Analysis of Cerebral Vasospasm in a Murine Model of Subarachnoid Hemorrhage with High Frequency Transcranial Duplex Ultrasound
Summary
The aim of this manuscript is to present a sonography-based method that allows in vivo imaging of blood flow in cerebral arteries in mice. We demonstrate its application to determine changes in blood flow velocities associated with vasospasm in murine models of subarachnoid hemorrhage (SAH).
Abstract
Cerebral vasospasm that occurs in the weeks after subarachnoid hemorrhage, a type of hemorrhagic stroke, contributes to delayed cerebral ischemia. A problem encountered in experimental studies using murine models of SAH is that methods for in vivo monitoring of cerebral vasospasm in mice are lacking. Here, we demonstrate the application of high frequency ultrasound to perform transcranial Duplex sonography examinations on mice. Using the method, the internal carotid arteries (ICA) could be identified. The blood flow velocities in the intracranial ICAs were accelerated significantly after induction of SAH, while blood flow velocities in the extracranial ICAs remained low, indicating cerebral vasospasm. In conclusion, the method demonstrated here allows functional, noninvasive in vivo monitoring of cerebral vasospasm in a murine SAH model.
Introduction
Spontaneous subarachnoid hemorrhage (SAH) is a form of hemorrhagic stroke mostly caused by the rupture of an intracranial aneurysm1. The neurological outcome is mainly influenced by two factors: early brain injury (EBI), which is caused by the effects of the bleeding and the associated transient global cerebral ischemia, and delayed cerebral ischemia (DCI), which occurs during the weeks following the bleeding2,3. DCI was reported to affect up to 30% of SAH patients2. The pathophysiology of DCI involves angiographic cerebral vasospasm, a disturbed microcirculation caused by microvasospasms and microthrombosis, cortical spreading depressions, and effects triggered by inflammation4. Unfortunately, the exact pathophysiology remains unclear and there is no treatment available that effectively prevents DCI3. Therefore, DCI is investigated in many clinical and experimental studies.
Nowadays, most experimental studies on SAH use small animal models, especially in mice5,6,7,8,9,10,11,12,13. In such studies, cerebral vasospasm is frequently investigated as an endpoint. It is common to determine the degree of vasospasm ex vivo. This is because noninvasive methods for in vivo examination of cerebral vasospasm requiring short anesthesia time and imposing only little distress on the animals are lacking. However, examination of cerebral vasospasm in vivo would be advantageous. This is because it would allow longitudinal in vivo studies on vasospasm in mice (i.e., imaging of cerebral vasospasm at different time points during the days after induction of SAH). This would enhance the comparability of data acquired at different time points. Furthermore, using a longitudinal study design is a strategy to reduce animal numbers.
Here we demonstrate the use of high frequency transcranial ultrasound to determine the blood flow in cerebral arteries in mice. We show that, similar to transcranial Doppler sonography (TCD) or transcranial color-coded Duplex sonography (TCCD) in clinical practice14,15,16,17,18, this method can be used to monitor cerebral vasospasm by measuring the blood flow velocities of the intracranial arteries after SAH induction in the murine model.
Protocol
The animal experiments were approved by the responsible animal care committee (Landesuntersuchungsamt Rheinland-Pfalz) and conducted in accordance with the German Animal Welfare Act (TierSchG). All applicable international, national, and institutional guidelines for the care and use of animals were followed. In this study, we performed measurements of blood flow velocities of intracranial and extracranial arteries in female C57BL/6N mice aged 11-12 weeks with a body weight between 19-21 g. The mice were subjected to either SAH induction or sham surgery, which has been described in detail elsewhere10,12,13.
1. Preparation of materials
- Switch on the ultrasound machine and enter the animal ID.
- Warm the heating plate of the ultrasound system to 37 °C. Ensure that the rectal temperature probe is ready for use.
- Use a water bath to heat the ultrasound gel to 37 °C. Prepare hair removal cream, contact cream for the electrodes, and eye ointment.
2. Anesthesia
- Induce anesthesia by putting the mouse in a chamber flushed with 4% isoflurane and 40% O2 for 1 min. Protect the eyes with eye ointment. Continue only after a sufficiently deep anesthesia has been reached (absence of reactions to pain stimuli).
- Maintain anesthesia with 1.5% isoflurane and 40% O2 using an anesthesia mask throughout the entire procedure.
3. Determination of blood flow velocities of the intracranial internal carotid arteries with transcranial high-frequency Duplex sonography
- Place the mouse in the prone position on the heating plate of the ultrasound system to maintain a body temperature of 37 °C.
- Coat the four extremities of the animal with conductive paste and fix them with tape on the ECG electrodes embedded in the board. Check if the physiological parameters (ECG, respiration signal) are displayed correctly on the screen of the imaging system (e.g., Vevo3100). If necessary, adjust the level of anesthesia to obtain target heart rate of 400-500 beats per minute (bpm).
- Place lube on a rectal temperature probe and carefully insert it to monitor the body temperature. Use an additional warming lamp if necessary.
- Before the first exam, remove the fur at the occiput chemically using hair removal cream. Use a cotton swab to spread and rub the cream for 2 min until the hairs start to fall out.
- After an additional 2 min, remove the cream and hairs with a spatula and disinfect the skin with an alcoholic skin antiseptic. Coat it with ultrasound gel warmed to 37 °C.
- Use a 38 MHz linear array transducer and a frame rate above 200 frames/s to acquire ultrasound images and fixate the probe in the mechanical arm. Place the transducer on the occiput tilted back by 30°.
- Use Brightness-(B)-mode and Color-wave-(CW) Doppler-mode to visualize the right intracranial internal carotid artery and move the transducer with the control unit back and forward, until the maximal flow of the arteries is found.
- To collect anatomical information, use the traditional B-Mode and CW-Doppler-mode and start acquisition by clicking on the Acquire button.
- To record information on the flow characteristics of the intracranial vessels click on the Pulse-Wave (PW) Doppler button, place the sample volume in the center of the vessel, and acquire a cine loop longer than 3 s.
- Proceed identically with the left side.
- Proceed with the extracranial carotid arteries.
4. Determination of blood flow velocities of the extracranial internal carotid arteries with high frequency Duplex sonography
- Place the mouse in the supine position on the heating plate of the ultrasound system to maintain a body temperature of 37 °C.
- Coat the four extremities of the animal with conductive paste and fix them with tape on the ECG electrodes embedded in the board. Check again for the correct display of the physiological parameters on the screen.
- Before the first exam, remove the hair at the front neck chemically by using hair removal cream as described above. Coat the front neck with ultrasound gel warmed to 37 °C.
- Use a 38 MHz linear array transducer and a frame rate above 200 frames/s to acquire ultrasound images. Place the transducer parallel to the animal and adjust the position in order to obtain longitudinal images of the right carotid artery.
- Use Brightness-(B)-mode and Color-wave-(CW) Doppler-mode to visualize the right carotid artery. The image should contain the right common carotid artery (RCC), the right internal carotid artery (RICA) and the right external carotid artery (RECA).
- To collect anatomical information, use the traditional B-Mode and CW-Doppler-mode and start acquisition by clicking on the Acquire button.
- To record information on the flow characteristics of the extracranial carotid artery click on the Pulse-Wave (PW) Doppler button, place the sample volume in the center of the middle of the common carotid artery, the internal carotid artery and the external carotid artery and acquire a cine loop longer than 3 s.
- Proceed identically with the left side.
- Terminate anesthesia and remove the animal from the warming plate. Return the animal to a cage placed in an incubator heated to 37 °C for 1 hour to prevent hypothermia and check for full recovery.
5. Processing of ultrasonography data
- Use an external workstation for post-processing of the high-frequency ultrasound data. Export the B-mode, CW-Doppler-mode and PW-Doppler-mode images and cine loops.
- Open the exported ultrasound study. Select one animal and open the PW-Doppler cine loop of the intracranial carotid artery. In this protocol typically 7 to 8 heartbeats and corresponding flow-velocity curves are recorded.
- Pause the cine loop and click on the Measurement button. Choose the Vascular Package and click on RICA PSV to measure the peak systolic pressure (PSV). Now click left on the peak of a velocity curve and pull the straight line to the zero line. Determine the measurement by a click with the right mouse button.
- Now choose RICA EDV to measure the enddiastolic velocity (EDV). Click left on minimal rash of the velocity curve at the end of the diastole. Pull the line straight to the zero line and determine measurement by a click with the right mouse button.
- Choose RICA VTI to measure the velocity time integral (VTI). Click left at the beginning of a velocity curve and follow the curve with the mouse until the end of the diastolic plateau. Then click right again to determine the measurement.
- Export the data of the intracerebral internal carotid arteries by using the report button. Press Export and save the data as a VSI Report file.
- Use the same approach to measure PSV, EDV and VTI of the right extracranial internal carotid arteries and export the data accordingly.
- Proceed identically with the left side.
Representative Results
In 6 mice, in 3 of which SAH was induced using the endovascular filament perforation model while 3 obtained sham surgery, the blood flow velocities of the intracranial internal carotid artery (ICA) and of the extracranial ICA were determined one day before surgery, and 1, 3, and 7 days after surgery. The measurements were performed as part of the echocardiography examinations of another study under anesthesia with isoflurane while maintaining the body temperature at 37 °C19.
Before surgery, extra- and intracranial blood flow velocities, as well as the quotients of intra- and extracranial blood flow were similar between SAH and sham animals. On the first day after SAH induction there were no major changes in intra- or extracranial blood flow velocities or the ratios of intra- and extracranial blood flow.
On days 3 and 7 the intracranial blood flow velocities of the ICA increased markedly in 2 of the SAH animals, indicating cerebral vasospasm after SAH. As the extracranial blood flow velocities remained nearly unchanged, the ratio of intra-/extracranial blood flow velocities also increased significantly on day 7 in the SAH animals, indicating cerebral vasospasm.
Representative Duplex sonography recordings of intra- and extracranial ICA are shown in Figure 1. The course of blood flow velocities is shown in Figure 2.
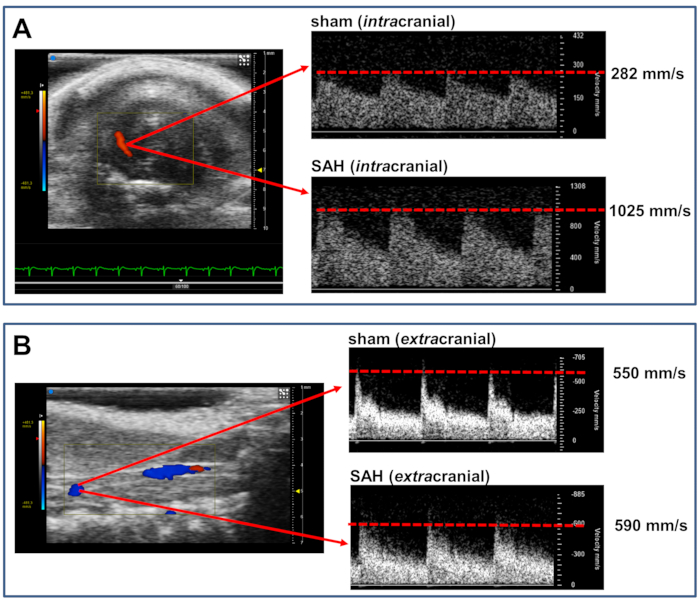
Figure 1 Representative Duplex sonography findings of intra- and extracranial ICA . (A) shows representative findings of the intracranial ICA at day 7 after SAH induction or sham surgery. Note the accelerated blood flow velocity after SAH. (B) shows representative findings of the extracranial ICA at day 7 after SAH induction or sham surgery. Please click here to view a larger version of this figure.
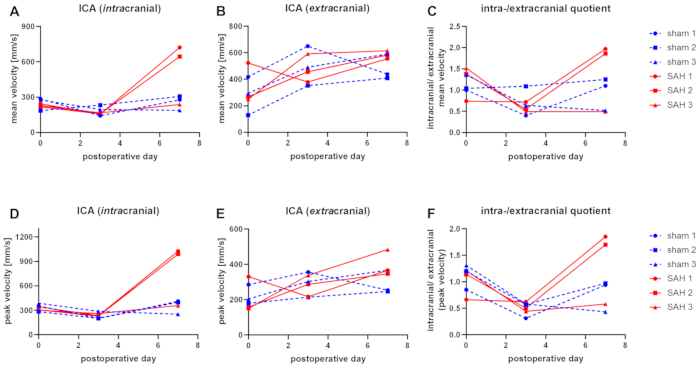
Figure 2 Blood flow velocities in SAH and sham operated mice Blood flow velocities in the right intracranial (A, D), and extracranial (B, E) ICA. (C) And (F) show the ratios of intra- and extracranial blood flow velocities. The upper panel (A-C) shows mean blood flow velocities, the lower panel (D-F) shows peak blood flow velocities. Please click here to view a larger version of this figure.
Discussion
To the best of our knowledge, this study is the first to present a protocol for monitoring of cerebral vasospasm in a murine model of SAH with high frequency transcranial color-coded Duplex ultrasound. We show that this method can measure an increase in intracranial blood flow velocities after SAH induction in mice. In human medicine this phenomenon is well known3,15. Several clinical studies have shown that elevated blood flow velocities of the large intracranial arteries and an elevated quotient of intra- and extracranial blood flow velocities are a functional consequence of vessel narrowing and correlate with angiographic vasospasm (reviewed in15). In clinical practice, it is therefore common to use TCD or TCCD for non-invasive bedside monitoring of cerebral vasospasm after SAH3,15.
DCI is a significant factor influencing neurological outcome after non-traumatic SAH2,3. As the pathophysiology of DCI is still unclear and effective strategies to prevent and treat DCI are lacking, it is in the focus of clinical and experimental research. Because vasospasm of the cerebral arteries contributes to DCI, many studies evaluate cerebral vasospasm as an endpoint5,6,7,8,9,11,12,20. While formerly large animals were frequently used in experimental studies on SAH, there has been a shift towards small animal models in the last years, particularly to murine models21. However, a problem is that imaging methods for cerebral vasospasm used in human medicine cannot be directly transferred to mice and other small animals. Clinical sonography equipment does not yield a sufficient resolution to monitor cerebral vasospasm in mice. There is the possibility of small animal MRI or CT scanning22. However, these methods are cost-intensive and time-consuming. Furthermore, they induce distress in the animals because of the duration of the imaging protocols and contrast application. Moreover, a precise measurement of diameters or volumes of intracranial vessel segments is also limited with these in vivo methods. In SAH studies using mice, it is therefore common to determine the degree of cerebral vasospasm ex vivo5,6,7,8,9,11,12,20. The method presented here is fast, reducing the anesthesia time for the exam to less than 10 minutes, and therefore presumably induces only little distress in the animals. The examination is noninvasive and exhibits a sufficient resolution to visualize and determine the blood flow velocities of large intracranial vessels (ICA and middle cerebral artery). It would therefore be well suited for functional monitoring of cerebral vasospasm in longitudinal studies, examining the same animals at different time points. In studies not requiring histology or other tissue examinations together with the examinations on vasospasm, a longitudinal study design could be used to reduce animal numbers. For future studies focusing on modulation of vasospasm after SAH, determination of blood gases should be performed at the time of the ultrasonographic determinations of cerebral blood flow velocities.
The method shown here contains several critical steps, which should be reviewed in case of methodological problems. It is critical that the body temperature of the animal is kept constant during the whole procedure. Mice quickly develop hypothermia after induction of anesthesia if they are not warmed (e.g., with a heating plate). Hypothermia may alter the results of the measurements. Because of this the ultrasound gel should also be warmed to 37 °C in a water bath before application. Secondly, in order to standardize the measurements, it is necessary that the angle in which the ultrasound probe is applied is constant between the exams. It is therefore necessary to position the animal carefully. The ultrasound probe should not be used free hand but be mounted on a holder with a micromanipulator to allow insonation at a defined position and angle. Furthermore, it is critical to use constant technical settings of the ultrasound device within an experimental series to reduce technical variations. Thirdly, it should be noted that the Duplex examination is not feasible in the time immediately after SAH induction. During this period, an elevated intracranial pressure leads to cerebral hypoperfusion, which limits the application of transcranial Duplex sonography. The Duplex examination of the extracranial carotid artery exposed during the operation for SAH induction may furthermore be impaired by surgical artifacts.
Finally, we want to discuss limitations and future directions of the method presented here. Similar to TCD or TCCD in clinical practice, we cannot directly measure the vessel diameter. An acceleration of the blood flow velocities of cerebral arteries could therefore also be caused by cerebral hyperperfusion. However, clinical studies showed a correlation between an accelerated blood flow velocity and angiographic vasospasm15. Furthermore, we did not observe cerebral cortical hyperperfusion after SAH induction in the murine model used here19, and the increase of intracranial blood flow velocities was accompanied by an increase of the quotients of intra- and extracranial blood flow velocities of the ICA, which was reported to indicate vasospasm in a clinical study23. We therefore assume that the accelerated blood flow velocities also indicate vasospasm in the SAH mouse model, although, as in the clinical application of Doppler ultrasonography, it is not possible to distinguish between vasospasm and cerebral hyperperfusion with hyperdynamic flow. Secondly, functional monitoring of cerebral blood flow velocities only allows conclusions on cerebral vasospasm. Direct imaging and quantification of cerebral perfusion in the context of DCI is not possible. Nevertheless, it should be noted that determination of cerebral perfusion with ultrasonography has been reported in a clinical application24. We therefore speculate that ultrasonographic quantification of cerebral perfusion in mice will become available in the future. A modification of the method in this respect would then allow conclusions not only on vasospasm of the large vessels, but also on microcirculatory disturbances. Thirdly, clinical studies have reported a high investigator dependence of bedside transcranial ultrasonography studies17,25. However, this is presumably not the case for the experimental application shown here, because of the highly standardized and controlled settings in experimental studies, and because in mice the imaging resolution allowed a clear identification of the vessel segments to be analyzed. Lastly, it is a disadvantage that vasospasm is determined at defined anatomical positions. Vasospasm of neighboring segments could therefore escape evaluation. It should be noted, however, that this problem also arises with other methods determining vasospasm. A measure to reduce errors from this source in future experimental studies would be to determine cerebral blood flow velocities of several intracranial vessel segments.
Disclosures
The authors have nothing to disclose.
Acknowledgements
The authors would like to thank Stefan Kindel for preparation of the illustrations in the video. PW, MM and SHK were supported by the German Federal Ministry for Education and Research (BMBF 01EO1503). The work was supported by a Large Instrumentation Grant of the German Research Foundation (DFG INST 371/47-1 FUGG). MM was supported by a grant from the Else Kröner-Fresenius-Stiftung (2020_EKEA.144).
Materials
| Balea hair removal creme | Balea; Germany | ASIN B0759XM39V | hair removal creme |
| C57BL/6N mice | Janvier; Saint-Berthevin Cedex, France | n.a. | mice |
| Corneregel | Bausch&Lomb; Rochester, NY, USA | REF 81552983 | eye ointment, lube |
| cotton swabs | Hecht Assistent; Sondenheim vor der Röhn, Germany | REF 44302010 | cotton swabs |
| Ecco-XS razor | Tondeo; Soligen, Germany | DE 28693396 | razor |
| Electrode cream | GE; Boston, MA, USA | REF 21708318 | conductive paste |
| Heating plate | Medax; Kiel, Germany | 2005-205-01 | |
| Isoflurane | Abvie; Wiesbaden, Germany | n.a. | volatile anesthetic |
| Leukofix | BSN medical; Hamburg, Germany | REF 02137-00 | tape |
| Mechanical arm + micromanipulator | VisualSonics; FujiFilm, Toronto, CA | P/N 11277 | |
| Microbac tissues | Paul Hartmann AG; Hamburg, Germany | REF 981387 | antimicrobial tissues |
| MZ400, 38 MHz linear array transducer | VisualSonics; FujiFilm, Toronto, CA | REF 51068-30 | ultrasound transducer |
| Sonosid | ASID Bonz GmbH; Herrenberg, Germany | REF 782010 | ultrasonography gel |
| Ultrasound platform with heating plate and ECG-recording | VisualSonics; FujiFilm, Toronto, CA | P/N 11179 | |
| UniVet-Porta | Groppler; Oberperasberg, Germany | S/N BKGM0437 | isoflurane vaporizer |
| Vevo3100 | VisualSonics; FujiFilm, Toronto, CA | REF 51073-45 | ultrasonography device |
| VevoLab software | VisualSonics; FujiFilm, Toronto, CA | n.a. | evaluation software |
References
- Macdonald, R. L., Schweizer, T. A. Spontaneous subarachnoid haemorrhage. Lancet. 389 (10069), 655-666 (2017).
- Macdonald, R. L. Delayed neurological deterioration after subarachnoid haemorrhage. Nature Reviews Neurology. 10 (1), 44-58 (2014).
- Francoeur, C. L., Mayer, S. A. Management of delayed cerebral ischemia after subarachnoid hemorrhage. Critical Care. 20 (1), 277 (2016).
- van Lieshout, J. H., et al. An introduction to the pathophysiology of aneurysmal subarachnoid hemorrhage. Neurosurgical Review. , (2017).
- Altay, T., et al. A novel method for subarachnoid hemorrhage to induce vasospasm in mice. J Neurosci Methods. 183 (2), 136-140 (2009).
- Momin, E. N., et al. Controlled delivery of nitric oxide inhibits leukocyte migration and prevents vasospasm in haptoglobin 2-2 mice after subarachnoid hemorrhage. Neurosurgery. 65 (5), 937-945 (2009).
- Froehler, M. T., et al. Vasospasm after subarachnoid hemorrhage in haptoglobin 2-2 mice can be prevented with a glutathione peroxidase mimetic. Journal of Clinical Neuroscience. 17 (9), 1169-1172 (2010).
- Provencio, J. J., Altay, T., Smithason, S., Moore, S. K., Ransohoff, R. M. Depletion of Ly6G/C(+) cells ameliorates delayed cerebral vasospasm in subarachnoid hemorrhage. Journal of Neuroimmunology. 232 (1-2), 94-100 (2011).
- Kamp, M. A., et al. Evaluation of a murine single-blood-injection SAH model. PLoS One. 9 (12), 114946 (2014).
- Luh, C., et al. The Contractile Apparatus Is Essential for the Integrity of the Blood-Brain Barrier After Experimental Subarachnoid Hemorrhage. Translational Stroke Research. , (2018).
- Neulen, A., et al. A Volumetric Method for Quantification of Cerebral Vasospasm in a Murine Model of Subarachnoid Hemorrhage. Journal of Visualized Experiments. (137), (2018).
- Neulen, A., et al. Large Vessel Vasospasm Is Not Associated with Cerebral Cortical Hypoperfusion in a Murine Model of Subarachnoid Hemorrhage. Translational Stroke Research. , (2018).
- Neulen, A., et al. Neutrophils mediate early cerebral cortical hypoperfusion in a murine model of subarachnoid haemorrhage. Scientific Reports. 9 (1), 8460 (2019).
- Neulen, A., et al. Volumetric analysis of intracranial vessels: a novel tool for evaluation of cerebral vasospasm. Int J Comput Assist Radiol Surg. 14 (1), 157-167 (2019).
- Washington, C. W., Zipfel, G. J. Participants in the International Multi-disciplinary Consensus Conference on the Critical Care Management of Subarachnoid, H. Detection and monitoring of vasospasm and delayed cerebral ischemia: a review and assessment of the literature. NeuroCritical Care. 15 (2), 312-317 (2011).
- Greke, C., et al. Image-guided transcranial Doppler sonography for monitoring of defined segments of intracranial arteries. Journal of Neurosurgical Anesthesiology. 25 (1), 55-61 (2013).
- Neulen, A., Prokesch, E., Stein, M., Konig, J., Giese, A. Image-guided transcranial Doppler sonography for monitoring of vasospasm after subarachnoid hemorrhage. Clinical Neurology and Neurosurgery. 145, 14-18 (2016).
- Neulen, A., et al. Image-Guided Transcranial Doppler Ultrasound for Monitoring Posthemorrhagic Vasospasms of Infratentorial Arteries: A Feasibility Study. World Neurosurgery. 134, 284-291 (2020).
- Neulen, A., et al. Correlation of cardiac function and cerebral perfusion in a murine model of subarachnoid hemorrhage. Scientific Reports. 11 (1), 3317 (2021).
- Neulen, A., et al. A segmentation-based volumetric approach to localize and quantify cerebral vasospasm based on tomographic imaging data. PLoS One. 12 (2), 0172010 (2017).
- Marbacher, S., et al. Systematic Review of In Vivo Animal Models of Subarachnoid Hemorrhage: Species, Standard Parameters, and Outcomes. Translational Stroke Research. , (2018).
- Figueiredo, G., et al. Comparison of digital subtraction angiography, micro-computed tomography angiography and magnetic resonance angiography in the assessment of the cerebrovascular system in live mice. Clinical Neuroradiology. 22 (1), 21-28 (2012).
- Lindegaard, K. F., Nornes, H., Bakke, S. J., Sorteberg, W., Nakstad, P. Cerebral vasospasm diagnosis by means of angiography and blood velocity measurements. Acta Neurochirurgica. 100 (1-2), 12-24 (1989).
- Cassia, G. S., Faingold, R., Bernard, C., Sant’Anna, G. M. Neonatal hypoxic-ischemic injury: sonography and dynamic color Doppler sonography perfusion of the brain and abdomen with pathologic correlation. American Journal of Roentgenology. 199 (6), 743-752 (2012).
- Shen, Q., Stuart, J., Venkatesh, B., Wallace, J., Lipman, J. Inter observer variability of the transcranial Doppler ultrasound technique: impact of lack of practice on the accuracy of measurement. Journal of Clinical Monitoring and Computing. 15 (3-4), 179-184 (1999).

