Handwriting Analysis Indicates Spontaneous Dyskinesias in Neuroleptic Naïve Adolescents at High Risk for Psychosis
Summary
Handwriting analysis software significantly improves upon existing instruments measuring movement disorders. Individuals at risk for psychosis and healthy controls completed handwriting tasks to test for dyskinesia. Results suggest that youth at risk for psychosis exhibit dyskinesia and that handwriting analysis could significantly contribute to wider dissemination of early identification efforts
Abstract
Growing evidence suggests that movement abnormalities are a core feature of psychosis. One marker of movement abnormality, dyskinesia, is a result of impaired neuromodulation of dopamine in fronto-striatal pathways. The traditional methods for identifying movement abnormalities include observer-based reports and force stability gauges. The drawbacks of these methods are long training times for raters, experimenter bias, large site differences in instrumental apparatus, and suboptimal reliability. Taking these drawbacks into account has guided the development of better standardized and more efficient procedures to examine movement abnormalities through handwriting analysis software and tablet. Individuals at risk for psychosis showed significantly more dysfluent pen movements (a proximal measure for dyskinesia) in a handwriting task. Handwriting kinematics offers a great advance over previous methods of assessing dyskinesia, which could clearly be beneficial for understanding the etiology of psychosis.
Introduction
The period preceding the onset of psychosis is of clinical and research interest as it may shed light on formal psychosis (prior to when a number of third variable confounds such as medication obfuscate our understanding), and also serves as a viable point of intervention (roughly ⅓ of youth showing a prodromal syndrome go on to develop schizophrenia in a 2 year period, and several studies suggest that psychosocial, cognitive training, and pharmacological interventions may ameliorate the course of illness)1. This prodromal period is marked by attenuated positive symptoms (perceptual abnormalities, suspiciousness, feelings of grandiosity, or unusual thoughts) and a decline in functioning2. Individuals who report a moderate degree of positive symptoms during a structured clinical interview, and/or a decline in functioning accompanying the presence of schizotypal personality disorder and/or a family history of schizophrenia are considered to have a prodromal or ultra high-risk (UHR) syndrome1-3. Current etiological conceptions of psychosis suggest that it is a neurodevelopmental disorder that affects an individual during late adolescence or early adulthood4. Constitutional factors such as genetics and prenatal insults result in vulnerability for psychosis4. Movement abnormalities are of keen interest to this model, as the same mechanisms believed to be contributing to psychotic symptoms are also responsible for governing the motor system5. Researchers argue that by understanding movement behavior prior to the onset of schizophrenia, we may improve our ability to predict, understand, and intervene in the development of schizophrenia6.
It is well known that individuals who later go on to develop schizophrenia often show subtle movement abnormalities prior to the onset of illness7,8. Walker and colleagues collected videotapes of patients with schizophrenia during childhood and rated the videos for movement abnormalities, showing that movement abnormalities are present long before the onset of illness and are indicative of a neurological constitutional vulnerability9,10. Research suggests that the basal ganglia may be implicated in this neurological constitutional vulnerability, as UHR individuals show impaired neural development and neurocognitive deficits related to basal ganglia function8,11. Additionally, Mittal and colleagues have used observer ratings to show that movement abnormalities, closely linked to basal ganglia function, could successfully classify UHR individuals likely to convert to psychosis8,12. Another at risk group, nonclinical psychosis individuals who report having a psychotic-like experience at least once a year, show dyskinesia during a finger force stability task5,13,14. These findings provide strong evidence for the idea that movement abnormalities may be a core feature of risk of psychosis. Clearly, research that can improve detection and understanding of movement abnormalities is crucial for the understanding of the etiology of psychosis and for preventive efforts.
Efforts to understand medication side-effects that affect dopamine regulation in schizophrenia and Parkinson's patients have guided technological improvements, such as the development of computerized tablets for handwriting analysis, in measuring movement abnormalitie15-17. Antipsychotic medication may lead to the development of tardive dyskinesia, characterized by slow involuntary repetitive movements18. Nicotine use has also been shown to affect dopamine regulation and handwriting kinematics19-21. For example, Tucha and Lange showed that pen movement fluency improved during a computerized handwriting task when healthy participants were given chewing gum containing nicotine22. During assessment, participants generally write in a western cursive handwriting with larger and smaller vertical strokes. Western cursive handwriting is optimal for examining pen movement smoothness because of the predominance of vertical strokes that require complex coordination of muscles to perform well23. Dysfluent pen movements result when the muscles that coordinate the movement receive disregulated signals from the basal ganglia15,16.
The software segments and analyzes pen movements per stroke and extracts a variable that is thought to be a proximal measure of dyskinesia, called average normalized jerk15-17. Jerk is defined as the change in acceleration over time per stroke23. Because of the different lengths in vertical strokes in most western style handwritings, jerk is normalized across strokes. Within each stroke, dysfluent pen movements are characterized by a greater number of acceleration peaks over a given distance. Thus, dysfluent pen movements are characterized by a lack of smoothness, a greater number of acceleration peaks, and a larger value of jerk.
The improvement of measures used to rate movement abnormalities in UHR youth is critical for improving our etiological conceptions of the illness and our understanding of movement disorders in general. In that effort to understand movement disorders in those at risk for psychosis, we examined handwriting kinematics from 36 neuroleptic naïve research participants using handwriting analysis software. Despite its wide use in investigating dyskinesia in Parkinson's and schizophrenia patients, this is surprisingly the first study to report on handwriting kinematics in an ultra-high-risk group for psychosis. We hypothesized that the UHR individuals would show more dysfluent pen movements, characterized by a larger value of jerk, when asked to write on a tablet computer than a group of healthy controls.
Protocol
1. Participants
- Provide approval for the protocol and informed consent procedures from the University Institutional Review Board.
- Recruit adolescent and young adult UHR participants by using Craigslist (i.e. local classified advertisements on the internet), email postings, newspaper ads, and community professional referrals.
- Recruit healthy control participants by craigslist, flyers and newspaper announcements.
- Advertise that the study looks at healthy development for volunteers with no family history of psychosis and no psychiatric symptoms.
- Exclude healthy controls based on the presence of any category of Axis I disorder or a psychotic disorder in a 1st degree relative.
Note: A psychotic disorder in a first degree relative is intended as exclusion criteria for healthy controls because of the familial or genetic risk of psychosis1.
- Exclude all participants based on criteria consisting of a history of head injury, the presence of a neurological disorder, substance dependence, or a history of taking neuroleptic medication.
- Exclude UHR participants based on the presence of an Axis I psychotic disorder (e.g. schizophrenia, schizoaffective disorder, schizophreniform).
2. Clinical Interviews
- Train interviewers to administer the Structured Interview for Prodromal Syndromes (SIPS) to diagnose a prodromal syndrome and the Structured Clinical Interview for Axis-I DSM IV Disorders (SCID) over a 2 month period.
- Establish inter-rater reliabilities on clinical interviews to exceed the minimum study criterion of Kappa ≥80.
- Define criteria for a prodromal or high-risk syndrome by moderate levels of positive symptoms and/or a decline in global functioning accompanying the presence of schizotypal personality disorder and/or a family history of schizophrenia.
- Compute a total sum score for each category as an indicator of the respective dimensions of symptomatology.
Note: The SIPS gauges several distinct categories of prodromal symptom domains including positive, negative, and disorganized dimensions. - Administer the Structured Clinical Interview for Axis-I DSM-IV Disorders (SCID) to rule out a psychotic disorder diagnosis.
Note: This measure has been demonstrated to have excellent inter-rater reliability in adolescent populations and has been used in several previous studies focusing on adolescent populations with schizophrenia spectrum disorders. - Assess the participant's nicotine usage during the past month. Rate tobacco usage on a 0-5 scale with 0 = abstinent and 5 = 20+ cigarettes per day.
3. Handwriting Task
- Run Neuroscript MovAlyzeR software with a tablet computer and a noninking pen.
- Create an example of LLeeLLee on a notecard (see Figure 1).
Note: The software and stimulus are described previously and have been shown to be valid tools for detecting movement abnormalities in schizophrenia patients and Parkinson's patients15-17.
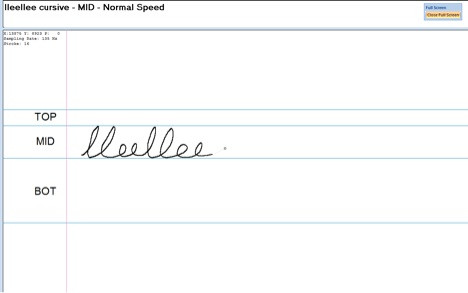
Figure 1. Example of the test condition. Participants are instructed to write the word LLeeLLee in cursive in the MID section. It is helpful to have an example such as this to show the participant so that they understand the instructions.
- Leave the example notecard visible to the participant throughout the experiment. Note: The notecard will help the participant understand the experiment.
- Orient tablet into landscape mode to provide a writing space of 18 cm x 28 cm with a resolution of 1,280 x 800 pixels.
- Allow participants to position computer screen into a comfortable writing position.
- Set the sampling rate in the software to the measured sampling rate (e.g. 100-200 Hz).
- Instruct participant to write the word LLeeLLee in cursive in the 2 cm guidelines with the dominant hand.
Note: The condition is programmed to divide the writing surface into 4 regions. There are horizontal lines measuring 1 cm, 2 cm, and 4 cm. The 1 cm region is marked TOP. The 2 cm region is marked MID, and the 4 cm region is marked BOT. Participants will use the MID section for all three trials. - Keep instructions visible during each trial.
Note: The instructions for the task are displayed at the top of the monitor and are as follows: "DH lleellee MID Normal Speed". The participant should be told prior to starting the program that these instructions mean to write the word LLeeLLee in the MID section with the dominant hand and at a comfortable handwriting speed. Also note that the software will redo trial automatically if the participant makes an error while writing.
4. Processing Trials
- Process trials using a Fast Fourier Transform Low Pass 12 Hz filter, with a 1.75 Sharpness, 1 Lump decimates sample, and 1 Up-sample Factor. Remove trailing pen lift and rotate to horizontal baseline. Set additional counter clockwise rotation when segmenting at vertical velocity to zero radians.
Note: The handwriting analysis software will automatically incorporate these processing steps if they are selected within the program options. - Summarize the absolute values of target variables LLeeLLee at two centimeters for Average Normalized Jerk (ANJ) per Trial. Collapse across trial and stroke.
Note: The ANJ is a measure of movement dysfluency. Higher ANJ indicates greater dysfluency (See Figure 2). The dysfluency measure is based on the vertical component of the jerk (in cm/sec3), i.e. the 3rd time derivative of vertical position of the pen tip. Dysfluencies are caused by sudden changes in force. The 2nd time derivative, which is acceleration, is proportional to the net muscle force (if friction is neglected). Therefore, the 3rd time derivative is proportional to the force changes. To obtain an overall measure of dysfluency the vertical jerk is squared and integrated across the duration of a stroke (unit is cm2/sec5). To make this measure independent upon the duration and the vertical size of the stroke, multiply the integral by the 5th power of stroke duration (unit is sec5) and the inverse of the vertical size squared (unit is 1/cm2). The result is therefore unitless. Normalized jerk describes the shape of the acceleration curve irrespective of width and height. Take the square root of the end result to make ANJ proportional with jerk
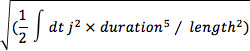
The ANJ of a trial is defined by the average of the normalized jerk estimates across all up and down strokes of a trial 23.
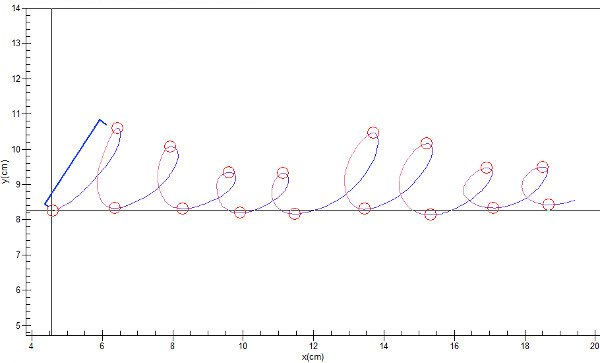
Figure 2. Trial from a control participant. Each trial is divided into 16 strokes. The segmentation of stroke for analysis of average normalize jerk is illustrated with the first pen stroke (in blue). A blue bracket outlines the stroke, and circles denote the start and stop of the stroke segment. Click here to view larger figure.
5. Statistical Analysis
- Employ independent two tailed t-tests and chi-square tests to examine differences between groups in continuous and categorical demographic variables, respectfully. If necessary, adjust for inequalities of variance by Levene's test.
- Employ an analysis of covariance (ANCOVA) controlling for nicotine use and gender with group (UHR and Control) as the independent variable and ANJ collapsed across trial.
Representative Results
There were no significant differences between groups on demographic characteristics including age, years of education, or parental education (see Table 1 for a demographic breakdown of the participants). Chi Square tests revealed significant differences between groups on gender χ2 (1, N = 36) = 5.46, p≤0.05, with more males in the UHR group and more females in the control group. There was a significant group differences in tobacco usage frequency, t(22.9) = 2.15, p≤0.05, showing that UHR participants smoke more than controls. UHR participants were rated significantly higher than controls on all SIPS symptom domains, including positive (t(37) = 10.9, p ≤ 0.001), negative (t(37)= 6.9, p≤0.001), disorganized (t(37) = 6.7, p≤0.001), and general (t(37) = 5.7, p≤0.001).
| UHR | Control | Total | p ≤ | |
| Age | ||||
| Mean (SD) | 18.43 (1.91) | 17.45 (2.43) | 17.97 (2.19) | 0.3 |
| Gender | ||||
| Male | 13 | 6 | 19 | |
| Female | 5 | 12 | 17 | |
| Total | 18 | 18 | 36 | |
| Race and Ethnicity | ||||
| Asian | 0 | 3 | 2 | |
| Black | 1 | 0 | 1 | |
| Hispanic | 2 | 5 | 7 | |
| White | 15 | 10 | 25 | |
| Education (years) | ||||
| Mean (SD) | 12.39 (1.85) | 11.67 (2.25) | 12.03 (2.06) | 0.3 |
| Parent Education | ||||
| Mean (SD) | 16.20 (1.57) | 15.94 (2.42) | 16.09 (2.01) | 1 |
| SIPS Positive | ||||
| Mean (SD) | 11.619 (4.33) | 0.78 (1.31) | 6.62 (6.37) | 0.001 |
| SIPS Negative | ||||
| Mean (SD) | 11.62 (6.83) | 1 (1.53) | 6.72 (7.37) | 0.001 |
| SIPS Disorganized | ||||
| Mean (SD) | 5.9 (3.56) | 0.45 (0.98) | 3.38 (3.84) | 0.001 |
| SIPS General | ||||
| Mean (SD) | 6.62 (4.26) | 0.78 (1.7) | 3.92 (4.42) | 0.001 |
| Average Normalized Jerk | ||||
| Mean (SD) | 43.92 (25.55) | 30.99 (17.29) | 36.47 (22.03) | 0.05 |
Table 1. Demographic Characteristics and Results. Demographics of the sample showed no differences in variables for age and parent education. There was a significant difference in gender between groups with more males in the ultra-high-risk group and more females in the control group.
Because tobacco use mediates the regulation of dopamine in areas responsible for movement 21,24, we examined group differences by treating frequency of tobacco use as a covariate. As gender was significantly different between groups, male/female was also treated as a statistical covariate. The groups showed a significant difference for average normalized jerk F(3, 32) = 3.98, p = 0.02, d = 0.59. These results suggest that the UHR group showed a larger value of ANJ, indicating more dysfluent pen movements (See Figure 3), and that the handwriting analysis may have detected the presence of dyskinesia in the high-risk participants.
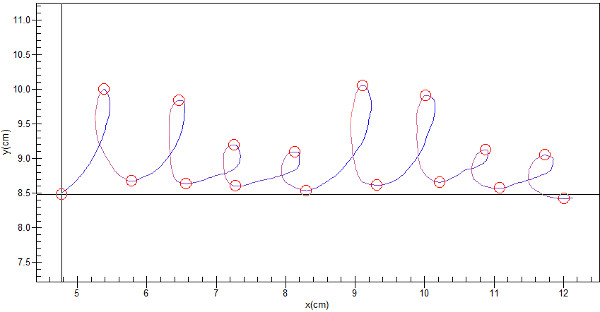
Figure 3. A UHR participant's dysfluent pen movement. Compared to a healthy control (see Figure 2), there is a significant increase in average normalized jerk for UHR participants. Click here to view larger figure.
Discussion
This study found significant evidence of more dysfluent pen movements and the presence of dyskinesia in an UHR sample using a handwriting analysis program to examine movement abnormalities.
Traditionally, observer based rating scales have been utilized to measure movement abnormalities in order to monitor drug side effects15-17. However, the observer ratings suffer from significant drawbacks including long training times for raters, experimenter error, and suboptimal reliability16. Other sources of measurement, use outdated software or computer hardware and while effective, are not practical for wide spread dissemination or study-by-study comparison because of large site-based heterogeneity in apparatuses and thresholds. This study improves upon previous work because it utilizes an easily available and reliable method of analyzing movement without requiring intensive training, set up time, or hard to find hardware25. It is also notable that instrumentally based assessments detect those patients who would be positive on a clinician rater scale (e.g. the Abnormal Involuntary Movement Scale; AIMS)20,26 in addition to sensing subtle/sub-threshold movement abnormalities in an additional proportion of patients that would be missed by the eye27. Thus, the use of a standardized instrumental approach, such as a computerized tablet for handwriting analysis, stands to be highly useful for an at-risk population that is only in the process of developing the significant movement abnormalities seen in psychosis.
The present findings support the body of work that indicates movement abnormalities are a core feature of risk for psychosis. Movement abnormalities and prodromal symptoms are strongly associated with disregulation of dopamine in the fronto-striatal circuit28. Handwriting kinematics has provided an incredible amount of research to support understanding of the role of dopamine in movement disorders and in psychosis. Previous studies to employ similar handwriting paradigms have found that Parkinson's patients treated with dopamine agonists show more dysfluent pen movements17,23,29 . Additionally, schizophrenia patients never treated with neuroleptics show higher ANJ than healthy control patients15. Taken together, the results show promise towards a method of analyzing the effects of disregulated dopamine and could be a strong aid in preventive efforts for those at risk for psychosis.
There are several limitations to this study that should be addressed in future studies. The sample size used in the previous study is similar to those comparing schizophrenia patients and healthy controls, however; clearly a larger sample size is needed to examine the present hypotheses. While the computerized tablet offers a number of benefits to measuring movement abnormalities, comparing observer based rating scales of movement abnormalities to the ANJ values observed in UHR individuals could strengthen this area of research. We included only one condition to analyze writing smoothness. Future studies utilizing a battery of other writing conditions stand to inform our understanding of movement abnormalities in UHR individuals. While the study sought to make the writing tasks as natural as possible for the participant, including conditions that more resemble the natural size of everyday handwriting tasks or do not require copying the stimulus from the notecard may help in generalizing results of handwriting analysis. Longitudinal studies using the handwriting analysis software could help to pinpoint developmentally based changes in the frontal-subcortical system before and after the onset of psychosis, which may guide efforts to understand potential risk markers and implement interventions for those at risk for psychosis.
Disclosures
The authors have nothing to disclose.
Acknowledgements
This work was supported by National Institute of Health Grants R01MH094650 to Dr. Mittal.
Materials
| Material Name | Company | Website | |
| Fujitsu Lifebook T901 Tablet Computer | Fujitsu Ltd. | http://www.shopfujitsu.com/store/ | |
| Neuroscript MovAlyzeR | Neuroscript LLC | http://www.neuroscript.net/movalyzer.php |
References
- Cannon, T. D., et al. Prediction of psychosis in youth at high clinical risk: a multisite longitudinal study in North America. Arch. Gen. Psychiatry. 65, 28-37 (2008).
- Yung, A. R., Phillips, L. J., Yuen, H. P., McGorry, P. D. Risk factors for psychosis in an ultra high-risk group: psychopathology and clinical features. Schizophr. Res. 67, 131-142 (2004).
- Miller, T. J., et al. Prodromal assessment with the structured interview for prodromal syndromes and the scale of prodromal symptoms: predictive validity, interrater reliability, and training to reliability. Schizophr. Bull. 29, 703-715 (2003).
- Cornblatt, B. A., et al. The schizophrenia prodrome revisited: a neurodevelopmental perspective. Schizophr. Bull. 29, 633-651 (2003).
- Mittal, V. A., Dean, D. J., Pelletier, A. Dermatoglyphic asymmetries and fronto-striatal dysfunction in young adults reporting non-clinical psychosis. Acta Psychiatr. Scand. 126, 290-297 (2012).
- Mittal, V. A., Neumann, C., Saczawa, M., Walker, E. F. Longitudinal progression of movement abnormalities in relation to psychotic symptoms in adolescents at high risk of schizophrenia. Arch. Gen. Psychiatry. 65, 165-171 (2008).
- Mittal, V. A., et al. Abnormal movements are associated with poor psychosocial functioning in adolescents at high risk for psychosis. Schizophr. Res. 130, 164-169 (2011).
- Mittal, V. A., et al. Markers of basal ganglia dysfunction and conversion to psychosis: neurocognitive deficits and dyskinesias in the prodromal period. Biol. Psychiatry. 68, 93-99 (2010).
- Walker, D., Diforio, Schizophrenia: a neural diathesis-stress model. Psychol. Rev. 104, 667-685 (1997).
- Walker, E. F., Savoie, T., Davis, D. Neuromotor precursors of schizophrenia. Schizophr. Bull. 20, 441-451 (1994).
- Mittal, V. A., et al. Striatal volumes and dyskinetic movements in youth at high-risk for psychosis. Schizophr. Res. 123, 68-70 (2010).
- Bechdolf, A., et al. Interventions in the initial prodromal states of psychosis in Germany: concept and recruitment. Br. J. Psychiatry Suppl. 48, s45-s48 (2005).
- Mittal, V. A., Dean, D. J., Pelletier, A., Caligiuri, M. Associations between spontaneous movement abnormalities and psychotic-like experiences in the general population. Schizophr. Res. 132, 194-196 (2011).
- Mittal, V. A., et al. BDNF Val66Met and spontaneous dyskinesias in non-clinical psychosis. Schizophr. Res. 140, 65-70 (2012).
- Caligiuri, M. P., Teulings, H. L., Dean, C. E., Niculescu, A. B. Handwriting movement analyses for monitoring drug-induced motor side effects in schizophrenia patients treated with risperidone. Hum. Mov. Sci. 28, 633-642 (2009).
- Caligiuri, M. P., Teulings, H. L., Dean, C. E., Niculescu, A. B., 3rd, J. B., Lohr, Handwriting movement kinematics for quantifying extrapyramidal side effects in patients treated with atypical antipsychotics. Psychiatry Res. 177, 77-83 (2010).
- Caligiuri, M. P., Teulings, H. L., Filoteo, J. V., Song, D., Lohr, J. B. Quantitative measurement of handwriting in the assessment of drug-induced parkinsonism. Hum. Mov. Sci. 25, 510-522 (2006).
- Schizophr Bull, . . 19, 303-315 (1993).
- Andersson, K., Fuxe, K., Agnati, L. F. Effects of single injections of nicotine on the ascending dopamine pathways in the rat. Evidence for increases of dopamine turnover in the mesostriatal and mesolimbic dopamine neurons. Acta Physiol. Scand. 112, 345-347 (1981).
- Lane, R. D., Glazer, W. M., Hansen, T. E., Berman, W. H., Kramer, S. I. Assessment of tardive dyskinesia using the Abnormal Involuntary Movement Scale. J. Nerv. Ment. Dis. 173, 353-357 (1985).
- Zhang, X. Y., et al. Smoking and tardive dyskinesia in male patients with chronic schizophrenia. Prog. Neuropsychopharmacol. Biol. Psychiatry. 35, 1765-1769 (2011).
- Tucha, O., Lange, K. W. Effects of nicotine chewing gum on a real-life motor task: a kinematic analysis of handwriting movements in smokers and non-smokers. Psychopharmacology. 173, 49-56 (2004).
- Teulings, H. L., Contreras-Vidal, J. L., Stelmach, G. E., Adler, C. H. Parkinsonism reduces coordination of fingers, wrist, and arm in fine motor control. Exp. Neurol. 146, 159-170 (1997).
- Lin, C. Y., Yeh, C. H., Chang, T. T., Kao, C. H., Tsai, S. Y. Smoking, dopamine transporter, and hand tremor. Clin. Nucl. Med. 37, 35-38 (2012).
- Van Gemmert, A. W., Teulings, H. L. Advances in graphonomics: studies on fine motor control, its development and disorders. Hum. Mov. Sci. 25, 447-453 (2006).
- Gharabawi, G. M., et al. Abnormal Involuntary Movement Scale (AIMS) and Extrapyramidal Symptom Rating Scale (ESRS): cross-scale comparison in assessing tardive dyskinesia. Schizophr. Res. 77, 119-128 (2005).
- Cortese, L., et al. Relationship of neuromotor disturbances to psychosis symptoms in first-episode neuroleptic-naive schizophrenia patients. Schizophr. Res. 75, 65-75 (2005).
- Howes, O. D., et al. Elevated striatal dopamine function linked to prodromal signs of schizophrenia. Arch. Gen. Psychiatry. 66, 13-20 (2009).
- Van Gemmert, A. W., Teulings, H. L., Contreras-Vidal, J. L., Stelmach, G. E. Parkinson’s disease and the control of size and speed in handwriting. Neuropsychologia. 37, 685-694 (1999).

