Studying Adipose Endothelial Cell/Adipocyte Cross-Talk in Human Subcutaneous Adipose Tissue
Summary
Here, we describe a protocol for isolating, culturing, and phenotyping microvascular endothelial cells from human subcutaneous adipose tissue (hSATMVECs). Additionally, we describe an experimental model of hSATMVEC-adipocyte cross-talk.
Abstract
Microvascular endothelial cells (MVECs) have many critical roles, including control of vascular tone, regulation of thrombosis, and angiogenesis. Significant heterogeneity in endothelial cell (EC) genotype and phenotype depends on their vascular bed and host disease state. The ability to isolate MVECs from tissue-specific vascular beds and individual patient groups offers the opportunity to directly compare MVEC function in different disease states. Here, using subcutaneous adipose tissue (SAT) taken at the time of insertion of cardiac implantable electronic devices (CIED), we describe a method for the isolation of a pure population of functional human subcutaneous adipose tissue MVEC (hSATMVEC) and an experimental model of hSATMVEC-adipocyte cross-talk.
hSATMVEC were isolated following enzymatic digestion of SAT by incubation with anti-CD31 antibody-coated magnetic beads and passage through magnetic columns. hSATMVEC were grown and passaged on gelatin-coated plates. Experiments used cells at passages 2-4. Cells maintained classic features of EC morphology until at least passage 5. Flow cytometric assessment showed 99.5% purity of isolated hSATMVEC, defined as CD31+/CD144+/CD45–. Isolated hSATMVEC from controls had a population doubling time of approximately 57 h, and active proliferation was confirmed using a cell proliferation imaging kit. Isolated hSATMVEC function was assessed using their response to insulin stimulation and angiogenic tube-forming potential. We then established an hSATMVEC-subcutaneous adipocyte co-culture model to study cellular cross-talk and demonstrated a downstream effect of hSATMVEC on adipocyte function.
hSATMVEC can be isolated from SAT taken at the time of CIED insertion and are of sufficient purity to both experimentally phenotype and study hSATMVEC-adipocyte cross-talk.
Introduction
Endothelial cells (ECs) are squamous cells that line the inner surface of the blood vessel wall as a monolayer. They have many essential roles, including control of vascular tone, regulation of thrombosis, modulating the inflammatory response, and contributing to angiogenesis1. Given the importance of endothelial cells in cardiometabolic physiology, they are frequently used experimentally to further the understanding of pathophysiology and to examine new pharmacological treatments for cardiometabolic disease.
However, there is enormous heterogeneity in endothelial cell morphology, function, gene expression, and antigen composition depending on the origin of their vascular bed2. While endothelial cells from large arteries are best suited to atherosclerosis studies, endothelial cells from small vessels, known as microvascular endothelial cells (MVECs), are more suitable for angiogenesis studies2. Understanding the molecular basis for endothelial heterogeneity may provide valuable insights into vascular bed-specific therapies. Microvascular endothelial function also significantly differs in numerous diseases, including diabetes, cardiovascular disease, and systemic infection3,4. Therefore, the ability to isolate endothelial cells from defined patient groups allows direct comparison of their endothelial cell function and cellular cross-talk5.
In this paper, we describe a novel method of isolating human MVECs from subcutaneous adipose tissue (hSATMVEC) taken at the time of cardiac implantable electronic device (CIED) insertion. hSATMVEC isolated following enzymatic digestion of subcutaneous adipose tissue (SAT) were grown and passaged on gelatin-coated plates. We then describe a range of phenotyping assays that have been successfully applied to hSATMVECs in order to validate their phenotype and demonstrate use in routine endothelial cell assays. Finally, we describe an application of hSATMVECs in an experimental model of hSATMVECs-adipocyte cross-talk.
Protocol
The samples of human tissue used in the technique described have been taken from patients undergoing guideline-indicated insertion of CIEDs according to routine clinical practice in Leeds Teaching Hospitals NHS Trust (Leeds, United Kingdom). The study protocol, along with all other documentation, was approved by the local ethics committee (11/YH/0291) prior to participant enrolment. The study was conducted in compliance with the principles of the Declaration of Helsinki.
1. Patient population
- Obtain fresh subcutaneous adipose tissue (SAT) during CIED implantation from SAT overlying the pectoralis major muscle.
- Isolate SAT samples under sterile conditions and handle the tissues samples following collection in a laminar flow hood under strict aseptic conditions to prevent bacterial contamination.
2. Endothelial cell isolation and culture
NOTE: A schematic for hSATMVEC isolation is shown in Figure 1.
- For hSATMVEC isolation, use a minimum of 250 mg of fresh subcutaneous adipose tissue (SAT) obtained during CIED implantation from SAT overlying the pectoralis major muscle (see Figure 1).
NOTE: Using larger amounts of fresh SAT increases the yield of hSATMVEC during isolation and has the highest chance of successful isolation and hSATMVEC culture. - Immediately place SAT into ice-cold magnetic-activated cell sorting (MACS) tissue storage solution in a 1.5 mL microcentrifuge tube before transferring to the laboratory.
NOTE: For the highest chance of successful isolation hSATMVEC isolation should be performed as soon as possible. However, SAT can be stored for up to 24 h on ice prior to isolation if required. - Prepare a 1 mg/mL collagenase/dispase working solution as follows.
- First, reconstitute 500 mg of collagenase/dispase lyophilized powder in 5 mL of sterile water to form a collagenase/dispase stock solution with a concentration of 100 mg/mL.
- For each hSATMVEC isolation, dilute 100 µL of collagenase/dispase stock solution in 10 mL of cold Hanks′ Balanced Salt solution to end up with a 1 mg/mL working solution.
- In a laminar flow cabinet, use two scalpels to mince tissues into ~1 mm3 pieces in 500 µL of 1 mg/mL collagenase/dispase solution on the lid of a Petri dish, triturate and transfer to a clean 50 mL centrifuge tube.
- Wash the Petri dish lid with 4.5 mL of fresh 1 mg/mL collagenase/dispase solution and add to the 50 mL centrifuge tube. Leave to digest for 30 min at 37 °C in a tube rotator at 20 rpm. Stop the digestion process by adding 10 mL of complete EC growth media MV.
- Triturate the digested mix and pass it through a 70 µm cell sieve. Rinse the sieve with 10 mL of 0.5% phosphate-buffered saline – bovine serum albumin (PBS-BSA) buffer. Centrifuge the sample at 300 x g for 10 minutes at room temperature and discard the supernatant. Repeat this step with another 5 mL of 0.5% PBS-BSA.
- Then, remove the dead cells using a dead cell removal kit. To do this, incubate the cell pellet in 200 µL of dead cell removal beads (vortex prior to use) for 15 min at room temperature (RT) in a 1.5 mL microcentrifuge tube.
- Attach an LS column with a 30 µm filter to the separator magnet and place a 15 mL centrifuge tube underneath. Wash the magnetic column once with 1 mL of dead cell removal binding buffer before adding the sample/bead suspension and allow it to passively pass through under gravity.
- Next, wash the column by adding 0.5 mL of binding buffer and allow it to passively pass through the column. Repeat this wash four times.
- Collect the eluate as a live cell fraction, spin the cells at 300 x g at RT for 10 min, and then wash and resuspend the resulting pellet in 400 µL of 0.5% PBS-BSA.
- Add 20 µL of anti-CD31 coated magnetic beads to the suspended cells and incubate for 20 min at 4 °C . Post incubation, centrifuge the sample at 300 x g for 5 min at RT and discard the supernatant. Resuspend the cell pellet in 500 µL of 0.5% PBS-BSA.
- Attach an MS column with a 30 µm filter to the separator magnet and place a 15 mL centrifuge tube underneath. Prime the column with 500 µL of 0.5% PBS-BSA. Repeat this step twice.
- Add the cell-microbead suspension and allow it to pass through under gravity. Wash the column with 500 µL of 0.5% PBS-BSA three times. The flow-through in the centrifuge tube underneath the column contains the CD31– fraction.
- To collect the CD31+ fraction (i.e., the fraction containing hSATMVECs), remove the MS column from the separator magnet and place it into a fresh 15 mL centrifuge tube. Add 1 mL of 0.5% PBS-BSA, and in one smooth action, apply the column plunger to release the captured hSATMVECs.
- Centrifuge the sample at 300 x g for 5 min at RT and discard the supernatant. Resuspend the cell pellet in 1 mL of complete EC growth media MV and divide the 1 mL cell solution between one or two wells (depending on pellet size) of a 2% gelatin-coated 24-well plate (Passage 0).
NOTE: Do not be concerned if there are few adherent cells in the first few days post-isolation. - Change media every 3 days. Culture cells at 37 °C with 5% CO2. Once isolated cells reach ~80% confluency (2-4 weeks), passage them onto a single well of a six-well plate (passage 1).
NOTE: Subsequent passages can re-plate cells from one confluent donor well to recipient wells. Experiments were performed in cells of passage 2-4 generation after cells had demonstrated >99% purity using flow cytometry (see section 3). Cells maintained typical endothelial morphology until at least passage 5.
3. Flow cytometry
- Prior to flow cytometry, visually check hSATMVECs to ensure that they appeared confluent and morphologically representative. Perform flow cytometric assessment of hSATMVECs at passage 2, using cells from a single well of a 6-well plate.
- Wash cells twice with PBS by adding 500 µL of PBS well and aspirating each time. Then, add 300 µL/well of warm trypsin/EDTA (0.25%) solution. Incubate at 37 °C with 5% CO2 for 2 min.
- Once detached, neutralize trypsin/EDTA solution with 700 µL of complete EC growth media MV and transfer to a 1.5 mL microcentrifuge tube.
- Centrifuge the cell suspension at 400 x g for 8 min at RT. Discard the supernatant without disturbing the pellet. Next, resuspend the cell pellet in 1 mL MACS buffer and divide between two 1.5 mL microcentrifuge tubes labeled unstained control and stained sample (500 µL per well).
- Add an additional 500 µL of MACS buffer to each microcentrifuge tube, before centrifuging again at 400 x g for 8 min at RT.
- Discard the supernatant and resuspend the cell pellet in 100 µL of MACS buffer for unstained control and 100 µL staining cocktail (Supplementary Table 1) for the stained sample. Stain the cells with CD45-FITC (the pan-leucocyte marker), as well as CD144-PE and CD31-PerCP (which are expressed by endothelial cells).
- Briefly vortex the suspended cells for 5 s, then incubate at 4 °C for 10 min. Next, add 1 mL of MACS buffer to each tube, centrifuge again at 400 x g for 8 min at RT, and discard the supernatant.
- Finally, resuspend the cell pellet in 500 µL of MACS buffer and transfer it into a fresh 1.5 mL microcentrifuge tube. Place the labeled tube in a covered ice box ready for analysis.
NOTE: All the flow cytometry analyses included were performed on a Beckman Coulter Cytoflex 4-laser flow cytometer system (using only the 488 nm excitation laser). - Set up the maximum emission wavelength and filter for each fluorochome as follows: CD45-FITC – emission maximum 520 nm, filter 525/50; CD144-PE – emission maximum 578 nm, filter 585/40; CD31-PerCP – emission maximum 675 nm, filter 655-730.
- As illustrated in Figure 2, record data for 10,000 cells per sample in a singlet gate (P2). Check that P1 surrounds a major cell cluster and that most of these cells fall in the P2 singlet gate. Ensure the unstained control has minimal CD45–CD144+CD31+ cells as % of singlets.
- Record the percentage of CD45-CD144+CD31+ cell singlets in the stained sample.
4. Endothelial cell doubling time and cell proliferation (Figure 3)
- At passages 2 and 3, count the number of viable hSATMVECs for each sample using hemocytometry. Record the date and time of each cell count.
- Calculate the number of population doublings between these points according to the equation: doubling time = (duration x log(2))/(log (final concentration)-log(initial concentration)).
NOTE: An online calculator is available at https://doubling-time.com/compute.php. - Assess the hSATMVECs proliferation using a commercially available cell proliferation imaging kit. Seed hSATMVECs at a density of 20,000 cells per well in a 24-well plate and leave them overnight in complete EC growth media MV to recover.
- The next day, add 5-Ethynyl-2´-deoxyuridine (EdU) to each well diluted in complete EC growth media MV at a final concentration of 10 µM. Incubate at 37 °C (5% CO2) for 2 h.
- Remove the EdU-containing media and wash each well twice with PBS. Fix the cells with 4% paraformaldehyde for 15 min at RT. Wash each well twice with PBS and add 500 µL of 0.5% Triton X-100 in tris-buffered saline (TBS) buffer. Leave to incubate at RT for 20 min.
NOTE: This permeabilizes the cell membrane, allowing entry of Alexa fluor 488-labeled azide into the cell. - Prepare the Alexa fluor 488-labeled azide cocktail as per the manufacturer's instructions, depending on the number of wells (see6). Wash each well twice with PBS before adding 100 µL of Alexa fluor 488-labeled azide cocktail and incubate for 30 min at RT protected from light.
NOTE: The Alexa fluor 488-labeled azide cocktail reacts with the EdU in a click reaction. - Remove the Alexa fluor 488-labeled azide cocktail and wash twice with PBS. Add 500 µL of propidium iodide per well and incubate for 20 min at RT.
NOTE: This step counterstains nuclei (both proliferating and non-proliferating) red.
Remove propidium iodide, wash twice with PBS, and leave each well in 500 µL of PBS for imaging. - Image each well in 4 high-powered fields at 10x magnification, with 495/519 nm excitation/emission for the 488 nm azide (see Figure 3C).
NOTE: The images in the figures were captured using a live-cell analysis system at 10x magnification with 800 ms exposure time. - Count the number of proliferating cells (green) and express as a percentage (%) of total cells within each high-powered field (average of 4 regions per well).
5. Endothelial cell tube formation
- Leave Matrigel (basement membrane matrix; BMM) to defrost overnight on ice. On the next day, with the plate on ice, add 160 µL of BMM to each well of a 24-well plate as required. Tilt the plate to get full coverage of each well with BMM. Place the plate in an incubator at 37 °C with 5% CO2 to set while preparing cells.
- Seed hSATMVECs at 100,000 cells (in 1 mL of media) per well. Pipette at the side of the well and take care to pipette slowly to avoid the matrix detaching. Incubate the plate at 37 °C with 5% CO2 for 4 h.
NOTE: At this point, the plate is ready to be imaged. The results and figures below the phase imaging on the live-cell analysis system at 10x magnification was used in 5 different well areas (see Figure 3D). - Count the number of whole tubes in each high-power field and calculate an average value for each sample.
6. Insulin stimulation of hSATMVEC
- Culture hSATMVEC in a 6-well plate at 37 °C with 5% CO2. Once confluent, remove complete endothelial cell growth media MV and wash twice with PBS.
- Add 500 µL of serum starvation media (endothelial cell growth media MV without supplements) to each well and leave to incubate at 37 °C with 5% CO2 for 4 h. During this time, prepare 500 µL aliquots of increasing insulin concentrations (0-150 µM) prepared in serum starvation media.
- After being serum starved for 4 h, remove media from the wells, add 1 mL of insulin-containing media (with increasing concentrations) to each well, and incubate for 10 min at 37 °C with 5% CO2.
- Wash twice with cold PBS before adding 100 µL of protein lysis buffer containing protease and phosphatase inhibitors to lyse cells for protein. Quantify the protein using BCA assay.
NOTE: In the experiment described below, cell lysates were incubated for 30 min in an ice-bath and centrifuged at 20,000 x g for 15 min. Prior to electrophoresis, protein samples were boiled to denature the proteins at 95 °C for 5 min. Proteins were resolved on a NuPAGE 4-12% Bis-Tris Gel and transferred to a nitrocellulose membrane. Immunoblot analysis was performed according to standard protocols using relevant phosphoprotein antibodies and total protein antibodies (according to the manufacturer's instructions). An appropriate Ig/HRP secondary antibody was used to detect the primary antibody (according to the manufacturer's instructions). Levels of protein were quantified using densitometry based on the intensity of bands from each sample. ß-actin was used as loading control where appropriate.
7. hSATMVEC-adipocyte co-culture set up (Figure 4)
NOTE: In the results below, commercially available human white subcutaneous preadipocytes at passage 2 from a single male Caucasian donor were used in all adipocyte assays. Preadipocytes were initially expanded from the vendor-supplied vial (passage 0) into twelve cryovials containing cryo-SFM freezing media (passage 1).
- Each 24-well co-culture plate requires one cryovial of preadipocytes (passage 1). Rapidly thaw each vial and plate into a T75 flask containing 12-15 mL of warm PGM-2 media (containing 10% FBS, 30 µg/mL L-glutamine, and 15 ng/mL GA-1000 SingleQuots). Change media every 3 days until 90% confluent.
- Once 90% confluent, wash the human white subcutaneous preadipocytes with PBS and then add 1 mL of trypsin/EDTA solution (0.25%). Leave at RT for 2 min and confirm detachment with light microscopy. Add 23 mL of PGM-2 media to neutralize the trypsin/EDTA and make a 24 mL preadipocyte-suspended solution.
- Put 1 mL of suspended human subcutaneous white preadipocyte solution into each well of a 24-well co-culture companion plate and grow to confluency (usually 2-3 days).
- While growing to confluence, prepare preadipocyte differentiation media (PDM). To prepare PDM, make a 2x PDM stock by adding a proprietary mix of insulin, dexamethasone, indomethacin, and isobutyl-methylxanthine to PGM base media. Dilute 2x PDM in a 1:1 ratio with PGM to make 1x PDM.
- Once confluent, differentiate the human subcutaneous white preadipocytes by changing media to 1 mL of 1x PDM media into each well (Day 0). Leave the human subcutaneous white preadipocytes to incubate at 37 °C 5% CO2 for 10 days (without media changes) to fully differentiate. Monitor differentiation using light phase microscopy (see Figure 4B).
NOTE: Differentiated adipocytes cannot be passaged and can be used for assays from day 10 to day 12. Adipocyte differentiation can be measured by mRNA amplification of leptin, adiponectin, and PPAR-γ. - On day 6 of differentiation, seed hSATMVECs at a density of 5 x 104 cells per insert in 500 µL complete EC growth media MV on transwell inserts (0.4 µM membrane). Place the transwell inserts into a well with 500 µL of complete EC growth media MV () and grow to confluence at 37 °C in 5% CO2.
- On day 10, when the adipocytes are fully differentiated, remove half the PDM media from each well and transfer the transwell inserts containing confluent hSATMVEC in their own media (ECGM-MV) to each well (see Figure 4A).
- Leave cells in co-culture for 24 hours before removing the transwell inserts and perform assays assessing adipocyte function.
NOTE: At this time point, adipocytes can also be lysed for either protein or RNA isolation if required.
8. Adipocyte 2-(N-(7-Nitrobenz-2-oxa-1,3-diazol-4-yl)Amino)-2-Deoxyglucose (2-NBD)-glucose uptake
- After 24 h in co-culture, remove cell inserts containing hSATMVEC. Next, add 2-NBD-glucose to the media in each well to achieve a final concentration of 20 µM. Protect from light and incubate for 30 min at 37 °C with 5% CO2.
- Wash the cells twice in PBS and fix the adipocytes using 500 µL of 4% paraformaldehyde (PFA) for 15 min at RT. Wash the cells three times in PBS before leaving in 100 µL of PBS.
NOTE: At this point, the adipocytes are ready to be imaged. In the included figures, phase imaging and green light (excitation 440-480 nm/emission 504-544 nm) were obtained on the a the live-cell analysis system at 10x magnification in four high-powered fields (see Figure 4C). - Quantify the level of glucose uptake by quantifying the percentage green of the total area using thresholding in ImageJ (or any other similar software package).
Representative Results
hSATMVEC purity and phenotype
Isolated hSATMVEC from control patients (that is, those people without a history of cardiometabolic disease) were 99.5% CD31+CD144+CD45- on flow cytometry (Figure 2). Isolated hSATMVEC had a cobblestone-like morphology typical of ECs (Figure 3A). hSATMVECs had a mean population doubling time of 56.6 h ± 8.1 h (mean ± SEM, n = 10) (Figure 3B), and active DNA replication in hSATMVECs was confirmed using a cell proliferation imaging kit (Figure 3C).
hSATMVEC behaved like functioning MVECs and formed tubes in Matrigel (Figure 3D). The relative expression of key proteins involved in the insulin signaling Akt-eNOS pathway is shown in Figure 3E. Both eNOs and Akt demonstrated increases in insulin induced phosphorylation, represented as the ratio of phosphorylated protein/total protein normalized to ß-actin (Figure 3E).
hSATMVEC-adipocyte co-culture
An illustrative model of hSATMVEC-adipocyte co-culture can be seen in Figure 4A. As the human subcutaneous white preadipocytes become more differentiated, one will notice the development of lipid vacuoles (Figure 4B), which can be quantified by Oil Red O staining (Figure 4B).
Illustrative phase contrast and fluorescence imaging (excitation 440-480 nm/emission 504-544 nm) of differentiated adipocytes following 30 min of incubation with 20 µM 2-NBD glucose is shown in Figure 4C. Glucose uptake can be quantified by measuring green area as a percentage of total cell area.
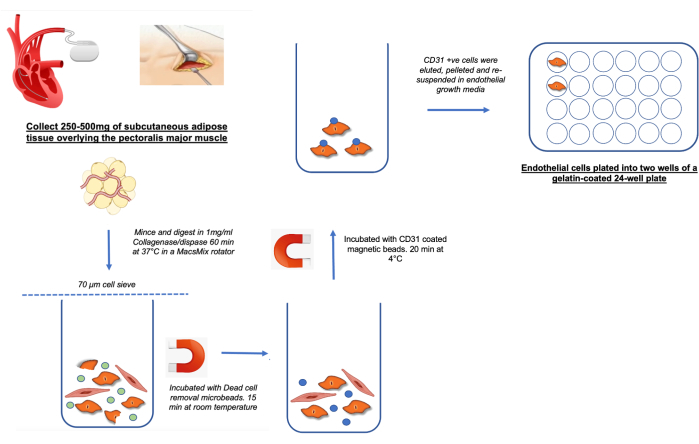
Figure 1: Schematic demonstrating the harvesting and processing of hSATMVECs Please click here to view a larger version of this figure.
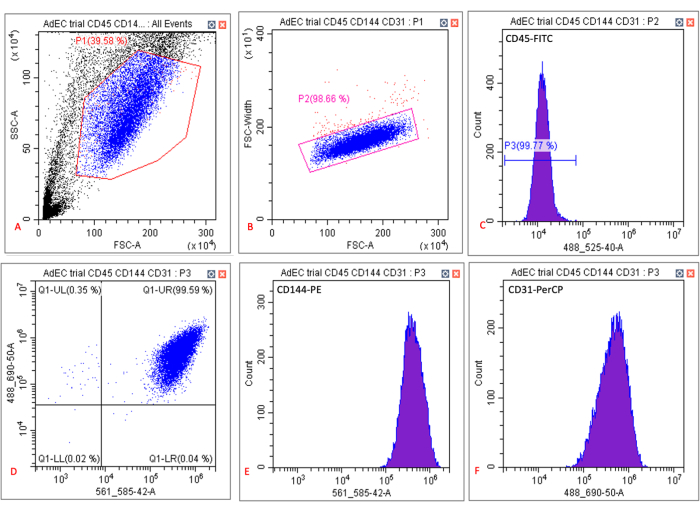
Figure 2: Typical output of flow cytometry analysis of cultured hSATMVECs. (A) Scatter plot of side scatter area (SSC-A) and forward scatter area (FSC-A) showing gating (red box) of cultured hSATMVECs around specific cell population density. (B) Scatter plot of forward scatter width (FSC-Width) and FSC-A showing gating (red box) of cultured hSATMVECs around specific cell population density. (C) Histogram showing fluorescence of gated cells to CD45-FITC. (D) Scatter plot of fluorescence intensity of CD144-PE (x-axis) and CD31-PerCP (y-axis). (E) Histogram showing fluorescence of gated cells to CD144-PE. (F) Histogram showing fluorescence of gated cells to CD31-PerCP. Please click here to view a larger version of this figure.
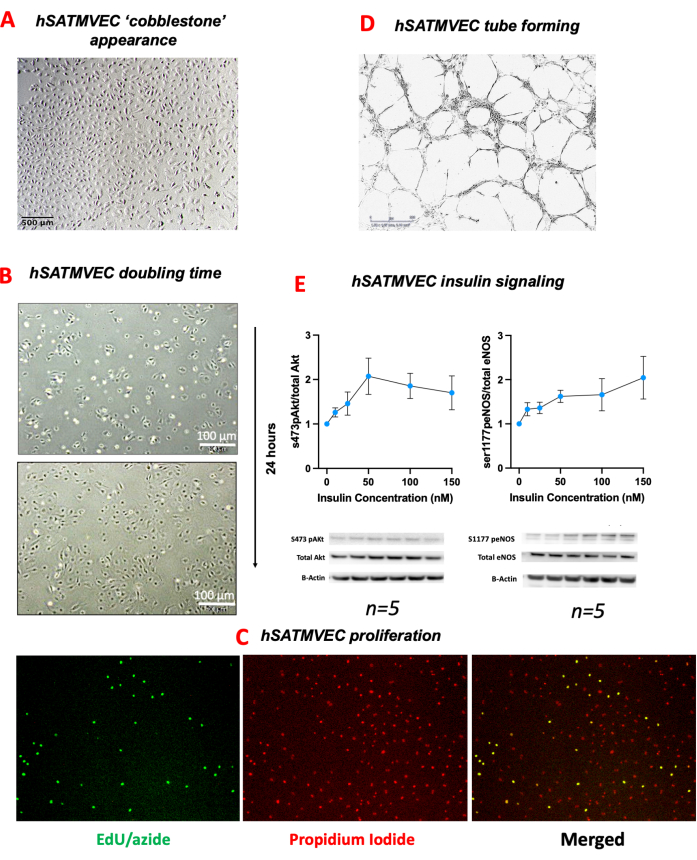
Figure 3: hSATMVEC phenotype. (A) Light microscopy image of hSATMVEC near confluence showing cobblestone-like appearance. (B) hSATMVEC doubling time – Light microscopy of HATEC taken 24 h apart demonstrating the extent of cell proliferation. (C) hSATMVEC proliferation. Fluorescence microscopy of hSATMVEC with propidium iodide and EdU/Alexa-fluor 488 from control subjects. (D) hSATMVEC tube formation from control subjects (images taken at 4x magnification). (E) Insulin stimulation of HATECs – showing relative expression of phosphorylated Akt (serine 473) to total Akt (left panel) phosphorylated eNOS (serine 1177) to total eNOS (right panel) at increasing insulin concentrations with illustrative western blots beneath standardized to B-actin. Data are shown as mean ± SEM. Sample sizes are beneath each panel. Abbreviations: 5-Ethynyl-2´-deoxyuridine (EdU), human subcutaneous adipose tissue microvascular endothelial cells (hSATMVEC), standard error of the mean (SEM). Please click here to view a larger version of this figure.
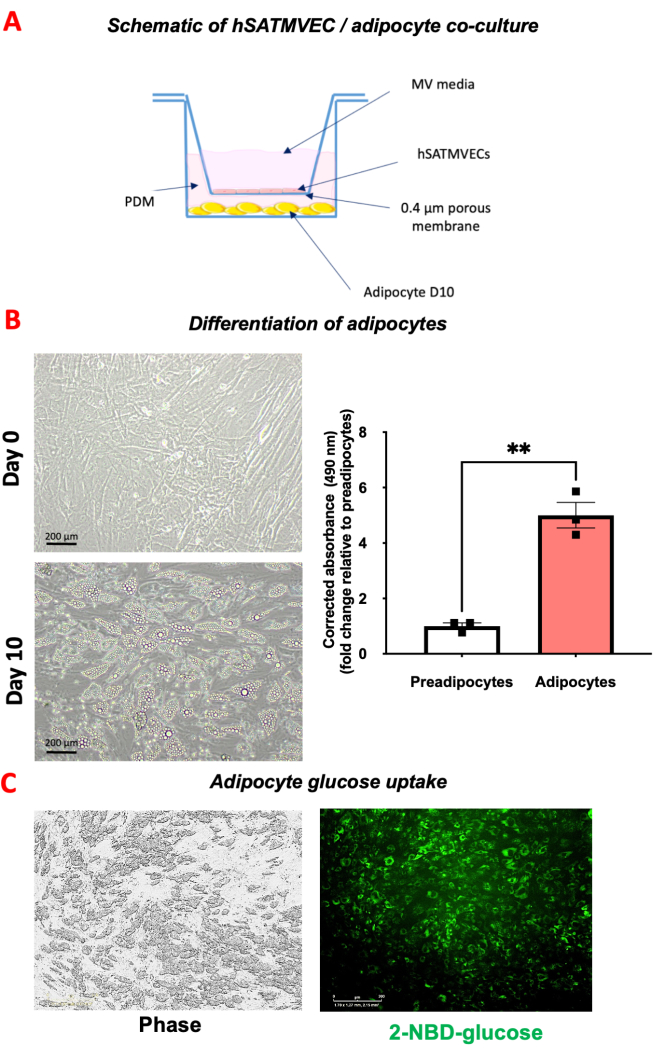
Figure 4: hSATMVEC-adipocyte co-culture. (A) Schematic image of hSATMVEC-adipocyte co-culture. (B) Differentiation of adipocytes. The left panel shows preadipocytes at day 0 and the right panel shows day 10 differentiated adipocytes after the addition of PDM. The bottom figure shows the amount of lipid stored in adipocytes and preadipocytes stained with Oil Red O. (C) Glucose uptake assay. The left panel shows phase imaging of adipocytes following co-culture and incubation with 20 µM of 2-NBD glucose for 30 min. The right panel shows green imaging from which glucose uptake (as % green of total area) can be quantified. Data are shown as mean ± SEM. Abbreviations: Day 10 (D10), human subcutaneous adipose tissue microvascular endothelial cells (hSATMVEC), preadipocyte differentiation media (PDM) Please click here to view a larger version of this figure.
Supplementary Table 1: Staining cocktail for flow cytometry. Please click here to download this File.
Discussion
This study describes a technique of isolating hSATMVEC taken from SAT during routine implantation of CIEDs. We demonstrate that the hSATMVEC isolated has high purity, expresses EC-specific transmembrane proteins CD144 and CD31, and shows no significant expression of the leukocyte CD45. We go on to show that, in a reproducible and reliable manner, isolated hSATMVEC proliferate and can be used experimentally to study the intracellular machinery involved in insulin signaling and angiogenesis. In addition to being able to culture them in isolation, they can also be used in co-culture to study hSATMVEC-adipocyte cross-talk.
Endothelial cells used in basic and translational research are commonly sourced from large vessels, such as the aorta and human umbilical vein, or microvasculature. These sources both have their own respective limitations7,8; endothelial cells from large vessels are either difficult to access (in the case of aortic tissue) or are derived from neonatal tissue with potentially differing physiology and environmental exposure9. Using endothelial cells isolated from tissue taken during CIED implantation allows for the investigation and experimentation of cellular physiology within specific real-world patient groups. CIEDs are implanted for a variety of indications, including in patients with bradyarrhythmias, heart failure and primary and secondary prevention of ventricular tachyarrhythmias10. These patients often have multiple co-morbidities, including diabetes, obesity, and coronary artery disease, which are a major global focus of cardiovascular research11,12,13. Moreover, while the illustrative data in this paper pertains to control patients, we have applied these techniques to isolate and study SATMVEC from a range of patients, including those with advanced heart failure and/or type 2 diabetes mellitus.
Not infrequently, we encounter problems with poor hSATMVEC yields following attempted cell isolation. This risk can be significantly reduced by using a larger starting volume of SAT to isolate hSATMVEC. In addition, we encounter this more frequently in SAT from people with cardiometabolic disease, and in particular, diabetes.
One limitation of this technique is that isolated hSATMVEC can only undergo a limited number of passages. In our experience after passage 5, regardless of patient phenotype, hSATMVEC proliferation slows significantly. In addition, hSATMVEC isolated using this technique do not proliferate well when too sparsely populated; therefore, we recommend not passaging hSATMVEC at a ratio greater than 1:6. as mentioned on page 1. We have successfully thawed and reanimated hSATMVEC stored in liquid nitrogen for up to 4 years, and in our experience, the chance of reanimation is greater when cryopreserved at a lower passage number (we usually cryopreserve hSATMVEC at passage 2).
Tissue taken at CIED insertion is freely available and can be harvested at no detriment to the patient. Therefore, an easy-to-access, relatively non-invasive source of endothelial cells from these patient groups is of great benefit in conducting targeted research. While the representative images in this paper are derived from 'control' patients (that is, patients without a diagnosis of heart failure or diabetes, albeit with an indication for CIED implantation), we have successfully isolated, cultured, and co-cultured SATMVECs from patients with heart failure, diabetes, and a combination of these pathologies. Moreover, these techniques can also be applied to other microvascular beds, including skeletal muscle, and we are currently optimizing a model of skeletal muscle MVEC-myocyte crosstalk.
hSATMVECs can be isolated from human tissue taken at the time of CIED insertion and are of sufficient purity to be used experimentally to study microvascular dysfunction and endothelial cell-adipocyte cross-talk in people with and without cardiometabolic disease.
Disclosures
The authors have nothing to disclose.
Acknowledgements
We are very grateful to the Faculty of Biological Sciences Bioimaging Department (University of Leeds, United Kingdom) for the use of the flow cytometry facility, which was supported by Biotechnology and Biological Sciences Research Council grant funding (BBSRC BB/R000352/1). SS was supported by a British Heart Foundation Clinical Research Training Fellowship (FS/CRTF/20/24071). CL was supported by a British Heart Foundation PhD studentship (FS/19/59/34896). LDR was supported by the Diabetes UK RD Lawrence Fellowship award (16/0005382). RMC was supported by a British Heart Foundation Intermediate Clinical Research Fellowship (FS/12/80/29821). MTK is a British Heart Foundation Professor of Cardiovascular and Diabetes Research (CH/13/1/30086) and holds a British Heart Foundation program grant (RG/F/22/110076)
Materials
| 170L CO2 Incubator | GS Biotech | 170G-014 | |
| 2-NBDG (2-(N-(7-Nitrobenz-2-oxa-1,3-diazol-4-yl)Amino)-2-Deoxyglucose) | Invitrogen | N13195 | |
| 4% PARAFIX buffered histological fixative | VWR Chemicals | PRC/R/38/1 | |
| Akt (tAkt) Rabbit 1:1000 | Cell Signalling Technology | 9272 | |
| BD Venflon Pro Safety 14 g x 45 mm, Orange, 50/pk | Medisave | 393230 | |
| Bovine Serum Albumin solution, 7.5% | Merck | A8412-100ML | |
| CD144 (VE-Cadherin) Antibody, anti-human, PE, REAfinity | Miltenyi Biotec | 130-118-495 | |
| CD31 Antibody, anti-human, PerCP-Vio 700, REAfinity | Miltenyi Biotec | 130-110-811 | |
| CD31 MicroBead Kit, human, 1 kit | Miltenyi Biotec | 130-091-935 | |
| CD45 Antibody, anti-human, FITC, REAfinity | Miltenyi Biotec | 130-110-769 | |
| Cell Extraction Buffer | Invitrogen | FNN0011 | |
| Centrifuge 5804 R | Eppendorf | 5805000060 | |
| Click-iT EdU Cell Proliferation Kit for Imaging, Alexa Fluor 488 dye | Invitrogen | C10337 | Cell proliferation imaging kit |
| Collagenase/Dispase, 500 mg | Roche/Merck | 11097113001 | |
| Corning Matrigel Growth Factor Reduced (GFR) Basement Membrane Matrix | Corning | 354230 | Basement Membrane Matrix |
| Corning 100 mm TC-treated Culture Dish | Corning | 430167 | |
| Costar 24-well Clear TC-treated Multiple Well Plates, Individually Wrapped, Sterile | Corning | 3526 | |
| Costar 6-well Clear TC-treated Multiple Well Plates, Individually Wrapped, Sterile | Corning | 3516 | |
| CytoFLEX S – 4 laser flow Cytometer | Beckman | ||
| Dead Cell Removal Kit | Miltenyi Biotec | 130-090-101 | |
| Dulbecco′s Phosphate Buffered Saline | Merck | D8537-500ML | |
| EASYstrainer Cell sieve for 50 mL tubes, 70 µm mesh, Blue, sterile, 50/pk | Greiner Bio-One | 542070 | |
| Endothelial Cell Growth Medium MV | PromoCell | C-22020 | |
| Eppendorf Safe-Lock micro test tubes | Merck | EP0030120094 | |
| Ethylenediaminetetraacetic acid solution | Merck | E8008-100ML | |
| Falcon 24 Well TC-Treated Cell Polystyrene Permeable Support Companion Plate, with Lid, Sterile, 1/Pack, 50/Case | Appleton Woods | CF537 | |
| Falcon Permeable Support for 24 Well Plate with 0.4 µm Transparent PET Membrane, Sterile, 1/Pack, 48/Case | Appleton Woods | CF521 | |
| Freezing Medium Cryo-SFM | PromoCell | C-29912 | |
| Gelatin solution, 2% in water | Merck | G1393-100ML | |
| Gibco Antibiotic-Antimycotic (100x), 100mL | Fisher Scientific | 11570486 | |
| Gibco TrypLE Select Enzyme (1x), no phenol red | Fisher Scientific | 12563029 | |
| Hanks′ Balanced Salt solution | Merck | H6648-500ML | |
| Human Subcutaneous Preadipocyte Cells | Lonza | PT-5020 | |
| Incucyte ZOOM | Essen BioScience | Live-cell analysis system | |
| Insulin solution human | Merck | I9278-5ML | |
| LS Columns, 25/pk | Miltenyi Biotec | 130-042-401 | |
| MACS MultiStand | Miltenyi Biotec | 130-042-303 | |
| MACS Tissue Storage Solution | Miltenyi Biotec | 130-100-008 | |
| MACSmix Tube Rotator | Miltenyi Biotec | 130-090-753 | Tube Rotator |
| MS Columns, 25/pk | Miltenyi Biotec | 130-042-201 | |
| NuPAGE 4–12% Bis-Tris Gel | Invitrogen | NP0322BOX | |
| OctoMACS Separator | Miltenyi Biotec | 130-042-109 | |
| PGM-2 Preadipocyte Growth Medium-2 BulletKit | Lonza | PT-8002 | |
| Phospho (Ser1177) eNOS Rabbit 1:1000 | Cell Signalling Technology | 9570 | |
| Phospho-Akt (Ser473) Rabbit 1:1000 | Cell Signalling Technology | 4060 | |
| Pre-Separation Filters 30 µm, 50/pk | Miltenyi Biotec | 130-041-407 | |
| Propidium Iodide (PI)/RNase Staining Solution | Cell Signalling Technology | 4087 | |
| QuadroMACS Separator | Miltenyi Biotec | 130-090-976 | |
| Scalpel Disposable Sterile Style 10 | VWRI | 501 | |
| Screw cap tube, 15 ml, (LxØ): 120 x 17 mm, PP, with print | Sarstetd | 62.554.502 | |
| Screw cap tube, 50 ml, (LxØ): 114 x 28 mm, PP, with print | Sarstedt | 62.547.254 | |
| Screw cap tube, 50 ml, (LxØ): 114 x 28 mm, PP, with print | Sarstetd | 62.547.254 | |
| Total eNOS Mouse 1:1000 | BD Biosciences | 610297 | |
| Triton X-100, BioUltra, for molecular biology | Merck | 93443-500ML | |
| β-Actin (C4) Mouse 1:5000 | Santa Cruz Biotechnology | Sc-47778 |
References
- Bierhansl, L., et al. Central role of metabolism in endothelial cell function and vascular disease. Physiology. 32 (2), 126-140 (2017).
- Aird, W. C. Endothelial cell heterogeneity. Cold Spring Harb Perspect Med. 2 (1), a006429 (2012).
- Rajendran, P., et al. The vascular endothelium and human diseases. Int J Biol Sci. 9 (10), 1057-1069 (2013).
- Brown, O. I., Bridge, K., Kearney, M. T. Nicotinamide adenine dinucleotide phosphate oxidases in glucose homeostasis and diabetes-related endothelial cell dysfunction. Cells. 10 (9), 2315 (2021).
- Luk, C., Haywood, N. J., Bridge, K. I., Kearney, M. T. Paracrine role of the endothelium in metabolic homeostasis in health and nutrient excess. Front Cardiovasc Med. 26 (9), 882923 (2022).
- . Click-iT EdU Imaging Kits Available from: https://www.thermofisher.com/document-connect/document-connect.html?url=https://assets.thermofisher.com/TFS-Assets%2FLSG%2Fmanuals%2Fmp10338.pdf (2024)
- Bouïs, D., et al. Endothelium in vitro: A review of human vascular endothelial cell lines for blood vessel-related research. Angiogenesis. 4 (2), 91-102 (2001).
- Ades, E. W., et al. HMEC-1: establishment of an immortalized human microvascular endothelial cell line. J Invest Dermatol. 99 (6), 683-690 (1992).
- Chi, J. T., et al. Endothelial cell diversity revealed by global expression profiling. Proc Natl Acad Sci U S A. 100 (19), 10623-10628 (2003).
- Brignole, M., et al. 213 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy. Eur Heart J. 34 (29), 2281-2329 (2013).
- Greenspon, A. J., et al. Trends in permanent pacemaker implantation in the United States from 1993 to 2009: Increasing complexity of patients and procedures. J Am Coll Cardiol. 60 (16), 1540-1545 (2012).
- Mendis, S. A., Alwan, A. . Prioritized Research Agenda for Prevention and Control of Noncommunicable Diseases. , (2011).
- Brown, O. I., et al. Relationship among diabetes, obesity, and cardiovascular disease phenotypes: A UK biobank cohort study. Diabetes Care. 46 (8), 1531-1540 (2023).

.
