Measurement of Healthy and Injured Triceps Surae Morphology
Instructor Prep
concepts
Student Protocol
The following protocol follows the guidelines set forth by and has been approved by the University Institutional Review Board to ensure safe and ethical human subject research. All subjects provided informed consent for participation in the research studies and dissemination of data. The full protocol takes approximately 20 minutes to perform by a trained sonographer. However, individual measurements may be taken per assessment need.
1. Marking of the skin
- Ask the participant to be seated at the end of a plinth with their legs hanging off the table.
- Palpate and mark the medial tibial plateau and most distal aspect of the medial malleolus bilaterally. Measure the distance between the ipsilateral markings to determine tibial length.
- Calculate 25% of the tibial length. Measure and mark this distance, distal from the medial tibial plateau, to indicate the location for gastrocnemius measurements (Figure 1).
- Calculate 30% of the tibial length. Measure and mark this distance, proximal from the most distal aspect of the medial malleolus, to indicate the location for soleus measurements (Figure 1).
- Record the 25% and 30% tibial length for longitudinally measuring the same location during future evaluations.
- Ask the participant to move into a prone position on the plinth with the knees fully extended and their feet hanging relaxed off the edge of the plinth with ankles in a resting position (Figure 2).
- Transfer the gastrocnemius and soleus markings to the posterior aspect of the lower leg. Palpate and mark the midpoint of the gastrocnemius (the distal most point between the two muscle bellies). Ask the participant to gently plantarflex against manual resistance to palpate this location.
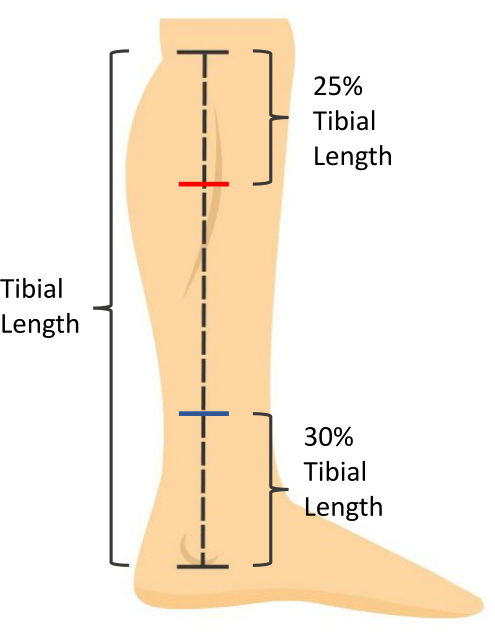
Figure 1: Skin measurement markings. Tibial length is measured as the distance from the medial tibial plateau to the most distal aspect of the medial malleolus. Soleus muscle thickness is measured at 30% of the tibial length proximal to the most distal aspect of the medial malleolus (blue mark). Gastrocnemius muscle CSA is measured at 25% of the tibial length distal to the medial tibial plateau (red mark). Please click here to view a larger version of this figure.

Figure 2: Participant positioning for ultrasound imaging. The participant is prone with knees fully extended and feet hanging relaxed in a resting ankle position off the edge of the plinth. Please click here to view a larger version of this figure.
2. Ultrasound imaging
NOTE: All images will be taken on both legs. All images should be taken along the midline of the Achilles tendon. Use palpation of the medial and lateral borders of the Achilles tendon to determine midline location.
- Use B-mode ultrasound with a 5 cm linear array transducer with parameters set for visualization of the triceps surae. Set frequency to 10 MHz and depth of measurement to 3.5 cm for visualization. Adjust the foci between 0.75 cm and 1.75 cm with gain adjusted to 49 for optimal visualization of tissue.
NOTE: Depth, foci, and gain may be adjusted as appropriate for visualization. - Place ultrasound gel on the posterior calcaneus. Holding the probe on the long axis, visualize the proximal calcaneal notch and align the notch with the midpoint of the ultrasound probe. Mark this location on the skin (Figure 3).
- Marking the skin for measurement of Achilles tendon thickness and CSA will vary depending on the participant. Use the following guidelines to determine this position.
- For healthy individuals, measure 2 cm proximal from the proximal calcaneal notch and mark this location on the skin.
- For individuals with Achilles tendinopathy, visualize the thickest portion of the Achilles tendon with the ultrasound probe on the long axis and mark this location on the skin. Record the distance of this marking from the proximal calcaneal notch forlongitudinally measuring the same location during future evaluations.
- For individuals with Achilles tendinopathy without visible fusiform thickening, mark the skin at the location of most tendon pain upon palpation. Record the distance of this marking from the proximal calcaneal notch for longitudinally measuring the same location during future evaluations.
- For individuals post Achilles tendon rupture, visualize the location of rupture with the ultrasound probe in the long axis and mark this location on the skin. Record the distance of this marking from the proximal calcaneal notch for longitudinally measuring the same location during future evaluations.
- For the uninvolved limb, make the skin marking at the same distance from the proximal calcaneal notch as the involved limb.
- Gastrocnemius tendon length (Full tendon length): Using an extended field-of-view and holding the probe on the long axis, begin the image at the calcaneus by visualizing the Achilles tendon insertion. Glide the probe proximally along the midline of the Achilles tendon towards the mark at the gastrocnemius midpoint until the myotendinous junction is visualized. This will end the image. Take three images of the Achilles' full tendon length (Figure 4).
- Soleus tendon length (Free tendon length): Using an extended field-of-view and holding the probe on the long axis, begin the image at the calcaneus by visualizing the Achilles tendon insertion. Glide the probe proximally along the midline of the Achilles tendon towards the mark at the soleus until the soleus myotendinous junction is visualized. Take three images of the Achilles' free tendon length.
- Achilles tendon thickness: Using the B-mode view, place the probe on the long axis on the skin marking made for Achilles tendon thickness and CSA (step 2.3). Take three images of Achilles tendon thickness.
- Achilles tendon cross-sectional area: Using the B-mode view, place a gel standoff pad on the skin marking made for Achilles tendon thickness and CSA (step 2.3). Holding the probe on the short axis, take three images of the Achilles tendon cross-section.
NOTE: Tendon is of an anisotropic quality; depending on the angle of the sound waves, it will reflect back, making it look bright, or reflect away, making it look dark (Figure 5). Therefore, toggling the probe back and forth will help with visualizing the border of the tendon. - Soleus thickness: Using the B-mode view, place the probe on the long axis on the skin marking made for the soleus (30% of the tibial length from the distal aspect of the medial malleolus). Visualize the anterior border of the soleus muscle. Take three images for soleus thickness19.
- To distinguish between the soleus and flexor hallucis longus, have the participant actively flex and extend the great toe. This will cause movement of the fibers of the flexor hallucis longus without moving the soleus fibers.
- Gastrocnemius cross-sectional area: Using an extended field-of-view, hold the ultrasound probe on the short axis and in line with the mark for the gastrocnemius (25% of the tibial length from the medial tibial plateau). Visualize the medial border of the medial gastrocnemius and begin the image by gliding the probe from medial to lateral until the lateral border of the lateral gastrocnemius is visualized. Take three images for gastrocnemius CSA13.
- To capture the most medial aspect of the medial gastrocnemius it may be needed to ask the participant to abduct their legs and internally rotate the hip slightly. If this is required, ensure the participant is not plantarflexing their foot, as this will impact measurements.
- Using the B-mode view, determine the presence or absence of calcifications within the Achilles tendon (Figure 6D) and/or at the Achilles tendon insertion (enthesis; Figure 6C). These calcifications are unattached from the calcaneus and appear as hyperechoic areas with a shadow below, present in multiple planes of view. Take an image to confirm the findings. Note whether the calcifications occur within the Achilles tendon or at the enthesis.
- Using the B-mode view, determine the presence or absence of bursitis. This is visualized by a hypoechoic area deep to the Achilles tendon at the proximal calcaneus (retrocalcaneal bursitis) and/or superficial to the Achilles tendon insertion (subcutaneous calcaneal bursitis). Take an image to confirm the findings (Figure 6B).
- Using the Doppler setting on the ultrasound, assess for the presence or absence of neovascularization within the Achilles tendon.
- Position the Doppler box (i.e., region of interest) on the tendon, hold the ultrasound probe still, and avoid pressing down or distending the tissue as this may occlude and prevent visualization of blood flow.
- Scan the length of the Achilles free tendon, being sure to assess each portion of the tendon without movement of the probe to prevent artifact. If there is vasculature visible within or in contact with the tendon, take three, 3 s videos in the region with maximal blood flow (Figure 6A).
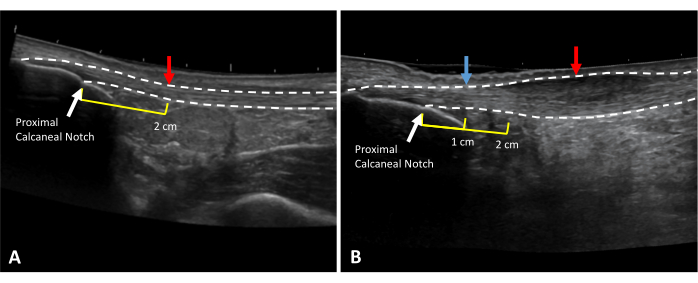
Figure 3: Achilles tendon thickness and CSA measurement locations. Extended field of view ultrasound images of (A) a healthy and (B) tendinopathic Achilles tendon. Dotted lines indicate tendon borders. Red arrows indicate measurement locations. Yellow lines indicate the distance proximal to the proximal calcaneal notch (white arrow). In the case of thickening at the 2 cm mark (B), healthy tendon thickness should be taken at a healthy area in the free tendon (blue arrow). Please click here to view a larger version of this figure.
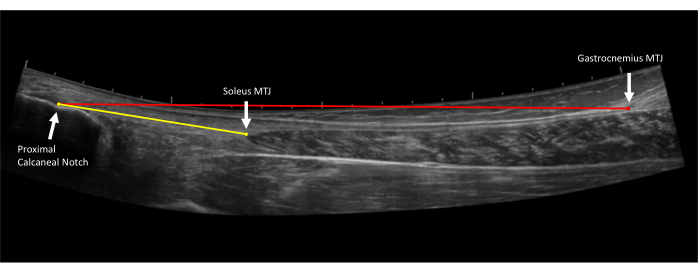
Figure 4: Achilles tendon length measurements. Extended field of view ultrasound image of the Achilles tendon. Free tendon length (yellow line) is measured from the proximal Achilles tendon insertion on the proximal calcaneal notch to the soleus myotendinous junction (MTJ). Full tendon length (red line) is measured from the proximal Achilles tendon insertion on the proximal calcaneal notch to the gastrocnemius myotendinous junction (MTJ)10. Please click here to view a larger version of this figure.
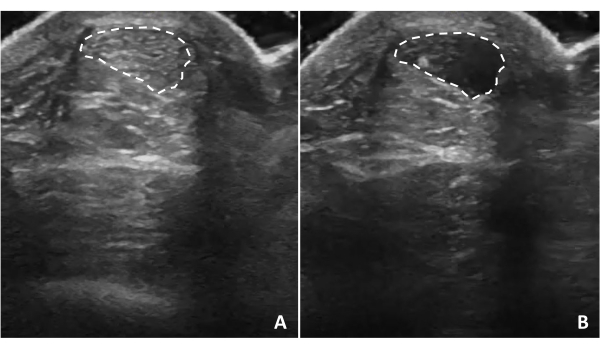
Figure 5: Tendon anisotropy. Achilles tendon anisotropy occurs when the ultrasound waves are not perpendicular to the structure. Tilting the ultrasound probe will cause the tendon structure to appear (A) hyperechoic or (B) hypoechoic depending on the relationship of ultrasound waves to the tendon. Dotted lines indicate tendon borders. Please click here to view a larger version of this figure.
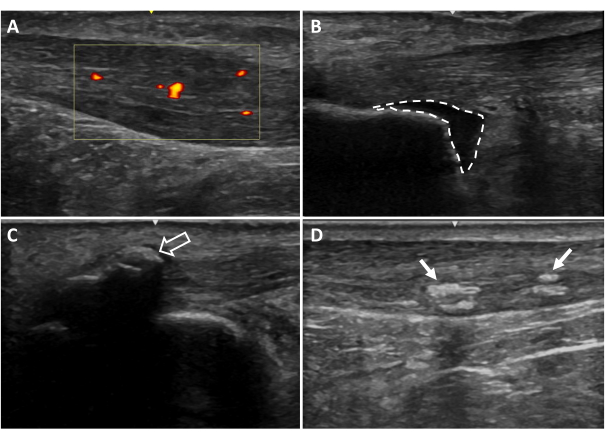
Figure 6: Additional ultrasound imaging findings. (A) Neovascularization, (B) retrocalcaneal bursitis, (C) entheseal calcifications, (D) intratendinous calcifications. Areas colored red and yellow indicate blood flow within the tendon region of interest (yellow box). Dotted lines indicate bursa borders. Arrows indicate calcifications20. Please click here to view a larger version of this figure.
3. Ultrasound measurements
NOTE: Ultrasound measurements can be made on the machine based on the settings and tools for the respective ultrasound machine. Images can also be exported for taking measurements on software such as Osirix DICOM viewer. The average of the three trials for each measure will be used for analysis.
- Gastrocnemius tendon length (full tendon length): Open the longer extended field-of-view tendon image (taken in step 2.4). Measure from the most proximal point of the tendon insertion (proximal calcaneal notch) to the gastrocnemius myotendinous junction (Figure 4).
- Soleus tendon length (free tendon length): Open the shorter extended field-of-view tendon image (taken in step 2.5). Measure from the most proximal point of the tendon insertion (proximal calcaneal notch) to the soleus myotendinous junction (Figure 4).
- Tendon thickness at 2 cm: Open the shoter extended field-of-view tendon image. Measure from the most proximal point of the tendon insertion (proximal calcaneal notch) to 2 cm, with the end of the measurement on the deep border of the tendon. Measure from this point on the deep border of the tendon to the direct superficial aspect of the tendon to get the 2 cm tendon thickness. This measure should represent healthy tendon thickness (Figure 7A).
- In the case of Achilles tendinopathy, if the tendon is thickened at this 2 cm distance, locate a healthy area in the free tendon to take this measurement and document the distance from the proximal calcaneal notch (Figure 7B).
NOTE: Thickness is used to describe the raw thickness of the tendon from the most superficial to deep.
- In the case of Achilles tendinopathy, if the tendon is thickened at this 2 cm distance, locate a healthy area in the free tendon to take this measurement and document the distance from the proximal calcaneal notch (Figure 7B).
- Tendon cross-sectional area: Open image taken in step 2.7. Visually identify the borders of the Achilles tendon and outline the circumference of the tendon (Figure 8A).
- Tendon thickness: Open image taken in step 2.6. At the center of the image, measure the Achilles tendon from the superficial border to the deep border of the tendon (Figure 8B).
- Soleus thickness: Open image taken in step 2.8. At the center of the image, measure from the superficial border to the deep border of the soleus muscle (Figure 9).
- Gastrocnemius cross-sectional area: Open image taken in step 2.9. Visualize the borders of both the medial and lateral heads of the gastrocnemius and outline the medial gastrocnemius and then the lateral gastrocnemius heads (Figure 10).
- Achilles tendon thickening: Use this calculation to determine the degree of thickening of the tendon in Achilles tendinopathy. Subtract thickness at 2 cm (or adjusted location; Figure 7A) from tendon thickness (Figure 7B) to obtain tendon thickening (measurement in step 3.5 minus measurement in step 3.3).
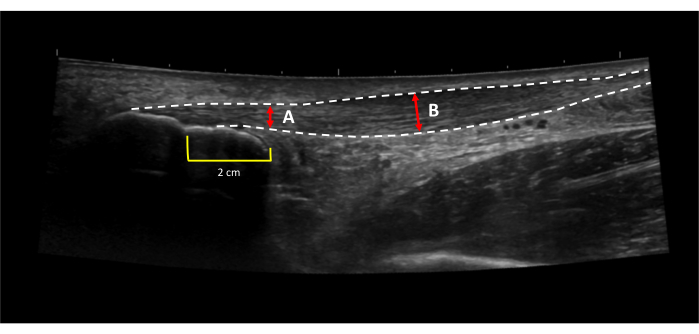
Figure 7: Achilles tendon thickening. Achilles tendon thickening is calculated by subtracting (A) the thickness of the healthy portion of the tendon from (B) the thickness of the thickest portion of the tendon31. Dotted lines indicate tendon borders. Red lines indicate tendon thickness. Yellow lines indicated a 2 cm distance proximal to the proximal calcaneal notch. Please click here to view a larger version of this figure.
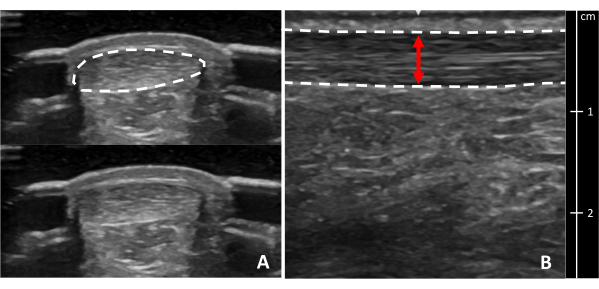
Figure 8: Achilles tendon cross-sectional area and thickness. Ultrasound images of the Achilles tendon in (A) cross-section and (B) longitudinal view at the thickest portion. Dotted lines indicate tendon borders. The red line indicates tendon thickness. A cross-section of the tendon is shown with and without a border for clarity. Please click here to view a larger version of this figure.
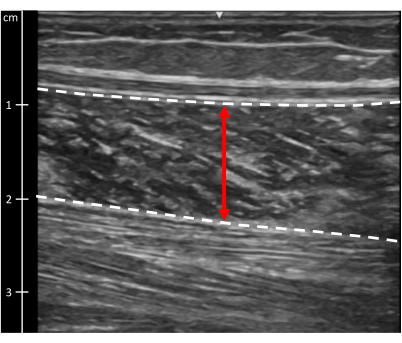
Figure 9: Soleus muscle thickness. Ultrasound image of the soleus muscle. Dotted lines indicate muscle borders. The red line indicates muscle thickness. Please click here to view a larger version of this figure.
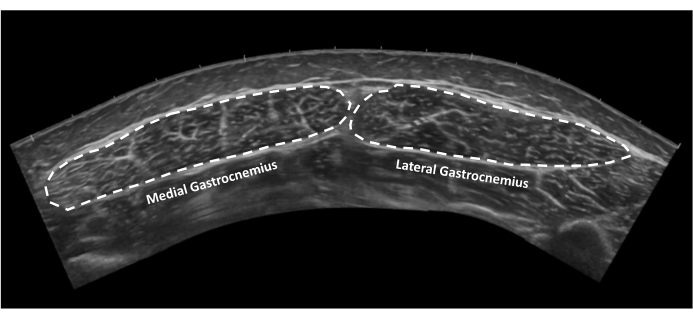
Figure 10: Gastrocnemius muscle cross-sectional area. Extended field of view ultrasound image of medial and lateral gastrocnemius muscles in cross-section. Dotted lines indicate tendon borders. Please click here to view a larger version of this figure.
Measurement of Healthy and Injured Triceps Surae Morphology
Learning Objectives
The measures in this protocol have been demonstrated to be reliable and valid10,20. Excellent reliability has been reported for extended field-of-view Achilles tendon length to gastrocnemius (interclass correlation coefficient (ICC): 0.944) and Achilles tendon length to soleus (ICC: 0.898)10. The minimal detectable change at the group level (MDCgroup) for Achilles tendon length measures is 0.43 cm for length to gastrocnemius and 0.41 cm for length to soleus. The MDC at the individual level (MDCindividual) is 1.83 cm for length to gastrocnemius and 1.73 cm for length to soleus10. Further, comparison between Achilles tendon length measures assessed via extended field-of-view ultrasound imaging and physical measurements on cadaver specimens reveals excellent validity for length to gastrocnemius (ICC: 0.895) and moderate to good validity for length to soleus (ICC:0.744)10. Excellent reliability has also been established for Achilles tendon thickness (ICC: 0.898)10 and Achilles tendon CSA measures (ICC: 0.986)20 with a MDCgroup of 0.007 cm for thickness (MDCindividual=0.03 cm) and 0.009 cm2 for CSA21.
Previously, Park et al. established the reliability and validity of anatomical CSA of the gastrocnemius muscles using ultrasound imaging13. Triceps surae muscle ultrasound imaging measures have also been established as reliable. In a sample of 10 health participants, excellent reliability was calculated for medial (ICC: 0.988, MDCgroup: 0.305 cm2, MDCindividual: 0.964 cm2) and lateral (ICC: 0.838, MDCgroup: 0.605 cm2, MDCindividual: 1.91 cm2) gastrocnemius CSA. In the same healthy sample, soleus thickness was found to have good reliability (ICC: 0.787, MDCgroup: 0.093 cm, MDCindividual: 0.293 cm).
Representative results are presented with data from healthy participants (Delaware, USA), participants with Achilles tendinopathy (Delaware, USA), and participants 6 months post Achilles tendon rupture (Delaware, USA and Stockholm, Sweden; Table 1). It is also important to note the demographic differences between groups (Table 2). Consistent with published literature, the sample of individuals post Achilles tendon rupture has a greater proportion of males to females, whereas the individuals with Achilles tendinopathy are closer to an even distribution of males and females22,23. Additionally, in this data set, the healthy participants are younger than the participants with Achilles tendinopathy and Achilles tendon rupture.
Key findings for healthy participants include an Achilles tendon mean thickness of 0.47 cm and CSA of 0.58 cm2, consistent with findings by Jackson et al.24 and Schmidt et al.25. While there are no significant differences between limbs in Achilles tendon length measures for healthy individuals10, there is a notably large range for all morphological values. Tendon thickness and CSA vary between individuals as a result of body size, sex, age, exercise, and comorbidities26,27,28,29. Therefore, when evaluating patients with injuries, it is important to use the uninvolved side for comparison. Further, when comparing individuals, using limb symmetry helps to account for body size, physical activity level, and other factors.
For individuals with Achilles tendinopathy, these findings, consistent with the current literature, show thicker tendons with larger CSA compared to asymptomatic limbs30, as well as tendon thickening in the symptomatic region. While CSA and tendon thickness are different within regions, the results also show that individuals post Achilles tendon rupture have Achilles tendon elongation, larger Achilles tendon CSA, and lower triceps surae muscle thickness/CSA in the involved compared to the uninvolved limb.
| Healthy | Achilles Tendinopathy | Achilles Tendon Rupture | |||||||
| Timepoint | Initial Evaluation | 6 weeks5 | 6 months4,5,20 | ||||||
| Side | Right (n=32) | Left (n=32) | Involved (n=72) | Uninvolved (n=72) | Involved | Uninvolved | Involved | Uninvolved | |
| AT Length to Gastrocnemius (cm) mean±SD (min, max) |
20.1±2.0 (15.8, 23.9) | 20.1±2.0 (16.0, 23.8) | 20.85±2.39 (13.44,25.93) | 20.57±2.26 (14.10, 24.60) | 24.00±2.305 (18.86, 29.33) | 22.16±2.265 (17.20, 28.87) | 22.3±2.720 24.14±2.345 (18.05, 29.97) | 20.6±2.720 22.39±2.375 (17.53, 28.97) | |
| AT Length to Soleus (cm) mean±SD (min, max) |
5.7±1.5 (2.9, 9.9) | 5.5±1.7 (2.1, 11.1) | 6.57±1.93 (3.17, 11.53) | 6.29±1.71 (2.88, 10.33) | |||||
| AT CSA (cm2) mean±SD |
0.58±0.10 (0.41, 0.79) | 0.58±0.12 (0.39, 0.79) | 0.91±0.49 (0.36, 2.49) | 0.70±0.25 (0.36, 1.61) | 3.31±1.004 2.77±0.655 | 0.61±0.124 0.59±0.155 | |||
| AT Thickness (cm) mean±SD (min, max) |
0.47±0.06 (0.33, 0.58) | 0.47±0.6 (0.38, 0.65) | 0.74±0.28 (0.39, 1.63) | 0.57±0.14 (0.38, 0.97) | |||||
| AT Thickening (mm) mean±SD (min, max) |
2.60±2.35 (0.09, 11.96) | 1.05±0.88 (0.00, 4.18) | |||||||
| Soleus Thickness (cm) mean±SD (min, max) |
1.30±0.34 (0.65, 2.28) | 1.25±0.34 (0.60, 2.55) | 1.12±0.335 (0.41, 1.81) | 1.29±0.325 (0.67, 2.17) | 1.02±0.315 (0.30, 1.71) | 1.39±0.385 (0.58, 2.46) | |||
| MG CSA (cm2) mean±SD (min, max) |
14.08±4.39 (5.98, 30.85) | 14.09±4.29 (6.80, 28.02) | 11.85±2.935 (5.14, 18.71) | 14.37±3.225 (8.15, 21.60) | 13.54±3.335 (6.30, 21.45) | 15.22±3.365 (8.12, 22.84) | |||
| LG CSA (cm2) mean±SD (min, max) |
8.06±2.41 (3.93, 14.30) | 7.92±2.28 (4.08, 13.63) | 6.89±1.855 (3.63, 13.02) | 8.85±2.025 (5.38, 13.90) | 8.41±2.135 (4.28, 15.69) | 9.36±1.985 (5.32, 14.60) | |||
Table 1: Representative results of healthy participants, participants with unilateral Achilles tendinopathy, and participants 6 months post Achilles tendon rupture. Abbreviations: AT = Achilles tendon; CSA = cross-sectional area; MG = medial gastrocnemius; LG = lateral gastrocnemius. Group data merged for presentation, 6 weeks n=54, 6 months n=565.
| Sex, female, n (%) | Age, years | BMI, kg/m2 | Treatment | |
| ATR: Zellers et al.20 (n=27) | 6 (22%) | 39±11 | 27.9±4.4 | 22 surgical, 5 non-surgical |
| ATR: Zellers et al.4 (n=22) | 5 (23%) | 40±11 | Not reported | 17 surgical, 5 non-surgical |
| ATR: Aufwerber et al.5 (n=56) | 12 (22%) | 38.4±8.2 | 25.1±2.9 | 56 surgical |
| Achilles tendinopathy (n=72) | 37 (51%) | 46±14 | 28.1±5.9 | |
| Healthy (n=32) | 13 (41%) | 31±12 | 26.1±4.9 |
Table 2: Demographics of each set of representative data. Abbreviations: ATR = Achilles tendon rupture. Subject data published in4 is a partial sample of subject data reported in20. Group data merged for presentation5.
List of Materials
| Aquaflex Stand Off Pad | Parker Laboratories | E8317C | |
| Aquasonic ultrasound Gel | Parker Laboratories | E8365AF | |
| Linear Array Ultrasound Probe L4-12t-RS | GE Healthcare | 5495987 | |
| LOGIC e Ultrasound | GE Healthcare | E8349PA | |
| Osirix Dicom Viewer | Pixmeo SARL | Software for measurements |
Lab Prep
Achilles tendon injuries occur throughout the lifespan and can negatively affect quality of life and overall health. Achilles tendinopathy is generally classified as an overuse injury associated with fusiform tendon thickening, neovascularization, and interstitial tendon degeneration. Current literature suggests these structural changes are associated with symptoms and lower physical activity levels, as well as symptoms and lower extremity function in the long term. Surgically and non-surgically managed Achilles tendon ruptures result in increased tendon cross-sectional area (CSA) and a lengthened Achilles tendon. Both structural outcomes have clinical implications, as larger CSA positively predicts function, whereas increased tendon lengthening predicts reduced function after Achilles tendon rupture. Given the relationship between structural changes associated with Achilles tendon injuries for both injury severity and injury recovery, it is critical to be able to quantify Achilles tendon structure reliably and accurately. Silbernagel's group has established a valid and reliable method for efficiently evaluating triceps surae muscle and tendon structure. In this protocol, B-mode musculoskeletal ultrasound imaging is used to measure triceps surae structure, including Achilles tendon thickness and CSA, soleus thickness, and the presence of additional findings (calcifications and bursitis). B-mode extended field-of-view is used to measure Achilles tendon length and gastrocnemius anatomical CSA. Finally, power Doppler is used to identify intratendinous neovascularization. Quantification of triceps surae structure allows for comparison between limbs as well as longitudinal changes in response to exercise and treatment for healthy individuals and those with Achilles tendon injuries. This protocol has been used in many research studies to date and proves valuable in understanding the relationship between tendon structure and injury development, severity, and recovery. As ultrasound devices are becoming more affordable and portable, this protocol proves promising as a clinical tool, given its quick and efficient methods.
Achilles tendon injuries occur throughout the lifespan and can negatively affect quality of life and overall health. Achilles tendinopathy is generally classified as an overuse injury associated with fusiform tendon thickening, neovascularization, and interstitial tendon degeneration. Current literature suggests these structural changes are associated with symptoms and lower physical activity levels, as well as symptoms and lower extremity function in the long term. Surgically and non-surgically managed Achilles tendon ruptures result in increased tendon cross-sectional area (CSA) and a lengthened Achilles tendon. Both structural outcomes have clinical implications, as larger CSA positively predicts function, whereas increased tendon lengthening predicts reduced function after Achilles tendon rupture. Given the relationship between structural changes associated with Achilles tendon injuries for both injury severity and injury recovery, it is critical to be able to quantify Achilles tendon structure reliably and accurately. Silbernagel's group has established a valid and reliable method for efficiently evaluating triceps surae muscle and tendon structure. In this protocol, B-mode musculoskeletal ultrasound imaging is used to measure triceps surae structure, including Achilles tendon thickness and CSA, soleus thickness, and the presence of additional findings (calcifications and bursitis). B-mode extended field-of-view is used to measure Achilles tendon length and gastrocnemius anatomical CSA. Finally, power Doppler is used to identify intratendinous neovascularization. Quantification of triceps surae structure allows for comparison between limbs as well as longitudinal changes in response to exercise and treatment for healthy individuals and those with Achilles tendon injuries. This protocol has been used in many research studies to date and proves valuable in understanding the relationship between tendon structure and injury development, severity, and recovery. As ultrasound devices are becoming more affordable and portable, this protocol proves promising as a clinical tool, given its quick and efficient methods.
Procedure
Achilles tendon injuries occur throughout the lifespan and can negatively affect quality of life and overall health. Achilles tendinopathy is generally classified as an overuse injury associated with fusiform tendon thickening, neovascularization, and interstitial tendon degeneration. Current literature suggests these structural changes are associated with symptoms and lower physical activity levels, as well as symptoms and lower extremity function in the long term. Surgically and non-surgically managed Achilles tendon ruptures result in increased tendon cross-sectional area (CSA) and a lengthened Achilles tendon. Both structural outcomes have clinical implications, as larger CSA positively predicts function, whereas increased tendon lengthening predicts reduced function after Achilles tendon rupture. Given the relationship between structural changes associated with Achilles tendon injuries for both injury severity and injury recovery, it is critical to be able to quantify Achilles tendon structure reliably and accurately. Silbernagel's group has established a valid and reliable method for efficiently evaluating triceps surae muscle and tendon structure. In this protocol, B-mode musculoskeletal ultrasound imaging is used to measure triceps surae structure, including Achilles tendon thickness and CSA, soleus thickness, and the presence of additional findings (calcifications and bursitis). B-mode extended field-of-view is used to measure Achilles tendon length and gastrocnemius anatomical CSA. Finally, power Doppler is used to identify intratendinous neovascularization. Quantification of triceps surae structure allows for comparison between limbs as well as longitudinal changes in response to exercise and treatment for healthy individuals and those with Achilles tendon injuries. This protocol has been used in many research studies to date and proves valuable in understanding the relationship between tendon structure and injury development, severity, and recovery. As ultrasound devices are becoming more affordable and portable, this protocol proves promising as a clinical tool, given its quick and efficient methods.
