Induced Pluripotent Stem Cell Generation from Blood Cells Using Sendai Virus and Centrifugation
Summary
We propose a protocol for reprogramming peripheral blood mononuclear cells (PBMCs) into induced pluripotent stem cells (iPSCs). By plating the transduced blood cells onto matrix-coated plates with centrifugation, iPSCs are successfully induced from floating cells. This technique suggests a simple and effective reprogramming protocol for cells such as PBMCs and CBMCs.
Abstract
The recent development of human induced pluripotent stem cells (hiPSCs) proved that mature somatic cells can return to an undifferentiated, pluripotent state. Now, reprogramming is done with various types of adult somatic cells: keratinocytes, urine cells, fibroblasts, etc. Early experiments were usually done with dermal fibroblasts. However, this required an invasive surgical procedure to obtain fibroblasts from the patients. Therefore, suspension cells, such as blood and urine cells, were considered ideal for reprogramming because of the convenience of obtaining the primary cells. Here, we report an efficient protocol for iPSC generation from peripheral blood mononuclear cells (PBMCs). By plating the transduced PBMCs serially to a new, matrix-coated plate using centrifugation, this protocol can easily provide iPSC colonies. This method is also applicable to umbilical cord blood mononuclear cells (CBMCs). This study presents a simple and efficient protocol for the reprogramming of PBMCs and CBMCs.
Introduction
Stem cells have been one of the most attractive materials in clinical therapy for the last several decades1. The attractive properties of stem cells are pluripotency and the ability to self-renew. In 1981, the first embryonic stem cells (ESCs) were isolated from the mouse embryo2. However, when the technique was applied to human embryos, it faced several ethical issues.
In 2006, when Dr. Yamanaka and his team reprogrammed the first pluripotent cell from mouse somatic cells, the stem cell field regained its possibility and interest was rekindled3. By delivering several defined factors, pluripotent stem cells were successfully "induced" from adult somatic cells, and were thus named "induced pluripotent stem cells (iPSCs)." In 2007, this technique was applied to human cells4, yielding cells with the exact characteristics of ESCs but none of the ethical debate. Theoretically, iPSCs can be generated from any cell type obtained from any individual or patient. Patient-specific iPSCs are rising as a potential tool that can simulate the disease phenotypes and epigenetic conditions of each individual patient. Using gene editing or other methods that can reverse the pathogenic condition, patient-specific iPSCs can also be used in personalized medicine5. Moreover, iPSCs are less associated with immune rejection because they have the same immune identity as the donor, making auto-transplantation more feasible6. Therefore, iPSCs have become the most promising platform in disease modeling, drug screening, and regenerative therapies. Given these benefits, improved protocols that can give purer and higher yields in the least amount of time from the smallest cell source are constantly under development. One major consideration of finding the most efficient protocol for future application is the primary cell type. Most of the early iPSC generation protocols are optimized for adherent cells since the original iPSC lines were induced from skin fibroblasts4. However, the isolation and preparation of these cells are labor intensive. Also, the isolation of skin fibroblasts includes invasive surgical procedures that can become a major shortcoming for broader application.
Therefore, for the further use of iPSCs, a cell source with convenient acquisition is required. Blood is regarded as an ideal cell source since it is obtained through a rather minimally invasive procedure7-9. In this study, we developed a simple modification to the protocol generating hiPSCs from peripheral blood mononuclear cells (PBMCs). Without the difficult expansion process of a specific cell type, such as CD34+ cells, whole blood cells or PBMCs were serially plated onto matrix-coated plates by centrifugation after transduction with Sendai virus containing Yamanaka factors. This method reduced the time required for the attachment of transduced floating cells and decreased the loss of reprogrammed cells that were not able to attach on their own.
Protocol
Ethics Statement: This study protocol was approved by the institutional review board of The Catholic University of Korea (KC12TISI0861).
1. Isolation of Monocytic Cells from Blood
- Isolation of monocytic cells (Day -5)
- Obtain at least 10 ml of fresh blood from a blood draw in a cell preparation tube (CPT).
- Transfer the blood to a new 50-ml conical tube and dilute it with sterile phosphate-buffered saline (PBS) at a 1:4 ratio.
NOTE: A higher ratio of dilution can be used for higher purity. - Add 10 ml of density gradient media to a new 50-ml conical tube and carefully layer the diluted blood on top of the density gradient media. Centrifuge at 750 x g for 30 min at room temperature (RT) without a centrifugation brake.
- Carefully transfer the buffy layer to a new 50-ml conical tube, add 30 ml of PBS to the tube, and wash the cells.
- Centrifuge the cells at 515 x g for 5 min at RT.
- Discard the PBS and resuspend the cells in 0.5 ml of blood cell media.
- Count the cells and plate 1 x 106 cells per well of a 24-well plate. Add PBS to the surrounding wells to prevent evaporation.
- Stabilize the cells for 5 days at 37 °C in 5% CO2 before transduction. Add an additional 0.5 ml of fresh blood cell media on days 3-4 without disturbing the cells.
2. Transduction by Sendai Virus
- Transduction (Day 0)
- Collect and transfer the blood cells to a 15-ml conical tube and count them using a hemocytometer.
- Prepare 3 x 105 cells per transduction and centrifuge the cells at 515 x g for 5 min at RT.
- Discard the supernatant by suction and resuspend the cells in 0.5 ml of blood cell media.
- Transfer the cells to a well of a non-coated 24-well plate.
- Thaw the Sendai virus mixture in ice and add it to the suspended cells. Add Sendai virus to the cells based on the manufacturer's recommendations.
- Seal the plate with a sealing film and centrifuge it at 1,150 x g for 30 min at 30 °C.
- After centrifugation, incubate the cells at 37 °C in 5% CO2 overnight (O/N).
- Cell transfer to feeder matrix (Day 1)
- The next day, coat a 24-well plate with vitronectin. Dilute the vitronectin solution in PBS for a final 5 µg/ml concentration. Add 1 ml of vitronectin to a well of a 24-well plate and incubate it at RT for at least 1 hr. Remove the coating solution before use. Coated plates can be stored in RT for 3 days.
- Transfer all the media containing the cells and the virus to the coated well.
- Collect the remaining cells with an additional 0.5 ml of fresh blood cell media and add it to the cell-containing well.
- Centrifuge the plate at 1,150 x g for 10 min at 35 °C.
- After centrifugation, remove the supernatant, add 1 ml of iPSC media, and maintain the cells at 37 °C in 5% CO2 O/N.
- Second cell transfer (Day 2)
- Coat the wells of a new 24-well plate with 5 µg/ml vitronectin, as described in step 2.2.1. Use one well of the plate for each transduction.
- Transfer the cell suspension from the first plate to the newly coated vitronectin plate.
NOTE: If not needed, suspension cells can be discarded. The procedure mentioned in step 2.3 can be repeated 2-3 times with the suspension cells. If the steps will be repeated, harvest the cells. - Meanwhile, add 1 ml of iPSC media to the well of the first plate, for maintenance, and incubate it at 37 °C in 5% CO2 O/N.
- Maintain the attached cells at 37 °C and 5% CO2 and perform a daily media change with fresh iPSC media. Colonies will appear on days 14-21 after transduction.
- Centrifuge the newly coated plate containing the suspension cells at 1,150 x g and 35 °C for 10 min.
- After centrifugation, incubate the cells at 37 °C in 5% CO2 O/N.
- The next day, remove the supernatant and replace it with fresh iPSC media.
NOTE: The procedure mentioned in step 2.3 can be repeated 2-3 times with the suspension cells. If the steps will be repeated, harvest the cells in the supernatant and repeat step 2.3. - Maintain the attached cells with daily media changes until 80% confluency is reached.
3. Reprogrammed Cell Maintenance
- Early maintenance after the 24-well plate culture
- 7-10 days after transduction, once the cells are confluent, prepare a vitronectin-coated, 60-mm dish. Dilute vitronectin solution in PBS for a final 5 µg/ml concentration. Add 1 ml of vitronectin to the dish and incubate it at RT for at least 1 hr.
- Wash the cells with PBS and add 1 ml of PBS/1 mM EDTA to detach the cells.
- Incubate them at 37 °C and 5% CO2 for 2 min.
- Harvest the cells and centrifuge them at 250 x g and RT for 2 min. Remove the supernatant and resuspend the cells in 3 ml of fresh iPSC media.
- Plate all resuspended cells onto the newly coated 60-mm dish.
- Add 10 mM RHO kinase inhibitor to the cells and maintain them at 37 °C in 5% CO2 until the cells are 80% confluent.
- Split for colony appearance (Subcloning Preparation)
- Prepare a vitronectin-coated, 100-mm dish, as described in step 3.1.2.
- Wash the cells with PBS and add 1 ml of PBS/1 mM EDTA to detach the cells.
- Incubate them at 37 °C and 5% CO2 for 2 min.
- Harvest the cells and centrifuge them at 250 x g and RT for 2 min.
- Count the cells using a hemocytometer and prepare 1 x 104 cells per dish.
- Centrifuge the cells at 250 x g and RT for 2 min.
- Resuspend 1 x 104 cells in 6 ml of iPSC media, plate them onto the coated 100-mm dish, and add 10 mM RHO kinase inhibitor to the media.
- Incubate the cells at 37 °C in 5% CO2 for a week until large colonies appear.
NOTE: Maintain and expand the colonies for subcloning. Subcloning is usually done in under 5 passages.
- Colony picking using iPSC colony detaching solution
- A week before colony picking, seed 1 x 104 cells in a vitronectin-coated, 100-mm dish, as mentioned in step 3.2.7.
- Prepare a vitronectin-coated, 60-mm dish by adding 2 ml of vitronectin solution and incubating at RT for at least 1 hr.
- By observing through a microscope (40X or 100X magnification), mark colonies with clear boundaries using a marker pen. Remove the vitronectin solution from the new plate made in step 3.3.2 and add 6 ml of iPSC media supplemented with 10 mM RHO kinase.
- Remove the culture medium from the cells and wash them with 3 ml of PBS.
- Add 1 ml of iPSC colony detaching solution and incubate them for 30 s at RT.
- Remove the solution from the plate and incubate it at RT for additional 30 sec.
- Using a P200 pipette, draw 200 µl of media from the plate and detach the targeted colonies by pipetting. Transfer the scattered colonies to the new 100-mm dish.
- Incubate and maintain the cells at 37 °C in 5% CO2.
NOTE: After obtaining a pure iPSC colony, cells were maintained until they reached passage 10. Characterization was done after at least 10 passages. Antibody dilutions and primer information are shown in Tables 1 and 2.
Representative Results
This protocol presents a simple method to reprogram PBMCs isolated from blood. Using the combination of serial plating and centrifugation, iPSCs were successfully generated. With this method, iPSCs could be generated with a small amount of whole blood cells without isolating or expanding a specific cell type. We successfully generated iPSCs from only 1×104 cells in a small cell culture plate.
Before reprogramming, blood cells were isolated using density gradient media. Blood cells were transduced 5 days after isolation. Figure 1A illustrates the scheme of the reprogramming method for the suspension cells. After isolation, PBMCs were transduced with Sendai virus containing Yamanaka factors in a non-coated well. The next day, the suspension cells were harvested and plated onto a vitronectin-coated plate using centrifugation, while the cells attached to the non-coated well were discarded. The attached cells that appeared on the vitronectin-coated plate were retained and expanded further. Attached cells were maintained with daily media changes using iPSC media. The plating process with centrifugation was repeated for the remaining suspension cells.
Reprogrammed iPSCs could be distinguished by their distinct morphology several days after transduction. However, during reprogramming, it was hard to expand the reprogrammed cells in a pure form. At the early stage of reprogramming, the iPSCs were mixed with attached non-reprogrammed differentiated cells (Figure 2A). The arrow in Figure 2A shows the iPSC-like cell types in the image. Before expansion, the iPSCs and other cells were difficult to discriminate. Therefore, a pure colony was only obtained by the colony picking process. By seeding the cells in a low density, colonies that were large enough for picking were obtained, as shown in Figure 2B. After isolating the colony, the cell clumps were dissociated into single cells and cultured (Figure 2C). Pure iPSC colonies were seen afterwards (Figure 2D). After the pure iPSCs were expanded, the quality of the cells was tested. Cells were stained with alkaline phosphatase to confirm the undifferentiated state of the iPSCs (Figure 3A). Colonies derived from isolated iPSCs all showed positive staining. Pluripotent markers were confirmed by immunofluorescence staining, shown in Figure 3B. The reprogrammed cells highly expressed pluripotent markers such as SSEA4, OCT4, SOX2, TRA-1-81, KLF4, and, most importantly, TRA-1-60. The expression of pluripotent markers was confirmed by RT-PCR, shown in Figure 3C. OCT4 and SOX2 were detected, as shown in the fluorescence data. Additional markers such as NANOG, DPPA5, TDGF1 were positively expressed as well.
For further analysis, a karyotype analysis was done. As shown in Figure 4A, the generated iPSCs showed a normal chromosomal pattern. To confirm true pluripotency, the cells were differentiated into ectoderm, mesoderm, and endoderm. The generated iPSCs successfully differentiated into all three germ layers, seen in Figure 4B. Since Sendai virus is known for its integration-free property, the removal of viral DNA is shown in Figure 4C. One out of three cells tended to have viral DNA remain, even after several passages. However, the integrated gene was removable by subcloning processes.
In conclusion, we have shown a protocol generating iPSCs from floating PBMCs. The protocol showed high efficiency and required only a small amount of blood. The generated iPSCs had high pluripotency and avoided viral integration.
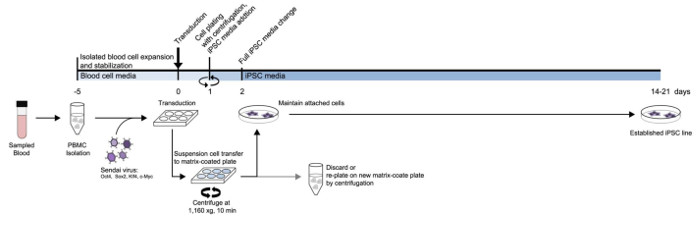
Figure 1: Scheme of the iPSC generation protocol from PBMCs. A detailed diagram of the designed protocol based on the medium type and timeline. Please click here to view a larger version of this figure.
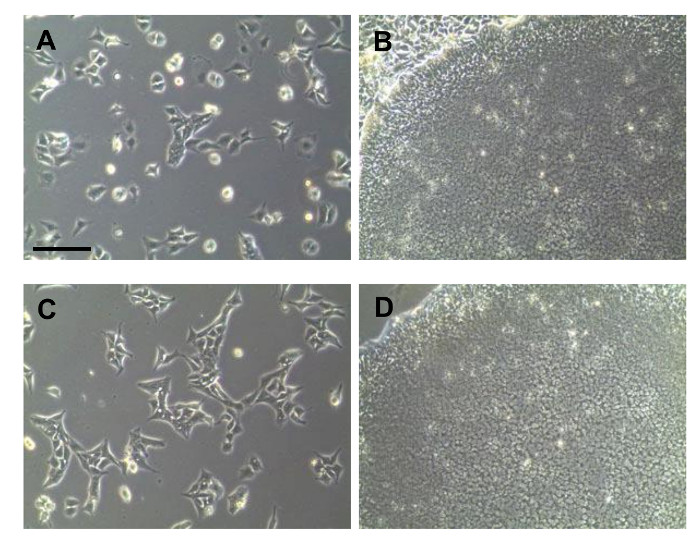
Figure 2: Bright-field image of iPSCs generated from PBMCs. (A) Early morphology of reprogrammed cells. (B) Image of a colony before picking. (C) Cells after the colony picking purification process. (D) Morphology of a pure colony. All scale bars indicate 200 µm. Please click here to view a larger version of this figure.
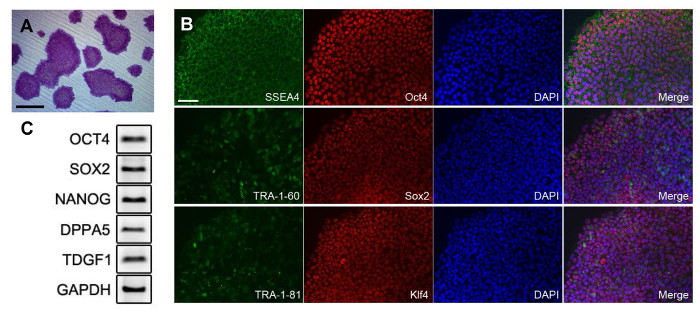
Figure 3: Pluripotency of iPSCs generated from PBMCs. (A) Colonies stained with alkaline phosphatase. (B) Fluorescence image of the generated iPSCs. The antibody dilution ratio is shown in Table 1. (C) PCR analysis of pluripotent markers. Primer information is provided in Table 2. All scale bars indicate 200 µm. Please click here to view a larger version of this figure.
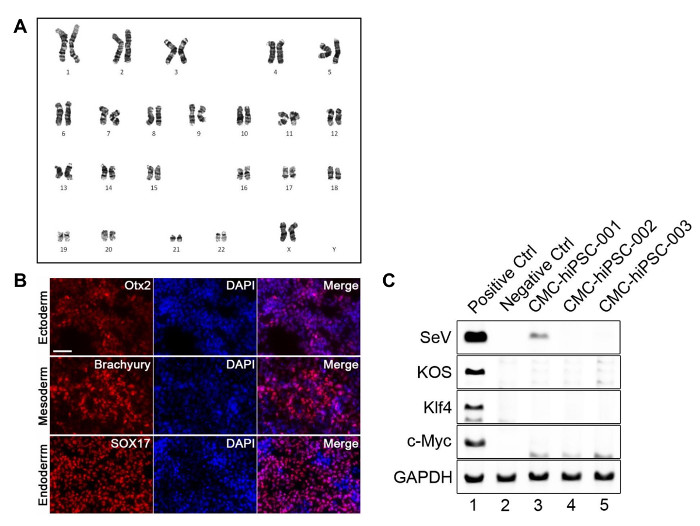
Figure 4: Further analysis of the generated iPSCs. (A) Normal karyogram of the iPSC. (B) Fluorescence image of the cells after three-germ layer differentiation. (C) PCR analysis of Sendai viral vectors. Non-transduced cells were used as negative control, and cells harvested a day after transduction were used as positive control. Primer information is provided in Table 2. All scale bars indicate 200 µm. Please click here to view a larger version of this figure.
| Antibody Name | Concentration |
| SSEA4 | 1:200 |
| Oct3/4 | 1:100 |
| TRA-1-60 | 1:200 |
| Sox2 | 1:100 |
| TRA-1-81 | 1:100 |
| Klf4 | 1:250 |
| Alexa Fluor 488 goat anti-mouse IgG (H+L) antibody | 1:400 |
| Alexa Fluor 594 goat anti-rabbit IgG (H+L) antibody | 1:400 |
Table 1. Antibody dilutions.
| Target Name | Direction | Primer Sequence | Size |
| OCT3/4 | Forward | ACC CCT GGT GCC GTG AA | 190 |
| Reverse | GGC TGA ATA CCT TCC CAA ATA | ||
| SOX2 | Forward | CAG CGC ATG GAC AGT TAC | 321 |
| Reverse | GGA GTG GGA GGA AGA GGT | ||
| NANOG | Forward | AAA GGC AAA CAA CCC ACT | 270 |
| Reverse | GCT ATT CTT CGG CCA GTT | ||
| LIN28 | Forward | GTT CGG CTT CCT GTC CAT | 122 |
| Reverse | CTG CCT CAC CCT CCT TCA | ||
| DPPB5 | Forward | CGG CTG CTG AAA GCC ATT TT | 215 |
| Reverse | AGT TTG AGC ATC CCT CGC TC | ||
| TDGF1 | Forward | TCC TTC TAC GGA CGG AAC TG | 140 |
| Reverse | AGA AAT GCC TGA GGA AAG CA | ||
| SeV | Forward | GGA TCA CTA GGT GAT ATC GAG C | 181 |
| Reverse | ACC AGA CAA GAG TTT AAG AGA TAT GTA TC | ||
| KOS | Forward | ATG CAC CGC TAC GAC GTG AGC GC | 528 |
| Reverse | ACC TTG ACA ATC CTG ATG TGG | ||
| Klf4 | Forward | TTC CTG CAT GCC AGA GGA GCC C | 410 |
| Reverse | AAT GTA TCG AAG GTG CTC AA |
Table 2. Primer information.
Discussion
Since embryonic stem cells (ESCs) showed several shortcomings, the need of an alternative tool was required. Therefore, the development of induced pluripotent stem cells (iPSCs) by Yamanaka came under the international spotlight. It has been almost a decade since Yamanaka discovered that pluripotency can be induced by adding only four genes into adult somatic cells. Since iPSCs are "induced" from mature somatic cells, they can evade ethical issues that had once been the concern relating to ESCs. Unlike ESCs, iPSCs can be generated from each individual. Therefore, they can be used in personalized medical research and other studies, such as drug screening, disease modeling, or regenerative medicines.
The first human iPSC was generated from dermal fibroblasts in 2007. Various groups successfully reprogrammed this cell type, but an invasive surgical procedure was required to obtain this primary cell. Therefore, it was not the ideal source for generating various disease iPSCs or designing regenerative medicine. An alternative and easily obtained cell types were needed, such as keratinocytes, urine monocytes, and blood cells. However, these cells are hard to expand, and some of them have a higher chance of contamination10.
In this study, we presented a protocol that can successfully generate iPSCs from whole blood cells such as PBMCs. Without any expansion process of a specific cell type, this protocol suggests a relatively simple method to generate iPSCs, even from a small amount of primary blood cells. Once the PBMCs were isolated from the blood, the cells were stabilized in blood cell media for 5 days. The stabilization step before transduction was critical in this protocol. The reprogramming efficiency was better after incubating the cells in blood cell media. This media was used for the expansion of CD34+ cells. However, when whole blood cells were maintained in this media for 5 days, the cell number was nearly identical with the first count. Using whole blood cells, it was hard to confirm if the CD34+ cells had been expanded. Nevertheless, the stabilization step itself seemed to be important for successful reprogramming.
After transduction, we serially plated the cells onto a vitronectin-coated plate by centrifugation. Originally, the reprogrammed cells sank to the bottom of the well after transduction. By boosting the cells with mechanical force or centrifugation, the transduced cells were able to attach and proliferate. However, since the protocol used whole blood cells, half of the attempted trials with different samples resulted in various types of morphologies when expanded. Therefore, isolation of pure iPSC colonies by colony picking was critical in this protocol. The cells expanded from the isolated colony showed all the characteristics of a pure iPSCs.
Despite other benefits, iPSCs have several hurdles to overcome. Since several Yamanaka factors are known oncogenes, there are concerns that iPSCs can develop into tumors in vivo. Therefore, it is important that the reprogrammed cells have no remaining exogenous gene expression by integration. In the early years after the development of iPSCs, viruses, such as retroviruses and lentiviruses, were used for reprogramming. The reprogramming rate was successfully high, yet these viruses required random integration into the cell genome. For this reason, several other methods have been developed. Viruses like Sendai virus are known to transduce the cells without integration, and other methods using small molecules and episomal vectors have been developed as well. In this study, we used Sendai virus for the reprogramming. The integration rate was relatively low compared to lentiviruses. We also confirmed that there were some remaining viral components in the generated iPSCs. One out of three trials resulted in integration, even after 15-20 passages. However, this integration was removable by subcloning the colonies derived from one single cell. In our experience, the density to obtain a healthy colony derived from a single cell was 1×104 cells per 100-mm dish. The colonies that resulted in a perfect circular form were picked and expanded for PCR re-confirmation of the remaining viral components. The colonies derived from non-integrated cells were maintained for further use. Once deleted, the cells maintained the non-integrated state.
In this study, we suggest a protocol for blood cell reprogramming. We added several steps, such as serial plating and centrifugation, to increase the reprogramming rate of the floating cells. This method was done with PBMCs and cord blood mononuclear cells (CBMCs). This protocol was used to generate homozygote iPSCs in GMP facilities in South Korea. Our group looks forward to the acceleration of the iPSC reprogramming process using our protocol.
Divulgazioni
The authors have nothing to disclose.
Acknowledgements
This work was supported by a grant from the Basic Science Research Program through the National Research Foundation of Korea (NRF), funded by the Ministry of Science, ICT, and Future Planning (2013R1A1A1076125).
Materials
| Plasticware | |||
| 100mm Dish | TPP | 93100 | |
| 6-well Plate | TPP | 92006 | |
| 50 mL Cornical Tube | SPL | 50050 | |
| 15 mL Cornical Tube | SPL | 50015 | |
| 10 mL Disposable Pipette | Falcon | 7551 | |
| 5 mL Disposable Pipette | Falcon | 7543 | |
| 12-well Plate | TPP | 92012 | |
| 24-well Plate | TPP | 92024 | |
| PBMC Isolation Materials | |||
| DPBS | Life Technologies | 14190-144 | |
| Ficoll | GE Healthcare | 17-1440-03 | |
| StemSpan | STEMCELL Technologies | 9805 | Blood cell media |
| CC110 | STEMCELL Technologies | 8697 | Blood cell media supplement (100x) |
| iPSC Generation and Culture Materials | |||
| CytoTune-iPSC Sendai Reprogramming Kit | Life Technologies | A16518 | |
| TeSR-E8 Media | STEMCELL Technologies | 5940 | iPSC media |
| Vitronectin | Life Technologies | A14700 | |
| ROCK Inhibitor | Sigma Aldrich | Y0503 | |
| TrypLE express (TrypLE) | Life Technologies | 12604-039 | |
| ReleSR | STEMCELL Technologies | 12604-039 | Colony detaching solution |
| Quality Control Materials | |||
| 18 mm Cover Glass | Superior | HSU-0111580 | |
| 4% Paraformaldyhyde | Tech & Innovation | BPP-9004 | |
| Triton X-100 | BIOSESANG | 9002-93-1 | |
| Bovine Serum Albumin | Vector Lab | SP-5050 | |
| Anti-SSEA4 Antibody | Millipore | MAB4304 | |
| Anti-Oct4 Antibody | Santa Cruz | SC9081 | |
| Anti-TRA-1-60 Antibody | Millipore | MAB4360 | |
| Anti-Sox2 Antibody | Biolegend | 630801 | |
| Anti-TRA-1-81 Antibody | Millipore | MAB4381 | |
| Anti-Klf4 Antibody | Abcam | ab151733 | |
| Alexa Fluor 488 goat anti-mouse IgG (H+L) antibody | Molecular Probe | A11029 | |
| Alexa Fluor 594 goat anti-rabbit IgG (H+L) antibody | Molecular Probe | A11037 | |
| DAPI | Molecular Probe | D1306 | |
| Prolong gold antifade reagent | Invitrogen | P36934 | |
| Slide Glass, Coated | Hyun Il Lab-Mate | HMA-S9914 | |
| Trizol | Invitrogen | 15596-018 | |
| Chloroform | Sigma Aldrich | 366919 | |
| Isoprypylalcohol | Millipore | 109634 | |
| Ethanol | Duksan | 64-17-5 | |
| RevertAid First Strand cDNA Synthesis kit | Thermo Scientfic | K1622 | |
| i-Taq DNA Polymerase | iNtRON BIOTECH | 25021 | |
| UltraPure 10X TBE Buffer | Life Technologies | 15581-044 | |
| loading star | Dyne Bio | A750 | |
| Agarose | Sigma-Aldrich | 9012-36-6 | |
| 1kb (+) DNA ladder marker | Enzynomics | DM003 | |
| Alkaline Phosphatase | Millipore | SCR004 | |
| Tris base | Fisher Scientific | BP152-1 | Rinse Buffer |
| Sodium Chloride | Duchefa Biochemie | S0520.1000 | Rinse Buffer |
| Tween-20 | BIOSESANG | T1027 | Rinse Buffer |
| Hydrochloric Acid | Duksan | 1129 | Rinse Buffer |
Riferimenti
- Serra, M., Brito, C., Correia, C., Alves, P. M. Process engineering of human pluripotent stem cells for clinical application. Trends Biotechnol. 30 (6), 350-359 (2012).
- Martin, G. R. Isolation of a pluripotent cell line from early mouse embryos cultured in medium conditioned by teratocarcinoma stem cells. Proc Natl Acad Sci U S A. 78 (12), 7634-7638 (1981).
- Takahashi, K., Yamanaka, S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell. 126 (4), 663-676 (2006).
- Takahashi, K., et al. Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell. 131 (5), 861-872 (2007).
- Chun, Y. S., Byun, K., Lee, B. Induced pluripotent stem cells and personalized medicine: current progress and future perspectives. Anat Cell Biol. 44 (4), 245-255 (2011).
- Seki, T., Fukuda, K. Methods of induced pluripotent stem cells for clinical application. World J Stem Cells. 7 (1), 116-125 (2015).
- Churko, J. M., Burridge, P. W., Wu, J. C. Generation of human iPSCs from human peripheral blood mononuclear cells using non-integrative Sendai virus in chemically defined conditions. Methods Mol Biol. 1036, 81-88 (2013).
- Loh, Y. H., et al. Reprogramming of T cells from human peripheral blood. Cell Stem Cell. 7 (1), 15-19 (2010).
- Ohmine, S., et al. Induced pluripotent stem cells from GMP-grade hematopoietic progenitor cells and mononuclear myeloid cells. Stem Cell Res Ther. 2 (6), (2011).
- Mae, S., et al. Monitoring and robust induction of nephrogenic intermediate mesoderm from human pluripotent stem cells. Nat Commun. 4, 1367 (2013).

