Corneal Donor Tissue Preparation for Endothelial Keratoplasty
Summary
Endothelial corneal transplantation is a surgical technique for treatment of posterior corneal diseases. Mechanical microkeratome dissection to prepare tissue results in thinner, more symmetric grafts with less endothelial cell loss and improved outcomes. Dissections can be performed at the eye bank prior to corneal transplantation surgery.
Abstract
Over the past ten years, corneal transplantation surgical techniques have undergone revolutionary changes1,2. Since its inception, traditional full thickness corneal transplantation has been the treatment to restore sight in those limited by corneal disease. Some disadvantages to this approach include a high degree of post-operative astigmatism, lack of predictable refractive outcome, and disturbance to the ocular surface. The development of Descemet’s stripping endothelial keratoplasty (DSEK), transplanting only the posterior corneal stroma, Descemet’s membrane, and endothelium, has dramatically changed treatment of corneal endothelial disease. DSEK is performed through a smaller incision; this technique avoids ‘open sky’ surgery with its risk of hemorrhage or expulsion, decreases the incidence of postoperative wound dehiscence, reduces unpredictable refractive outcomes, and may decrease the rate of transplant rejection3-6.
Initially, cornea donor posterior lamellar dissection for DSEK was performed manually1 resulting in variable graft thickness and damage to the delicate corneal endothelial tissue during tissue processing. Automated lamellar dissection (Descemet’s stripping automated endothelial keratoplasty, DSAEK) was developed to address these issues. Automated dissection utilizes the same technology as LASIK corneal flap creation with a mechanical microkeratome blade that helps to create uniform and thin tissue grafts for DSAEK surgery with minimal corneal endothelial cell loss in tissue processing.
Eye banks have been providing full thickness corneas for surgical transplantation for many years. In 2006, eye banks began to develop methodologies for supplying precut corneal tissue for endothelial keratoplasty. With the input of corneal surgeons, eye banks have developed thorough protocols to safely and effectively prepare posterior lamellar tissue for DSAEK surgery. This can be performed preoperatively at the eye bank. Research shows no significant difference in terms of the quality of the tissue7 or patient outcomes8,9 using eye bank precut tissue versus surgeon-prepared tissue for DSAEK surgery. For most corneal surgeons, the availability of precut DSAEK corneal tissue saves time and money10, and reduces the stress of performing the donor corneal dissection in the operating room. In part because of the ability of the eye banks to provide high quality posterior lamellar corneal in a timely manner, DSAEK has become the standard of care for surgical management of corneal endothelial disease.
The procedure that we are describing is the preparation of the posterior lamellar cornea at the eye bank for transplantation in DSAEK surgery (Figure 1).
Protocol
1. Setup: Aseptic Technique11
- Turn on Laminar Flow Hood (LFH).
- Turn on the Nitrogen gas control unit. Ensure that hose is connected between console unit and Nitrogen tank. Turn gas on. Gas setting should be set to 50-60 PSI on regulator tank. Turbine pressure on unit should read 3.3 to 3.4 Bars.
- Press Test button. Atmospheric pressure will read in the 700s and pumps 1 and 2 should be below 200. The unit will beep when testing is complete. Don mask with eye protection, as applicable, and cap. Wash hands and don non-sterile gloves. Place sterile kits inside LFH and open wraps to establish sterile field.
- Place one sterile medicine cup and one sterile plastic basin with sterile gauze next to the established sterile field. Pour sterile isopropyl alcohol into medicine cup. Wipe pachymetry probe with alcohol swab/pad and place probe, tip down, into medicine cup. The probe tip should soak in isopropyl alcohol for 10 minutes. After pachymetry probe has soaked for 10 minutes, rinse the probe tip with sterile water from the prefilled syringe to remove alcohol and place probe in the plastic basin.
- Using aseptic technique, open and drop sterile items (blade, sterile gloves, and corneal viewing chambers) onto sterile field unless already part of the pre-made pack.
- Obtain corneal tissue in preservation media and place inside LFH (Figure 2).
- Open vial(s) and dispose of the lid(s) into an appropriate biohazard receptacle. Discard non-sterile gloves.
- Don sterile gloves. Place pre-packed plastic basin to the side of the field where pachymeter is located. Connect infusion line to stopcock and place spike end of infusion line outside of hood securing the line in such a way as to prevent the line outside of the hood from reentering the hood and touching the sterile field.
- Perform corneal tissue transfer. Gently pour the tissue and medium, in a single motion, from the existing vial to a sterile viewing chamber. Be sure to keep the endothelial side up. Place the cap on the chamber. Keep chambers containing tissue and media on sterile field. Remove vial(s) from LFH. Remove and discard sterile gloves.
- Spike balanced salt solution (BSS) bottle with infusion line. Hang bottle of sterile BSS approximately four feet from working area surface.
- Open two pairs of sterile gloves and sterile gown with towel.
- Perform six minute surgical scrub and dry hands.
- Put on sterile gown, then both pairs of sterile gloves.
- Open instrument boxes and place the contents onto the sterile field.
- Dispense 10-20 cc of BSS solution into metal basin or medicine cup. Fill sterile pipette with BSS solution. Connect stopcock and infusion line to infusion port of the anterior chamber and flush with BSS so that a small amount is visible on top of the piston.
- Position artificial chamber in LFH on top of gauze. Lower piston by turning graft tightening ring counterclockwise.
2. Procedure
- Using forceps, gently grasp cornea by scleral rim. Open stopcock to flush system with BSS while carefully centering cornea on top of the piston with the endothelial side down. If bubbles are visible beneath the cornea, continue infusing with BSS and slightly moving the cornea to remove them. Discontinue infusion once air bubbles are removed. Ensure that the cornea is centered on the piston (Figure 3a).
- Position anterior chamber cover on base locking ring so that the tabs of the cover fit into the open spaces on the base. Lock cover into base by turning cover clockwise 15°. Raise piston up and tighten completely (Figure 3b).
- With a sterile gloved finger, touch top of cornea to ensure that there is sufficient pressure to perform procedure.
- Check pachymetry by placing probe on surface of cornea to obtain thickness reading (Figure 4). The standard deviation must be less than 10. If not, retake measurement. With the sterile gloved hand that was not used to perform the pachymetry, pass the turbine hose to the hand that performed pachymetry and screw the turbine hose into the control unit. Have the assisting technician record pachymetry reading.
- Remove contaminated gloves.
- Using sterile marking pen, draw a 4mm line from limbus toward center of the cornea (or do not mark if surgeon prefers no marking). Use pipette to place five drops of BSS on top of the cornea.
- Unless specific instructions are provided by the surgeon, the 300 μm cutting head will be used if the pre-cut pachymetry measurement is less than 600 μm. If over 600 μm, the 350 μm cutting head will be used.
- With thread facing toward you and number facing up, load blade into right side of microkeratome head, pointed end first, avoiding contact with the blade.
- Holding head at each side, screw head onto turbine. Tighten the artificial chamber with fingers.
- Screw turbine onto turbine hose.
- Test the blade oscillation by pressing the vacuum pedal once, submerging the cutting head in the sterile water and pulse the turbine for 5 seconds.
- Retighten piston.
- Place microkeratome onto the base with mounting post and position at five o’clock. Press and hold turbine pedal to oscillate blade (Figure 5a).
- Using index finger and thumb, hold microkeratome midway between the base and the top of the turbine. Turn wrist to make a smooth, even cut through and across the cornea. Release turbine pedal and lift microkeratome straight off unit. Press vacuum pedal to turn off vacuum (Figure 5b).
- Don a sterile glove and recheck pachymetry reading after corneal cap is removed by placing probe on corneal surface to obtain second thickness reading being mindful that the tissue is very thin and easily damaged. Remove contaminated glove. Have assisting technician record second pachymetry reading.
- Using sterile marking pen, place a mark if requested by surgeon, on the mid-peripheral edge of the residual stromal bed in the artificial chamber. Place a few drops of sterile BSS onto residual stromal bed.
- Remove the anterior cornea cap from the microkeratome (Figure 6) and replace it onto the cornea before removing cornea from artificial anterior chamber. Cap should be centered on cornea using peripheral marking to align the cap correctly if applicable. Use swab spear to gently reposition the cap onto the cornea. Use fresh spear to absorb any BSS underneath anterior cap.
- Open stopcock, turn chamber upside-down and lower piston slow enough to prevent cornea from deforming. Unlock base and allow pressure from the BSS flow to push the artificial chamber cup from the base. With forceps, gently pull at the corneal rim at 9, 12 and 3 o’clock positions to loosen it from the cup. Once loosened, use forceps at the 12 o’clock position to remove cornea. Place the cornea in the viewing chamber, endothelial side up (Figure 7). Place the lid on the viewing chamber. Remove sterile glove.
- Tighten viewing chamber lid.
- Perform post-cut slit lamp evaluation and specular microscopy of cornea and record findings.
- Place chamber(s) in appropriate section of refrigerator.
- Package for transport to surgeon (Figure 8).
3. Representative Results
Proper mechanical microkeratome dissection of the donor cornea results in smooth, uniform lamellar corneal donor tissue. This is shown by an optical coherence tomography (OCT) image of the cornea in cross section (Figure 9). The final posterior corneal tissue should be of adequate thickness as measured by pachymetry. Over the past 6 months at the Michigan Eye Bank, the mean pre-processing corneal thickness was 558 microns, and post-processing thickness of the posterior corneal tissue was 158 microns. Eighty-seven percent of microkeratome-dissected donor tissue measured between 100-200 microns, 10.9% measured >200 microns, and 2.1% measured <100 microns.
The posterior corneal tissue must retain high endothelial cell density (ECD) to provide improved endothelial function to the transplant recipient. Specular microscopy is used to measure ECD. In the past 6 months, all of the corneal tissue deemed eligible for endothelial keratoplasty from the Michigan Eye Bank had an ECD of >2200 cells/mm2. Ninety-nine percent of the precut DSAEK tissue had a post-processing ECD >2400 cells/mm2, and 19% had an ECD > 3000 cells/mm2. The mean change in pre- to post-processing ECD was negligible at 1.2% (p=0.0003, paired two-tailed t-test). Complications that can occur during the procedure include loss of pressure, asymmetric dissection, and significant tissue indentation (resulting in corneal endothelial cell loss). Improper dissection can also result in tissue perforation.
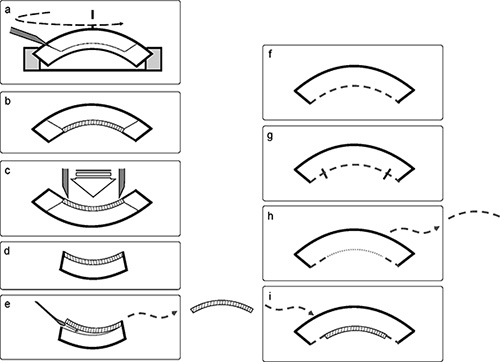
Figure 1. Overall Scheme of Corneal Tissue Preparation for Endothelial Keratoplasty Figures 1a to 1e are cross-section representations of the donor cornea preparation. Figures 1f to 1i are cross-section representations of the transplant recipient’s cornea during DSAEK surgery.
- The donor cornea is mounted onto an artificial anterior chamber and dissected with the microkeratome head.
- After tissue dissection, the two lamellae are separate but the anterior lamella (cap) is positioned back onto the remained corneal bed for transportation to the surgeon.
- In the operating room, the surgeon uses a trephine to cut the central corneal tissue vertically through both anterior and posterior lamella.
- After trephine cutting, the peripheral donor cornea is removed from the field.
- The posterior lamella is gently removed from the anterior lamella with a spatula. The donor posterior lamella (DSAEK tissue) replaces the diseased portion of the recipient cornea (1i).
- The patient has a diseased posterior cornea to be removed.
- The diseased posterior cornea is scored with an intraocular instrument (reverse Sinsky hook) in a large diameter circle.
- After scoring the diseased cornea, the posterior corneal membrane is removed.
- The donor posterior lamella (DSAEK tissue) is placed in the recipient’s eye.
Figure 2. Corneal Tissue in Media. Corneal tissue is in preservation media after harvesting from donor.
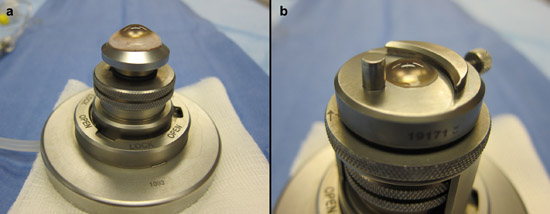
Figure 3. Corneal Tissue on Artificial Anterior Chamber.
- Corneal tissue is mounted onto the artificial anterior chamber prior base locking ring or tissue dissection.
- Corneal tissue is mounted onto artificial anterior chamber with base locking ring sealed over the tissue.

Figure 4. Corneal Tissue Thickness Check. The corneal thickness is checked using ultrasound pachymetry probe on surface of cornea.
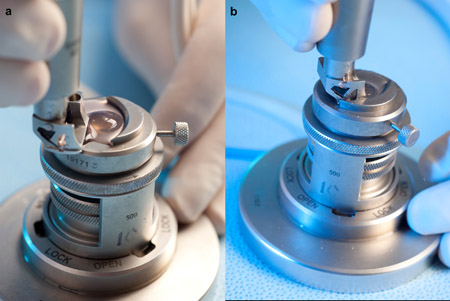
Figure 5. Corneal Tissue Dissection.
- Microkeratome blade is placed on the base with mounting post and position at five o’clock.
- Microkeratome is passed through cornea to make the lamellar dissection.

Figure 6. Anterior Cap of Cornea after Dissection. The anterior cornea cap is free after microkeratome dissection is complete.

Figure 7. Dissected Cornea in Viewing Chamber. After dissection is completed, the cornea is returned to the viewing chamber for transportation.

Figure 8. Cornea in Packaging for Transportation. The cornea in the viewing chamber is then securely packaged for transportation to the surgeon.
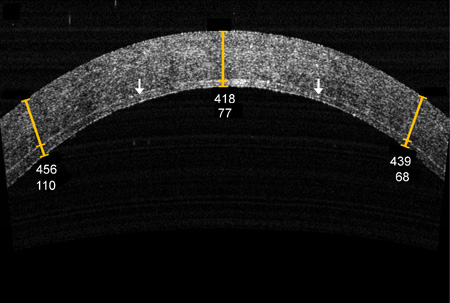
Figure 9. OCT Appearance of Cornea. The OCT of the final dissected cornea (in cross-section) shows that the cornea is split into two halves. The interface is more intensely reflective than the surrounding tissue as indicated by the arrow.
Discussion
The inner-most layer of the cornea, the endothelium, maintains the optical clarity of the cornea by maintaining corneal dehydration. Numerous disease states specifically affect the health and viability of the corneal endothelium including dystrophies, infections, inflammatory processes, and degenerations. Until recently, corneal transplantation to replace diseased corneal endothelium required full thickness transplantation of the cornea. In the past decade, targeted replacement of the posterior cornea by partial thickness corneal transplantation, such as DSAEK surgery, has been able to achieve the same goal with a shorter recovery time. Regardless of technique, transplanted tissues must retain a healthy corneal endothelium to maintain optical clarity in the transplanted cornea; as a result, all tissue processing techniques have additional steps to protect the corneal endothelium.
Automated microkeratome dissection is currently the standard for corneal tissue preparation for endothelial keratoplasty. Use of the microkeratome was shown to decrease donor tissue perforation and speed visual recovery as compared to manual dissection 5. When DSAEK was initially introduced, some surgeons purchased microkeratome equipment and performed donor lamellar dissection in the operating room at the start of surgery. If tissue preparation failed, the surgery would have to be cancelled causing inconvenience and expense to the patient and the surgeon. In 2006 eye banks began performing microkeratome dissection “off site” under controlled conditions in the eye bank laboratory a day prior to surgery 12. If tissue preparation fails in this setting, there is time to perform another dissection with fresh tissue.
Microkeratome dissection of donor posterior lamellar corneal tissue requires gentle and precise technique to minimize complications. The cornea must be placed gently on the artificial anterior chamber (AAC) to avoid any damage to the delicate endothelial cells. Once the cornea is mounted and aligned on the AAC, the locking ring must be positioned and adjusted for a tight seal to maintain high pressure within the chamber and decrease the chances of tissue collapse during the microkeratome dissection. To ensure uniform dissection, the microkeratome head should be rotated in a constant, smooth manner. After dissection, the tissue must again be handled carefully to minimize endothelial cell damage. Further, it is critical to confirm that the lamellar cut is centered and complete in order to ensure that the posterior lamella will be suitable for use in surgery 13.
Corneal donor perforation is a dreaded complication of this procedure; it becomes less frequent with experience. If repeated perforations occur during microkeratome passes, it is important to check multiple steps in the procedure. The cornea needs to be properly mounted and aligned on the AAC. A tight seal and high pressure should be obtained prior to microkeratome pass and maintained throughout the procedure. On occasion, residual conjunctiva exists on the sclera rim and needs to be dissected off prior to mounting. The microkeratome blade should be sharp and without notches. The correct microkeratome head thickness should be selected based on the estimated corneal thickness. The microkeratome head must be oscillating properly prior to the pass. With further problems with this technique, consult the microkeratome provider to verify that all equipment is working properly.
Even when performed perfectly, there are some limitations to this technique. Microkeratome heads are available to cut corneal tissue at various thicknesses; however, the relationship of microkeratome head to final tissue thickness is imprecise with the same head providing a wide range of final tissue thicknesses 7. In addition, a significant learning curve exists and complications in preparation are more frequent for new users. Performing the lamellar dissection in the eye bank setting allows trained technicians who perform this procedure many times per day to optimize their technique, thereby minimizing complications due to inexperience.
Modifications of the technique for microkeratome-assisted corneal dissection for endothelial keratoplasty exist. Some prefer to use viscoelastic material or corneal storage media rather than balanced salt solution beneath the corneal button on the artificial anterior chamber with the intent of providing increased protection to the corneal endothelium. There are also variations in the method for determining the location in which the microkeratome incision should be initiated. Different eye banks and different corneal surgeons may have particular preferences as to how the cornea is marked for identification of the anterior corneal cap or posterior lamellar orientation. It should be noted that manufacturers make similar equipment to that used in this protocol. The particular manufacturer’s instructions should be followed with whichever equipment is used.
Dependable eye bank preparation of dissected corneal tissue for DSAEK surgery has been beneficial for the widespread acceptance of this relatively new surgical technique. Once surgeons became confident in eye banks performing the “first step” in corneal transplantation – namely tissue preparation, many practical limitations to DSAEK were alleviated. Eye banks have been able to reliably keep up with the demand for processed tissue with safe, effective, and timely supply of donor tissue. High quality DSAEK tissue can now be ordered in advance and operating room time and tissue preparation complications have decreased 9, 14-15.
This protocol describes the preparation of DSAEK grafts from the perspective of eye bank processing of corneal donor tissue; however, this technique is directly applicable to surgeons interested in preparing their own lamellar corneal donor tissue as well as those interested in performing laboratory-based or clinical studies on lamellar corneal transplantation.
Future directions for corneal lamellar preparation include use of the femtosecond laser for tissue processing, creation of “ultra-thin” DSAEK corneal tissue, or preparation of corneal endothelial scrolls for Descemet’s membrane endothelial keratoplasty (DMEK) surgery. Endothelial keratoplasty is a surgical field in evolution and the symbiotic relationship between the eye bank and corneal surgeon will continue to change as surgical techniques are optimized.
Disclosures
The authors have nothing to disclose.
Acknowledgements
Supported in part by NIH/NEI EY017885 (RMS).
Materials
| Name of the Equipment | Company | Catalogue number |
| Microkeratome | Moria | 1021174 |
| Artificial Anterior Chamber base | Moria | 19161-562 |
| Artificial Anterior Chamber cap | Moria | 19172-220 |
| Microkeratome Head 300 | Moria | O304 |
| Microkeratome Head 350 | Moria | N791 |
| Console | Moria | 19360-3482 |
References
- Melles, G. R., et al. A surgical technique for posterior lamellar keratoplasty. Cornea. 17, 618-626 (1998).
- Melles, G. R., et al. Preliminary clinical results of posterior lamellar keratoplasty through a sclerocorneal pocket incision. Ophthal. 107, 1850-1856 (2000).
- Terry, M. A., Ousley, P. J. Replacing the endothelium without corneal surface incisions or sutures: the first United States clinical series using the deep lamellar endothelial keratoplasty procedure. Ophthal. 110, 755-764 (2003).
- Price, F. W., Price, M. O. Descemet’s stripping with endothelial keratoplasty in 50 eyes: a refractive neutral corneal transplant. J. Refract Surg. 21, 339-345 (2005).
- Price, M. O., Price, F. W. Descemet’s stripping with endothelial keratoplasty: comparative outcomes with microkeratome-dissected and manually dissected donor tissue. Ophthal. 113, 1936-1942 (2006).
- Bahar, I., et al. Retrospective contralateral study comparing descemet stripping automated endothelial keratoplasty with penetrating keratoplasty. Cornea. 28, 485-488 (2009).
- Rose, L., Briceno, C. A., Stark, W. J., Gloria, D. G., Jun, A. S. Assessment of Eye Bank-Prepared Posterior Lamellar Corneal Tissue for Endothelial Keratoplasty. Ophthal. 115, 279-286 (2008).
- Price, M. O., Baig, K. M., Brubaker, J. W., et al. prospective comparison of precut versus surgeon-dissected grafts for Descemet stripping automated endothelial keratoplasty. Am. J. Ophthalmol. 146, 36-41 (2008).
- Chen, E. S., Terry, M. A., Shamie, N., Hoar, K. L., Friend, D. J. Precut tissue in Descemet’s stripping automated endothelial keratoplasty donor characteristics and early postoperative complications. Ophthalmology. 115, 497-502 (2008).
- Terry, M. A. Endothelial Keratoplasty: A Comparision of Complication Rates and Endothelial Survival between Precut Tissue and Surgeon-cut Tissue by a Single DSAEK Surgeon. Trans. Am. Ophthalmol. Soc. 107, 184-193 (2009).
- . . Reference document E1.710 Corneal Tissue Preparation for Lamellar Procedures. , 1-5 (2010).
- . . Eye Banking Statistical Report. , 1-5 (2009).
- Glasser, D. B. Tissue complications during endothelial keratoplasty. Cornea. 29, 1428-1429 (2010).
- Kelliher, C., Engler, C., Speck, C., et al. A comprehensive analysis of eye bank-prepared posterior lamellar corneal tissue for use in endothelial keratoplasty. Cornea. 28, 966-970 (2009).
- Price, F. W. Precut tissue for Descemet stripping automated endothelial keratoplasty. Cornea. 27, 630-631 (2008).

