynamic monitoring.
- Positioning
- Position the patient supine with her arms out and a footboard to facilitate steep reverse Trendelenburg positioning26. The chest and abdomen are always prepped into the field for foregut surgeries to have adequate access to the abdomen and chest if needed.
- Port placement and docking
- Use the open Hasson technique27 to enter the peritoneal cavity in the left supra-umbilical space. Insert the camera port here.
- Insert two more 8 mm ports in the left upper quadrant and one 8 mm port in the right upper quadrant. Place the ports about 10 cm above the umbilicus and ensure a handbreadth space between the ports.
- Place the assistant port in the right lower quadrant. Insert the liver retractor (see Table of Materials) through a 5 mm port placed in the extreme lateral portion of the right upper quadrant.
NOTE: It is the authors' preference to place a left-sided chest tube during surgery because the hernia sac tends to be tethered to the pleura, especially in reoperative surgeries. - Perform this before starting the dissection to minimize the chances of having to undock and reposition during the operation if there are significant hemodynamic changes from a pneumothorax that develops acutely during dissection.
- Dock the robot (see Table of Materials).
2. Surgery procedure
- Reducing hiatal hernia
- Remove the adhesions of the bowel to the abdominal wall and open the gastrohepatic ligament using a robotic bipolar surgical energy device.
- Open the lesser sac by removing adhesions and additional short gastric artery branches.
- Dissect the hernia sac circumferentially at the hiatus using a combination of blunt and electrocautery dissection with the robot.
- Dissect the dense adhesions between the liver and stomach carefully with laparoscopic scissors (see Table of Materials).
- Takedown of previous fundoplications.
NOTE: Some but not all sutures from the previous wrap were visible.- Perform sharp dissection with laparoscopic scissors and undo the wrap to completely free the stomach.
- Carefully stay in the thin scar tissue to avoid damage to the stomach or esophagus.
- Esophageal mobilization
- Mobilize the esophagus transhiatally in the mediastinum. Perform this with a combination of blunt and sharp dissection and minimize the use of energy close to the esophagus.
- Next, confirm at least 3 cm of intraabdominal esophagus length. Use endoscopy to locate the gastroesophageal junction (GEJ) and measure the esophagus from the hiatus to the GEJ to confirm the adequate length.
- Leak test
- Perform endoscopy and visualize the mucosa clearly to ensure no injuries. Fill the upper abdomen with warm water and insufflate the esophagus and stomach to ensure no air leakage.
- Hiatal repair
- Perform crural repair using 0-silk sutures with two posterior crural stitches and one anterior crural stitch.
- Pass a 56 Fr bougie (see Table of Materials) into the esophagus, and with the bougie in place, pass a grasper comfortably into the hiatus. This is to ensure that the crural repair was not too tight.
- Nissen fundoplication
- Bring the fundus across the right side, posterior to the esophagus, and under the vagus nerve.
- Pass a 58 Fr bougie (see Table of Materials) into the esophagus.
- Perform a loose fundoplication over the bougie with three 2-0 silk sutures.
NOTE: Endoscopy confirmed a loose stack of coin-like appearance.
- Gastropexy and G tube
- Insert a percutaneous endoscopic gastrostomy tube into the stomach to serve as a gastropexy and a venting tube.
3. Follow-up procedure
- Postoperatively, administer antiemetics to minimize the risk of postoperative nausea and vomiting as retching can disrupt the hernia repair or cause early recurrence.
- Initially, the gastric tube is left open to serve as a vent to prevent gastric distention. Eventually, clamp it on postoperative day 2 or 3 once the patient is tolerating liquids.
- Provide the patient with ice chips on the night of surgery. On postoperative day 1, ask the patient to start with sips of clear liquids with the gastric tube still open. On postoperative day 2, initiate a clear liquid diet and if the patient tolerates well, clamp the gastric tube.
NOTE: If tolerating clear liquids while clamped, a full liquid diet is started. - Finally, instruct the patient on the advancement to a soft diet after 1 week with plans for clinic follow-up in 4 weeks with an esophagram and plans for gastric tube removal if not requiring significant venting.
Representative Results
The patient had an uneventful postoperative course. She slowly advanced to a full liquid diet over a period of 3 days and was then discharged on a liquid diet with instructions to advance to a soft diet after 1 week.
By virtue of being a quaternary referral center and a major university hospital, we frequently manage patients needing reoperative foregut surgery. Our data from the last 5 years with 43 patients undergoing reoperative hiatal hernia repairs showed a mean length of stay of 7 days and a 23% 30-day complication rate. The outcomes are summarized in Table 1. Most published data on reoperative hiatal hernias show similar outcomes1,2,6,18.
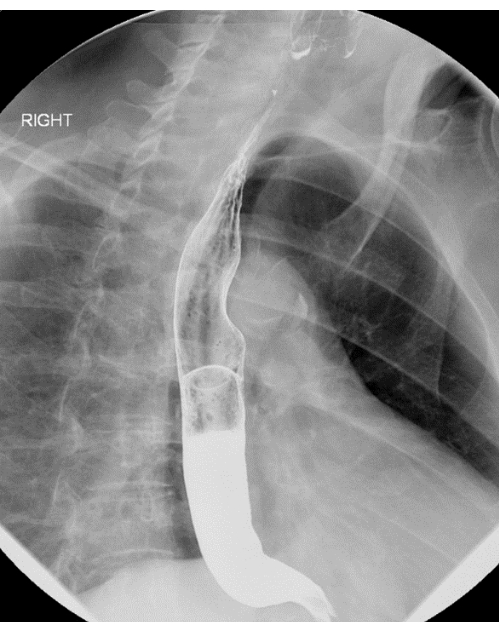
Figure 1: Esophagram demonstrating moderate to severe esophageal dysmotility. Please click here to view a larger version of this figure.

Figure 2: Abdominal CT scan demonstrating a herniated Nissen fundoplication wrap. Please click here to view a larger version of this figure.
| Value | Total | |
| N | 43 | |
| Age (years) | 58.9 | ± 15.5 |
| Average length of stay (days) | 7 | ± 5.7 |
| 30 day mortality (n, %) | 1 | 2.30% |
| 30 day morbidity | 10 | 23.20% |
| Return to operating room | 2 | 4.70% |
| Other invasive procedure | 2 | 4.70% |
| Pneumonia | 3 | 7.00% |
| Respiratory failure | 3 | 7.00% |
| Surgical site infection | 3 | 7.00% |
| Transfusion | 4 | 9.30% |
| Post-operative atrial fibrillation | 2 | 4.70% |
| 30 readmission rate | 4 | 9.30% |
| Continuous data summarized as mean ± SD; Categorical data expressed as frequency and percentage | ||
Table 1: Postoperative outcomes after redoing hiatal hernia repair. Continuous data are summarized as mean ± SD; categorical data are expressed as frequency and percentage.
Discussion
Reoperative foregut surgery is technically challenging but can be performed safely with a well-planned and thoughtful surgical approach. A thorough preoperative evaluation is essential to determine the etiology of symptoms and to guide diagnostic adjuncts. It is of utmost importance to determine the correct diagnosis prior to reintervention in order to determine the proper surgery and approach. For example, in patients undergoing redo anti-reflux surgery (ARS) after Nissan fundoplication, one should understand the primary symptoms the patient is experiencing. In those who have gas-bloat symptoms, pain and dysphagia as their primary problems, some studies have demonstrated that conversion to a Toupet fundoplication may reduce postoperative dysphagia and gas-bloat symptoms28,29. Similarly, in patients with altered esophageal motility after previous foregut surgery, a partial wrap such as a Toupet may be preferred over a complete wrap like a Nissen30. In another example, when treating pseudoachalasia, one must determine the underlying etiology of dysmotility – if secondary to malignancy, this may involve esophagectomy versus redo anti-reflux surgery in the case of an improperly constructed wrap31,32,33. Failure to recognize this may result in increased complexity and morbidity, particularly during redo foregut surgery.
Even with a complete preoperative evaluation, it is impossible to predict every challenge that will be faced intraoperatively; therefore, the foregut surgeon must be familiar with various access techniques and surgical approaches. Multiple studies have demonstrated the safety of various redo foregut procedures via a minimally invasive approach5,6,34,35. Regardless, the foregut surgeon should be ready to convert to an open approach or consider it from the onset if dictated by the case. In some instances, it may be necessary to use an alternate approach. Using complex recurrent hiatal hernias as an example, in order to achieve adequate intra-abdominal esophageal length, a transthoracic approach, such as a Belsey Mark IV repair, may be necessary to adequately mobilize the esophagus36.
Other times, a different surgical procedure might be necessary depending on previous surgery or intraoperative complications. The hiatal mesh may be associated with a more complex resection, including the esophagus or stomach, and thus require major reconstruction9,10. While redo fundoplication is the most common approach after failed anti-reflux surgery, there is an increased likelihood of alterations in the regional blood supply from previous dissection; therefore, hollow viscus injury, GEJ devascularization, and vagal nerve division are more likely37. Roux-en-Y reconstruction rather than fundoplication may be needed in these cases where there is injury, severe scarring precluding fundoplication, esophageal dysmotility or delayed gastric emptying38.
Endoluminal therapies have become an attractive option for treating foregut diseases such as achalasia and reflux. Although transoral incisionless fundoplication (TIF) has increased in popularity, it has demonstrated less complete control of GERD versus laparoscopic fundoplication12,39 and therefore may require revisional surgery. In TIF, the use of multiple full-thickness fasteners can result in traction diverticula and be a source of leak if removed. To minimize this, these fasteners should be sharply divided rather than pulled out and diverticula resected or imbricated to prevent leaks12,13,40. Although the foregut surgeon may not routinely perform these advanced endoscopic procedures, a thorough understanding is necessary if attempting to revise surgically.
In conclusion, reoperative foregut surgery presents a significant technical challenge. The surgeon must be adept in abdominal and thoracic surgery, open and minimally invasive approaches. Furthermore, with advances in endoscopic techniques, the surgeon must be familiar with these procedures before re-intervention. An exhaustive preoperative workup is essential. It is important to establish a clear indication that reoperation will likely benefit the patient and improve the quality of life.
Divulgazioni
The authors have nothing to disclose.
Acknowledgements
We would like to acknowledge the Division of Thoracic and Foregut Surgery and the Department of Surgery at the University of Minnesota for helping us proceed with this study.
Materials
| Bravo calibration-free reflux testing system | Medtronic | FGS-0635 | Wireless esophageal pH testing system |
| Cadiere forceps | IS | 470049 | Used as a grasper |
| da Vinci Surgeon Console | IS | SS999 | Used to control surgical robot |
| da Vinci Vision Cart | IS | VS999 | Houses advanced vision and energy technologies to provide communication across the platform components |
| da Vinci Xi | IS | K131861 | The surgical robot |
| da Vinci Xi Endoscope with Camera, 8 mm, 30° | IS | 470027 | The camera for the da Vinci robot |
| Lapro-Flex Articulating Retractors | Mediflex | 91682 | Used as liver retractor |
| Large needle driver | IS | 470006 | Used as a needle driver |
| Maloney Tapered Esophageal Bougie, 56 Fr | Pilling | 507956 | Esophageal bougie for hiatal repair |
| Maloney Tapered Esophageal Bougie, 58 Fr | Pilling | 507958 | Esophageal bougie for wrap creation |
| Mega SutureCut needle driver | IS | 470309 | Used as a needle driver |
| Monolithic FlexArm Plus | Mediflex | 99045-QC | Used to hold liver retractor to OR bed |
| Round tip scissors | IS | 470007 | Used for cutting |
| Shiley Hi-Lo oral/nasal endotracheal tube cuffed, 8.0 mm | Covidien | 86113 | Endotracheal tube for intubation |
| SynchroSeal | IS | 480440 | Used for dissecting, vessel sealing, and dividing |
| Tip-Up fenestrated grasper | IS | 470347 | Used as a grasper |
Riferimenti
- Awais, O., et al. Reoperative antireflux surgery for failed fundoplication: an analysis of outcomes in 275 patients. The Annals of Thoracic Surgery. 92 (3), 1083-1089 (2011).
- Furnee, E. J., Draaisma, W. A., Broeders, I. A., Gooszen, H. G. Surgical reintervention after failed antireflux surgery: a systematic review of the literature. Journal of Gastrointestinal Surgery. 13 (8), 1539-1549 (2009).
- Singhal, S., Kirkpatrick, D. R., Masuda, T., Gerhardt, J., Mittal, S. K. Primary and redo antireflux surgery: outcomes and lessons learned. Journal of Gastrointestinal Surgery. 22 (2), 177-186 (2018).
- van Beek, D. B., Auyang, E. D., Soper, N. J. A comprehensive review of laparoscopic redo fundoplication. Surgical Endoscopy. 25 (3), 706-712 (2011).
- Witek, T. D., Luketich, J. D., Pennathur, A., Awais, O. Management of recurrent paraesophageal hernia. Thoracic Surgury Clinics. 29 (4), 427-436 (2019).
- Bathla, L., Legner, A., Tsuboi, K., Mittal, S. Efficacy and feasibility of laparoscopic redo fundoplication. World Journal of Surgery. 35 (11), 2445-2453 (2011).
- Pessaux, P., et al. Laparoscopic antireflux surgery: five-year results and beyond in 1340 patients. The Archives of Surgery. 140 (10), 946-951 (2005).
- Skinner, D. B. Surgical management after failed antireflux operations. World Journal of Surgery. 16 (2), 359-363 (1992).
- Nandipati, K., et al. Reoperative intervention in patients with mesh at the hiatus is associated with high incidence of esophageal resection–a single-center experience. Journal of Gastrointestinal Surgery. 17 (12), 2039-2044 (2013).
- Parker, M., et al. Hiatal mesh is associated with major resection at revisional operation. Surgical Endoscopy. 24 (12), 3095-3101 (2010).
- Ashfaq, A., Rhee, H. K., Harold, K. L. Revision of failed transoral incisionless fundoplication by subsequent laparoscopic Nissen fundoplication. World Journal of Gastroenterology. 20 (45), 17115-17119 (2014).
- Bell, R. C., Kurian, A. A., Freeman, K. D. Laparoscopic anti-reflux revision surgery after transoral incisionless fundoplication is safe and effective. Surgical Endoscopy. 29 (7), 1746-1752 (2015).
- Puri, R., Smith, C. D., Bowers, S. P. The spectrum of surgical remediation of transoral incisionless fundoplication-related failures. Journal of Laparoendoscopic & Advanced Surgical Techniques. 28 (9), 1089-1093 (2018).
- Del Campo, S. E. M., Mansfield, S. A., Suzo, A. J., Hazey, J. W., Perry, K. A. Laparoscopic redo fundoplication improves disease-specific and global quality of life following failed laparoscopic or open fundoplication. Surgical Endoscopy. 31 (11), 4649-4655 (2017).
- Smith, C. D., McClusky, D. A., Rajad, M. A., Lederman, A. B., Hunter, J. G. When fundoplication fails: redo. Annals of Surgery. 241 (6), 861-869 (2005).
- Wilshire, C. L., et al. Clinical outcomes of reoperation for failed antireflux operations. The Annals of thoracic surgery. 101 (4), 1290-1296 (2016).
- Zundel, N., Melvin, W. S., Patti, M. G., Camacho, D. . Benign Esophageal Disease: Modern Surgical Approaches and Techniques. , (2021).
- Addo, A., et al. Laparoscopic revision paraesophageal hernia repair: a 16-year experience at a single institution. Surgical Endoscopy. 37 (1), 624-630 (2023).
- Autorino, R., Zargar, H., Kaouk, J. H. Robotic-assisted laparoscopic surgery: recent advances in urology. Fertility and sterility. 102 (4), 939-949 (2014).
- Matanes, E., Lauterbach, R., Boulus, S., Amit, A., Lowenstein, L. Robotic laparoendoscopic single-site surgery in gynecology: a systematic review. European Journal of Obstetrics & Gynecology and Reproductive Biology. 231, 1-7 (2018).
- Font, A. C., Farrarons, S. S., Bosch, C. A., Martín, M. V., Savall, E. G. 635 robotic redo funduplication for a two time recurrent hiatal hernia. How we do. Diseases of the Esophagus. 34 (Supplement_1), (2021).
- Soliman, B. G., et al. Robot-assisted hiatal hernia repair demonstrates favorable short-term outcomes compared to laparoscopic hiatal hernia repair. Surgical Endoscopy. 34 (6), 2495-2502 (2020).
- Tolboom, R. C., Draaisma, W. A., Broeders, I. A. Evaluation of conventional laparoscopic versus robot-assisted laparoscopic redo hiatal hernia and antireflux surgery: a cohort study. Journal of robotic surgery. 10, 33-39 (2016).
- Jamieson, J. R., et al. Ambulatory 24-h esophageal pH monitoring: normal values, optimal thresholds, specificity, sensitivity, and reproducibility. American Journal of Gastroenterology. 87 (9), 1102-1102 (1992).
- Johnson, L. F., DeMeester, T. R. Development of the 24-hour intraesophageal pH monitoring composite scoring system. Journal of clinical gastroenterology. 8, 52-58 (1986).
- Siegal, S. R., Dolan, J. P., Hunter, J. G. Modern diagnosis and treatment of hiatal hernias. Langenbeck’s Archives of Surgery. 402 (8), 1145-1151 (2017).
- Hasson, H. A modified instrument and method for laparoscopy. American Journal of Obstetrics and Gynecology. 110 (6), 886-887 (1971).
- Al Hashmi, A. -. W., et al. A retrospective multicenter analysis on redo-laparoscopic anti-reflux surgery: conservative or conversion fundoplication. Surgical Endoscopy. 33 (1), 243-251 (2019).
- Broeders, J., et al. Systematic review and meta-analysis of laparoscopic Nissen (posterior total) versus Toupet (posterior partial) fundoplication for gastro-oesophageal reflux disease. Journal of British Surgery. 97 (9), 1318-1330 (2010).
- Bakhos, C. T., Petrov, R. V., Parkman, H. P., Malik, Z., Abbas, A. E. Role and safety of fundoplication in esophageal disease and dysmotility syndromes. Journal of Thoracic Disease. 11 (Suppl 12), S1610 (2019).
- Barnett, D. R., Balalis, G. L., Myers, J. C., Devitt, P. G. Diagnosis and treatment of pseudoachalasia: how to catch the mimic. 3, (2020).
- Bonavina, L., Bona, D., Saino, G., Clemente, C. Pseudoachalasia occurring after laparoscopic Nissen fundoplication and crural mesh repair. Langenbeck’s Archives of Surgery. 392 (5), 653-656 (2007).
- Haj Ali, S. N., Nguyen, N. Q., Abu Sneineh, A. T. Pseudoachalasia: a diagnostic challenge. When to consider and how to manage. Scandinavian Journal of Gastroenterology. 56 (7), 747-752 (2021).
- Felix, V. N., Murayama, K. M., Bonavina, L., Park, M. I. Achalasia: what to do in the face of failures of Heller myotomy. Annals of the New York Academy of Sciences. 1481 (1), 236-246 (2020).
- Gorecki, P. J., Hinder, R. A., Libbey, J. S., Bammer, T., Floch, N. Redo laparoscopic surgery for achalasia. Surgical Endoscopy. 16 (5), 772-776 (2002).
- Markakis, C., et al. The Belsey Mark IV: an operation with an enduring role in the management of complicated hiatal hernia. BMC surgery. 13, 1-6 (2013).
- Cowgill, S. M., Arnaoutakis, D., Villadolid, D., Rosemurgy, A. S. 34;Redo" fundoplications: satisfactory symptomatic outcomes with higher cost of care. Journal of Surgical Research. 143 (1), 183-188 (2007).
- Makris, K. I., et al. The role of short-limb Roux-en-Y reconstruction for failed antireflux surgery: a single-center 5-year experience. Surgical Endoscopy. 26 (5), 1279-1286 (2012).
- Wendling, M. R., Melvin, W. S., Perry, K. A. Impact of transoral incisionless fundoplication (TIF) on subjective and objective GERD indices: a systematic review of the published literature. Surgical Endoscopy. 27 (10), 3754-3761 (2013).
- Parker, B., Reavis, K. Benign Esophageal Disease. , 71-89 (2021).

