Come to the Light Side: In Vivo Monitoring of Pseudomonas aeruginosa Biofilm Infections in Chronic Wounds in a Diabetic Hairless Murine Model
Summary
Here we describe a novel diabetic murine model utilizing hairless mice for real-time, non-invasive, monitoring of biofilm wound infections of bioluminescent Pseudomonas aeruginosa. This method can be adapted to evaluate infection of other bacterial species and genetically modified microorganisms, including multi-species biofilms, and test the efficacy of antibiofilm strategies.
Abstract
The presence of bacteria as structured biofilms in chronic wounds, especially in diabetic patients, is thought to prevent wound healing and resolution. Chronic mouse wounds models have been used to understand the underlying interactions between the microorganisms and the host. The models developed to date rely on the use of haired animals and terminal collection of wound tissue for determination of viable bacteria. While significant insight has been gained with these models, this experimental procedure requires a large number of animals and sampling is time consuming. We have developed a novel murine model that incorporates several optimal innovations to evaluate biofilm progression in chronic wounds: a) it utilizes hairless mice, eliminating the need for hair removal; b) applies pre-formed biofilms to the wounds allowing for the immediate evaluation of persistence and effect of these communities on host; c) monitors biofilm progression by quantifying light production by a genetically engineered bioluminescent strain of Pseudomonas aeruginosa, allowing real-time monitoring of the infection thus reducing the number of animals required per study. In this model, a single full-depth wound is produced on the back of STZ-induced diabetic hairless mice and inoculated with biofilms of the P. aeruginosa bioluminescent strain Xen 41. Light output from the wounds is recorded daily in an in vivo imaging system, allowing for in vivo and in situ rapid biofilm visualization and localization of biofilm bacteria within the wounds. This novel method is flexible as it can be used to study other microorganisms, including genetically engineered species and multi-species biofilms, and may be of special value in testing anti-biofilm strategies including antimicrobial occlusive dressings.
Introduction
Biofilms are complex communities of microorganisms embedded in a matrix of polymeric substances that have been highlighted as a contributing factor for the poor resolution of chronic wounds1. The study of these highly organized, persistent microbial populations is particularly important for diabetic patients where poor circulation on the limbs and altered peripheral sensory mechanisms lead to undetected lesions2. In the United States, it is estimated that 15% of diabetic patients will develop at least one ulcer during the course of their lives. This translates to an economic expenditure of around 28 billion dollars in treatment3,4, not to mention the immensurable emotional and social burden. Understanding the factors that allow microbial communities to persist in the wound bed and the impact these biofilms have in the healing events is imperative to drive better care for affected patients and propel the development of new treatment approaches. Therefore, the establishment of reproducible and translatable in vivo models for exploring bacterial-host interactions is paramount.
Murine models have been successfully developed to study the impact of biofilms in chronic wounds. These models, however, often utilize haired species and evaluate biofilm clearance by plate counts for viable bacterial cells of excised tissue from sacrificed animals, making them time consuming and costly.
A biophotonic alternative to the end point sampling of animals in evaluating infection was first proposed by Contag et al. (1995)5, who developed a method to capture luminescence from constitutively bioluminescent Salmonella typhimurium to measure antibiotic treatment efficacy. Other studies taking advantage of bioluminescence-emitting bacteria followed. For example, Rochetta et al. (2001)6 validated an infection model to study Escherichia coli thigh infections in mice by measuring luminescence using an intensified charge-coupled device and later, Kadurugamuwa et al. (2003)7 took advantage of the photon emitting properties of an engineered strain of Staphylococcus aureus to investigate the efficacy of several antibiotics in a catheter wound model in mice.
The method characterized here presents a straightforward protocol to induce diabetes in hairless mice, produce and inoculate wounds with pre-formed bioluminescent biofilms of P. aeruginosa, and conduct biophotonic monitoring of the infection using an in vivo imaging system. It offers a direct, rapid, in situ, non-invasive and quantitative process to evaluate biofilms in chronic wounds and in addition, allows for additional analysis such as microscopic imaging of the healing wounds, intermittent blood collection for cytokine measurements, and terminal tissue collection for histology.
Protocol
Animal experiments were approved by the Institutional Animal Care and Use Committee of Michigan State University.
1. Preparation of Occlusive Dressings and Silicone Spacers
- Cut the transparent occlusive dressing to make squares approximately 1 cm x 1 cm with scissors.
- Cut 10 mm circles on a 0.5 mm thick silicone sheet using a 10 mm biopsy punch. Center a 5 mm biopsy punch in the middle of the 10 mm circle and press firmly to create a hole to form a "donut"-like disc that will be used as a splint.
2. Experimental Animals
- Use 8 week old (22-26 g) male SKH-1 mice from a commercial breeder. Keep mice in standard conditions of 21 °C and a 12 h light-dark cycle with free access to food and water.
- To induce diabetes, inject mice intraperitonially with a 13 mg/ml streptozotocin (STZ) solutionand 25% Glucose (250 µl per/ mouse) on 5 consecutive days.
- Make the STZ solution by diluting 65 µg of STZ in 5 µL of 100 mM Citric Acid, pH 4.5.
- Adjust the injected volume for each mouse to a final mass of 65 mg STZ per 1 kg of mouse body weight. Inject control mice with 100 mM Citric Acid solution pH 4.5 on the same days.
- Confirm hyperglycemia by blood glucose monitoring with a glucometer 14 days after the last STZ injection. Diabetic mice may have polyuria and so their bedding may need to be changed more frequently to eliminate wetness and their weights should be monitored 3 times a week.
3. Biofilms
- Biofilm preparation
- Grow colony biofilms8 to inoculate the wounds. Two days prior to surgery start an overnight culture of bioluminescent P. aeruginosa Xen 41 in tryptic soy broth (TSB) incubated at 37 °C and shaking at 200 rpm and sterilize polycarbonate membrane filters with 0.2 µm pore size by exposure to UV light in a biological safety hood for 15 min per side.
- One day prior to surgery centrifuge overnight culture at 20,000 x g for 2 min and wash 3 times with 1 mL of Dulbelcco's phosphate buffered saline (DPBS) by pipetting up and down.
- Dilute suspension in DPBS to an absorbance of 0.05 at 600 nm.
- Pipette 10 µL of the diluted culture on each membrane resting on a tryptic soy agar (TSA) plate. After allowing to dry, incubate the membranes at 35 °C for 72 h to grow biofilms transferring to fresh TSA plates every 24 h.
- Standard curve
- Prior to the start of the experiment make a standard curve to correlate bioluminescence and bacterial counts.
- Prepare biofilms as described in 3.1.
- Make serial dilutions of biofilms ranging from ½ to 1/24 by mixing biofilm with DPBS and vortexing until a visually homogeneous solution is produced. Pipette 200µL of the diluted solutions in a black 96-well plate and image with the in vivo imaging system.
- Spread plate dilutions onto TSA plates and incubate at 35 °C for 24 h.
- Count colony forming units (CFU) on plates and create a standard curve to correlate bioluminescence and bacterial counts.
4. Wound Surgery
- Induce general anesthesia using isoflurane in 95% oxygen/5% CO2 (to prevent death from ketoacidosis) at a flow rate of 1 L/min and maintain anesthesia using 1-3% isoflurane. Maintain animals on heat mats during surgery.
- Ensure the deep pedal reflexes of the mouse are suppressed by pinching the foot with tweezers and place the mouse in the prone position.
- Administer meloxicam (0.2 mg/kg) via sub-cutaneous injection (30 μl) for pain management.
- Wipe the skin of the back with 10% povidone-iodine three times and an isopropanol pad.
- Use a sterile 4 mm biopsy punch to outline one circular pattern for the wound on one side of the mouse's midline at the level of the shoulders. Outline the pattern with a permanent marker.
- Use serrated forceps to lift the skin in the middle of the outline and iris scissors to create a full-thickness wound that extends through the subcutaneous tissue including the panniculus carnosus and excise the circular piece of tissue.
- Apply a medical waterproof skin adhesive glue to the skin of the mice and position the silicone splint applying mild pressure. Cover the wound with a transparent occlusive dressing. After surgery, individually cage the animals.
5. Postoperative Management
- Administer meloxicam (0.2 mg/kg) once daily via sub-cutaneous injection for post-operative pain relief for the next 2 days.
- Monitor animals daily for manifestations of pain and weight loss. Diabetic animals need insulin injections when they have lost 15% or more of the body weight.
6. Biofilm Inoculum Preparation and Infection
- Inoculate mice 48 h after surgery as described in the following steps.
- Scrape 72 h biofilms from the membranes using a sterile spatula, place it in a microcentrifuge tube and dilute 1:2 in DPBS. Mix by briefly pipetting up and down.
- Spread plate inoculum onto TSA plates to calculate total CFU. To ensure that counts are accurate, break down the biofilm inoculum further by a series of two 1 min vortexing steps intercalated by a 2 min sonication step at 40 kHz in an ultrasonic cleaner.
- Remove dressing covering the wound and silicone splint and take a micrograph of the wound with a microscope with attached camera using a ruler for reference.
- Cut the tips of 200 µL pipette tips and pipette 10 µL of the biofilm inoculum onto each wound.
- Image mouse using the in vivo imaging system using auto settings: exposure time 5-300 s, with medium binning, 1 f/stop and open filter, and field of view C (12.9 cm x 12.9 cm).
- Cover wound with fresh dressing.
7. Wound Measurement and Imaging
- Evaluate the clinical signs of animals daily9.
- Provide food, water and change cages as needed.
- Check integrity of dressings daily. When the dressing is present, only bioluminescence can be measured due to occlusion of the wound. At day 8, dressings are removed and not replaced allowing measurement of wound closure.
- Weigh animals every other day.
- For all days, place mice individually in an isolation chamber equipped with a HEPA filter and image using the in vivo imaging system daily or every other day until luminescence values fall below background level.
- After day 8, induce general anesthesia and take micrographs of the wound with a microscope with attached camera using a ruler for reference every other day until wounds are healed.
8. Histological Analysis
- Euthanize the mice with a flow of 2 l/min of CO2 in an euthanasia chamber after luminescence falls below background levels and the wounds are completely healed. Confirm death by cervical dislocation as a second method of euthanasia.
- Use iris scissors to create a wide, full excision around and under the wound area (around 1 cm in diameter) and preserve the tissue in 4% paraformaldehyde for histological analysis.
- Other analysis: Cytokine detection
- Collect blood retro-orbitally from animals under anesthesia using a capillary glass tube and transfer it to EDTA-treated tubes.
- Centrifuge blood at 2,000 rpm for 20 min at 4 °C and freeze plasma for cytokine detection.
Representative Results
In developing this new model, we observed many advantages in utilizing hairless SKH-1 over C57BL/6J mice, which we have used in the past. Animals subjected to STZ injections normally experience gradual weight loss with the onset of diabetes; however, in wound healing experiments previously conducted by our laboratories reproducing the model presented by Dunn et al. (2012)9 using C57BL/6J, drastic weight loss was observed (Figure 1). In contrast, when using this wound model with SKH-1 mice a statistically significant lower weight loss was observed (P<0.0001, Mann-Whitney U test). Furthermore, no deaths occurred in the diabetic SKH-1 mice cohort infected with P. aeruginosa Xen 41 biofilms while a 40% mortality rate was observed for C57BL/6J infected mice in previous experiments (Figure 2).
Another advantage to the model presented here is that the experimental procedure for the hair removal step mandatory for C57BL/6J mice is unnecessary for SKH-1 mice. Although in our previous experiments with haired mice special attention was given to minimize irritation to the skin, some damage inevitably occurred (Figure 3). Notably, however, the greatest advantage in utilizing hairless mice in this model is the elimination of the problem of hair re-growth observed in long term wound healing studies. In our experience with C57BL/6J mice, hair re-growth varied from animal to animal but given the long-term nature of the studies, it always occurred and interfered with wound area measurements or dislocated wound splints and/or dressings used to cover infected wounds, potentially resulting in drying of the wound (Figure 4).
In the SKH-1 wound healing model, after diabetes is confirmed, surgery can easily be executed to create a circular full-thickness wound on the back of the animal. The silicone splint is kept in place by a medical waterproof skin adhesive and avoids direct contact from the occlusive dressing with the newly created wound bed (Figure 5).
P. aeruginosa Xen 41 bioluminescent biofilms grown on polycarbonate membranes (Figure 6) are easily and aseptically transferred to a syringe to be prepared for delivery to the wounds and the inoculated mice are monitored daily for clinical signs of infection (Figure 7). For this model, we implemented two distinct phases. In the first phase, after inoculation of the biofilm the wound was surrounded by a splint covered with a transparent occlusive dressing. This results in pus accumulation that occluded the wound. Biofilm-containing wounds were imaged daily with the in vivo imaging system to monitor infection development and assess biofilm evolution (Figure 8 and Figure 9). Bioluminescence, recorded as total flux (p/s), can be correlated with bacterial density using a standard curve (Figure 10).
At day 8, the splint and dressing were removed to allow visualization of wound healing. Bioluminescence subsequently drops due to the loss of the pus surrounding the wound; however, bacteria remained associated with the wound as determined by histology. This approach of removing the dressing to measure wound healing has been utilized in other chronic wounds healing studies (REFs). Wound healing progression can be determined by taking micrographs with a camera attached to a microscope (Figure 11).
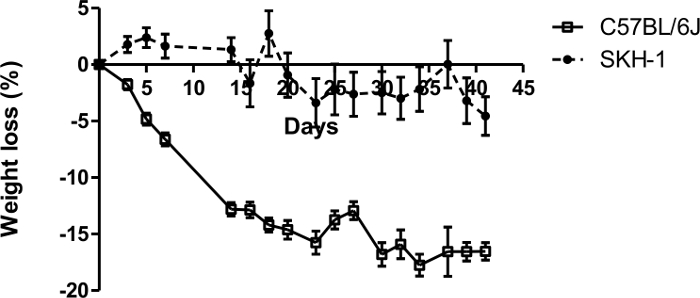
Figure 1: Comparative percentage weight loss of SKH-1 and C57BL/6J diabetic mice. Day zero corresponds to weight at the day of last (5th) STZ injection. n = 10 mice for SKH-1 and n = 12 mice for C57BL/6J. Please click here to view a larger version of this figure.
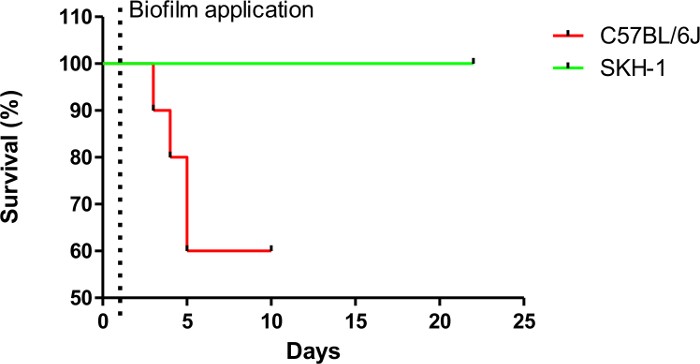
Figure 2: Percent survival rates of SKH-1 and C57BL/6J diabetic mice after P. aeruginosa Xen 41 biofilm application (day 1). n = 5 mice for SKH-1 and n = 10 mice for C57BL/6J. Please click here to view a larger version of this figure.
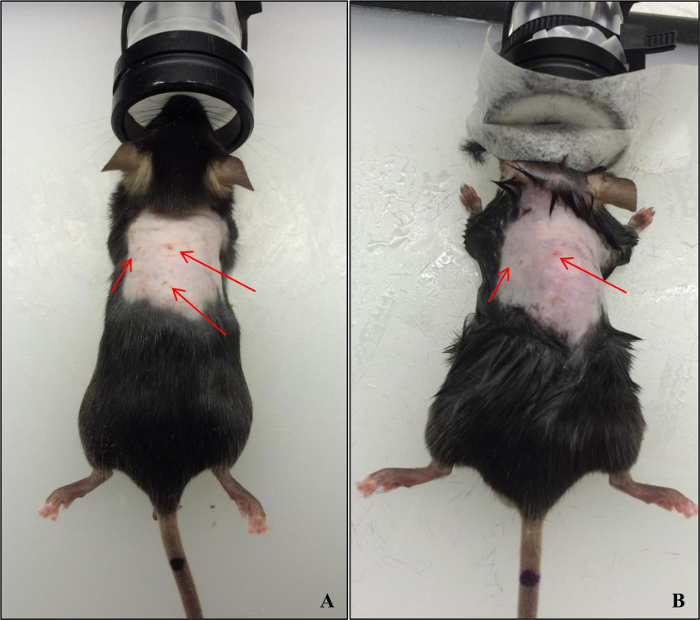
Figure 3: Skin lacerations in the future wounded area after shaving and using depilatory cream on C57BL/6J mice. (A): day of procedure; (B): 4 days after procedure. Please click here to view a larger version of this figure.
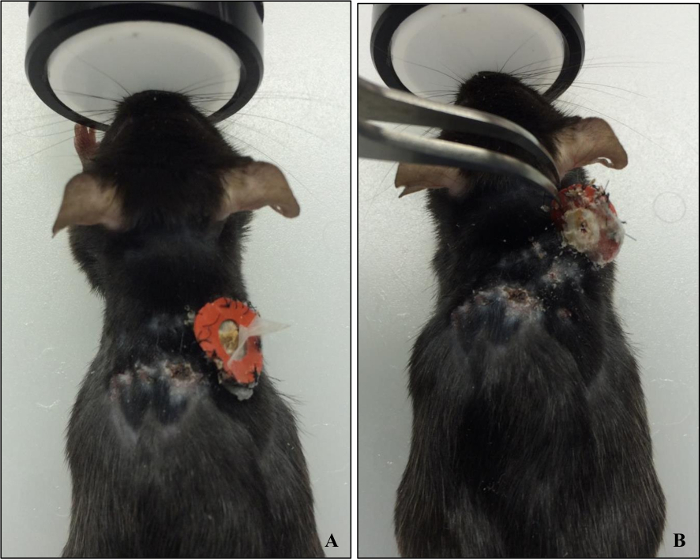
Figure 4: (A) C57BL/6J mouse with a partially removed wound splint. (B) Lifting of the splint revealed a healed wound surrounded by fully re-grown hair. Please click here to view a larger version of this figure.
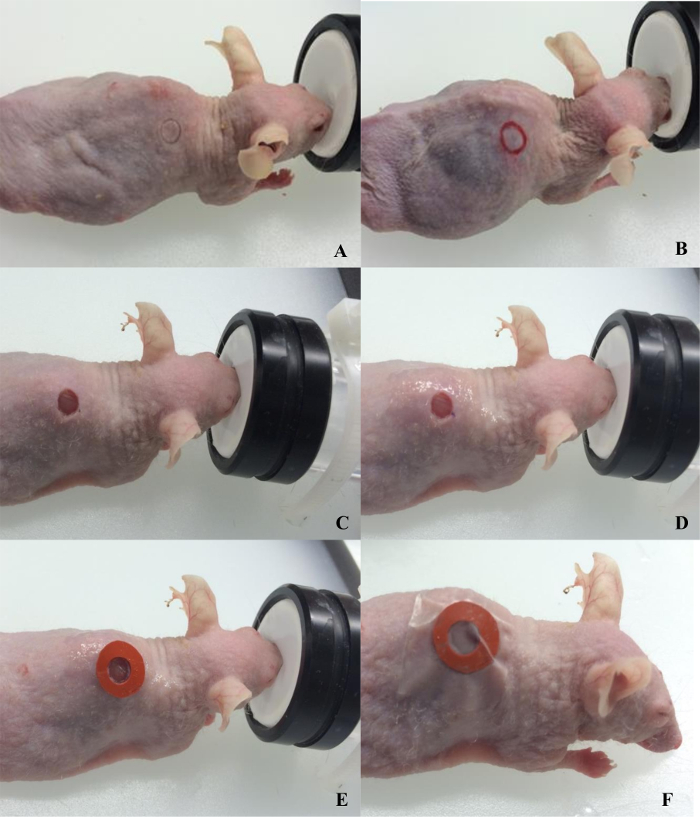
Figure 5: Surgical procedure for wounding SKH-1 mice. (A) demarcation with biopsy punch; (B) outline of the demarcation; (C) wounding completed; (D) application of medical waterproof skin adhesive; (E) glueing splint; (F) wound covered with occlusive dressing. Please click here to view a larger version of this figure.
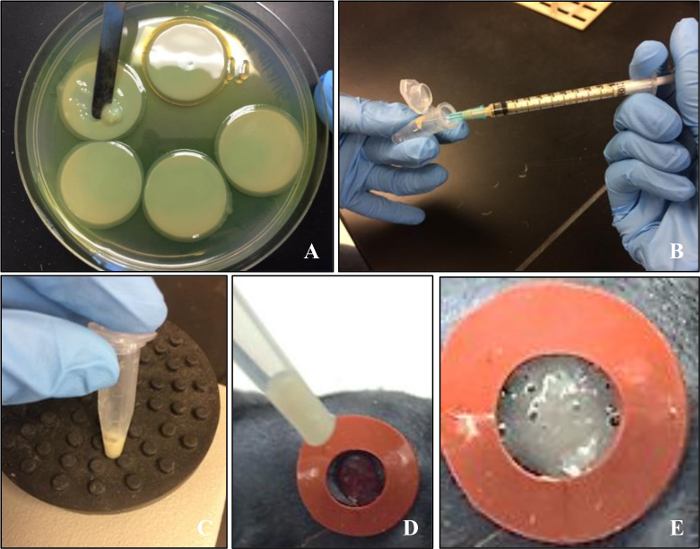
Figure 6: Preparation of the biofilm inoculum. (A) 72 h colony biofilms of Pseudomonas aeruginosa Xen 41 grown on polycarbonate membranes; (B) measurement of biofilm using a syringe. Please click here to view a larger version of this figure.

Figure 7: SKH-1 diabetic mouse 6 days after wound was inoculated with the P. aeruginosa Xen 41 biofilm. Please click here to view a larger version of this figure.
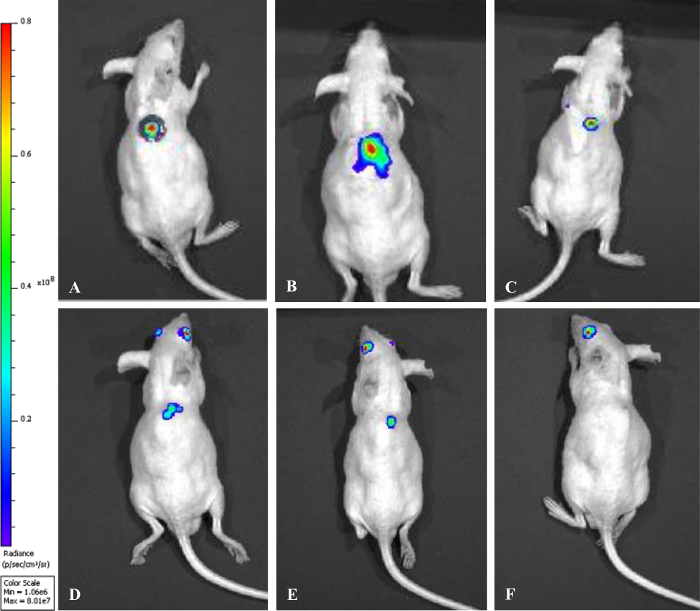
Figure 8: Monitoring of biofilm infection by tracking bioluminescence evolution over time in diabetic SKH-1 mice. (A) day of biofilm application; (B) 5 days post-biofilm; (C) 8 days post-biofilm; (D) 12 days post-biofilm; (E) 16 days post-biofilm; (F) 20 days post-biofilm. Please click here to view a larger version of this figure.
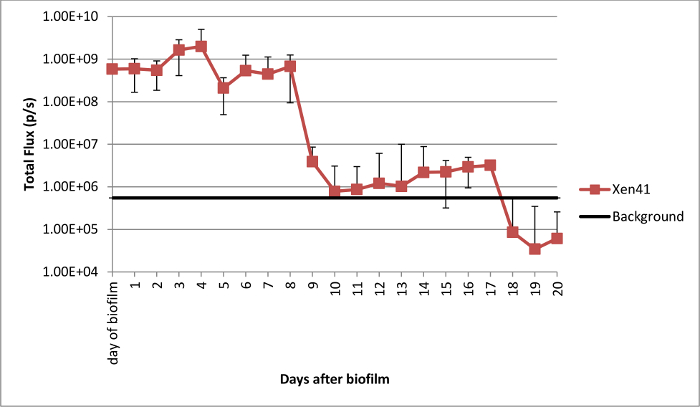
Figure 9: Total flux from wounds in SKH-1 diabetic mice infected with P. aeruginosa Xen 41 biofilms during the course of the experiment. Please click here to view a larger version of this figure.
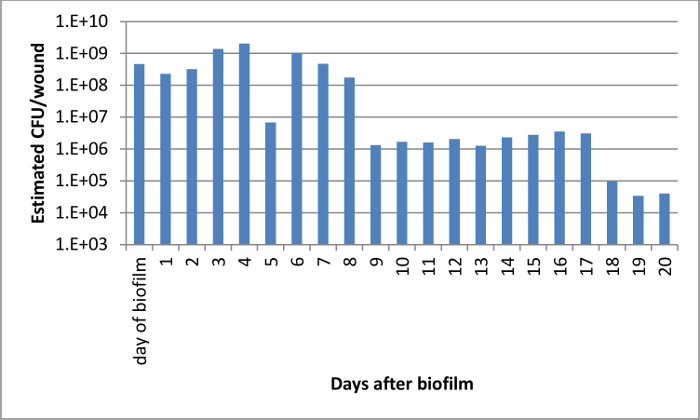
Figure 10: Estimated CFU per wound using a standard curve of bioluminescence per CFU produced with P. aeruginosa Xen 41 biofilms. Please click here to view a larger version of this figure.
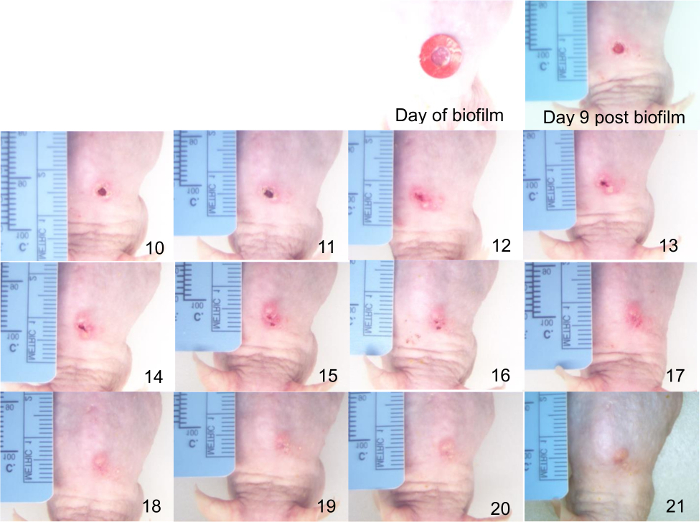
Figure 11: Micrograph timeline of wounds infected with P. aeruginosa Xen 41 biofilms in diabetic SKH-1 mouse showing progression of healing. The days after biofilm infection are indicated in the bottom left corner of each picture. Please click here to view a larger version of this figure.
Discussion
Here we describe a new mouse model for the study of biofilms in diabetic chronic wounds that has many advantages to create a reproducible, translatable, and flexible model.
The first innovation is the use of hairless mice. Other mouse models have been developed to study diabetic chronic wound healing10,11, but all have relied on the use of haired mice requiring the removal of fur by processes that involve either waxing or hair clipping combined with depilatory creams. This step is not only time consuming and messy but potentially injures the skin of the animals in the area where the wound will be placed. While hairless mice have been used in a series of carcinogenesis studies12,13, these mice have not been used to evaluate biofilm persistence in chronic wounds. Another common problem solved by the use of hairless animals, especially in long term studies, is hair re-growth in the wound area, which may jeopardize evaluation of wound healing and disrupt bandaging.
SKH-1 animals also proved amenable to STZ-induced Type I diabetes and, in comparison with C57BL/6J mice, had statistically significant lower weight loss during the course of the experiment, making dosing with insulin unnecessary. This is a particularly interesting trait as treatment with insulin can potentially impact the infection outcome as evidenced by Watters et al. (2014)14 who described an increase in bacterial counts in insulin-treated diabetic animals infected with P. aeruginosa biofilms in comparison to no insulin counterparts. In addition, in our model, there was a drastic reduction in mortality rates in the hairless cohort indicating that the animals are potentially more resilient in dealing with infection.
A second feature of this model is the application of measured pre-formed biofilm inoculum slurry to infect the wounds in contrast to planktonic grown cells. By delivering an already metabolically complex and structured bacterial community to the wound, the bacterial cells are able to evade the immune system and the immediate effects of the biofilms on the lesions can be determined.
The third advantage of this new wound model is the use of a microbial strain capable of producing bioluminescence that can be measured with an in vivo imaging system to spatially localize and quantify the bacteria. This allows real-time tracking of biofilm evolution over time. The P. aeruginosa Xen 41 strain possesses a single stable copy of the P. luminescences luxCDABE operon on the bacterial chromosome that results in the constitutive emission of luminescence, which can be captured by the ultra-sensitive camera in the imaging system. This real-time, non-invasive, in situ feature allows measuring of biofilm by bioluminescence even while the splint and cover are in place. This feature drastically decreases the number of animals needed per study, as there is no need to sacrifice animals at certain time points for biofilm monitoring. However, the presence of biofilm and pus occluded measuring wound healing. In this study, we removed the dressing at day 8 to allow visualization of wound healing, but this parameter could be modified depending on the questions being addressed.
Lastly, as the imaging system is capable of detecting bioluminescence up to 2.5 cm in depth, the newly proposed model is amenable to testing of antimicrobial therapies whether in form of solution or gels or incorporated to occlusive dressings. A real-time infection monitoring model allows much greater flexibility to measure the impact of different dosing concentrations and durations as opposed to a static end-point assay. This model can contribute to the validation of potential novel treatments to eradicate biofilms in chronic wounds.
Disclosures
The authors have nothing to disclose.
Acknowledgements
The authors would like to thank the American Diabetes Association for supporting this work (Grant # #7-13-BS-180), the Michigan State University Research Technology Support Facility for providing training and access to the in vivo imaging system and the Michigan State University Investigative Histopathology Lab for processing the mouse biopsies for histopathological examination.
Materials
| Opsite | Smith & Nephew | Model 66000041 | Smith & Nephew Flexfix Opsite Transparent Adhesive Film Roll 4" x 11yards |
| SKH-1 mice Crl:SKH1-Hrhr | Charles River Breeding Laboratories | SKH1 | Hairless mice, 8 weeks old |
| Streptozotocin (STZ) | Sigma Aldrich | S0130-1G | Streptozocin powder, 1g |
| AccuChek glucometer | Accu-Chek Roche | Art No. 05046025001 | ACCU-CHEK CompactPlus Diabetes Monitoring Care Kit |
| Pseudomonas aeruginosa Xen 41 | Perkin Elmer | 119229 | Bioluminescent Pseudomonas aeruginosa |
| Polycarbonate membrane filters | Sigma Aldrich | P9199 | Millipore polycarbonate membrane filters with 0.2 μm pore size |
| Dulbelcco phosphate buffer saline (DPBS) | Sigma Aldrich | D8537 | PBS |
| Tryptic soy agar | Sigma Aldrich | 22091 | Culture agar |
| Meloxicam | Henry Schein Animal Health | 49755 | Eloxiject (Meloxicam) 5mg/mL, solution for injection |
| 10% povidone-iodine (Betadine) | Purdue Products LP | 301879-OA | Swabstick, Betadine Solution. Antiseptic. Individ. Wrapped, 200/case |
| 4% paraformaldehyde | Fisher Scientific | AAJ61899AK | Alfa Aesar Paraformaldehyde, 4% in PBS |
| Capillary glass tube | Fisher Scientific | 22-362-566 | Heparinized Micro-Hematocrit Capillary Tubes |
| Silicone to make splints | Invitrogen Life Technologies Corp | P-18178 | Press-to-Seal Silicone Sheet, 13cm x 18cm, 0.5mm thick, set of 5 sheets |
| Tryptic soy broth | Sigma Aldrich | 22092 | Culture broth |
| IVIS Spectrum | Perkin Elmer | 124262 | In vivo imaging system |
| IVIS Spectrum Isolation chamber | Perkin Elmer | 123997 | XIC-3 animal isolation chamber |
| HEPA filter | Teleflex | 28022 | Gibeck ISO-Gard HEPA Light number 28022 |
| Biopsy punches | VWR International Inc | 21909-142 | Disposable Biopsy Punch, 5mm, Sterile, pack of 50. |
| Biopsy punches | VWR International Inc | 21909-140 | Disposable Biopsy Punch, 4mm, Sterile, pack of 50. |
| Glucose | J.T.Baker | 1916-01 | Dextrose, Anhydrous, Powder |
| Citric acid | Sigma Aldrich | C2404-100G | Citric Acid |
| Mastisol | Eloquest Healthcare | HRI 0496-0523-48 | Mastisol Medical Liquid Adhesive 2/3 mL vial, box of 48 |
| Corning 96-well black plates | Fisher Scientific | 07-200-567 | 96-well clear bottom black polysterene microplates |
| 25 gauge 5/8 inch needle | BD | 305122 | Regular bevel needle |
| Bransonic M Ultrasonic Cleaning Bath | Branson Ultrasonics | N/A | Ultrasonic Cleaner |
References
- James, G. A., et al. Biofilms in chronic wounds. Wound Repair Regen. 16 (1), 37-44 (2008).
- Gordois, A., Scuffham, P., Shearer, A., Oglesby, A., Tobian, J. A. The health care costs of diabetic peripheral neuropathy in the US. Diabetes Care. 26 (6), 1790-1795 (2003).
- Reiber, G. E., McDonell, M. B., Schleyer, A. M., Fihn, S. D., Reda, D. J. A comprehensive system for quality improvement in ambulatory care: assessing the quality of diabetes care. Patient Educ Couns. 26 (1-3), 337-341 (1995).
- Driver, V. R., Fabbi, M., Lavery, L. A., Gibbons, G. The costs of diabetic foot: The economic case for the limb salvage team. J Vasc Surg. 52 (Suppl 3), 17S-22S (2010).
- Contag, C. H., et al. Photonic detection of bacterial pathogens in living hosts. Mol Microbiol. 18 (4), 593-603 (1995).
- Rocchetta, H. L., et al. Validation of a noninvasive, real-time imaging technology using bioluminescent Escherichia coli in the neutropenic mouse thigh model of infection. Antimicrob Agents Chemother. 45 (1), 129-137 (2001).
- Kadurugamuwa, J. L., et al. Rapid direct method for monitoring antibiotics in a mouse model of bacterial biofilm infection. Antimicrob Agents Chemother. 47 (0066-4804), 3130-3137 (2003).
- Anderl, J. N., Franklin, M. J., Stewart, P. S. Role of antibiotic penetration limitation in Klebsiella pneumoniae biofilm resistance to ampicillin and ciprofloxacin. Antimicrob Agents Chemother. 44 (7), 1818-1824 (2000).
- Morton, D. B. A systematic approach for establishing humane endpoints. ILAR J. 41 (2), 80-86 (2000).
- Dunn, L., et al. Murine model of wound healing. J Vis Exp. (75), e50265 (2013).
- Zhao, G., et al. Delayed wound healing in diabetic (db/db) mice with Pseudomonas aeruginosa biofilm challenge – a model for the study of chronic wounds. Wound Repair Regen. 18 (5), 467-477 (2010).
- Holley, A. K., Xu, Y., Noel, T., Bakthavatchalu, V., Batinic-Haberle, I., St. Clair, D. K. Manganese superoxide dismutase-mediated inside-out signaling in HaCaT human keratinocytes and SKH-1 mouse skin. Antioxid Redox Signal. 20 (15), 2347-2360 (2014).
- Abbas, S., Alam, S., Pal, A., Kumar, M., Singh, D., Ansari, K. M. UVB exposure enhanced benzanthrone-induced inflammatory responses in SKH-1 mouse skin by activating the expression of COX-2 and iNOS through MAP kinases/NF-ĸB/AP-1 signalling pathways. Food Chem Toxicol. 96, 183-190 (2016).
- Watters, C., Everett, J. A., Haley, C., Clinton, A., Rumbaugh, K. P. Insulin treatment modulates the host immune system to enhance Pseudomonas aeruginosa wound biofilms. Infect Immun. 82 (1), 92-100 (2014).

