Systematic Endobronchial Ultrasound – The Six Landmarks Approach
Summary
Endobronchial ultrasound-guided sampling using transbronchial needle aspiration plays a key role in staging and diagnosing lung cancer. We propose a systematic stepwise approach dividing the procedure into six landmarks that should be taught to new operators.
Abstract
Lung cancer is the leading cause of cancer mortality globally. To ensure the correct diagnosis and staging in relation to treatment options, it is crucial to obtain valid biopsies from suspected tumors and mediastinal lymph nodes and accurate identification of the mediastinal lymph nodes regarding the Tumor-Node-Metastasis (TNM)-classification. Flexible bronchoscopy combined with endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) is essential in the workup and diagnosis of patients suspected of lung cancer. EBUS-TBNA from mediastinal lymph nodes is a technically difficult procedure and has been identified as one of the most important procedures that should be integrated into a simulation-based training program for invasive pulmonologists. More specific guidelines that govern training in EBUS-TBNA are needed to meet this demand. We hereby propose a systematic, stepwise approach with specific attention to six landmarks that support the endoscopist when navigating through the bronchial maze. The stepwise approach relying on the six landmarks is used in the EBUS-certified training program offered by the European Respiratory Society (ERS).
Introduction
Lung cancer is one of the most common cancers worldwide with 2.21 million cases in 2020, and the most frequent cause of cancer death with 1.80 million deaths in 20201. As with most cancers, fast and accurate diagnosis of lung cancer is crucial to be able to offer the best treatment, which in cases with a localized disease with no or little spreading to mediastinal lymph nodes can be surgical removal of the tumor. In order to be able to confirm or invalidate the suspicion of malignancy and to determine the Tumor-Node-Metastasis (TNM)-classification if lung cancer is confirmed2, it is extremely important to have good and representative biopsies from the suspected tumor or lymph nodes.
Among the invasive techniques, flexible bronchoscopy combined with endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) plays a key role3. However, it is a complex technical procedure, and the success is dependent on the competence of the operator4. Anatomic orientation can easily be lost if the endoscopist does not know the anatomy of the mediastinum. Knowledge of endosonographic anatomy and its relation to the TNM lung cancer classification system is therefore crucial. In the case of lung cancer, if no tumor cells are found in any lymph node stations, the disease is classified as N0 disease and is often operable and thus, potentially curable. In the case of a right-sided lung tumor, the disease is classified as N1 disease if tumor cells are solely found in station 10R and could be operable and thus potentially curable. However, if tumor cells are found in station 4R, the disease is classified as N2 disease, and the patient can only be offered life-prolonging chemotherapy5. Three borders should therefore be remembered as they are important for treatment and prognosis.
(i)The left border of the trachea is the border between stations 4R and 4L.
(ii)The upper border of the left pulmonary artery is the border between stations 4L and 10L.
(iii)The lower border of the azygos vein is the border between stations 4R and 10R6.
To be qualified to perform EBUS-TBNA in the diagnostic process of possible lung cancer, it is therefore essential that EBUS-TBNA is thoroughly trained in a simulator-based setting based on a structured training curriculum before being performed on patients. Therefore, a stepwise approach relying on the six anatomical landmarks is used in the EBUS-certified training program offered by the European Respiratory Society (ERS)7.
We demonstrate the stepwise structured guide in a simulation-based setting at Copenhagen Academy for Medical Education and Simulation (CAMES), Denmark8, on how to perform EBUS-TBNA with the EBUS endoscope relying on the six anatomical landmarks9 as a guide.
Protocol
This study uses the EVIS Exera II endoscopy tower with a BF-UC180F EBUS endoscope (Figure 1) to demonstrate the scope and the Surgical Science Simulator (ENDO mentor suite) with the GI-Bronch Mentor software from Simbionix, Essential EBUS Case 6, when performing the EBUS procedure in the simulation-based setting. No patients are included in the study as the entire procedure is performed on the Surgical Science Simulator (ENDO mentor suite). Prior to the EBUS procedure, a complete bronchoscopy is performed using a regular bronchoscope to make sure the bronchial tree has been visualized systematically and to identify key anatomical positions where the underlying lymph node stations must be located (Figure 2).
1. Handling of the endoscope
NOTE: The EBUS endoscope is handled similarly to the bronchoscope. However, it is important to note that contrary to the bronchoscope, the EBUS endoscope gives an oblique angle view as the ultrasound transducer reduces the visibility (Figure 3).
- Hold the endoscope in the left hand with the left thumb on the steering lever.
- Hold the distal end of the endoscope in the right hand and enter the trachea through the nasal or oral cavity. When the vocal cords are visualized at the bottom of the picture (Figure 3B), administer 2 mL of 2% lidocaine twice via the simulator by pressing the appropriate button on the screen, and pass the vocal cords with care.
- Administer a further 2 mL of 2% lidocaine in the trachea as well as in the right and left main bronchus, respectively.
2. Anatomy
- After having inspected the bronchial tree, retract the bronchoscope and change to the EBUS scope. Turn on the ultrasound transducer and locate the six anatomical EBUS landmarks in the order mentioned below.
- Locate Landmark 1 = station 4L
- Locate station 4L at the left side of the trachea, just cranial to the carina. To find station 4L, turn the endoscope counterclockwise in the trachea and locate it between the arch of the aorta and the left pulmonary artery, sometimes referred to as "the Mickey Mouse window" (Figure 4).
- Locate Landmark 2 = Station 7
- Locate station 7 between the right pulmonary artery and the left atrium below the carina. Place the EBUS scope in the right or the left main bronchus and turn the endoscope facing medially (Figure 5).
- Locate Landmark 3 = Station 10L
- Locate station 10L adjacent to the left main bronchus cranial to the left upper lobe. Place the endoscope in the left main bronchus or the left upper lobe and look upwards. The upper border of the left pulmonary artery forms the boundary between stations 4L and 10L (Figure 6).
- Locate Landmark 4 = Station 10R
- Locate station 10R on the lateral wall of the right main bronchus, just caudal to the inferior border of the azygos vein. The upper border is the lower border of the azygos vein. Place the endoscope in the right main bronchus or the right upper lobe bronchus and look upwards (Figure 7).
- Locate Landmark 5 = The azygos vein
- To find the azygos vein, retract the endoscope slightly cranially and turn the transducer clockwise in the trachea. Turn the transducer counterclockwise to visualize the azygos vein draining into the superior vena cava (Figure 8).
- Locate Landmark 6 = Station 4R
- To find station 4R, retract the endoscope further cranially from the azygos vein and turn the transducer clockwise in the trachea. Locate station 4R to the right or in front of the trachea above the lower border of the azygos vein, which marks the border between station 10R and 4R (Figure 9).
- Locate Landmark 1 = station 4L
- After having located the six landmarks, look for other lymph node stations, i.e., stations 2R, 2L, 11R, and 11L, and other structures of clinical importance. At least stations 4L, 7, and 4R should be biopsied3.
- When the relevant lymph node is localized, ask the assistant for the biopsy equipment. The biopsy equipment includes a sheath protecting the needle, connected to a handle that can be locked onto the endoscope. Inside the sheath is the needle, and inside the needle is the stylet. When inserting the needle into the working channel, keep the steering lever in a neutral position as shown in the video to avoid damage to the endoscope.
NOTE: The needle used here comes with the simulator. However, the recommended needle size for this procedure is 21 G. - Adjust the sheath so it is visible at the end of the endoscope; however, no more than 1-2 mm.
- Turn the transducer towards the bronchial wall so the lymph node is visualized on the left side of the ultrasound picture. Now, perform the biopsy.
- After puncturing the lymph node with the needle, ask the assistant to remove the stylet and then apply suction to the needle by pressing the appropriate button on the screen. The needle must be moved back and forward several times.
- Remove the suction and retract the needle tip while inside the sheath. Ensure that the distal end of the endoscope is not flexed and remains in a neutral position to prevent damage to the endoscope. Each lymph node must be punctured at least three times10,11.
- After the final biopsy, check for bleeding. Inspect the place for biopsy with the white light view and stay for a few seconds. If no bleeding is observed, retract the endoscope.
Representative Results
The above-mentioned structured approach to an EBUS-TBNA procedure has been taught at CAMES since 2016 as part of the EBUS-certified training program offered by the European Respiratory Society (ERS)7. The 6 landmarks approach is based on a validated assessment tool for measuring competency in EBUS-guided transbronchial needle aspiration4. By performing EBUS-TBNA in a structured way, as shown above, no important lymph nodes will be missed, and the diagnostic accuracy will be very high.
As described in the protocol and shown in the video, we suggest a very structured approach to the EBUS procedure to make sure no essential lymph nodes will be missed.
It is important to note that the order mentioned above (station 4L (Figure 4)→ station 7 (Figure 5) → station 10L/11L (Figure 6) → station 10R/11R (Figure 7) → azygos vein (Figure 8) → station 4R (Figure 9)) is the initial diagnostic approach to ensure that the procedure is done systematically (Figure 10).
However, if radiology has shown a suspicious mass or lymph node on the left side, it will be correct to start on the right side as far away from the tumor as possible.
Several studies have shown that a systematic approach is important when performing endoscopic pulmonary procedures (Table 1)11,12,13. Sanz-Santos et al. compared systematic and targeted staging in 107 patients and found that systematic EBUS-TBNA sampling provided additional important clinical information in 14 cases (13%) compared to targeted EBUS-TBNA12. Similar results were found by Crombag et al. in 2019, showing that systematic EBUS was superior to PET-CT-targeted EBUS alone13.

Figure 1: EVIS Exera II endoscopy tower with a BF-UC180F EBUS endoscope (Olympus, Japan). Please click here to view a larger version of this figure.
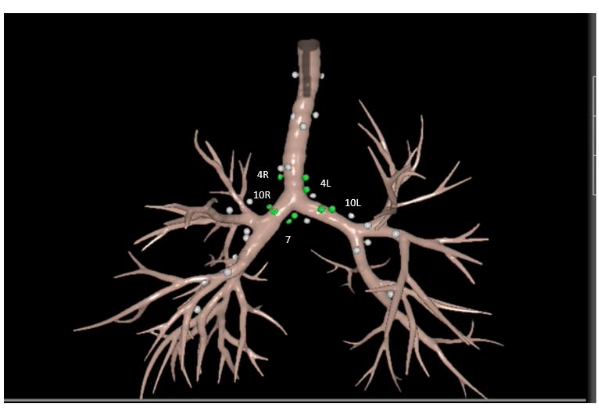
Figure 2: Location of the mediastinal lymph nodes. Stations 4R, 4L, 7, 10R and 10L are highlighted. Picture from Surgical Science Simulator, GI-Bronch Mentor, Essential Bronchoscopy Task 4. Lung Anatomy, Lymph Nodes. Please click here to view a larger version of this figure.
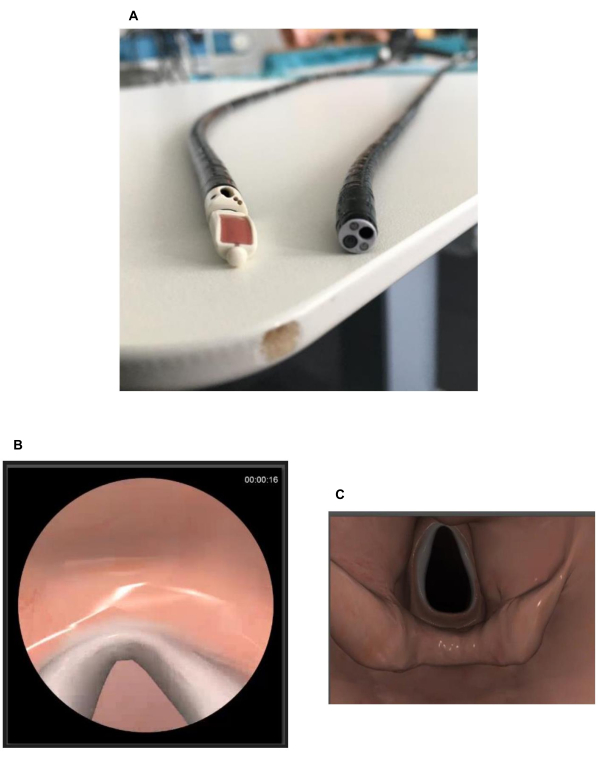
Figure 3: Differences between the endoscope and the bronchoscope. (A) The end of the endoscope compared to the end of a bronchoscope showing the endoscope's oblique angle view as the ultrasound transducer reduces the visibility.(B) The vocal cords seen from the endoscope. (C) The vocal cords from a bronchoscope. Please click here to view a larger version of this figure.
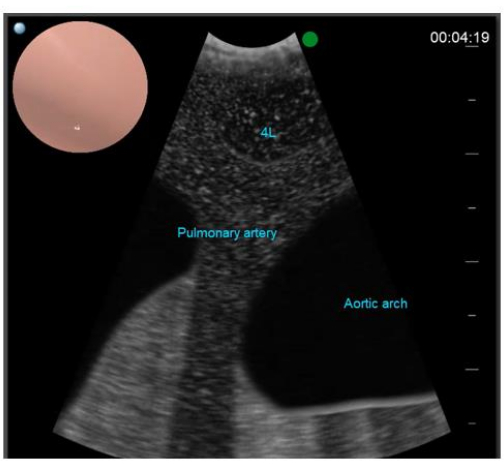
Figure 4: Landmark 1. Station 4L is located at the left side of the trachea, just cranial to the carina. Picture from Surgical Science Simulator, GI-Bronch Mentor, Essential EBUS Case 6. Please click here to view a larger version of this figure.
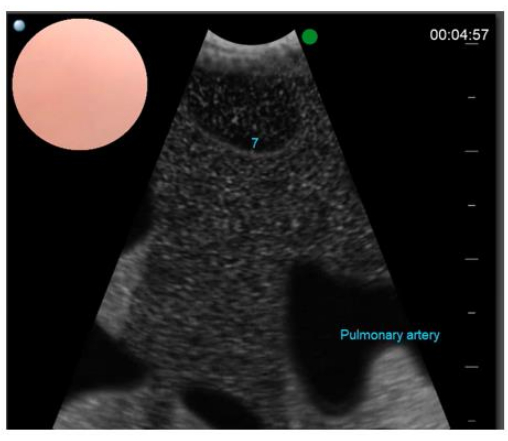
Figure 5: Landmark 2. Station 7 is found between the right pulmonary artery and the left atrium below the carina. Picture from Surgical Science Simulator, GI-Bronch Mentor, Essential EBUS Case 6. Please click here to view a larger version of this figure.
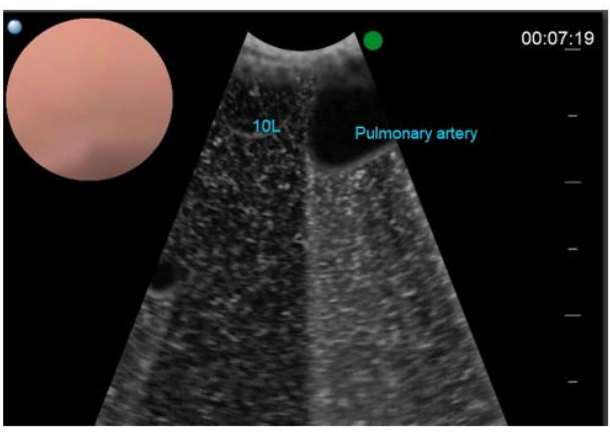
Figure 6: Landmark 3. Station 10L is located adjacent to the left main bronchus cranial to the left upper lobe. Picture from Surgical Science Simulator, GI-Bronch Mentor, Essential EBUS Case 6. Please click here to view a larger version of this figure.
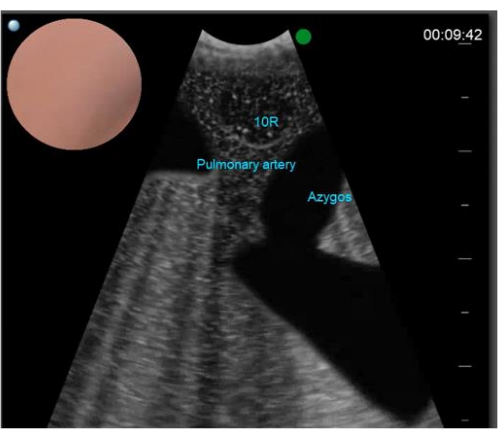
Figure 7: Landmark 4. Station 10R is located on the right side of the right main bronchus, just caudal to the inferior border of the azygos vein. Picture from Surgical Science Simulator, GI-Bronch Mentor, Essential EBUS Case 6. Please click here to view a larger version of this figure.

Figure 8: Landmark 5. The azygos vein can be found by turning the transducer clockwise in the trachea. The figure shows how the azygos vein drains into the superior vena cava. Picture from Surgical Science Simulator, GI-Bronch Mentor, Essential EBUS Case 6. Please click here to view a larger version of this figure.

Figure 9: Landmark 6. Station 4R is found to the right or anterior to the trachea above the lower border of the azygos vein. Picture from Surgical Science Simulator, GI-Bronch Mentor, Essential EBUS Case 6. Please click here to view a larger version of this figure.
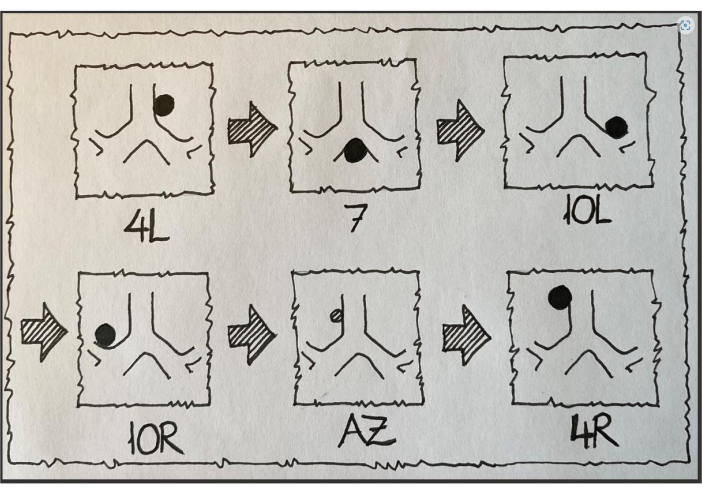
Figure 10: Overview of the six EBUS landmarks. AZ, azygos vein. Illustration by Paul Frost Clementsen, 2023. Please click here to view a larger version of this figure.
| Targeted EBUS by PET-CT | Systematic EBUS-TBNA | Reference | ||||||
| 107 patients staged with N2 disease | Provided additional clinical information in 14 (13%) of the 107 patients (3 patients upstaged with N3 disease + 11 patients with N2b disease [staged as N2a disease on PET-CT]) | 12 | ||||||
| Sensitivity 73% (75/103) Negative predictive value 81% (122/150) | Sensitivity 77% (79/103) Negative predictive value 84% (122/146) | 13 | ||||||
Table 1: Data comparing targeted EBUS by PET-CT and systemic EBUS-TBNA approaches.
Discussion
We hereby propose a systematic approach to the EBUS-TBNA procedure by splitting the anatomy into six landmarks to help guide the endoscopist through the bronchial maze. Furthermore, we demonstrate how to perform needle aspiration in a systematic way possible to repeat every time to standardize the procedure.
Even though the simulation-based setting is a safe environment, the endoscopist should be aware of some critical steps in the procedure. Initially, it is important to know the oblique angle of the EBUS-scope to be able to pass the vocal cords. Subsequently, it is important to know how to handle the biopsy equipment. Demonstrating the needle does not fall within the scope of this manuscript, as several slightly different needles are found on the market, and correct handling depends on what needle is used. However, it is important to know where to place the transducer so the lymph node is visualized on the left side of the ultrasound picture as the needle punctures the lymph node from the right side. Finally, it is important to check the airways for bleeding. How to handle acute postoperative bleeding does not fall within the scope of this manuscript; however, before performing an EBUS-procedure, the endoscopist must be familiar with how to handle a bleeding in the airways.
As the above-mentioned EBUS-procedure is performed in a simulator, it is impossible to completely avoid technical problems. One of the most frequent problems with the technique is that the ultrasound picture freezes. This often happens in the most distal parts of the airways (stations 10R and 10L). This problem can be handled by retracting the endoscope to the carina and waiting a few seconds for the picture to come back. If the problem persists, the endoscopist can activate the balloon by touching the balloon indicator on the screen and continue with the procedure.
As the EBUS procedure is performed in a simulator, some limitations can be mentioned. Most obviously, the endoscopist does not learn to deal with challenges that may arise in a real-life setting. Patients may be restless, coughing, or complaining about pain and discomfort. Furthermore, the patients can desaturate during the procedure. However, the software has incorporated both coughing and desaturating into the cases, making the procedure as close to reality as possible. Another limitation is that the endoscopist practices in a quiet and undisturbed environment. In a real-life setting, there will be several disturbances with persons in the room talking, doors opening and closing, and phones ringing. However, a recent study by Andersen et al. focusing on simulation-based training in combination with immersive virtual reality (iVR)has shown that iVR has the potential as an educational tool to reduce the gap between traditional simulation environments and the real world14.
Despite the above-mentioned critical steps and limitations, we propose learning the EBUS-TBNA procedure in a simulated setting, as learning EBUS-TBNA in a simulation-based setting still outperforms learning it in a clinical setting4, and several studies have shown that simulation-based training in both bronchoscopy and EBUS-TBNA is equally efficient to laboratory training and apprenticeship training, respectively4,15. However, in the simulation-based setting, the environment is safe, and the trainee should not be nervous and afraid of doing something wrong that might be life-threatening16,17,18.
Since 2016, CAMES Denmark has educated pulmonologists in EBUS-TBNA as part of the EBUS-certified training program offered by the European Respiratory Society (ERS)7. The training program consists of three parts. Part 1 is a theoretical part based on online modules and a theoretical course finishing with an online post-assessment test. Part 2 focuses on clinical observation and intensive simulation training, completed over 2-3 days at a center in either Heidelberg, Amsterdam or at CAMES, Copenhagen. Part 3 covers supervised training and is completed at the participants' own institutions under supervision. Participants must create a portfolio of 20 EBUS cases and three videos of EBUS procedures. The case reports and videos are then reviewed and rated blindly to determine if the participant is qualified to perform EBUS independently.
Still, the performance of bronchoscopies with or without EBUS needs to be standardized, and education in the procedure varies among countries and even inside countries from hospital to hospital. Many medical doctors learn how to perform a bronchoscopy by practicing on patients while supervised by a more experienced doctor. This setup is not optimal as the trainee might be nervous and afraid of doing something wrong that might be life-threatening, which will influence the learning curve, the time of the procedure will be prolonged, and finally, the safety of the patient will be threatened15,16,18. Therefore, we strongly encourage pulmonologists and others performing endobronchial procedures to learn and train bronchoscopy and EBUS based on a systematic approach in a simulation-based setting instead of the traditional way, with medical doctors training on patients.
This study only focuses on the EBUS-TBNA procedure. Several recent studies have shown that diagnostic accuracy improves significantly by performing supplementary examinations, e.g., transesophageal ultrasound-guided fine-needle aspirations (EUS-FNA) using the bronchoscope (EUS-B)19,20. However, to date, no simulators have incorporated software with a training module in EUS-B, making it impossible to learn and practice in a simulation-based setting19. We believe that the demand for pulmonologists who can perform EUS-B will rise in the future and that developing an EUS-B-FNA simulation-based training program with a validated test to assess user competency will be of great importance.
Divulgazioni
The authors have nothing to disclose.
Acknowledgements
The authors have no acknowledgments.
Materials
| EVIS Exera II endoscopy tower with a BF-UC180F EBUS endoscope | Olympus | https://medical.olympusamerica.com/products/bf-uc180f-ebus-bronchoscope | |
| ENDO mentor suite | Surgical Science | https://simbionix.com/endo-mentor-suite/ | Surgical Science Simulator |
| GI-Bronch Mentor software | Simbionix | https://simbionix.com/simulators/gi-mentor/ |
Riferimenti
- WHO. Cancer. , (2022).
- Kutob, L., Schneider, F. Lung cancer staging. Surgical Pathology Clinics. 13 (1), 57-71 (2020).
- Vilmann, P., et al. Combined endobronchial and esophageal endosonography for the diagnosis and staging of lung cancer: European Society of Gastrointestinal Endoscopy (ESGE) Guideline, in cooperation with the European Respiratory Society (ERS) and the European Society of Thoracic Surgeons (ESTS). Endoscopy. 47 (6), 545-559 (2015).
- Konge, L., et al. Simulator training for endobronchial ultrasound: a randomised controlled trial. European Respiratory Journal. 46 (4), 1140-1149 (2015).
- Liam, C. K., Lee, P., Yu, C. J., Bai, C., Yasufuku, K. The diagnosis of lung cancer in the era of interventional pulmonology. International Journal of Tuberculosis and Lung Disease. 25 (1), 6-15 (2021).
- Clementsen, P., et al. Diagnosis and staging of lung cancer with the use of one single echoendoscope in both the trachea and the esophagus: A practical guide. Journal of Endoscopic Ultrasound. 10 (5), 325-334 (2021).
- Farr, A., et al. Endobronchial ultrasound: launch of an ERS structured training programme. Breathe (Sheffield, England). 12 (3), 217-220 (2016).
- Konge, L., et al. The Simulation Centre at Rigshospitalet, Copenhagen, Denmark. Journal of Surgical Education. 72 (2), 362-365 (2015).
- Jenssen, C., et al. Ultrasound techniques in the evaluation of the mediastinum, part 2: mediastinal lymph node anatomy and diagnostic reach of ultrasound techniques, clinical work up of neoplastic and inflammatory mediastinal lymphadenopathy using ultrasound techniques and how to learn mediastinal endosonography. Journal of Thoracic Diseases. 7 (10), 439-458 (2015).
- Lee, H. S., et al. Real-time endobronchial ultrasound-guided transbronchial needle aspiration in mediastinal staging of non-small cell lung cancer: how many aspirations per target lymph node station. Chest. 134 (2), 368-374 (2008).
- Kinsey, C. M., Arenberg, D. A. Endobronchial ultrasound-guided transbronchial needle aspiration for non-small cell lung cancer staging. American Journal of Respiratory and Critical Care Medicine. 189 (6), 640-649 (2014).
- Sanz-Santos, J., et al. Systematic compared with targeted staging with endobronchial ultrasound in patients with lung cancer. Annals of Thoracic Surgery. 106 (2), 398-403 (2018).
- Crombag, L. M. M., et al. Systematic and combined endosonographic staging of lung cancer (SCORE study). The European Respiratory Journal. 53 (2), 1800800 (2019).
- Andersen, A. G., et al. Preparing for reality: A randomized trial on immersive virtual reality for bronchoscopy training. Respiration. 102 (4), 316-323 (2023).
- Naur, T. M. H., Nilsson, P. M., Pietersen, P. I., Clementsen, P. F., Konge, L. Simulation-based training in flexible bronchoscopy and endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA): A systematic review. Respiration. 93 (5), 355-362 (2017).
- Konge, L., et al. Reliable and valid assessment of clinical bronchoscopy performance. Respiration. 83 (1), 53-60 (2012).
- Du Rand, I. A., et al. British Thoracic Society guideline for diagnostic flexible bronchoscopy in adults: accredited by NICE. Thorax. 68 (Suppl 1), 1-44 (2013).
- Nilsson, P. M., Naur, T. M. H., Clementsen, P. F., Konge, L. Simulation in bronchoscopy: current and future perspectives. Advances in Medical Education and Practice. 8, 755-760 (2017).
- Cold, K. M., Clementsen, P. F. Diagnosis and staging of lung cancer using transesophageal ultrasound: Training and assessment. Journal of Endoscopic Ultrasound. 11 (2), 92-94 (2022).
- Korevaar, D. A., et al. Added value of combined endobronchial and oesophageal endosonography for mediastinal nodal staging in lung cancer: a systematic review and meta-analysis. Lancet Respiratory Medicine. 4 (12), 960-968 (2016).

