Ex Vivo Organotypic Corneal Model of Acute Epithelial Herpes Simplex Virus Type I Infection
Summary
In this video article we describe the use of a new ex vivo model of acute herpes simplex virus type I corneal epithelial infection.
Abstract
Herpes keratitis is one of the most severe pathologies associated with the herpes simplex virus-type 1 (HSV-1). Herpes keratitis is currently the leading cause of both cornea-derived and infection-associated blindness in the developed world. Typical presentation of herpes keratitis includes infection of the corneal epithelium and sometimes the deeper corneal stroma and endothelium, leading to such permanent corneal pathologies as scarring, thinning, and opacity 1.
Corneal HSV-1 infection is traditionally studied in two types of experimental models. The in vitro model, in which cultured monolayers of corneal epithelial cells are infected in a Petri dish, offers simplicity, high level of replicability, fast experiments, and relatively low costs. On the other hand, the in vivo model, in which animals such as rabbits or mice are inoculated directly in the cornea, offers a highly sophisticated physiological system, but has higher costs, longer experiments, necessary animal care, and a greater degree of variability.
In this video article, we provide a detailed demonstration of a new ex vivo model of corneal epithelial HSV-1 infection, which combines the strengths of both the in vitro and the in vivo models. The ex vivo model utilizes intact corneas organotypically maintained in culture and infected with HSV-1. The use of the ex vivo model allows for highly physiologically-based conclusions, yet it is rather inexpensive and requires time commitment comparable to that of the in vitro model.
Protocol
All reagents and equipment were purchased sterile or were sterilized prior to the procedure. This article describes the steps of setting up the ex vivo model beginning with a pre-enucleated eye. In our experiments, we use fresh whole eyeballs from young (8-12 wks) albino rabbits (Pel-Freez Biologicals, Rogers, AR). In addition, we use human corneas obtained from the local eye bank. If performing enucleation yourself, take care to avoid damaging the cornea or the limbus during the procedure. Rabbit enucleation protocols can be found elsewhere 2.
Part 1: Excision of the Corneoscleral Button
- Wet a narrow strip of gauze with PBS and wrap it around the eyeball to facilitate holding it during the procedure.
- Use a sharp scalpel to make a tangential incision in the sclera, about 0.5 cm away from the limbus.
- Use sharp scissors to extend the incision and completely excise the corneoscleral button.
- Once the corneoscleral button is isolated, tease away the iris while holding the scleral rim with forceps. Avoid damaging the endothelium or exerting excessive stress on the cornea.
Part 2: Introduction of Cornea into Organotypic Culture
- Explanted corneas are cultured in Minimum Essential Medium (MEM) supplemented with Non-Essential Amino Acids (1X), L-Glutamine (2 mM), Penicillin (200 U/ml), and Streptomycin (200 μg/ml). An antifungal agent, such as amphotericin, may also be added if necessary.
- Prepare a 1% agarose solution in culture medium and keep it ready at 55 °C.
- Thoroughly rinse the cornea in sterile PBS containing Penicillin (200 U/ml) and Streptomycin (200 μg/ml).
- Place the cornea epithelial side down into a well of a sterile spot plate.
- Add the agarose-containing medium to the endothelial concavity of the cornea just enough to fill it completely. Allow ~1 min for the agarose to solidify.
- Place the cornea with the supporting gel scaffold epithelial side up into a 35 mm tissue culture dish and add culture medium to cover the epithelial surface.
- The cornea may be cultured in this way for over a week, with medium changes every 48 hr.
Part 3: Infection with HSV-1 and Treatment with Experimental Drugs
- Add 1 ml of medium containing the desired amount of virus into a 35 mm tissue culture dish. We usually infect with 1×104 PFU of strain KOS HSV-1 per cornea. Our stock titers are determined by performing plaque assays on CV-1 monolayers.
- Place the cornea together with the agarose scaffold epithelial side down into the virus-containing medium.
- Place the cornea into a tissue culture incubator to infect for 1 hr with intermittent rocking every 10-15 min.
- After 1 hr, aspirate the virus-containing medium and rinse 2-3 times with PBS to remove any residual viral particles.
- Place the cornea back into its previous position and add fresh culture medium to cover the epithelial surface.
- Experimental treatments may be started before or after infection, depending on the nature of the experiment.
- Culture medium is changed every 48 hr.
Part 4: Sample Collection
- Medium for plaque assay analysis. Mix the medium well and use it immediately for a plaque assay or store at -80 °C for later use if collecting samples at different time points.
- DNA, RNA, protein, or cells from corneal epithelium
- Remove the agarose scaffold and rinse the cornea well with PBS.
- Excise the ring of scleral tissue from the cornea to ensure that only corneal epithelial material is collected.
- Using a scalpel, scrape off the corneal epithelial cells into the appropriate buffer, depending on the type of material to be isolated. For isolation of DNA and RNA, we use the DNeasy Blood & Tissue Kit and the RNeasy Mini Kit, respectively (QIAGEN, Hilden, Germany). For collection of protein lysates, we use Laemmli buffer. For flow cytometry analysis of corneal epithelial cells, we pre-incubate the corneas in a small amount of trypsin to loosen the cells, and then dislodge them into trypsin with a scalpel. Since scraping the corneal epithelium does not yield equal amounts of tissue, it is important to include appropriate controls when analyzing the samples. We use 18S rRNA as a reference transcript in qRT-PCRs, GAPDH as a reference gene in qPCRs, and nucleolin as a loading control for Western blots.
- Tissue samples for immunohistochemistry or immunofluorescence
- Remove the agarose scaffold and rinse the cornea well with PBS.
- Depending on your experimental goal, use the cornea to make a paraffin tissue block or a frozen tissue block, as shown in the video. We follow standard procedures when preparing corneal tissue sections.
Representative Results
Most of the methods available for studying cells in tissue culture can be easily adapted for use in corneas infected with HSV-1 ex vivo. Shown here are representative results for a few of the most common techniques applicable to studying HSV-1 infection – qPCR (Figure 1D), qRT-PCR (Figure 1B), Western blot (Figure 1F), plaque assay (Figure 1C), and tissue immunofluorescence (Figure 1E).
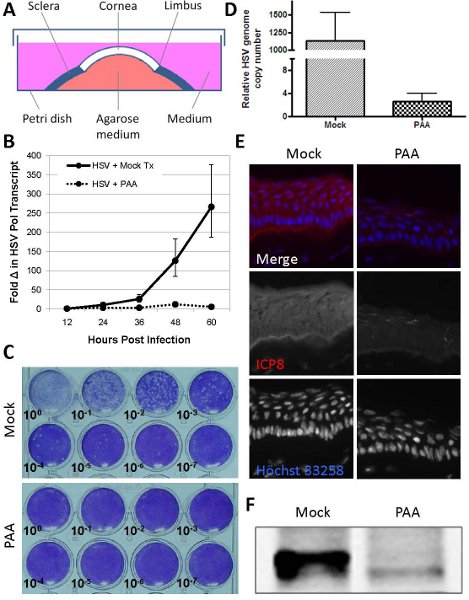
Figure 1. Analysis of corneas infected with HSV-1 ex vivo. (A) Schematic representation of the ex vivo model of acute corneal epithelial HSV-1 infection. (B-F) Analysis of corneas infected using the method outlined in this video article. Explanted rabbit corneas were infected with 1×104 PFU/cornea of strain KOS HSV-1 and cultured in the presence (PAA) or absence (Mock) of phosphonoacetic acid (400 μg/ml), a known inhibitor of HSV replication. (B) Total RNA was collected at the indicated time points, and viral transcription was assessed by qRT-PCR with primers for HSV-1 polymerase. Primers against 18S rRNA were used as a reference. n=3. Error bars indicate ± SEM. (C) Culture medium was collected at 48 hpi, and infectious particle production was assessed by plaque assay on CV-1 monolayers. (D) Total DNA was collected at 48 hpi, and viral genome replication was assessed in a qPCR assay with primers for the HSV-1 genome. Primers against GAPDH were used as a reference. n=3. Error bars indicate ± SEM. (E) Mock-treated corneas were flash-frozen at 48 hpi, sectioned, and analyzed by indirect immunofluorescence for the presence of a viral early protein (ICP8) within the infected epithelium. Nuclei are counterstained with Höchst 33258. (F) Protein lysates were collected at 48 hpi, and expression of a viral protein (ICP0) was assessed by Western blot. BCA assay was used to ensure equal loading of samples. hpi = hours post infection.
Discussion
In this video article we describe a method for studying acute corneal epithelial HSV-1 infection in an ex vivo model. This model is a useful stepping stone between the in vitro and the in vivo models, because it allows for physiologically-accurate validation of cell culture results and, thereby, limits the amount of animal experimentation that must be performed. In addition, the ex vivo model provides a unique and invaluable opportunity to study epithelial herpes infection in intact human corneas. Outlined below are some considerations that must be taken into account when using this model:
- It is important to emphasize that the approach outlined in this video article is not meant to be a model of herpes keratitis, but is rather a model of acute corneal epithelial HSV-1 infection. Herpes keratitis is a result of several confounding processes, including infection, inflammation, and the host immune response to the virus. Antigen-specific CD4+ and CD8+ T cell responses are a significant component of the pathogenesis of herpes keratitis, which cannot be reproduced in this model, because explanted corneas are not subject to infiltration by cells of the immune system. For this reason, they do not develop the typical epithelial dendritic ulcers and lack the stromal involvement classically observed in herpes stromal keratitis 3. Therefore, scoring of the disease severity and fluorescein imaging of corneal ulcers is not possible in the ex vivo model. In addition, most cases of herpes keratitis are caused by viral reactivation from latency. Since our approach relies on direct infection of explanted corneas with exogenous virus, it models acute HSV-1 corneal infection and not reactivation disease. For these reasons, the model presented here is not appropriate for understanding the overall pathology of the disease, but rather should be used to study viral replication and virus-host interactions strictly in the corneal epithelium.
- The ex vivo herpes keratitis model yields results with greater variability than the in vitro tissue culture experiments. This is probably due to the fact that each cornea is collected from a different rabbit and may be processed slightly differently. Human corneas show an even greater variability of results than rabbit corneas, because they originate from donors of variable age, race, and health status, and are preserved for different amounts of time postmortem. However, with the use at least five corneas per experimental treatment, we were able to generate statistically-reliable data.
- The traditional method for culturing explanted corneas 4-5 suggests using just enough culture medium to cover the limbus of the cornea. We found that increasing the amount of medium to completely cover the epithelium yields more consistent results, likely due to minimizing the differences between individual corneas’ access to the medium and experimental drugs contained therein.
- When using rabbit corneas for any application utilizing antibodies, it is important to keep in mind that traditional antibodies with specificities to human, mouse, rat, etc. are likely to not cross-react against rabbit antigens. In addition, secondary anti-rabbit antibodies of course cannot be used in these applications. For these reasons, we use human corneas in experiments involving antibody staining of cellular targets.
- When collecting epithelial cells for flow cytometry analysis, the experimenter must be cautious about the effects of trypsin on membrane-bound proteins. Thus, for detection of surface proteins, it may be beneficial to use other means of dislodging the cells, such as collagenases or non-trypsin proteases.
- Animal models of herpes keratitis rely on corneal scarification prior to inoculation with the virus. We have been able to achieve consistent levels of infection without scarifying the explanted corneas. This is most likely due to the absence of the tear film and blinking that rapidly eliminate the virus from the corneal surface in a live animal.
Potential modifications of the ex vivo herpes keratitis model not explored in this video article:
- Genetic modification of corneal epithelial cells prior to HSV-1 infection by using DNA delivery methods utilized in cell culture and in gene therapy research, such as transfection, viral delivery, and gene gunning 6.
- Use of GFP-expressing HSV-1 7-8 or FITC-conjugated anti-HSV antibodies 9-10 to visually assess the extent of infection.
Declarações
The authors have nothing to disclose.
Acknowledgements
The support of the Lions Eye Bank of Delaware Valley was invaluable for this work. Primary mouse monoclonal antibody against ICP8 was a kind gift from Dr. David Knipe (Harvard Medical School). We also thank Dr. Stephen Jennings (Drexel University College of Medicine) and Dr. Peter Laibson (Wills Eye Institute) for helpful discussions and expertise.
Materials
| Reagents/Supplies | Company | Catalogue # |
| Minimum Essential Medium (MEM) | Mediatech | 10-010-CV |
| Non-Essential Amino Acids (100x solution) | Mediatech | 25-025-CI |
| L-Glutamine | Mediatech | 25-005-CI |
| Penicillin G Sodium Salt | Sigma | P3032 |
| Streptomycin Sulfate Salt | Sigma | S9137 |
| Agarose | Invitrogen | 15510-027 |
| Phosphate Buffered Saline (PBS) | Prepared in lab | N/A |
| Trypsin EDTA (1x) | Mediatech | 25-053-CI |
| DNeasy Blood & Tissue Kit | QIAGEN | 69504 |
| RNeasy Mini Kit | QIAGEN | 74104 |
| Laemmli Buffer | Prepared in lab | N/A |
| Optimal Cutting Temperature (OCT) Compound | Tissue-Tek | 4583 |
| Whole Rabbit Eyes (Young) | Pel-Freez | 41211-2 |
| Human Corneas and Whole Eyes | Local Eye Bank | N/A |
| 12 Well Porcelain Spot Plate | Avogadro’s Lab Supply | 1877 |
| 35 mm Tissue Culture Dish | Falcon | 353001 |
| 6 Well Cell Culture Plate | Greiner Bio-One | 657160 |
| Cryomold Intermediate | Tissue-Tek | 4566 |
Referências
- Kaye, S., Choudhary, A. Herpes simplex keratitis. Prog. Retin. Eye Res. 25, 355-380 (2006).
- Holmberg, B. J. Enucleation of exotic pets. Journal of Exotic Pet Medicine. 16, 88-94 (2007).
- Remeijer, L., Osterhaus, A., Verjans, G. Human herpes simplex virus keratitis: the pathogenesis revisited. Ocul. Immunol. Inflamm. 12, 255-285 (2004).
- Foreman, D. M., Pancholi, S., Jarvis-Evans, J., McLeod, D., Boulton, M. E. A simple organ culture model for assessing the effects of growth factors on corneal re-epithelialization. Exp. Eye Res. 62, 555-564 (1996).
- Xu, K. P., Li, X. F., Yu, F. S. Corneal organ culture model for assessing epithelial responses to surfactants. Toxicol. Sci. 58, 306-314 (2000).
- Klausner, E. A., Peer, D., Chapman, R. L., Multack, R. F., Andurkar, S. V. Corneal gene therapy. J. Control Release. 124, 107-133 (2007).
- Halford, W. P. ICP0 antagonizes Stat 1-dependent repression of herpes simplex virus: implications for the regulation of viral latency. Virol. J. 3, 44 (2006).
- Bhattacharjee, P. S. Effective treatment of ocular HSK with a human apolipoprotein E mimetic peptide in a mouse eye model. Invest Ophthalmol Vis. Sci. 49, 4263-4268 (2008).
- Novitskaya, E. S. Difficulties imaging herpes simplex keratitis with fluorescein isothiocynate-labeled anti-HSV-1 antibodies in an ex vivo model. Cornea. 28, 421-425 (2009).
- Sharma, A., Shimeld, C. In vivo immunofluorescence to diagnose herpes simplex virus keratitis in mice. Br. J. Ophthalmol. 81, 785-788 (1997).

