Summary
To investigate the immune response to brain disorders, one common approach is to analyze changes in immune cells. Here, two simple and effective protocols are provided for isolating immune cells from murine brain tissue and skull bone marrow.
Abstract
Mounting evidence indicates that the immune response triggered by brain disorders (e.g., brain ischemia and autoimmune encephalomyelitis) occurs not only in the brain, but also in the skull. A key step toward analyzing changes in immune cell populations in both the brain and skull bone marrow after brain damage (e.g., stroke) is to obtain sufficient numbers of high-quality immune cells for downstream analyses. Here, two optimized protocols are provided for isolating immune cells from the brain and skull bone marrow. The advantages of both protocols are reflected in their simplicity, speed, and efficacy in yielding a large quantity of viable immune cells. These cells may be suitable for a range of downstream applications, such as cell sorting, flow cytometry, and transcriptomic analysis. To demonstrate the effectiveness of the protocols, immunophenotyping experiments were performed on stroke brains and normal brain skull bone marrow using flow cytometry analysis, and the results aligned with findings from published studies.
Introduction
The brain, the central hub of the nervous system, is protected by the skull. Beneath the skull are three layers of connective tissue known as the meninges – the dura mater, arachnoid mater, and pia mater. Cerebrospinal fluid (CSF) circulates in the subarachnoid space between the arachnoid mater and pia mater, cushioning the brain and also removing waste via the glymphatic system1,2. Together, this unique architecture provides a secure and supportive environment that maintains the stability of the brain and shields it from potential injury.
The brain has long been considered immune-privileged. However, this notion has been partially abandoned as mounting evidence indicates that, in addition to resident microglia in the parenchyma, the borders of the brain, including the choroid plexus and meninges, host a diverse array of immune cells3. These cells play critical roles in maintaining homeostasis, surveilling brain health, and initiating the immune response to brain injury. Notably, recent findings indicate that the skull is involved in meninges immunity, and may contribute to the immune response in the brain after injury. In 2018, Herisson et al. made a seminal discovery of direct vascular channels that link the skull bone marrow to the meninges, thereby establishing an anatomical route for leukocyte migration4,5. Later, Cugurra et al. demonstrated that many myeloid cells (e.g., monocytes and neutrophils) and B cells in the meninges do not originate from the blood6. Using techniques such as calvaria bone-flap transplantation and selective irradiation regimens, the authors provided compelling evidence that the skull bone marrow serves as a local source for myeloid cells in the meninges as well as CNS parenchyma after CNS injury6. Further, another study proposed that meningeal B cells are constantly supplied by the skull bone marrow7. More recently, a novel structure, termed the arachnoid cuff exit (ACE), has been identified as a direct gateway between the dura mater and the brain for immune cell trafficking8.
These exciting findings have important implications for the origin of infiltrating immune cells into the injured brain (e.g., after ischemic stroke). A large body of evidence has indicated that after stroke, many immune cells infiltrate the brain, contributing to both acute brain damage and chronic brain recovery. The conventional notion is that these cells are circulating leukocytes in the blood that infiltrate the brain, which is largely facilitated by stroke-induced blood-brain barrier damage. However, this notion has been challenged. In one study, immune cells in the skull and the tibia of mice were labeled differently, and at 6 h after stroke, a significantly greater decrease in neutrophils and monocytes was found in the skull vs. the tibia, and more skull-derived neutrophils were present in the ischemic brain. These data suggest that in the acute stroke phase, neutrophils in the ischemic brain primarily originate from the skull bone marrow4. Interestingly, CSF may guide this migration. Indeed, two recent reports demonstrated that CSF can directly relay signaling cues from the brain into the skull bone marrow via skull channels, and instruct cell migration and hematopoiesis in the skull bone marrow after CNS injury9,10.
In light of these recent findings, it has become important to analyze changes in immune cells in both the brain and the skull bone marrow, when studying the immune response to brain disorders. In such investigations, sufficient numbers of high-quality immune cells are needed for downstream analyses such as cell sorting, flow cytometry analysis, and single-cell RNA sequencing (scRNA-seq). Here, the overall goal is to present two optimized procedures for preparing single-cell suspensions from brain tissue and skull bone marrow. It is important to note that the calvaria (frontal bone, occipital bone, and parietal bones) of the skull are typically used to extract bone marrow, and this bone marrow is specifically referred to as skull bone marrow throughout this study.
Protocol
The protocol was approved by the Duke Institute Animal Care and Use Committee (IACUC). Male C57Bl/6 mice (3-4 months old; 22-28 g) were used in the current study. The details of the reagents and the equipment used are listed in the Table of Materials.
1. Single-cell suspension from mouse brain
NOTE: Figure 1 illustrates the overview of the brain cell isolation protocol.
- Anesthetize, intubate, and secure the mouse, as demonstrated previously11.
- Make an upper abdominal incision through the skin and underlying muscle layers, and carefully cut through the diaphragm and ribs to create the opening into the thoracic cavity.
- Fill a 30 mL syringe with cold PBS and attach it to the blunt perfusion needle via silicone tubing. Carefully insert the perfusion needle into the left ventricle.
- Perform a small nick at the right atrium to allow blood drainage and then perfuse12 the mouse at a flow rate of ~ 10 mL/min for 3-4 min.
NOTE: To improve blood clearance in the brain, increasing the volume of perfusion solution and adding heparin may be considered. - Decapitate the mouse and make a midline incision through the skin on the top of the head to expose the skull.
- Carefully scrape away any connective tissue overlying the skull using blunt forceps.
- Use sharp dissection scissors to carefully cut through the skull sutures along the midline and on both sides, creating a flap.
- Gently lift the skull flap to expose the brain, and use blunt forceps to carefully remove the brain from the cranial cavity.
- Immerse the brain in a Petri dish containing ice-cold PBS and remove any remaining meninge tissues.
NOTE: To better preserve cell viability, it is recommended to perform all following steps on ice or at 4 °C. - Place the brain in a pre-cooled 15 mL glass Dounce homogenizer containing 20 mL (whole brain) or 12 mL (half brain) of ice-old HBSS buffer.
- Use the loose Dounce pestle to gently and slowly dissociate the brain tissue with around 100-120 strokes on ice.
NOTE: This step is critical to obtaining a large quantity of healthy brain cells. This step takes approximately 10 min. Stop homogenization when no substantial brain tissue chunks are visible in the suspension. At this point, the pestle can easily move down without any force. - Filter the resulting brain tissue suspension through a 70 µm cell strainer in a 50 mL centrifuge tube.
- Rinse the Dounce tube with 5 mL HBSS, and proceed with filtration to maximize the cell collection.
- Centrifuge the filtered tissue suspension at 550 x g for 6 min at 4 °C.
- Remove the supernatant using a vacuum aspirator, and resuspend the cell pellet in 1 mL of 30% isotonic density gradient solution.
NOTE: To make 15 mL of 30% isotonic density gradient solution, mix 4.5 mL of 100% stock density gradient medium, 1.5 mL of 10× PBS, and 9 mL of ddH2O. - Transfer the cell suspension into a 15 mL centrifuge tube, and add 9 mL (whole brain) or 6 mL (half brain) of 30% density gradient solution.
- Gently invert the tube to ensure thorough mixing.
- Immediately centrifuge the tube at 845 x g with acceleration and brake set at level 3, for 20 min at 4 °C.
- Gently remove the tube from the centrifuge without shaking, and carefully aspirate the upper myelin layer using a 1 mL tip connected to the vacuum.
NOTE: It is critically important not to disturb this layer. Any remaining myelin can negatively impact cell health and compromise downstream analyses. - Aspirate the supernatant, leaving 1-2 mL behind, and resuspend the cell pellet with a minimum of 10 mL cold HBSS.
- Centrifuge at 550 x g for 6 min at 4 °C.
- Wash one more time with a minimum of 7 mL of cold HBSS.
- Remove as much of the supernatant as possible, and resuspend the cells for flow cytometry analysis using 100-200 µL of flow cytometry buffer.
NOTE: The flow cytometry FACS buffer used for this study contains 0.5% BSA and 2 mM EDTA in 1× PBS. A 96-well V-bottom plate for cell staining is recommended to minimize cell loss during the washing steps. - Perform flow cytometry analysis using a standard protocol established in individual laboratories13.
- Briefly, mix 80 µL of cell suspension with 20 µL of the antibody mixture in a 96-well V-bottom plate and incubate for 25 min at 4 °C.
- Wash with 200 µL of FACS buffer and then resuspend the cells with 100 µL of HBSS plus cell viability staining reagent.
- After a 15 min incubation at 4 °C, wash with FACS buffer and resuspend the cells in 200 µL of FACS buffer for flow cytometry analysis.
2. Preparation of bone marrow single-cell suspension from mouse calvaria
NOTE: Figure 2 depicts the overview of the skull bone marrow isolation procedure.
- Perfuse the mouse as described in step 1.4.
- Decapitate the mouse and make a midline skin incision on the scalp to expose the skull.
- Cut through the skull, starting from the foramen magnum and moving forward along the lateral sides of the calvaria using sharp scissors. Then, lift and remove the calvaria.
NOTE: The brain can be harvested from the same mouse and processed using step 1, enabling analysis of immune cells from both the brain and skull bone marrow. - Carefully peel off the dura mater from the skull under a dissecting microscope using blunt forceps.
NOTE: It is easier to start at the edges of the occipital bone, slowly detach, and progress steadily towards the frontal area, working inward. - Place the calvaria in the dish on ice and use a 1 mL pipette to rinse the calvaria, ensuring the removal of blood residues from its surface.
- Transfer the calvaria to a new dish with fresh, cold PBS sufficient to immerse the calvaria.
- Use sterile scissors to cut the calvaria into approximately 3 mm x 3 mm fragments in cold PBS.
NOTE: Cropping methods may affect the efficiency of calvaria bone marrow extraction. It is recommended that the same cropping method be used to minimize variability. It is also important to cut open the sutures. Figure 2B illustrates one approach. - Poke a hole in the bottom of a 500 µL microcentrifuge tube using an 18 G needle.
- Insert this tube into a 1.5 mL microcentrifuge tube containing 20 µL of cold PBS.
- Transfer the calvaria fragments into the 500 µL tube.
NOTE: The bone fragments should be loosely packed to increase extraction efficiency. - Centrifuge at 10,000 x g for 30 s at 4 °C.
NOTE: To maximize cell recovery, use an 18 G needle to gently stir the calvaria fragments, and repeat this step 1-2 more times. - Resuspend the collected calvaria bone marrow cells in 500 µL of Red Blood Cell lysis buffer and incubate at room temperature for 30 s.
- Transfer the suspension to a 15 mL centrifuge tube containing 4 mL of cold PBS.
- Centrifuge at 400 x g for 6 min at 4 °C.
- Wash one more time with 5 mL of cold PBS.
- Resuspend the cell pellet in an appropriate buffer. For flow cytometry, we typically use 500 µL of FACS buffer.
- For flow cytometry analysis, perform cell counting and use approximately 1 x 106 cells for antibody staining.
NOTE: Ensure to include the Fc block step before antibody staining13.
Representative Results
To prepare immune cells from the mouse brain tissue, the protocol generally yields cells with high viability (84.1% ± 2.3% [mean ± SD]). Approximately 70%-80% of these cells are CD45 positive. In the normal mouse brain, nearly all CD45+ cells are microglia (CD45LowCD11b+), as expected. This protocol has been used in the laboratory for various applications, including flow cytometry analysis, fluorescence-activated cell sorting (FACS), and scRNA-seq analysis. As an example, a flow cytometry analysis was conducted in a stroke model (Figure 3). Mice were subjected to a transient stroke model, 30 min filament middle cerebral artery occlusion (MCAO)14. On day 3 after stroke, cells were prepared from mouse brains and stained with common immune cell surface markers. The gating strategy is depicted in Figure 3A. Consistent with prior research13,15, a marked increase in CD45High cells in the ipsilateral hemisphere was observed (Figure 3B,C), indicating infiltration of the immune cell into the brain.
For the skull bone marrow protocol, a substantial yield of skull bone marrow cells (around 2 x 106 cells) was consistently achieved with excellent viability (93.8% ± 1.8% [mean ± SD]). As expected, most of these cells are CD45 positive. To illustrate the utility of this protocol, a comparative study was performed to characterize the immune cell composition in both the femur and skull bone marrow of naive mice (Figure 4). As depicted in the representative plots, the immune cell composition was similar between the femur and skull bone marrow (Figure 4A,B). Interestingly, the frequency of neutrophils appears to be higher in the femur than in the skull bone (Figure 4C). However, this finding requires further validation, as the sample size was small for this pilot study.
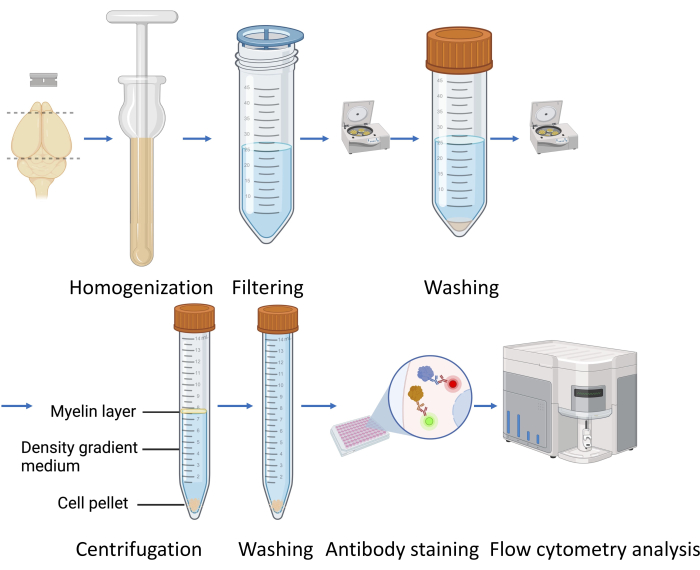
Figure 1: Overview of the brain cell isolation protocol. Please click here to view a larger version of this figure.
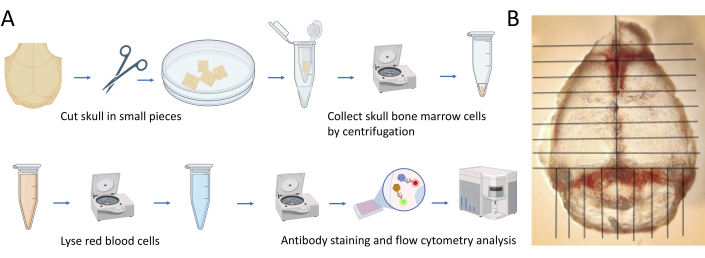
Figure 2: The skull bone marrow cell isolation protocol. (A) Overview of the procedure. (B) The recommended pattern for skull cutting. Please click here to view a larger version of this figure.
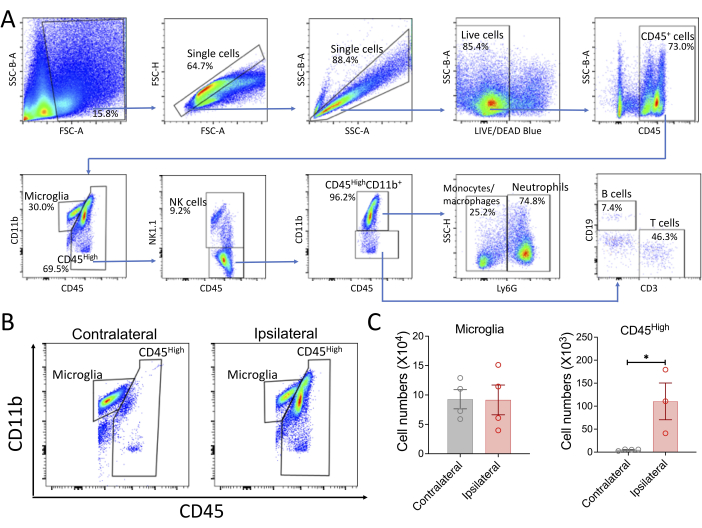
Figure 3: Representative flow cytometry analysis of the immune cells in the stroke brain. (A) An example of the gating strategy. The plots depict the following immune cell populations: microglia (CD45LowCD11b+), NK cells (CD45HighNK1.1+), neutrophils (CD45HighLy6G+), T cells (CD45HighCD11b–CD3+), and B cells (CD45HighCD11b–CD19+). This example represents an analysis of brain immune cells in the ipsilateral hemisphere on day 3 after stroke. (B,C) Infiltrating immune cells into the stroke brain. Young male mice were subjected to transient middle cerebral artery occlusion (MCAO). On day 3, brains were collected and split into left (contralateral) and right (ipsilateral) hemispheres. Brain cells were prepared according to the described protocol and then subjected to flow cytometry analysis. Representative plots illustrate increased infiltrating immune cells into the ipsilateral hemisphere (CD45High cells; B). Quantitative data are shown in the bar graphs (C). The cell numbers were calculated based on the cell count and volume recorded in the flow cytometry data. The data are presented as mean ± SEM. *p < 0.05. Please click here to view a larger version of this figure.
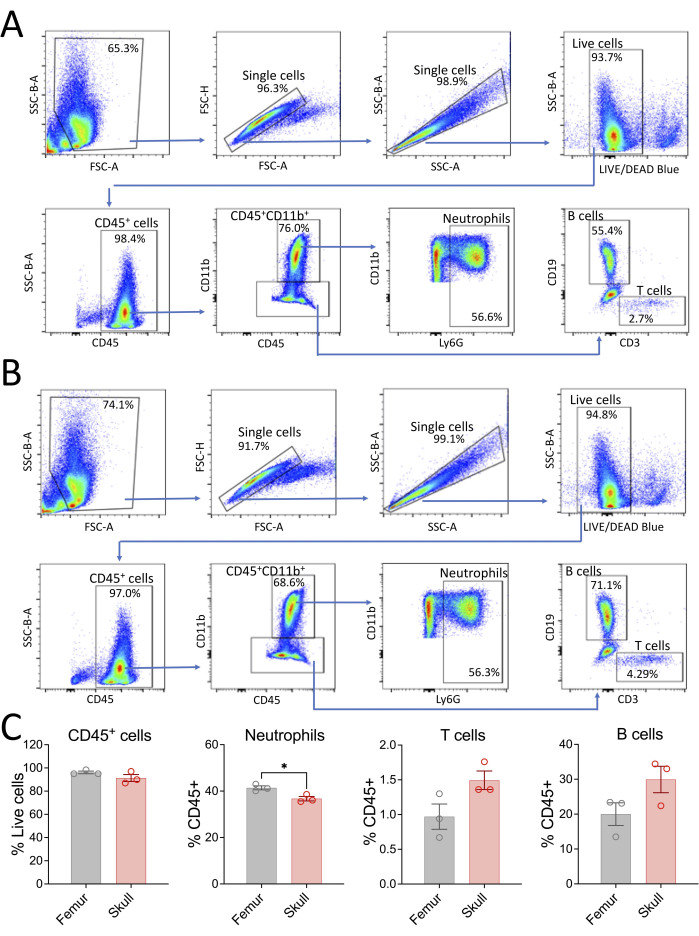
Figure 4: Representative flow cytometry analysis of the skull bone marrow cells. For comparison, analysis of bone marrow cells from the femur was included. The plots depict the following immune cell populations: NK cells (CD45+NK1.1+), neutrophils (CD45+CD11b+Ly6G+), T cells (CD45+CD11b–CD3+), and B cells (CD45+CD11b–CD19+). (A) Representative plots for femur bone marrow. (B) Representative plots for skull bone marrow. (C) Comparison of the immune cell composition between femur and skull bone marrow. The data are presented as mean ± SEM. *p < 0.05. Please click here to view a larger version of this figure.
Discussion
Here, two simple yet effective protocols are presented for isolating immune cells from the brain and skull bone marrow. These protocols can reliably yield a large quantity of viable immune cells that may be suitable for diverse downstream applications, in particular for flow cytometry.
To study neuroinflammation in various brain disorders, many protocols for immune cell preparations from the brain have been established and used in different laboratories15,16,17. The common approaches involve enzyme-based cell dissociation followed by gradient separation. Typically, in these protocols, brain tissue is minced and then incubated in an enzyme digestion solution containing both collagenase and DNase for 30-60 min at 37 °C with gentle shaking. After digestion, cells undergo further dissociation using a mechanical method such as pipetting or Dounce homogenization. After passing through a cell strainer (e.g., 70 µm strainer), cells are then subjected to gradient centrifugation (often 30%/70% density gradient solution) to remove myelin, red blood cells, and debris and to enrich leukocytes. However, this approach requires a prolonged enzymatic incubation at 37 °C that may substantially alter the transcriptome and proteome of brain immune cells. Indeed, a systematic investigation suggested that the enzymatic approach introduces profound alterations in the transcriptome and proteotype of specific brain cells18. This could lead to artifacts in subsequent transcriptomic analyses such as scRNA-seq. In contrast, the protocol reported here uses a mechanical dissociation approach at cold temperatures throughout the procedure, thus suppressing cellular metabolism. This ensures better preservation of the transcriptional and proteomic state, minimizing potential artifacts. During protocol development, we noticed that using a large Dounce homogenizer for homogenizing brain tissue is critical to achieving higher cell counts with lower cell death. It is likely that during Dounce homogenization, the massive presence of extracellular matrices, cell debris, and cytoplasmic components is toxic to cells. Using an excessive amount of buffer helps to dilute these toxic substances and, thus, mitigates their harmful effects, leading to better cell viability. The flow cytometry data confirmed an approximate 85% viability rate of immune cells prepared with this protocol. Moreover, it is notable that centrifugation with only a 30% density gradient solution effectively enriches brain immune cells and removes myelin. This can also reduce the cost of cell preparation.
Studies on immune cells in the skull bone marrow are still limited. A method commonly used to isolate cells from the mouse skull calvarium involves cutting the skull into small pieces and then mechanically crushing the pieces with a pestle6. In the current protocol, brief centrifugation is used. This method is adapted from a published protocol for preparing bone marrow from femurs and tibias19. For these long bones, one needs only to cut off one end of the bone to collect bone marrow by centrifugation. For the skull, this step is modified by cutting it into several small pieces to open the marrow cavity. It is recommended to use a consistent pattern for cutting the skull in order to obtain reproducible cell counts. Moreover, to maximize the recovery of bone marrow cells, the skull pieces can undergo 2-3 rounds of centrifugation with mixing between each centrifugation.
Both protocols have limitations. First, the use of 30% density gradient solution centrifugation may not effectively remove the remaining red blood cells in the brain, which may occur due to incomplete perfusion. Moreover, if myelin structure is modulated under certain conditions, a 30% density gradient solution may not be an optimal concentration for their removal. In this case, another working concentration of density gradient solution needs to be established. Second, although flow cytometry analysis indicates good cell viability of the brain immune cells using the described protocol, it still needs to be evaluated for other applications, such as transcriptomic analysis in which actinomycin D may be used. Third, the calvaria is used to prepare skull bone marrow. However, it must be noted that immune cells exist in many other parts of the skull. Lastly, the meninges, especially the dura mater, harbor diverse immune cells and play roles in brain homeostasis and dysfunction20. For immune analysis of the meninges, a protocol published elsewhere may be adopted17,21,22,23.
In summary, two robust protocols for isolating immune cells from both the mouse brain and skull are described. These protocols are expected to be useful for obtaining a large quantity of high-quality cells, suitable for various downstream applications.
Disclosures
The authors have nothing to disclose.
Acknowledgements
We thank Kathy Gage for her excellent editorial contribution. The illustration figures were created with BioRender.com. This study was supported by funds from the Department of Anesthesiology (Duke University Medical Center) and NIH grants NS099590, HL157354, and NS127163.
Materials
| 0.5 mL microcentrifuge tubes | VWR | 76332-066 | |
| 1.5 mL microcentrifuge tubes | VWR | 76332-068 | |
| 15 mL conical tubes | Thermo Fisher Scientific | 339651 | |
| 18 G x 1 in BD PrecisionGlide Needle | BD Biosciences | 305195 | |
| 1x HBSS | Gibco | 14175-095 | |
| 50 mL conical tubes | Thermo Fisher Scientific | 339653 | |
| 96-well V-bottom microplate | SARSTEDT | 82.1583 | |
| AURORA flow cytometer | Cytek bioscience | ||
| BSA | Fisher | BP9706-100 | |
| CD11b-AF594 | BioLegend | 101254 | 1:500 dilution |
| CD19-BV785 | BioLegend | 115543 | 1:500 dilution |
| CD19-FITC | BioLegend | 115506 | 1:500 dilution |
| CD3-APC | BioLegend | 100312 | 1:500 dilution |
| CD3-PE | BioLegend | 100206 | 1:500 dilution |
| CD45-Alex 700 | BioLegend | 103128 | 1:500 dilution |
| CD45-BV421 | Biolegend | 103133 | 1:500 dilution |
| Cell Strainer 70 um | Avantor | 732-2758 | |
| Dressing Forceps | V. Mueller | NL1410 | |
| EDTA | Invitrogen | 15575-038 | |
| Fc Block | Biolegend | 101320 | 1:100 dilution |
| Forceps | Roboz | RS-5047 | |
| LIVE/DEAD Fixable Blue Dead Cell Stain Kit | Thermo Fisher Scientific | N7167 | 1:500 dilution |
| Ly6G-BV421 | BioLegend | 127628 | 1:500 dilution |
| Ly6G-PerCp-cy5.5 | BioLegend | 127615 | 1:500 dilution |
| NK1.1-APC-cy7 | BioLegend | 108723 | 1:500 dilution |
| Percoll (density gradient medium) | Cytiva | 17089101 | |
| Phosphate buffer saline (10x) | Gibco | 70011-044 | |
| RBC Lysis Buffer (10x) | BioLegend | 420302 | |
| Scissors | SKLAR | 64-1250 | |
| WHEATON Dounce Tissue, 15 mL Size | DWK Life Sciences | 357544 |
References
- Bohr, T., et al. The glymphatic system: Current understanding and modeling. iScience. 25 (9), 104987 (2022).
- Jiang-Xie, L. F., et al. Neuronal dynamics direct cerebrospinal fluid perfusion and brain clearance. Nature. 627 (8002), 157-164 (2024).
- Goertz, J. E., Garcia-Bonilla, L., Iadecola, C., Anrather, J. Immune compartments at the brain’s borders in health and neurovascular diseases. Semin Immunopathol. 45 (3), 437-449 (2023).
- Herisson, F., et al. Direct vascular channels connect skull bone marrow and the brain surface enabling myeloid cell migration. Nat Neurosci. 21 (9), 1209-1217 (2018).
- Mazzitelli, J. A., et al. Skull bone marrow channels as immune gateways to the central nervous system. Nat Neurosci. 26 (12), 2052-2062 (2023).
- Cugurra, A., et al. Skull and vertebral bone marrow are myeloid cell reservoirs for the meninges and CNS parenchyma. Science. 373 (6553), eabf7844 (2021).
- Brioschi, S., et al. Heterogeneity of meningeal b cells reveals a lymphopoietic niche at the CNS borders. Science. 373 (6553), eabf9277 (2021).
- Smyth, L. C. D., et al. Identification of direct connections between the dura and the brain. Nature. 627, 165-173 (2024).
- Mazzitelli, J. A., et al. Cerebrospinal fluid regulates skull bone marrow niches via direct access through dural channels. Nat Neurosci. 25 (5), 555-560 (2022).
- Pulous, F. E., et al. Cerebrospinal fluid can exit into the skull bone marrow and instruct cranial hematopoiesis in mice with bacterial meningitis. Nat Neurosci. 25 (5), 567-576 (2022).
- Li, R., et al. Mouse cardiac arrest model for brain imaging and brain physiology monitoring during ischemia and resuscitation. J Vis Exp. (194), e65340 (2023).
- Wang, W., et al. Development and evaluation of a novel mouse model of asphyxial cardiac arrest revealed severely impaired lymphopoiesis after resuscitation. J Am Heart Assoc. 10 (11), e019142 (2021).
- Li, X., et al. Single-cell transcriptomic analysis of the immune cell landscape in the aged mouse brain after ischemic stroke. J Neuroinflammation. 19 (1), 83 (2022).
- Wang, Y. C., et al. Perk (protein kinase RNA-like er kinase) branch of the unfolded protein response confers neuroprotection in ischemic stroke by suppressing protein synthesis. Stroke. 51 (5), 1570-1577 (2020).
- Posel, C., Moller, K., Boltze, J., Wagner, D. C., Weise, G. Isolation and flow cytometric analysis of immune cells from the ischemic mouse brain. J Vis Exp. 108, e53658 (2016).
- Srakocic, S., et al. Proposed practical protocol for flow cytometry analysis of microglia from the healthy adult mouse brain: Systematic review and isolation methods’ evaluation. Front Cell Neurosci. 16, 1017976 (2022).
- Disano, K. D., et al. Isolating central nervous system tissues and associated meninges for the downstream analysis of immune cells. J Vis Exp. 159, e61166 (2020).
- Mattei, D., et al. Enzymatic dissociation induces transcriptional and proteotype bias in brain cell populations. Int J Mol Sci. 21 (21), (2020).
- Mcgill, C. J., Lu, R. J., Benayoun, B. A. Protocol for analysis of mouse neutrophil netosis by flow cytometry. STAR Protoc. 2 (4), 100948 (2021).
- Su, Y., et al. Meningeal immunity and neurological diseases: New approaches, new insights. J Neuroinflammation. 20 (1), 125 (2023).
- Niu, C., et al. Mechanical isolation of neonatal and adult mouse dura leukocytes for flow cytometry analysis. STAR Protoc. 4 (2), 102272 (2023).
- Roussel-Queval, A., Rebejac, J., Eme-Scolan, E., Paroutaud, L. A., Rua, R. Flow cytometry and immunohistochemistry of the mouse dural meninges for immunological and virological assessments. STAR Protoc. 4 (1), 102119 (2023).
- Louveau, A., Filiano, A. J., Kipnis, J. Meningeal whole mount preparation and characterization of neural cells by flow cytometry. Curr Protoc Immunol. 121 (1), e50 (2018).

